Abstract
Introduction
The aim was to investigate psychiatric health care utilization two years before death by suicide among individuals with previous suicide attempts (PSA) compared with those without (NSA).
Method
A retrospective population-based cohort study was conducted including 484 individuals who died by suicide in Sweden in 2015 and were in contact with psychiatric services within the two years preceding death, identified through the Cause of Death register. Data on psychiatric health care two years before death, including suicide attempts according to notes in the medical record was used. Associations between having at least one PSA vs. NSA and health care utilization were estimated as odds ratios (OR) with 95% confidence intervals (CI) by logistic regression analyses.
Results
Of the 484 individuals included, 51% had PSA. Those with PSA were more likely than NSA to have received a psychiatric diagnosis [OR 1.96 (CI 95% 1.17–3.30)], to have ongoing psychotropic medication [OR 1.96 (CI 95% 1.15–3.36)] and to have been absent from appointments during the last three months [1.97 (1.25–3.13)]. In addition, elevated suicide risk was more often noted in the psychiatric case records of those with a PSA than those without [OR 2.17 (CI 95% 1.24–3.79)].
Conclusion
The results underline the importance of improved suicide risk assessment as well as thorough diagnostic assessment and when indicated, psychiatric treatment as suicide preventive interventions regardless of PSA. Furthermore, the larger proportion of absence from appointments in individuals with PSA may indicate a need of improved alliance between psychiatric care providers and individuals with PSA.
Being assessed with elevated suicide risk was more common among those with previous attempt/s (PSA).
One-fifth of all with no previous attempt (NSA) had no psychiatric diagnosis, compared to one in ten in those with PSA.
Receiving psychotropic medication was more common among those with PSA.
HIGHLIGHTS
INTRODUCTION
Suicide is a multifaceted problem and efforts are needed in many different domains in society, including a need for effective health and medical care strategies to reduce deaths by suicide (Stanley & Mann, Citation2020). People who die by suicide have often sought health care in close proximity to death (Ahmedani et al., Citation2014; Luoma, Martin, & Pearson, Citation2002). For example, a recent systematic review of contact with primary and mental health care before suicide in men and women and across a range of age categories (Stene-Larsen & Reneflot, Citation2019) showed that 35% had been in contact with mental health services during the 3 months preceding death. Suicide is strongly associated with mental disorders (Harris & Barraclough, Citation1997). Studies have repeatedly shown that ∼90% of all individuals who died by suicide in western countries had a mental disorder at the time of death (Cavanagh, Carson, Sharpe, & Lawrie, Citation2003; Nock et al., Citation2008). This indicates that to improve prevention efforts, specific attention to mental health issues is warranted. A recent Australian study (Wyder et al., Citation2021) investigated suicide victims who had been in contact with psychiatric services before death. They found that 70% had been formally assessed regarding suicide risk within a month before death but none of them had been assessed as being at high risk of suicide. Psychiatric services constitute an important domain for improved suicide risk assessment and suicide prevention measures.
Although a previous suicide attempt is a well-documented risk factor (Bostwick, Pabbati, Geske, & McKean, Citation2016), as many as 60% of people who die by suicide die on their first attempt (Bostwick et al., Citation2016). A lack of knowledge about these individuals has been identified (Buchman-Schmitt et al., Citation2017; Jordan & McNiel, Citation2020), even though they make up a significant proportion of all individuals who die by suicide. The few studies that exist indicate that they are, to a greater extent, men (Isometsä & Lönnqvist, Citation1998; Yook et al., Citation2021), who are older (Blow, Brockmann, & Barry, Citation2004; Yook et al., Citation2021) and are less often diagnosed with a psychiatric disorder (Yook et al., Citation2021) and have used firearms as suicide method (Anestis, Citation2016; Bostwick et al., Citation2016; Jamison & Bol, Citation2016). Furthermore, compared to people with previous suicide attempts, they seem to have experienced fewer stressful life events before death (Buchman-Schmitt et al., Citation2017). A recent Korean study (Yook et al., Citation2021) compared individuals who died by suicide with and without previous suicide attempts. They found that individuals with previous attempts were more likely to have talked about suicide and death before death by suicide, while those with no previous attempt were reported to have been troubled by relationship problems and somatic complaints. The knowledge of psychiatric care utilization before suicide regarding individuals with and without previous suicide attempts specifically is scarce. To the best of our knowledge, no previous studies have been conducted comparing these two groups in the context of psychiatric health care services.
Aims and Research Questions
The aim was to compare psychiatric health care utilization two years before suicide among individuals with and without previous suicide attempts. Specific areas of focus include the length of psychiatric contact and proximity of contact before suicide, suicide risk assessment, ongoing and planned treatment interventions, and individual factors, such as gender, age, type of psychiatric diagnosis, and comorbidity. The study includes 484 individuals who died by suicide in Sweden in 2015 and had been in contact with psychiatric services within the two years preceding death.
METHOD AND MATERIAL
The present study was carried out within the ongoing nationwide research project titled Retrospective investigation of health care utilization of individuals who died by suicide in Sweden 2015. The project analyses the patterns of health care utilization and includes data for 20 of Sweden’s 21 regions (Stockholm data not currently available). Data were retrieved from the Cause of Death Register (The National Board of Health & Welfare, Citation2021). Suicide was recorded in the CDR as the underlying cause of death according to the International Statistical Classification of Diseases and Related Health Problems (ICD, version 10) (World Health Organization, Citation1992) as suicide (ICD 10: X60–X84).
Medical Record Protocol
Medical records from psychiatric health care services were investigated using a structured protocol developed for this purpose. The research group developed a protocol following the recommendations of the Swedish Psychiatric Organization (Salander Renberg & Swedish Psychiatric Association, Citation2013), including questions regarding a range of aspects connected to health care utilization. Records from private psychiatric health care services were also included. In some cases, information could be retrieved from any of the medical records, i.e., also including primary care and somatic care. Data regarding previous suicide attempts were collected from any available medical record information within two years. All visits at psychiatric service units were taken into consideration; outpatient clinics, inpatient wards, psychiatric emergency visits, psychiatric consultations, mobile team visits, private psychiatric care. Data of visits/contacts to all professions were collected including psychiatrist, psychologist, social worker, nurse, physiotherapist, and assistant nurse.
Medical Records Reviewers
Regional health care representatives signed patient confidentiality documents with the research group project leader, agreeing to adhere to the Swedish law of patient confidentialityFootnote1 when handling the research data. They were then given access to data on the individuals residing in their geographic region who died by suicide. The regional representatives made agreements with local investigators who also signed a confidentiality statement with the local representative and thus were assigned to the research project. Access to medical records was granted regionally. Investigators around the country were all invited to a day of training to use the investigation protocol. Members of the research group provided the training, which was offered on repeated occasions as new investigators were included. A written guide was created to further assist investigators in data collection. After the training, the investigators had access to continuous support and updates by the research group.
Investigators were primarily clinicians with experience in using the region’s electronic record system. If an investigator came across an individual they had met as a clinician, that case was investigated by someone else to maintain objectivity. All data analyzed in this study were collected from medical records and were entered into excel files.
Included Variables
Based on medical record data for the two years before the suicide, a person with one or more notations of a suicide attempt at any point during lifetime was considered to have a previous attempt. A binary dependent variable was created (previous attempt (PSA)/no previous attempt (NSA). The presence of previous suicide attempts was assessed according to notes of any lifetime attempts in the medical records.
Independent variables included: Gender was categorized as men and women. Age at time of suicide was categorized as ≤19, 20–29, 30–39, 40–49, 50–59, 60–69, ≥70. Psychiatric diagnoses refer to a diagnosis noted in the medical record at the last contact with psychiatric health care services, as ICD-10 codes in chapter F using three digits (e.g., F32.1) (World Health Organization, Citation1992). Comorbidity refers to two or more psychiatric diagnoses (any) noted in the medical record at the last contact with psychiatric health care services. The number of days between the last contact with psychiatric services and the suicide (“proximity of psychiatric care”) was transformed into a categorical variable (one week, one-four weeks, over four weeks up to three months, over three months up to one year, more than one year). The total length of the psychiatric treatment was coded as the number of days between the first psychiatric health care contact and the suicide. If the contact exceeded two years, it was assigned a maximum of 730 days. The continuous variable was transformed into a categorical variable (up to three months, three months up to one year, one year up to two years, or two years or more). Psychiatric treatment includes interventions, such as pharmacological treatment, psychotherapy (any method, offered by a therapist with at least basic psychotherapy training), counseling (supportive talk therapy, without specific training), physiotherapy, electroconvulsive therapy (ECT), and daycare treatment. All interventions were analyzed as ongoing yes/no or planned yes/no. Community psychiatry refers to support offered by social services, typically including supportive interventions in the home environment. Assessments of suicide risk refer to whether suicide risk was assessed within four weeks before death (yes/no) and whether suicide risk was assessed as elevated at the last visit to a psychiatrist (yes/no).
Statistical Analysis
Frequency distributions with the chi-square test were calculated. Associations between suicide with previous suicide attempts (PSA) vs. without (NSA) and independent variables were estimated by crude and adjusted OR with 95% CI using logistic regressions. The results are presented as crude and adjusted odds ratios (ORs) and 95% confidence intervals (95% CIs). As a first step, ORs with 95% CIs were estimated for each independent variable. As a second step, ORs were adjusted for gender and age. In the final regression models, all included variables were adjusted for gender, age, all psychiatric diagnoses, and any psychiatric comorbidity, in turn, thereby adjusting also for the effect of psychiatric diagnosis on the clinical variables. Results were considered statistically significant when p < .05. Statistical assumptions of the regression model: All variables were tested for possible collinearity. All analyses were performed by SPSS version 25 (20).
Ethical Considerations
According to the Swedish Act Concerning the Ethical Review of Research Involving Humans (2003:460) and an advisory opinion from the Regional Ethical Review Board (no. 2017/234), this study was exempt from ethical review as it did not include living human participants.
RESULTS
Sample Description
All 484 individuals were included who were in contact with psychiatric health care services during their last two years of life, representing 51% of all suicides in the 20-county catchment area. As can be seen in , among those, 65% (n = 316) were men and 35% (n = 168) were women and age ranged from 13 to 94 years, mean 47 years (SD 17), median 48 years (SD 17).
TABLE 1. Characteristics of individuals in contact with psychiatric services who died by suicide (n = 484), crude and adjusted odds ratio (OR) with 95% confidence interval (95% CI) for the association between gender, age, type of diagnosis, and having at least one known previous attempt/s (PSA) vs. without previous attempt/s (NSA).
Gender, Age, Psychiatric Diagnosis, and Comorbidity
Almost two-thirds of the women who were in contact with psychiatric services and who died by suicide had at least one previous suicide attempt (PSA) compared to 44% of the men. Bivariable associations revealed that women, those with psychiatric diagnoses (any), those with psychiatric comorbidity (any), those with a mood disorder, bipolar affective disorder, personality disorder had higher ORs of having at least one suicide attempt (PSA) compared to those with NSA.
Age differences between PSA and NSA were found, as presented in . Three-quarters of those who died by suicide before the age of 20 died at their first known attempt. Those who died at their first attempt in this age group were equally distributed between genders.
Being diagnosed with any psychiatric disorder was more common in individuals with PSA than in those with NSA. Of the 22% of individuals with NSA that did not have a psychiatric diagnosis, 24% had been in contact with psychiatry for two years (or more), 24% between one-two years, 21% between three months and a year, and 32% for three months or less. Comorbidity was high in both groups but significantly higher in individuals with PSA than in those without. A comparison between psychiatric diagnoses in individuals with PSA and NSA is presented in . Only diagnoses with statistically significant differences (in the crude model) between individuals with PSA and NSA are presented in . Except for schizophrenia, all diagnoses were more common in PSA compared to NSA. Among the individuals diagnosed with schizophrenia (n = 16), half had been assessed regarding suicide risk within four weeks before death, suicide risk was rated as elevated in none. Diagnoses without significant differences include substance use disorders, anxiety, and stress disorders, eating disorders, and attention deficit disorders.
The Length and Proximity of Contact
As shown in , the duration of contact with psychiatric services was longer in individuals with PSA compared to those with NSA. Of all the individuals in contact with psychiatry within a week of the suicide, individuals with PSA represented more than half. Of all individuals with PSA, 41% had been in contact with psychiatric services within a week and the corresponding proportion in NSA was 33%. As opposed to individuals with PSA, individuals with NSA were more likely to have been in contact with psychiatric health care services within a year. Results were slightly attenuated when adjusted for gender, age, and comorbidity, but associations remained significant. As seen in the OR of being absent from appointments during the final three months of life was twice as high in individuals with PSA than in those with NSA, a result that remained significant after controlling for age, gender, and comorbidity. Of all individuals with PSA, 28% were absent from at least one appointment during the last three months.
TABLE 2. Individuals in contact with psychiatric services who died by suicide (n = 484), crude and adjusted odds ratio (OR) with 95% confidence interval (95% CI) for the association between length and proximity of psychiatric contact, absence from appointment, and having at least one known previous attempt/s (PSA) vs. without previous attempt/s (NSA).
Suicide Risk Assessment
as well as show an association between elevated suicide risk assessed at the last visit to a psychiatrist and having PSA in crude and adjusted models. After adjusting for gender, age and comorbidity, no difference was found between individuals with and without PSA regarding whether or not suicide risk had been assessed within the four weeks before suicide.
FIGURE 1. Proportions (%) with ongoing and planned psychiatric interventions and suicide risk assessment among patients who died by suicide, by suicide attempt history (n = 238).
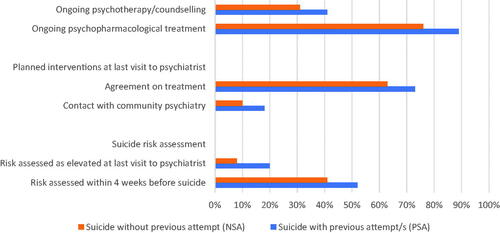
TABLE 3. Crude and adjusted odds ratio (OR) with 95% confidence interval (95% CI) for associations between the ongoing and planned psychiatric interventions, suicide risk assessment, and having at least one known previous attempt/s (PSA) vs. without previous attempt/s (NSA).
Ongoing and Planned Treatment Interventions
As presented in and , ongoing pharmacological treatment, psychological treatments as well as planned contact with social services were more common in those with PSA. These results remained significant for pharmacological treatment after adjustment for gender, age, comorbidity, and psychological treatment. The association of psychopharmacological and psychological treatment with having PSA was also controlled for each of the diagnoses, but the effect was negligible. Regarding all other treatment variables noted as ongoing at the time of death, no differences were found.
DISCUSSION
This study showed that the patterns of psychiatric health care utilization before suicide differed significantly between individuals with PSA and those with NSA. The results indicate that individuals with PSA had a longer duration of health care utilization. Further, they were more often assessed with elevated suicide risk. Individuals having PSA also had significant associations with psychotropic medication and planned interventions and a larger proportion of care contacts close to suicide, compared to patients with NSA.
The result that half of the study population had previous suicide attempts was in line with Bostwick et al. (Citation2016) reporting that 60% of individuals who die by suicide die at their first attempt. The finding that individuals with PSA compared to those with NSA more often had ongoing psychotropic medication and planned interventions indicate an independent association between having a history of suicide attempt/s and treatment and planning of interventions. The planned support offered by social services points at the clinicians having detected a wider range of needs than what could be met in the health care system.
Over 40% of the individuals with PSA, had been in contact with psychiatric services within one week before death. This can be compared to the 33% of individuals with NSA. Schaeffer et al. reported an overall percentage of contact with psychiatric services within a week before the suicide of 22% (Schaffer et al., Citation2016), but no comparison depending on previous suicide attempts was made. Further, being absent from appointments during the last three months before suicide was more common among individuals with PSA, 28% of individuals with PSA, and 16% of those with NSA. It is not known what strategies, if any, were used to reach the patient when they missed an appointment and what role this aspect might play in the trajectory of prevention efforts.
Individuals with PSA were more likely to be assessed with elevated suicide risk than those with NSA. Since previous suicide attempts are a well-known risk factor, this may point to suicide risk being more easily detected since the presence of earlier attempts can be weighed into the assessment. Yook et al. (Citation2021) found that, as opposed to those with NSA, individuals with PSA are more likely to have talked about suicide and death, a factor that might help to explain the differences found in this study. For some of the individuals, the last contact with psychiatric services before death may have been in connection with a suicide attempt, though this was not analyzed specifically in this study.
Although the suicide risk was assessed in many cases and some were in contact with psychiatric services just days before death, suicide was not prevented in the individuals in this study. A suicide risk assessment is, by nature, a very challenging task for clinicians, just as the prediction of any human behavior. Risk factors on the group level do not necessarily apply to a specific individual, as the suicide risk level is a complex combination of contributing factors and varies over time. A problematic finding is that although the study analyzes psychiatric health care services, suicide risk was not always assessed—or at least was not always recorded in the medical chart. This indicates a possible area of improvement in psychiatric services in Sweden.
The majority of the women who died by suicide had at least one previous attempt while the majority of the men died at their first attempt, confirming the results of previous research (Isometsä & Lönnqvist, Citation1998; Kodaka et al., Citation2017; Yook et al., Citation2021). The first attempt was fatal in three-quarters of those in the youngest age band, a proportion similar to that reported by Gagnon et al. who investigated suicides in teens and young adults (Gagnon, Davidson, Cheifetz, Martineau, & Beauchamp, Citation2009). Cho et al. (Citation2013), investigating age differences in health care utilization before suicide, stated that community-based prevention strategies may be necessary to prevent suicide in adolescents with psychiatric disorders as they may not seek the help they need in the health care system. However, the high proportion of the youngest individuals in this study who died in connection with their first suicide attempt can reflect the fact that the older a person gets, the more likely it is that previous suicide attempts have occurred.
Being diagnosed with a psychiatric disorder (any) and psychiatric comorbidity (any) was more common in individuals with PSA than in those with NSA. The finding regarding psychiatric disorders confirms the results of a recent Korean study (Yook et al., Citation2021). Further, each individual psychiatric diagnosis was more common among individuals with PSA than those with NSA—except for schizophrenia. This finding raises important questions as to whether individuals with NSA are an underdiagnosed group, which in turn could have an impact on receiving the correct treatment as well as the overall prognoses. The difference may reflect that individuals with PSA as a group were in longer contact with psychiatric health care services, allowing a more thorough psychiatric assessment over time. It could also be explained by an effort to assess diagnosis after a suicide attempt. Personality disorder and bipolar disorder were markedly associated with individuals with PSA, paralleling the results of previous research (Benjamin et al., Citation2003; Christiansen & Jensen, Citation2007; Irigoyen et al., Citation2019; Isabel et al., Citation2017).
Three-quarters of the study population with a diagnosis of schizophrenia died on their first known suicide attempt. While suicide risk had been evaluated during the final month of life in half of the cases, none of the individuals with schizophrenia were assessed with elevated risk. Large and Ryan argue that since suicide mortality is 20–75 times higher in individuals with schizophrenia compared to the general population, all individuals with schizophrenia should be considered at risk of death by suicide and be targets of treatment efforts suited to the individual (Large & Ryan, Citation2014).
It is important to note that the current study focuses on individuals who had been in contact with psychiatric services. The portion of for example individuals with psychiatric disorders and psychiatric treatment must be interpreted in light of this. The results can therefore not be generalized to all individuals who die by suicide.
Strengths and Limitations
The present study has several strengths. It provides detailed data on the type of contacts, treatment, interventions as well as the duration of the provided psychiatric health care, something that is rare in the previous literature in the field. Further, the study population is large enough to allow for multivariate analyses and includes almost an entire nation.
The study relies exclusively on the information noted in medical records. It is possible that there were cases of previous suicide attempts that were not included in the chart, and these individuals would in such cases be incorrectly classified as having no previous suicide attempt/s (NSA). This would mean an underestimation of the number of PSA and an overestimation of NSA. Further, this study did not include information from any of the national registers. Doing so would have yielded more information that would have added to the analysis in several of the investigated areas.
As all subjects in this study died by suicide, no analyses of health care utilization effect on suicide as the outcome could be performed. The current study did not include a control group of individuals in contact with psychiatric services who are still alive, with or without previous suicide attempts, to allow for such an analysis.
Data from medical records were collected by numerous investigators and there was no testing of inter-rater reliability (IRR). Some of the questions in the protocol involve a level of assessment by the investigator, among them the categorization of PSA/NSA. The lack of inter-rater reliability testing could reduce the validity of the data. One aspect hindering IRR testing was that the investigators came from different parts of the country. Due to the confidentiality law, medical records could only be assessed within one region. Efforts to make sure investigators uniformly collected data included group training, investigator guidelines, and a high level of support from the research group. Another issue is that there were regional differences in the organization of psychiatric services which made the protocol more challenging to use in some regions. Information could have been omitted as a result.
This study may not have gained access to data from psychiatric medical records of all private health care facilities. In Sweden, private healthcare represents about 19% of all psychiatric health care services nationwide, though with large regional differences (Vårdföretagarna, Citation2020). In the medical chart systems investigated in this study, private health care is not always automatically recorded and for this reason, data on some psychiatric health care may have been omitted. In cases where information on private care was available in regional registers or medical records, efforts were made to obtain the medical records from the private clinic. The amount of missing data due to the lack of private care records is not known. Further, any psychiatric disorder diagnosed in primary care settings would be omitted since this study only investigated records in psychiatric service settings.
Suicide risk, when assessed, was coded in the study protocol as a dichotomous variable (elevated yes/no). In a clinical setting, a more nuanced grading is usually employed. For this reason, levels of complexity may have been lost to the coding.
The wide confidence intervals seen in in the crude and adjusted model regarding personality disorder suggest that there may be a power problem. The result, for this reason, should be interpreted with caution.
Conclusions
Suicide risk in the group of individuals with PSA was more often detected, they more often had a diagnosed psychiatric disorder and they were in pharmacological treatment more often than individuals with NSA. Still, suicide in these cases was not prevented, indicating a need for access to efficient treatment interventions. The larger proportion of absence from appointments in individuals with PSA may indicate a need for an improved alliance between psychiatric care providers and individuals with PSA. In individuals with NSA, suicide risk was less often detected, they were less often diagnosed with a psychiatric disorder and in pharmacological treatment compared with individuals with PSA. Improved suicide risk assessment strategies, as well as diagnostic assessment and psychiatric treatment, are important regardless of previous suicide attempts.
Implications for Future Research
The finding that individuals with PSA to a higher degree receive pharmacological treatment, even when adjusting for diagnosis, raises several questions. Could this be an expression of clinicians detecting a higher severity in these patients because of the earlier attempt/s and therefore a higher inclination to offer pharmacological treatment? Or is the difference better explained by individuals with PSA generally having been in contact with psychiatric health care services for a longer time and clinicians, therefore, had time to assess the need for pharmacological treatment? These questions remain unanswered and need further investigation in future research.
Being absent from appointments during the last three months before suicide was more common among individuals with PSA than among those with NSA. This study did not analyze if any strategies were used to reach a patient when they missed an appointment. It would be an interesting focus of future studies to investigate this and in light of suicide prevention efforts.
In future research, the findings of this study would benefit from being tested against a control group of individuals with contact with psychiatric health care services but who did not die by suicide. Further, this study investigated the Swedish health care system, and future research might investigate if the results are similar in other contexts.
AUTHOR NOTES
ÅW is the principal investigator, initiated and designed the study, and acquired the data. ÅW, EF, AE, and NPÖ developed the protocol that was used to extract medical record data. SPL, EF, EB, NPÖ, and TS collected data, and SPL, EB, and NPÖ trained other investigators to collect data. SPL and MV designed the statistical strategy. SPL, MV, EF, MW, and ÅW contributed to the presentation of data in the tables. ÅW, SPL, MV, MW, EF, LA, AE, and TS contributed to designing the study and interpretation of the data. SPL drafted the manuscript and made the statistical analysis. ÅW, MW, MV, LA, AE, EF, TS, EB, and NPÖ revised the manuscript. All authors read and approved the final manuscript.
ACKNOWLEDGMENTS
The authors are grateful to all regional representatives of Sweden and investigators who participated in data collection, to the Swedish suicide prevention network and health care management network in Sweden who encouraged all regions to join the study, and to Catharina Nygren, research administrator, Region Skåne, who aided in the implementation of this study.
DISCLOSURE STATEMENT
The authors declare no conflict of interest.
DATA AVAILABILITY STATEMENT
Data are available upon reasonable request.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
Notes on contributors
Sara Probert-Lindström
Sara Probert-Lindström, Livia Ambrus, MD, PhD, Erik Bergqvist, MD, Nina Palmqvist-Öberg, MD, and Åsa Westrin, MD, PhD, Lund University, Lund, Sweden.
Marjan Vaez
Marjan Vaez, Division of Insurance Medicine, Department of Clinical Neuroscience, Karolinska Institute, Stockholm, Sweden.
Elin Fröding
Elin Fröding, MD, Jönköping University, Jönköping, Sweden.
Anna Ehnvall
Anna Ehnvall, MD, PhD, and Margda Waern, MD, PhD, University of Gothenburg, Gothenburg, Sweden.
Tabita Sellin
Tabita Sellin, PhD, University Health Care Research Center, Örebro University, Örebro, Sweden.
Livia Ambrus
Sara Probert-Lindström, Livia Ambrus, MD, PhD, Erik Bergqvist, MD, Nina Palmqvist-Öberg, MD, and Åsa Westrin, MD, PhD, Lund University, Lund, Sweden.
Erik Bergqvist
Sara Probert-Lindström, Livia Ambrus, MD, PhD, Erik Bergqvist, MD, Nina Palmqvist-Öberg, MD, and Åsa Westrin, MD, PhD, Lund University, Lund, Sweden.
Nina Palmqvist-Öberg
Sara Probert-Lindström, Livia Ambrus, MD, PhD, Erik Bergqvist, MD, Nina Palmqvist-Öberg, MD, and Åsa Westrin, MD, PhD, Lund University, Lund, Sweden.
Margda Waern
Anna Ehnvall, MD, PhD, and Margda Waern, MD, PhD, University of Gothenburg, Gothenburg, Sweden.
Åsa Westrin
Sara Probert-Lindström, Livia Ambrus, MD, PhD, Erik Bergqvist, MD, Nina Palmqvist-Öberg, MD, and Åsa Westrin, MD, PhD, Lund University, Lund, Sweden.
Notes
1 Swedish law of public access to information and secrecy, SFS 2009:400 C.F.R.
REFERENCES
- Ahmedani, B. K., Simon, G. E., Stewart, C., Beck, A., Waitzfelder, B. E., Rossom, R., … Solberg, L. I. (2014). Health care contacts in the year before suicide death. Journal of General Internal Medicine, 29(6), 870–877. doi:10.1007/s11606-014-2767-3
- Anestis, M. D. (2016). Prior suicide attempts are less common in suicide decedents who died by firearms relative to those who died by other means. Journal of Affective Disorders, 189, 106–109. doi:10.1016/j.jad.2015.09.007
- Benjamin, H. M., Joseph, F. G., Tara, M. S., Jessica, L. G., Carrie, L. E., & Glen, P. D. (2003). Characteristics of first suicide attempts in single versus multiple suicide attempters with bipolar disorder. Comprehensive Psychiatry, 44(1), 15–20. doi:10.1053/comp.2003.50004
- Blow, F. C., Brockmann, L. M., & Barry, K. L. (2004). Role of alcohol in late-life suicide. Alcoholism, Clinical and Experimental Research, 28(5 Suppl), 48S–56S. doi:10.1097/01.alc.0000127414.15000.83
- Bostwick, J. M., Pabbati, C., Geske, J. R., & McKean, A. J. (2016). Suicide attempt as a risk factor for completed suicide: Even more lethal than we knew. American Journal of Psychiatry, 173(11), 1094–1100. doi:10.1176/appi.ajp.2016.15070854
- Buchman-Schmitt, J. M., Chu, C., Michaels, M. S., Hames, J. L., Silva, C., Hagan, C. R., … Joiner, T. E. (2017). The role of stressful life events preceding death by suicide: Evidence from two samples of suicide decedents. Psychiatry Research, 256, 345–352. doi:10.1016/j.psychres.2017.06.078
- Cavanagh, J. T., Carson, A. J., Sharpe, M., & Lawrie, S. M. (2003). Psychological autopsy studies of suicide: A systematic review. Psychological Medicine, 33(3), 395–405. doi:10.1017/s0033291702006943
- Cho, J., Kang, D. R., Moon, K. T., Suh, M., Ha, K. H., Kim, C., … Jung, S. H. (2013). Age and gender differences in medical care utilization prior to suicide. Journal of Affective Disorders, 146(2), 181–188. doi:10.1016/j.jad.2012.09.001
- Christiansen, E., & Jensen, B. F. (2007). Risk of repetition of suicide attempt, suicide or all deaths after an episode of attempted suicide: A register-based survival analysis. The Australian and New Zealand Journal of Psychiatry, 41(3), 257–265. doi:10.1080/00048670601172749
- Gagnon, A., Davidson, S., Cheifetz, P., Martineau, M., & Beauchamp, G. (2009). Youth suicide: A psychological autopsy study of completers and controls. Vulnerable Children and Youth Studies, 4(1), 13–22. doi:10.1080/17450120802270400
- Harris, E. C., & Barraclough, B. (1997). Suicide as an outcome for mental disorders. A meta-analysis. British Journal of Psychiatry, 170(3), 205–228. doi:10.1192/bjp.170.3.205
- Irigoyen, M., Segovia, A. P., Galván, L., Puigdevall, M., Giner, L., De Leon, S., … Porras-Segovia, A. (2019). Predictors of re-attempt in a cohort of suicide attempters: A survival analysis. Journal of Affective Disorders, 247, 20–28. doi:10.1016/j.jad.2018.12.050
- Isabel, P.-U., Hilario, B.-F., Gemma, G.-P., Luis, M.-N., Oliver, V.-C., Annabel, C.-M., … Diego, P.-V. (2017). Risk of re-attempts and suicide death after a suicide attempt: A survival analysis. BMC Psychiatry, 17(1), 1–11. doi:10.1186/s12888-017-1317-z
- Isometsä, E. T., & Lönnqvist, J. K. (1998). Suicide attempts preceding completed suicide. British Journal of Psychiatry, 173(6), 531–535. doi:10.1192/bjp.173.6.531
- Jamison, E. C., & Bol, K. A. (2016). Previous suicide attempt and its association with method used in a suicide death. American Journal of Preventive Medicine, 51(5), S226–S233. doi:10.1016/j.amepre.2016.07.023
- Jordan, J. T., & McNiel, D. E. (2020). Characteristics of persons who die on their first suicide attempt: Results from the National Violent Death Reporting System. Psychological Medicine, 50(8), 1390–1397. doi:10.1017/S0033291719001375
- Kodaka, M., Matsumoto, T., Yamauchi, T., Takai, M., Shirakawa, N., & Takeshima, T. (2017). Female suicides: Psychosocial and psychiatric characteristics identified by a psychological autopsy study in Japan. Psychiatry and Clinical Neurosciences, 71(4), 271–279. doi:10.1111/pcn.12498
- Large, M. M., & Ryan, C. J. (2014). ‘Heed not the oracle’: Risk assessment has no role in preventing suicide in schizophrenia. Acta Psychiatrica Scandinavica, 130(6), 415–417. doi:10.1111/acps.12333
- Luoma, J. B., Martin, C. E., & Pearson, J. L. (2002). Contact with mental health and primary care providers before suicide: A review of the evidence. The American Journal of Psychiatry, 159(6), 909–916. doi:10.1176/appi.ajp.159.6.909
- Nock, M. K., Borges, G., Bromet, E. J., Cha, C. B., Kessler, R. C., & Lee, S. (2008). Suicide and suicidal behavior. Epidemiologic Reviews, 30, 133–154. doi:10.1093/epirev/mxn002
- Salander Renberg, E., & Swedish Psychiatric Association (2013). Suicidnära patienter: Kliniska riktlinjer för utredning och vård [Suicidal patients: Clinical guidelines for assessment and care] (1. uppl. ed.). Gothia Fortbildning: Swedish Psychiatric Association.
- Schaffer, A., Sinyor, M., Kurdyak, P., Vigod, S., Sareen, J., Reis, C., … Cheung, A. (2016). Population-based analysis of health care contacts among suicide decedents: Identifying opportunities for more targeted suicide prevention strategies. World Psychiatry, 15(2), 135–145. doi:10.1002/wps.20321
- Stanley, B., & Mann, J. J. (2020). The need for innovation in health care systems to improve suicide prevention. JAMA Psychiatry, 77(1), 96–98. doi:10.1001/jamapsychiatry.2019.2769
- Stene-Larsen, K., & Reneflot, A. (2019). Contact with primary and mental health care prior to suicide: A systematic review of the literature from 2000 to 2017. Scandinavian Journal of Public Health, 47(1), 9–17. doi:10.1177/1403494817746274
- The National Board of Health and Welfare (2021). Statistikdatabas för dödsorsaker [Statistical databease, c. o. d. Cause of death register]. Retrieved Jan 28, 2021, from https://sdb.socialstyrelsen.se/if_dor/resultat.aspx
- Vårdföretagarna (2020). Care entrepreneurs. Retrieved from https://www.vardforetagarna.se/vardfakta/sjukvard/sektion/patientbesok
- World Health Organization (1992). International statistical classification of diseases and related health problems: ICD-10 (10. rev. ed.). World Health Organization. [cited 2021 Nov 18]. Available from: https://search.ebscohost.com/login.aspx?direct=true&db=cat07147a&AN=lub.870593&site=eds-live&scope=site
- Wyder, M., Ray, M. K., Russell, S., Kinsella, K., Crompton, D., & van den Akker, J. (2021). Suicide risk assessment in a large public mental health service: Do suicide risk classifications identify those at risk? Australasian Psychiatry, 39(3), 322–325. doi:10.1177/1039856220984032
- Yook, V., Kim, H., Kim, E. J., Kim, Y., Lee, G., Choi, J. H., & Jeon, H. J. (2021). Psychological autopsy study comparing suicide decedents with and without a history of suicide attempts in a nationwide sample of South Korea. Suicide and Life-Threatening Behavior, 00, 1–9. doi:10.1111/sltb.12750
