Abstract
This study used ecological momentary assessment (EMA) to explore the correlates of suicidal ideation (SI) instability in patients hospitalized for depression and SI. Thirty-nine adult inpatients were given smartphones with visual analogue scales to rate current depressed mood, anger/irritability, feeling socially connected, and SI three times a day throughout hospitalization. Affective Lability Scales (ALS) were also completed at baseline. SI instability was correlated with SI intensity, depressed mood instability, and social connection instability. Social connection instability was not associated with SI instability after controlling for depressed mood instability. ALS scores were not associated with EMA-derived SI instability. Participants with multiple past suicide attempts experienced greater SI instability. More research examining the clinical significance of SI instability is warranted.
INTRODUCTION
According to the DSM, major depression involves periods of low mood that are both stable (i.e., “present most of the day, nearly every day”) and persistent (i.e., “for at least 2 consecutive weeks”) (American Psychiatric Association, Citation2013, p. 163). In actuality, depressed individuals experience rapid and intense mood fluctuations over the course of hours/days (Bowen, Peters, Marwaha, Baetz, & Balbuena, Citation2017; Houben, Van Den Noortgate, & Kuppens, Citation2015; Köhling et al., Citation2016; Peters, Balbuena, Baetz, Marwaha, & Bowen, Citation2015; Thompson, Berenbaum, & Bredemeier, Citation2011; Thompson et al., Citation2012), including brief periods of high mood (Bylsma, Taylor-Clift, & Rottenberg, Citation2011; Peeters, Berkhof, Delespaul, Rottenberg, & Nicolson, Citation2006; Peeters, Nicolson, Berkhof, Delespaul, & deVries, Citation2003; Thompson et al., Citation2012), which are neither acknowledged in the DSM (American Psychiatric Association, Citation2013), nor captured by depression rating scales (Ben-Zeev, Young, & Madsen, Citation2009; Bowen, Balbuena, & Baetz, Citation2014; Solhan, Trull, Jahng, & Wood, Citation2009). The DSM-5 mixed features specifier allows for features of elevated mood (e.g., high energy, goal-directed activity) in depressive episodes, but the requirement that these be present for “the majority of days” discounts brief, recurrent mood elevations (American Psychiatric Association, Citation2013, p. 184). Mood instability is reported by up to 60% of people with depression when it is assessed directly by questionnaires (Peters et al., Citation2015; Solmi et al., Citation2016; Thompson et al., Citation2011), and is apparent when measured prospectively with ecological momentary assessment (EMA; Bowen et al., Citation2017; Bylsma et al., Citation2011; Houben et al., Citation2015; Köhling et al., Citation2016; Peeters et al., Citation2006; Solhan et al., Citation2009; Thompson et al., Citation2012; but see also Bos, de Jonge, & Cox, Citation2019; Koval, Pe, Meers, & Kuppens, Citation2013; Verdolini et al., Citation2019).
Mood instability is associated with suicidality and self-harm (Palmier-Claus, Taylor, Varese, & Pratt, Citation2012; Peters, Baetz, Marwaha, Balbuena, & Bowen, Citation2016; Peters, John, Bowen, Baetz, & Balbuena, Citation2018), even after controlling for depressed mood (Bowen et al., Citation2015; Peters, Balbuena, Marwaha, Baetz, & Bowen, Citation2016). Similar to mood, suicidal ideation (SI) can fluctuate considerably over a day (Forkmann et al., Citation2018; Hallensleben et al., Citation2018; Kleiman et al., Citation2017; Nock, Prinstein, & Sterba, Citation2009; Witte, Fitzpatrick, Joiner, & Schmidt, Citation2005; Witte, Fitzpatrick, Warren, Schatschneider, & Schmidt, Citation2006). Accordingly, there have been recent calls for EMA research to capture the dynamic nature of suicidality (Davidson, Anestis, & Gutierrez, Citation2017; Kleiman et al., Citation2017; Nock, Citation2016; Witte et al., Citation2006). So far, most EMA studies have examined factors that predict SI at subsequent time points (Ben-Zeev, Young, & Depp, Citation2012; Husky et al., Citation2017; Kleiman et al., Citation2017). It may also be pertinent to elucidate the factors associated with SI instability—the overall volatility and unpredictability of an individual’s desire to end their life. One study did find greater SI instability in individuals with multiple suicide attempts compared to those without (Witte et al., Citation2005, Citation2006), although contradictory results have been reported (Peters, Mereish, Solomon, Spirito, & Yen, Citation2019).
The main goal of this study was to use EMA to explore the effect of mood instability on SI instability in patients hospitalized for a major depressive episode. In addition to depressed mood, we also measured anger/irritability because it is associated with mood instability (Oliver & Simons, Citation2004), depression (Judd, Schettler, Coryell, Akiskal, & Fiedorowicz, Citation2013), and suicidality (albeit inconsistently, in clinical samples; Massimiliano, Perret, Turecki, & Geoffroy, Citation2018). Our second goal was to use EMA to measure instability in feeling socially connected/close to others, similar to the concept of belongingness from the interpersonal theory of suicide (Kleiman et al., Citation2017; Van Orden et al., Citation2010), and to examine potential associations with mood instability and SI instability. Past research has documented considerable within-person variability in feelings of loneliness (Kleiman et al., Citation2017), but it is unclear to what extent this correlates with mood and SI instability. It was hypothesized that instability in all three variables (i.e., depressed mood, anger/irritability, social connectedness), but not necessarily their average level of intensity, would be associated with SI instability, and that mood instability and social connectedness instability would be related. Additional goals were to compare the predictive value of questionnaire-rated mood instability on SI instability to EMA-derived mood instability; to compare SI instability between groups defined by the presence of past suicide attempts, in an attempt to replicate previous results (Witte et al., Citation2005, Citation2006); and finally, because mood instability has been associated with poorer treatment response (Stange et al., Citation2016) and symptom recurrence (Wichers et al., Citation2010), to determine if improvement in depression and SI throughout hospitalization are associated with mood and SI instability.
METHODS
Sample
The sample consisted of 39 patients (M age = 36.3 years, SD = 13.0; 69.2% female) hospitalized on a psychiatric unit with a chief diagnosis of a major depressive episode secondary to major depressive disorder or bipolar disorder (n = 12; 30.8%). To be included patients had to be 18-70 years old, be experiencing suicidal ideation at the time of admission, be admitted voluntarily, and not be withdrawing from any substances. All participants provided written informed consent and the study received local ethical approval. No compensation was provided.
Procedure
Recruitment began in December of 2016. Patients were referred to the study by their inpatient psychiatrist or social worker. A trained research assistant then met with potential participants, explained the study, obtained consent, administered the Mini-International Neuropsychiatric Interview (Sheehan et al., Citation1998) to confirm eligibility, showed participants how to use the phone, and had participants complete baseline questionnaire assessments (Time 1). Participants remained in the study until they were discharged. At this time questionnaire assessments were repeated (Time 2).
Materials and Measures
Beck Depression Inventory
Depressive symptoms were assessed at Time 1 (study entry) and Time 2 (study exit/discharge) with the Beck Depression Inventory (BDI; Beck, Steer, & Brown, Citation1996). The BDI has 21 items, scored 0 to 4, which are summed to yield a total score reflecting greater depression severity. The internal consistencies were good to excellent (α = .89 and .94). BDI change scores (Time 1–Time 2) were used to measure depression improvement throughout hospitalization.
Beck Scale for Suicide Ideation
SI at Time 1 and Time 2 was assessed with the Beck Scale for Suicide Ideation (BSS; Beck & Steer, Citation1991). The BSS has 21 items, scored 0–2, the first 19 of which are summed to yield a total score reflecting greater SI. The internal consistencies were excellent (α = .94 and .97). Responses to item 20 were used to assess past suicide attempts. BSS change scores (Time 1–Time 2) were used to measure SI improvement throughout hospitalization.
Affective Lability Scales
Mood instability at Time 1 was assessed with the short Affective Lability Scales (ALS; Oliver & Simons, Citation2004). The ALS consists of 18 items rated on a Likert scale from 1 to 4 (Oliver & Simons, Citation2004). There are six ALS subscales that represent rapid and intense fluctuations between different combinations of mood states: euthymia/anxiety, euthymia/depression, euthymia/elation, euthymia/anger, anxiety/depression, and depression/elation. The total ALS (the sum of all 18 items) and each subscale had adequate to excellent internal consistency (α = .75–.94).
EMA
Each participant was provided with an Android smartphone for the duration of the study. Phones were installed with Ethica (Hashemian, Qian, Stanley, & Osgood, Citation2012; Knowles, Stanley, & Osgood, Citation2014) to facilitate data collection. This application employed four questions, each rated on a visual analogue scale from 0 to 100, designed to reflect the following constructs: depressed mood (“How depressed do you feel right now?”), anger/irritability (“How irritable/angry do you feel right now?”), perceived social connectedness (“How close or connected to people do you feel right now?”), and suicidality (“How suicidal are you right now?”). Participants were prompted to answer each question three times a day at 09:00, 15:00, and 20:00, with a 60-minute window to answer each question, after which the response was set to missing if no response was given.
Analysis
Missing Data
Two participants did not complete any Time 1 questionnaires, and 14 participants were discharged before completing Time 2 questionnaires. Imputation was not attempted for these individuals, and analyses with questionnaire data had reduced sample sizes as a result (Time 1, n = 37; BDI/BSS change scores, n = 25). If questionnaires were completed but some items were missing then these were filled using random forest imputation (Stekhoven & Bühlmann, Citation2012). For each questionnaire, less than 1% of responses were missing.
Creation of EMA Variables
Responses to the EMA questions were used to create variables representing intensity and instability. Intensity was defined as the mean of all ratings for a question over the study period. Instability was defined as the mean squared successive difference (von Neumann, Kent, Bellinson, & Hart, Citation1941), which takes into account both the within-person variability and the temporal sequence between measurements (Solhan et al., Citation2009). Mean square successive difference scores were left skewed but were normalized after a square root transformation. Social connection instability was not normally distributed after transformation, but this corrected after removing one strong outlier (score = 92.8; range excluding this score = 2.32–44.8) that was larger than three times the IQR (19.8) added to the 75th percentile (33.0). Most intensity scores were also left skewed, so they were also normalized by square rooting. The final analysis used eight EMA variables: SI intensity (SIINT), SI instability (SIINST), depressed mood intensity (DEPINT), depressed mood instability (DEPINST), anger/irritability intensity (ANGINT), anger/irritability instability (ANGINST), social connection intensity (CONINT), and social connection instability (CONINST).
Exploratory Correlations
Pairwise correlations between all variables were calculated. Prior to calculating each correlation, scatter plots were used to assess for linearity and heteroscedasticity. Pearson’s r was calculated if assumptions were met. Nonparametric Kendall’s τB correlation coefficients were used to explore the associations for the following variables that were not normally distributed: ALS euthymia/anger, ALS anxiety/depression, BDI change scores, and BSS change scores.
Multiple Regression Models
Multiple linear regression models predicting SIINST were created to observe what variables remained associated with SIINST when multiple predictors were included in the same model. In general, we were interested in models that included different instability variables, pairs of EMA intensity and instability variables (e.g., DEPINT and DEPINST), and instability variables with their ALS counterparts (e.g., DEPINST and the ALS euthymia/depression subscale). We did not include any variables in the regression analysis that had nonsignificant relationships with SIINST in the correlation analyses. However, given the small sample size and possibility of type II error, we did add variables with small but nonsignificant p values if the effect size was not trivial (r ∼ .20 or higher; Dupont, Citation2009).
Group Comparisons
We conducted Wilcoxon rank-sum tests to compare SIINST between groups defined by past suicide attempts on the BSS: no past attempts (n = 9) vs. past attempt(s) (n = 28), one past attempt (n = 12) vs. multiple past attempts (n = 16), no past attempts (n = 9) vs. one past attempt (n = 12). We chose a nonparametric test due to the small and unbalanced group sizes, as well as concerns about data normality. Two participants had outlying scores, so the comparisons were repeated without their data to ensure the results did not differ. Differences in SIINST could be driven by differences in DEPINST, so we also compared DEPINST between any groups that had significant differences in SIINST.
RESULTS
EMA Usage and Compliance
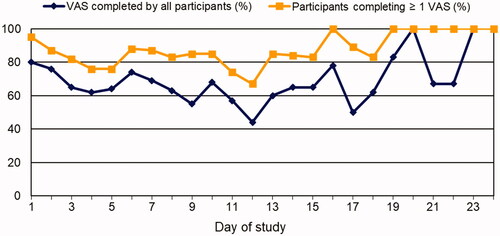
The average number of days participants were enrolled in the study was 12.0 (SD = 5.61). VAS completion rates by study duration are presented in . The correlation between total VAS completion rates and study duration was not statistically significant (r = .07, p = .69). Total VAS completion rates for each participant were not significantly associated with Time 1 BDI scores (r = .26, p = .12), DEPINT (r = .17, p = .30), DEPINST (r = −.14, p = .40), Time 1 BSS scores (r = .19, p = .27), SIINT (r = .03, p = .88), or SIINST (r = −.10, p = .56).
Exploratory Correlations
Pairwise correlations between EMA variables are presented in and . SIINST was significantly positively correlated with SIINT, DEPINST, and CONINST. Bivariate correlations between EMA and questionnaire variables are presented in . ALS total and subscale scores were not significantly correlated with any EMA instability variable. Time 1 BDI scores (M = 42.1, SD = 10.8) were positively correlated with DEPINT, SIINT, and CONINST. Time 1 BSS scores (M = 20.4, SD = 10.1) were positively correlated with DEPINT, SIINT, and ANGINT; the correlation with SIINST was small and borderline significant (r = .28, p = .09). BDI and BSS change scores were not significantly correlated with any EMA variable.
FIGURE 2. Bivariate correlations between EMA variables. Variables were derived from ratings on visual analogue scales measuring suicidal ideation (SI), depressed mood (DEP), feeling socially connected/close to others (CON), and anger/irritability (ANG). Intensity variables were defined as the mean of all ratings. Instability variables were defined as the mean squared successive difference. Correlation not shown if r < .20 and p > .20, except for CONINT with DEPINT (r = −.22, p =.17) and ANGINST (r = −.21, p = .19). EMA: ecological momentary assessment. *p < .05; **p < .01; ***p < .001.
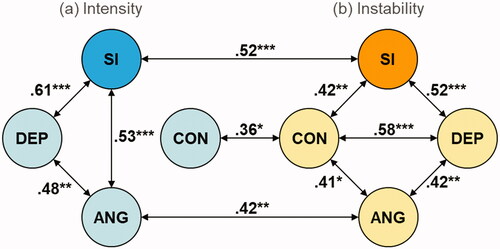
TABLE 1. Pairwise correlations between EMA variables.
TABLE 2. Correlations between EMA indices (first column) and questionnaire scores (first row).
Multiple Regression Models
First we estimated a model with Time 1 BSS scores and SIINT predicting SIINST; the effect of SIINT remained significant (β = .61, SE = 1.02, p = .006), whereas the effect of Time 1 BSS scores became negative and nonsignificant (β = −.16, SE = 0.26, p = .47). Therefore, we did not include Time 1 BSS scores in any subsequent models. Based on the remaining results, we estimated models predicting SIINST with different combinations of DEPINST, CONINST, and SIINT (see ). Both DEPINST and CONINST remained significant after adding SIINT to the model. When DEPINST and CONINST were included in the same model the coefficient for CONINST became nonsignificant, whereas the coefficient for DEPINST remained significant.
TABLE 3. Multiple linear regression models predicting suicidal ideation instability.
We conducted additional analyses with ANGINST because the effect size was roughly “small” and it was one of the hypothesized correlates of SIINST. In a model with SIINT, the effect remained largely unchanged (β = .22, SE = 0.15, p = .12), although it became trivial in size with DEPINST in the model (β = −.03, SE = 0.17, p = .83); DEPINST had a significant effect (β = .54, SE = 0.18, p = .001).
We also estimated exploratory models with ALS euthymia/anxiety scores predicting SIINST given the size of the correlation (the largest of all ALS variables) and the relatively small p value (r = .27, p = .10). SIINT and CONINST were used as covariates as these had the largest associations with ALS euthymia/anxiety scores. The effect decreased after controlling for SIINT (β = .16, SE = 0.67, p = .30) or CONINST (β = .16, SE = 0.61, p = .29), and was trivial in size with both covariates in the model (β = .09, SE = 0.57, p = .54).
Group Comparisons
SIINST group means and comparisons are presented in . The only statistically significant difference was between participants with multiple past attempts compared to individuals with one past attempt. DEPINST scores did not significantly differ between these groups (M = 21.0 and 23.0, respectively; z = 0.33, p = .75).
TABLE 4. Mean suicidal ideation instability with comparisons by past suicide attempt status.
DISCUSSION
It should be first stated that given the large number of exploratory analyses, significant correlations may have occurred due to chance; the results could be useful for generating hypotheses, but replication is required before drawing firm conclusions.
Correlates of SI Instability
SI intensity was strongly associated with SI instability, demonstrating that patients who were more suicidal, on average, throughout hospitalization also tended to have greater SI instability. The potential significance of this finding is that rapid but temporary reductions in SI could be misinterpreted as improvement in patients who are likely to remain more severely suicidal during hospital admissions. The only other EMA variables clearly associated with SI instability were depressed mood instability and instability in feelings of social connectedness, although the former may be more proximally related to SI instability than the latter. In contrast to our expectations, anger/irritability instability was not significantly associated with SI instability, and the small nonsignificant association that was present appeared to be due to the correlation with depressed mood instability.
Among the questionnaire variables, Time 1 BSS scores had the largest association with SI instability, consistent with EMA-derived SI intensity also being correlated with SI instability. The finding that BDI and BSS change scores were unrelated to SI instability and depressed mood instability suggests that, in this sample, it would have been inappropriate to conflate instability and improvement when it comes to depression and suicidality. However, missing data makes this result difficult to interpret as we cannot rule out the possibility that participants who were unreachable at Time 2 had different outcomes.
Mood Instability Questionnaires vs. EMA Indices
One noteworthy finding is that ALS scores were not significantly associated with SI instability, although the correlation with the ALS euthymia/anxiety subscale was nontrivial in size and approached statistical significance, in keeping with previous research (Ben-Zeev et al., Citation2012; Berman, Citation2018; Forkmann et al., Citation2018; Husky et al., Citation2017). The ALS and EMA-derived mood instability indices purportedly measure the same phenomenon (Marwaha et al., Citation2014; Solhan et al., Citation2009), yet this finding suggests the ALS may not sufficiently discriminate individuals with unstable SI. ALS scores were also unrelated to the other EMA instability variables, further suggesting these may not be measuring the same underlying construct. A similar finding was reported by Links, Heisel, and Garland (Citation2003), who suggested the ALS may be a better index of affective intensity than affective instability. One ostensible difference is that the ALS measures shifts between discrete emotions (i.e., euthymia to anger, anxiety to depression) and not fluctuations within a particular emotional state (Oliver & Simons, Citation2004). A question for future research is whether shifts between emotions or within emotional states are similarly related to suicidality, and the extent to which these phenomena are independent.
SI Instability by Past Suicide Attempts
Consistent with a previous study of a student sample (Witte et al., Citation2005, Citation2006), we found that participants with multiple past suicide attempts experienced the highest degree of SI instability, although unlike this past study, we did not find higher SI instability in participants with a previous attempt compared to those without (Witte et al., Citation2005, Citation2006). This discrepancy could have been due to the sample differences, as most of the subgroup without past attempts would not have been depressed (Witte et al., Citation2005, Citation2006). A more recent longitudinal study of hospitalized adolescents found that SI instability did not predict future suicide attempts, nor was SI instability associated with the mean of all SI ratings over a 6-month period (Peters et al., Citation2018). SI in this study was measured weekly with questionnaires (Peters et al., Citation2018), so it may be misleading to compare “instability” variables with differing sampling frequencies (Ebner-Priemer & Sawitzki, Citation2007; Thompson et al., Citation2012). More research using diverse samples, additional measurement schemes and covariates, and longitudinal designs is needed to fully understand the clinical significance of SI instability, particularly in relation to future suicide attempts.
Feasibility of Smartphone EMA
The current study adds to the existing research supporting the feasibility of smartphone EMA among depressed inpatients (Ben-Zeev et al., Citation2012; Hallensleben et al., Citation2018; Husky et al., Citation2014; Kleiman et al., Citation2017). Previous studies have tended to limit sampling to one week (Ben-Zeev et al., Citation2012; Hallensleben et al., Citation2018; Husky et al., Citation2014), although we sampled participants for the duration of admission (up to 24 days). Therefore, it is notable that EMA compliance did not decrease as sampling durations increased. Furthermore, we did not find EMA compliance to be significantly associated with baseline depression/SI severity, or EMA-derived depression/SI intensity during hospitalization, further suggesting illness severity among depressed patients does not preclude the use of EMA.
Limitations
Major limitations were the small, heterogeneous sample (i.e., patients with unipolar or bipolar depression, and various comorbidities) and the lack of long-term follow-up that prevented us from considering outcomes such as readmission to hospital and future suicide attempts. It is possible that some of the smaller correlations in the .20–.29 range would have been statistically significant had a larger sample been recruited. We also did not compare patients admitted for a suicide attempt to the rest of the sample, nor were treatments monitored. Patients were not excluded if they had comorbid diagnoses that could have inflated estimates of mood/SI instability, such as personality disorders or PTSD (American Psychiatric Association, Citation2013; Marwaha et al., Citation2014; Santangelo et al., Citation2014), although doing so would have limited the generalizability of the sample. The fact that we did not measure anxiety/agitation is another limitation, as it tends to be associated with SI (Ben-Zeev et al., Citation2012; Berman, Citation2018; Forkmann et al., Citation2018; Husky et al., Citation2017). EMA compliance was generally satisfactory, although missing data on Time 2 questionnaires was common and further limits the results from these analyses. This study was also not designed to answer the question of whether depressed individuals experience greater mood instability than nondepressed individuals, which remains debated (Bos et al., Citation2019; Koval et al., Citation2013).
CONCLUSIONS
SI instability in depressed inpatients can be successfully captured with smartphone EMA. These preliminary results suggest that SI instability is associated with more intense suicidality and depressed mood instability during hospitalization. A single assessment with the ALS may not adequately distinguish depressed patients with greater SI instability from patients with more stable SI. SI instability also seems to be more pronounced in patients with multiple past suicide attempts, although the clinical significance of this finding in relation to future suicide attempts remains unknown. More research on SI instability using EMA is warranted.
Additional information
Notes on contributors
Evyn M. Peters
Evyn M. Peters, Department of Psychiatry, University of Saskatchewan, Saskatoon, Saskatchewan, Canada.
Lisa Yue Dong
Lisa Yue Dong, Department of Psychiatry, University of Saskatchewan, Saskatoon, Saskatchewan, Canada.
Teena Thomas
Teena Thomas, Department of Computer Science, University of Saskatchewan, Saskatoon, Saskatchewan, Canada.
Sara Khalaj
Sara Khalaj, Department of Psychiatry, University of Saskatchewan, Saskatoon, Saskatchewan, Canada.
Lloyd Balbuena
Lloyd Balbuena, Department of Psychiatry, University of Saskatchewan, Saskatoon, Saskatchewan, Canada.
Marilyn Baetz
Marilyn Baetz, Department of Psychiatry, University of Saskatchewan, Saskatoon, Saskatchewan, Canada.
Nathaniel Osgood
Nathaniel Osgood, Department of Computer Science, University of Saskatchewan, Saskatoon, Saskatchewan, Canada.
Rudy Bowen
Rudy Bowen, Department of Psychiatry, University of Saskatchewan, Saskatoon, Saskatchewan, Canada.
REFERENCES
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
- Beck, A. T., & Steer, R. A. (1991). Beck scale for suicide ideation manual. San Antonio, TX: The Psychological Corporation.
- Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Manual for the Beck depression inventory-II. San Antonio, TX: Psychological Corporation.
- Ben-Zeev, D., Young, M. A., & Depp, C. A. (2012). Real-time predictors of suicidal ideation: Mobile assessment of hospitalized depressed patients. Psychiatry Research, 197(1–2), 55–59. doi:https://doi.org/10.1016/j.psychres.2011.11.025
- Ben-Zeev, D., Young, M. A., & Madsen, J. W. (2009). Retrospective recall of affect in clinically depressed individuals and controls. Cognition & Emotion, 23(5), 1021–1040. doi:https://doi.org/10.1080/02699930802607937
- Berman, A. L. (2018). Risk factors proximate to suicide and suicide risk assessment in the context of denied suicide ideation. Suicide & Life-Threatening Behavior, 48(3), 340–352. doi:https://doi.org/10.1111/sltb.12351
- Bos, E. H., Jonge, P., & Cox, R. F. A. (2019). Affective variability in depression: Revisiting the inertia–instability paradox. British Journal of Psychology (London, England: 1953), 110(4), 814–827. doi:https://doi.org/10.1111/bjop.12372
- Bowen, R. C., Balbuena, L., & Baetz, M. (2014). Lamotrigine reduces affective instability in depressed patients with mixed mood and anxiety disorders. Journal of Clinical Psychopharmacology, 34(6), 747–749. doi:https://doi.org/10.1097/JCP.0000000000000164
- Bowen, R., Balbuena, L., Peters, E. M., Leuschen-Mewis, C., & Baetz, M. (2015). The relationship between mood instability and suicidal thoughts. Archives of Suicide Research, 19(2), 161–171. doi:https://doi.org/10.1080/13811118.2015.1004474
- Bowen, R., Peters, E., Marwaha, S., Baetz, M., & Balbuena, L. (2017). Moods in clinical depression are more unstable than severe normal sadness. Frontiers in Psychiatry, 8, 56. doi:https://doi.org/10.3389/fpsyt.2017.00056
- Bylsma, L. M., Taylor-Clift, A., & Rottenberg, J. (2011). Emotional reactivity to daily events in major and minor depression. Journal of Abnormal Psychology, 120(1), 155–167. doi:https://doi.org/10.1037/a0021662
- Davidson, C. L., Anestis, M. D., & Gutierrez, P. M. (2017). Ecological momentary assessment is a neglected methodology in suicidology. Archives of Suicide Research: Official Journal of the International Academy for Suicide Research, 21(1), 1–11. doi:https://doi.org/10.1080/13811118.2015.1004482
- Dupont, W. D. (2009). Statistical modeling for biomedical researchers: A simple introduction to the analysis of complex data (2nd ed.). Cambridge: Cambridge University Press.
- Ebner-Priemer, U. W., & Sawitzki, G. (2007). Ambulatory assessment of affective instability in borderline personality disorder. European Journal of Psychological Assessment, 23(4), 238–247. doi:https://doi.org/10.1027/1015-5759.23.4.238
- Forkmann, T., Spangenberg, L., Rath, D., Hallensleben, N., Hegerl, U., Kersting, A., & Glaesmer, H. (2018). Assessing suicidality in real time: A psychometric evaluation of self-report items for the assessment of suicidal ideation and its proximal risk factors using ecological momentary assessments. Journal of Abnormal Psychology, 127(8), 758–769. doi:https://doi.org/10.1037/abn0000381
- Hallensleben, N., Spangenberg, L., Forkmann, T., Rath, D., Hegerl, U., Kersting, A., … Glaesmer, H. (2018). Investigating the dynamics of suicidal ideation. Crisis, 39(1), 65–69. doi:https://doi.org/10.1027/0227-5910/a000464
- Hashemian, M., Qian, W., Stanley, K. G., & Osgood, N. D. (2012). Temporal aggregation impacts on epidemiological simulations employing microcontact data. BMC Medical Informatics and Decision Making, 12(1), 1–15. doi:https://doi.org/10.1186/1472-6947-12-132.
- Houben, M., Van Den Noortgate, W., & Kuppens, P. (2015). The relation between short-term emotion dynamics and psychological well-being: A meta-analysis. Psychological Bulletin, 141(4), 901–930. doi:https://doi.org/10.1037/a0038822
- Husky, M., Olié, E., Guillaume, S., Genty, C., Swendsen, J., & Courtet, P. (2014). Feasibility and validity of ecological momentary assessment in the investigation of suicide risk. Psychiatry Research, 220(1–2), 564–570. doi:https://doi.org/10.1016/j.psychres.2014.08.019
- Husky, M., Swendsen, J., Ionita, A., Jaussent, I., Genty, C., & Courtet, P. (2017). Predictors of daily life suicidal ideation in adults recently discharged after a serious suicide attempt: A pilot study. Psychiatry Research, 256, 79–84. doi:https://doi.org/10.1016/j.psychres.2017.06.035
- Judd, L. L., Schettler, P. J., Coryell, W., Akiskal, H. S., & Fiedorowicz, J. G. (2013). Overt irritability/anger in unipolar major depressive episodes: Past and current characteristics and implications for long-term course. JAMA Psychiatry, 70(11), 1171–1180. doi:https://doi.org/10.1001/jamapsychiatry.2013.1957
- Kleiman, E. M., Turner, B. J., Fedor, S., Beale, E. E., Huffman, J. C., & Nock, M. K. (2017). Examination of real-time fluctuations in suicidal ideation and its risk factors: Results from two ecological momentary assessment studies. Journal of Abnormal Psychology, 126(6), 726–738. doi:https://doi.org/10.1037/abn0000273
- Knowles, D. L., Stanley, K. G., & Osgood, N. D. (2014, Sept). A field-validated architecture for the collection of health-relevant behavioural data. Paper presented at the 2014 IEEE International Conference on Healthcare Informatics, Verona.
- Köhling, J., Moessner, M., Ehrenthal, J. C., Bauer, S., Cierpka, M., Kämmerer, A., … Dinger, U. (2016). Affective instability and reactivity in depressed patients with and without borderline pathology. Journal of Personality Disorders, 30(6), 776–795. doi:https://doi.org/10.1521/pedi_2015_29_230
- Koval, P., Pe, M. L., Meers, K., & Kuppens, P. (2013). Affect dynamics in relation to depressive symptoms: Variable, unstable or inert? Emotion (Washington, D.C.), 13(6), 1132–1141. doi:https://doi.org/10.1037/a0033579
- Links, P. S., Heisel, M. J., & Garland, A. (2003). Affective instability in personality disorders. The American Journal of Psychiatry, 160(2), 394–395. doi:https://doi.org/10.1176/appi.ajp.160.2.394-a
- Marwaha, S., He, Z., Broome, M., Singh, S. P., Scott, J., Eyden, J., & Wolke, D. (2014). How is affective instability defined and measured? A systematic review. Psychological Medicine, 44(9), 1793–1808. doi:https://doi.org/10.1017/S0033291713002407
- Massimiliano, O., Perret, L. C., Turecki, G., & Geoffroy, M.-C. (2018). Association between irritability and suicide-related outcomes across the life-course. Systematic review of both community and clinical studies. Journal of Affective Disorders, 239, 220–233. doi:https://doi.org/10.1016/j.jad.2018.07.010
- Nock, M. K. (2016). Recent and needed advances in the understanding, prediction, and prevention of suicidal behavior. Depression and Anxiety, 33(6), 460–463. doi:https://doi.org/10.1002/da.22528
- Nock, M. K., Prinstein, M. J., & Sterba, S. K. (2009). Revealing the form and function of self-injurious thoughts and behaviors: A real-time ecological assessment study among adolescents and young adults. Journal of Abnormal Psychology, 118(4), 816–827. doi:https://doi.org/10.1037/a0016948
- Oliver, M. N., & Simons, J. S. (2004). The affective lability scales: Development of a short-form measure. Personality and Individual Differences, 37(6), 1279–1288. doi:https://doi.org/10.1016/j.paid.2003.12.013
- Palmier-Claus, J., Taylor, P., Varese, F., & Pratt, D. (2012). Does unstable mood increase risk of suicide? Theory, research and practice. Journal of Affective Disorders, 143(1–3), 5–15. doi:https://doi.org/10.1016/j.jad.2012.05.030
- Peeters, F., Berkhof, J., Delespaul, P., Rottenberg, J., & Nicolson, N. A. (2006). Diurnal mood variation in major depressive disorder. Emotion (Washington, D.C.), 6(3), 383–391. doi:https://doi.org/10.1037/1528-3542.6.3.383
- Peeters, F., Nicolson, N. A., Berkhof, J., Delespaul, P., & deVries, M. (2003). Effects of daily events on mood states in major depressive disorder. Journal of Abnormal Psychology, 112(2), 203–211. doi:https://doi.org/10.1037/0021-843X.112.2.203
- Peters, E. M., Baetz, M., Marwaha, S., Balbuena, L., & Bowen, R. (2016). Affective instability and impulsivity predict nonsuicidal self-injury in the general population: A longitudinal analysis. Borderline Personality Disorder and Emotion Dysregulation, 3(1), 17. doi:https://doi.org/10.1186/s40479-016-0051-3
- Peters, E. M., Balbuena, L., Baetz, M., Marwaha, S., & Bowen, R. (2015). Mood instability underlies the relationship between impulsivity and internalizing psychopathology. Medical Hypotheses, 85(4), 447–451. doi:https://doi.org/10.1016/j.mehy.2015.06.026
- Peters, E. M., Balbuena, L., Marwaha, S., Baetz, M., & Bowen, R. (2016). Mood instability and impulsivity as trait predictors of suicidal thoughts. Psychology and Psychotherapy: Theory, Research and Practice, 89(4), 435–444. doi:https://doi.org/10.1111/papt.12088
- Peters, E. M., John, A., Bowen, R., Baetz, M., & Balbuena, L. (2018). Neuroticism and suicide in a general population cohort: Results from the UK Biobank Project. BJPsych Open, 4(2), 62–68. doi:https://doi.org/10.1192/bjo.2017.12
- Peters, J. R., Mereish, E. H., Solomon, J. B., Spirito, A. S., & Yen, S. (2019). Suicide ideation in adolescents following inpatient hospitalization: Examination of intensity and lability over 6 months. Suicide & Life-Threatening Behavior, 49(2), 572–585. doi:https://doi.org/10.1111/sltb.12448
- Santangelo, P., Reinhard, I., Mussgay, L., Steil, R., Sawitzki, G., Klein, C., … Ebner-Priemer, U. W. (2014). Specificity of affective instability in patients with borderline personality disorder compared to posttraumatic stress disorder, bulimia nervosa, and healthy controls. Journal of Abnormal Psychology, 123(1), 258–272. doi:https://doi.org/10.1037/a0035619
- Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., … Dunbar, G. C. (1998). The mini-international neuropsychiatric interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry, 59(Suppl. 20), 2022–2033.
- Solhan, M. B., Trull, T. J., Jahng, S., & Wood, P. K. (2009). Clinical assessment of affective instability: Comparing EMA indices, questionnaire reports, and retrospective recall. Psychological Assessment, 21(3), 425–436. doi:https://doi.org/10.1037/a0016869
- Solmi, M., Zaninotto, L., Toffanin, T., Veronese, N., Lin, K., Stubbs, B., … Correll, C. U. (2016). A comparative meta-analysis of TEMPS scores across mood disorder patients, their first-degree relatives, healthy controls, and other psychiatric disorders. Journal of Affective Disorders, 196, 32–46. doi:https://doi.org/10.1016/j.jad.2016.02.013
- Stange, J. P., Sylvia, L. G., da Silva Magalhães, P. V., Miklowitz, D. J., Otto, M. W., Frank, E., … Deckersbach, T. (2016). Affective instability and the course of bipolar depression: Results from the STEP-BD randomised controlled trial of psychosocial treatment. The British Journal of Psychiatry: The Journal of Mental Science, 208(4), 352–358. doi:https://doi.org/10.1192/bjp.bp.114.162073
- Stekhoven, D. J., & Bühlmann, P. (2012). MissForest—non-parametric missing value imputation for mixed-type data. Bioinformatics (Oxford, England), 28(1), 112–118. doi:https://doi.org/10.1093/bioinformatics/btr597
- Thompson, R. J., Berenbaum, H., & Bredemeier, K. (2011). Cross-sectional and longitudinal relations between affective instability and depression. Journal of Affective Disorders, 130(1–2), 53–59. doi:https://doi.org/10.1016/j.jad.2010.09.021
- Thompson, R. J., Mata, J., Jaeggi, S. M., Buschkuehl, M., Jonides, J., & Gotlib, I. H. (2012). The everyday emotional experience of adults with major depressive disorder: Examining emotional instability, inertia, and reactivity. Journal of Abnormal Psychology, 121(4), 819–829. doi:https://doi.org/10.1037/a0027978
- Van Orden, K. A., Witte, T. K., Cukrowicz, K. C., Braithwaite, S. R., Selby, E. A., & Joiner, T. E. Jr, (2010). The interpersonal theory of suicide. Psychological Review, 117(2), 575–600. doi:https://doi.org/10.1037/a0018697
- Verdolini, N., Menculini, G., Perugi, G., Murru, A., Samalin, L., Angst, J., … Pacchiarotti, I. (2019). Sultans of swing: A reappraisal of the intertwined association between affective lability and mood reactivity in a post hoc analysis of the BRIDGE-II-MIX study. The Journal of Clinical Psychiatry, 80(2), 17m12082. doi:https://doi.org/10.4088/JCP.17m12082
- von Neumann, J., Kent, R. H., Bellinson, H. R., & Hart, B. I. (1941). The mean square successive difference. The Annals of Mathematical Statistics, 12(2), 153–162. doi:https://doi.org/10.1214/aoms/1177731746
- Wichers, M., Peeters, F., Geschwind, N., Jacobs, N., Simons, C. J. P., Derom, C., … van Os, J. (2010). Unveiling patterns of affective responses in daily life may improve outcome prediction in depression: A momentary assessment study. Journal of Affective Disorders, 124(1–2), 191–195. doi:https://doi.org/10.1016/j.jad.2009.11.010
- Witte, T. K., Fitzpatrick, K. K., Joiner, T. E., & Schmidt, N. B. (2005). Variability in suicidal ideation: A better predictor of suicide attempts than intensity or duration of ideation? Journal of Affective Disorders, 88(2), 131–136. doi:https://doi.org/10.1016/j.jad.2005.05.019
- Witte, T. K., Fitzpatrick, K. K., Warren, K. L., Schatschneider, C., & Schmidt, N. B. (2006). Naturalistic evaluation of suicidal ideation: Variability and relation to attempt status. Behaviour Research and Therapy, 44(7), 1029–1040. doi:https://doi.org/10.1016/j.brat.2005.08.004