Abstract
Objective
Client suicide, used to refer to situations where a mental health practitioner (MHP) is exposed, affected, or bereaved by a client’s suicide, is known to have a profound impact on MHPs. The current study investigated (1) the short- and long-term impact of client suicide and (2) to what extent gender, years of experience, therapeutic background, and exposure to suicidality predicted impact.
Methods
An international sample of 213 mental health practitioners completed an online survey on the impact of client suicide.
Results and Conclusion
Overall, results indicate MHPs are significantly affected by client suicide. A two-factor model in which impact of client suicide was predicted by two latent variables, MHP Characteristics and Exposure to Suicidality, explained 43% of short-term, 69% of long-term emotional, and 60% of long-term professional impact. Whereas MHP characteristics did not significantly predict any of the three impact variables (ps >.05), Exposure to Suicidality significantly predicted all three outcome variables (ps <.001). Interestingly, lived experience or exposure to suicidality of friends/family members predicted more impact, while exposure to suicidality at work predicted less impact of client suicide. Implications for both research and clinical practice are discussed.
MHPs are significantly affected by client suicide;
Previous exposure to suicidality predicts the impact of client suicide;
MHP characteristics do not predict the impact of client suicide.
HIGHLIGHTS
INTRODUCTION
Client suicide is used to refer to cases where a mental health practitioner (MHP) is exposed, affected, or bereaved by a client’s suicide (Ellis & Patel, Citation2012). Unfortunately, client suicides are not uncommon in clinical practice. Incidence rates vary depending on the geographical area of interest, with 30–80% of MHPs in Belgium, the U.S., Ireland, and Australia, as well as approximately 98% of MHPs in Slovenia who indicate to have lost a client to suicide (Finlayson & Simmonds, Citation2018; Grad, Zavasnik, & Groleger, Citation1997; Greenberg & Shefler, Citation2014; Landers, O'Brien, & Phelan, Citation2010; Rothes, Scheerder, Van Audenhove, & Henriques, Citation2013). To no surprise, 97% of clinicians claim client suicide to be their greatest fear (Ellis & Patel, Citation2012), as client suicide can have far-reaching consequences for psychologists, psychiatrists, nurses, general practitioners, and social workers, alike.
In the immediate aftermath of client suicide, MHPs are reported to experience emotions of shock, disbelief, confusion, and denial (Kleespies, Smith, & Becker, Citation1990). Feelings of distress, depression, anger at the client and/or agency/society, guilt, shame, a profound sense of responsibility, failure, and feelings of incompetence soon follow (Ting, Sanders, Jacobson, & Power, Citation2006). Research suggests about 50% of psychologists and social workers who have experienced client suicide go on to display post-traumatic stress symptoms such as intrusive thoughts, avoidant behavior toward potential suicidal clients, sleep disturbances, irritability, difficulty managing life events, and emotional burnout (Chemtob, Hamada, Bauer, Kinney, & Torigoe, Citation1988; Dransart, Gutjahr, Gulfi, Didisheim, & Séguin, Citation2014; Ellis & Patel, Citation2012; Ting et al., Citation2006). As such, client suicide seems to elicit symptomatology comparable to what we see when one loses a parent (Chemtob et al., Citation1988; Greenberg & Shefler, Citation2014).
Looking at the long-term impact of client suicide, MPH’s are likely to be subject to both far-reaching personal and professional consequences. Long-term emotional consequences may include depressive rumination, increased feelings of self-doubt and inadequacy, increased feelings of aloneness and isolation from their peers, increased sensitivity to signs of suicidal risk, increased concern over one’s competence to treat, as well as increased feelings of anxiety of helplessness when doing so (Alexander, Klein, Gray, Dewar, & Eagles, Citation2000; Ellis & Patel, Citation2012; Hendin, Lipschitz, Maltsberger, Haas, & Wynecoop, Citation2000; Mitchell, Gale, Garand, & Wesner, Citation2003; Thomyangkoon & Leenaars, Citation2008). Long-term professional consequences may include more attentiveness to legal matters of the profession, increased hours of supervision and peer to peer consultation, more vigilant and cautious when dealing with at-risk patients, or in general, for one to adopt a more conservative approach when treating suicidal clients, i.e., to be more inclined to hospitalize or to require no-suicide contracts (Alexander et al., Citation2000; Biermann, Citation2003; Finlayson & Simmonds, Citation2018; Rothes et al., Citation2013; Ting et al., Citation2006). In addition, research suggests about 15% of MHPs considered early retirement following a client loss (Alexander et al., Citation2000; Gulfi, Castelli Dransart, Heeb, & Gutjahr, Citation2010).
Individual differences regarding the impact of client suicide on MHPs have long been the topic of investigation. Grad et al. (Citation1997) investigated gender differences in impact by client suicide and found women compared to men report more feelings of shame and guilt, sought more consultation, and experienced more doubt regarding their professional knowledge. More recently, Wurst et al. (Citation2010) found women more than men to experience severe distress following client suicide, as well as to experience more sadness after, whereas Rothes et al. (Citation2013) noted that women compared to men reported significantly more feelings of failure and defeat. Concerning age or years of experience, research suggests trainees compared to experienced colleagues are more likely to experience client suicide (Ellis & Patel, Citation2012) and more likely to experience a complicated grieving process (Gill, Citation2012). Moreover, research suggests more professional experience is associated with fewer adverse consequences following client suicide (Hendin et al., Citation2000). In line with that, adequate training as provided by internship programs or offered while obtaining postgraduate degrees have been suggested as important protective factors when dealing with suicidal clients or in the aftermath of completed suicide (Anderson & Jenkins, Citation2005; Gill, Citation2012). For now, to what extent age, gender, years of experience, separately or combined, dictate the impact of client suicide is not entirely clear.
More recently, exposure to suicide, albeit within a personal or professional context, has also become been a topic of interest in light of how MHPs may deal with a suicide loss. Swain and Domino (Citation1985) investigated the prevalence of suicide exposure in a sample of 128 MHPs. Their results revealed that 30% of MHPs had considered suicide and 25% of MHPs had undertaken a non-fatal suicide attempt in the past. In addition, 60% of MHP knew someone who had died by suicide, 10% had lost a family member or relative to suicide, and 25% had lost a friend or acquaintance to suicide. Interestingly, Swain and Domino also revealed that MHPs with lived experience, albeit related to themselves or friends/relatives, were more accepting of suicidality and better able to recognize signs of suicidality (Citation1985). Later on, Pope and Tabachnick (1994) conducted a similar survey, with 29% of psychologists reporting they had been suicidal before and 4% of psychologists reporting a non-fatal suicide attempt previously. Likewise, Gilroy, Carroll, & Murra (Citation2002) surveyed a large group of psychologists and revealed that 62% of respondents self-identified as depressed and 42% of those reported experiencing some form of suicidal ideation or behavior. Finally, in a 2009 APA Colleague Assistance and Wellness Survey, 18% of MHPs acknowledged they had suffered from suicidal ideation while dealing with personal and professional stressors or challenges (American Psychological Association, Citation2010). Taken together, these results suggest a substantial amount of MHPs has lived experience or has been exposed to suicidality. The question remains, however, to what extent such exposure to suicidality helps or hinders when one is dealing with the trauma of client suicide.
The current study aims to investigate the short- and long-term impact of client suicide and to what extent characteristics like gender, years of experience, therapeutic background, and exposure to suicidality are associated with the impact of client suicide on MHPs using structural equation modeling.
METHODS
Participants
The study included 213 MHPs who experienced one or more client suicides. 53 identified as male (25%), 158 as female (74%) and 2 as non-binary (1%). Age ranged between 18 and 75, with 90% of participants aged between 18 and 55 years. Professions included psychologists (46%), psychiatric nurses (14%), psychiatrists (13%), counselors (10%), social workers (9%) or others (8%). The majority of the sample originated from Belgium (47%), Germany (16%), the Netherlands (16%), and the USA (15%). The remaining MHPs (6%) originated from Australia, China, Greece, Italy, Norway, South Africa, Togo, and the United Kingdom.
Procedure
The present study is part of a larger research project looking into the impact of client suicide. Study protocols were in accordance with the ethical standards of the ethical committee of the Erasmus University of Rotterdam, Netherlands. Individual informed consent was obtained prior to participation. Participant recruitment was set up through the distribution of the survey via email, social media, or professional newsletters, employing a convenience sample. Data was collected using a self-administered, online survey available in English, Dutch, and German. Participants were instructed that in the case that they had experienced multiple client suicide throughout their career, they would answer with their most distressing case of client suicide in mind. Survey completion took approximately 15 minutes.
Measures
To evaluate the impact of client suicide the Impact of Event Scale-R (IES-22-R; Creamer, Bell, & Failla, Citation2003; Weiss & Marmar, Citation1997), Long-Term Emotional Impact Scale (LTEIS; Gulfi et al., Citation2010; Horn, Citation1994), and Professional Practice Impact Scale (PPIS; Gulfi et al., Citation2010) were employed.
The IES-22-R is a revised version of the original IES (Creamer et al., Citation2003; Weiss & Marmar, Citation1997), a self-report questionnaire developed to assess the impact of a particular (traumatic) event in the seven days following the event. The IES-22-R includes 22 items divided over 3 subscales: (1) intrusion, (2) hyperarousal, and (3) avoidance. Each item is rated on a 5-point Likert scale, ranging from 0 “Not at all” to 4 “Extremely.” While the IES-22-R is not a diagnostic tool for PTSD, the consensus is sum scores between 24 and 32 suggest partial PTSD, sum scores between 33 and 38 suggest a PTSD diagnosis is probable, and sum scores of 39 or above suggest long-term impact (Asukai et al., Citation2002; Creamer et al., Citation2003). The IES-R is typically characterized by good internal consistency and test-retest reliability (for instance, see Beck et al., Citation2008). Cronbach’s alpha as calculated for the current sample was α = 0.95, suggesting excellent scale reliability.
The LTEIS (Gulfi et al., Citation2010; Horn, Citation1994) is a self-report questionnaire developed to assess the long-term emotional impact of client suicide. The LTEIS includes 10 items, each referring to one of ten emotional consequences that may present after client suicide. Items include, for example, increased concern, increased helplessness when working with suicidal clients, or increased sensitivity to signs of suicidal risk. Each item is rated on a 5-point Likert scale, ranging from 1 “Disagree” to 5 “Agree.” Cronbach’s alpha as calculated for the current sample was α = 0.87, suggesting good scale reliability.
The PPIS ( Gulfi et al., Citation2010; inspired by Henry, Séguin, & Drouin, Citation2004 ) is a self-report questionnaire developed to assess the professional consequences of client suicide. The PPIS includes 9 items, each referring to one of nine professional consequences common after client suicide. Items include, for example, more inclined to hospitalize, more inclined to consult, refusing to work with suicidal clients, or considering leaving the profession. Each item is rated on a 5-point Likert scale, ranging from 1 “Disagree” to 5 “Agree”. Cronbach’s alpha as calculated for the current sample was α = 0.77, suggesting good scale reliability.
To evaluate gender, years of experience, therapeutic background, and previous exposure to suicidality, participants were asked to answer the following questions: (1) What is your gender? (Gender; “male,” “female,” “non-binary”); (2) How many years of experience do you have as a MHP? (Years of Experience; <1 y, 3–5 y, 5–10 y, 10–15 y, 15–20 y, 25 y+); (3) What is your therapeutic background, if any? (Background; “no,” “CBT,” “psychoanalytic/psychodynamic,” “humanistic,” “systemic,” “other”); (4) Did you ever contemplate suicide or experience suicidal thoughts? (Self; “no,” “as child,” “as teenager,” “as adult”); (5) Do you have a close friend or relative who has struggled with suicidality? (Friends/Family; “thoughts,” “attempt,”, “suicide”); and (6) How often are you confronted with suicidal clients within your mental health setting? (Work; “never,” “few times a year,” “monthly,” “weekly or more”).
Data Analysis
To investigate whether MHP characteristics like gender, years of experience and therapeutic background and the extent to which one has been exposed to suicidality are associated with the impact of client suicide, simplified subgroups were created based on participants’ responses: (i) Gender: Male vs. Female; (ii) Years of Experience: <10 y vs. ≥10 y; (iii) Therapeutic Background: Yes vs. No; (iv) Self: Yes vs. No; (v) Friends/Family: Yes vs. No; (vi) Work: Seldom/Few times a year vs. Weekly/Monthly.
Statistical analyses were conducted using AMOS 24.0 for Windows. Confirmatory factor analysis (CFA) and structural equation modeling (SEM) analyses were estimated using the maximum likelihood estimation method. The Comparative Fit Index (CFI) and Root Mean Square Error of Approximation (RMSEA) were used as indicators of model fit. For the CFI, model fit is deemed acceptable if CFI values are greater than 0.90. For the RMSEA, values below 0.05 indicate close approximate fit, while values between 0.05 and 0.08 suggest a reasonable error of approximation (Wang, Chen, Dai, & Richardson, Citation2018). The data that support the findings of this study are available from the corresponding author upon reasonable request.
RESULTS
Impact of Client Suicide
To evaluate the short- and long-term impact of client suicide, three distinct outcomes were evaluated, for descriptives see . For short-term impact, as evaluated by the sum scores for the IES-R-22, results suggest participants on average experienced (at least) some PTSD symptomatology (M = 25.66, SD = 19.25, range = 0 − 83), with 11% experiencing some symptoms (4–32), 5% experiencing full PTSD symptomatology (33–38) and 27% experiencing PTSD symptomatology suggestive of long-term impact (39+), in the 7 days following the client suicide. Participants mostly endorsed items referring to intrusions (M = 11.69, SD = 8.28; 8 items), compared to hyperarousal (M = 6.51, SD = 6.00; 6 items). and avoidance (M = 7.46, SD = 6.75; 8 items). Concerning long-term emotional impact, as indicated by the LTEIS (M = 2.90, SD = 0.92), participants endorsed a wide range of experiences, in particular, items related to increased “concern,” “anxiety” and “guilt” related to the client suicide, as well as “acceptance (of the fact) that suicide occurs” and “sensitivity to signs of suicidal risk.” Concerning long-term professional impact, as indicated by the PPIS (M = 2.65, SD = 0.73), participants tended to endorse items related to an increased inclination to “consult colleagues/supervisor,” “more precise note keeping,” “more attentive and sensitive to legal matters” and “more interest in the phenomenon of suicide.” Overall, 5% of participants indicated they now refuse to work with suicidal clients and 12% indicated they consider leaving the profession as a result of client suicide they experienced.
TABLE 1. Descriptive statistics for the IES-R, LTEIS, and PPIS.
Predicting Impact of Client Suicide
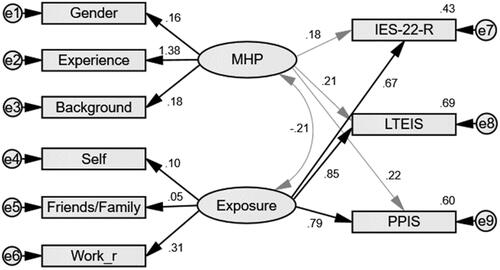
To investigate whether MHP characteristics such as gender, years of experience, and therapeutic background and the extent to which one has been exposed to suicidality are associated with the impact of client suicide, a CFA and path analysis in SEM were conducted. First, a model including two higher-order latent variables was created. Factor 1, defined as MHP characteristics (“MHP”), included the variables for Gender, Years of Experience, and Background). Factor 2, defined as Exposure to Suicidality (“Exposure”), included the variables for exposure to suicidality related to the Self, Friends/Family, and Work excellent model fit (CFI = 1.00 and RMSEA = 0.00) was achieved (Wang et al., Citation2018). No error correlations were utilized to achieve this fit.
Secondly, this two-factor model was used to predict the short- and long-term impact of client suicide. Conducting a path analysis in SEM, adequate model fit, with CFI = 0.94 and RMSEA = 0.05 (Wang et al., Citation2018) was achieved. Again, no error correlations were utilized to achieve this fit. To help interpretation, Work was included as a reversed factor. Standardized estimates of the confirmatory model and R-squared multiple correlations are shown in . The two-factor model explained 43% of the short-term, 69% of the long-term emotional, and 60% of the long-term professional impact variance. Factor 1, MHP, did not significantly predict any of the three impact scales (ps >.05). In other words, the impact of client suicide cannot be predicted by gender, years of experience, and therapeutic background. Factor 2, Exposure, did have a positive significant predictive value for all three outcome variables: short-term impact (β = 0.67, p <.001), long-term emotional impact (β = 0.85, p < .001), and long-term professional impact (β = 0.79, p < .001). This indicates that the level of exposure to suicidality, either because one was suicidal themselves, had friends or family members who were at one point suicidal or whether one is often confronted with suicidal clients at work, predicts higher levels of impact of client suicide. Interestingly, the model suggests that lived exposure to suicidality within oneself (β = 0.10) or with friends/family (β = 0.05) predicted more impact, while exposure to suicidality at work (β = 0.30) predicted less impact of client suicide. Moreover, the correlation between Factor 1, MHP, and Factor 2, Exposure, was not significant (r = −0.21, p > .05).
DISCUSSION
The current study aimed to investigate the short- and long-term impact of client suicide and to what extent MHP characteristics such as gender, years of experience, and therapeutic background as well as exposure to suicidality within a personal or professional context, are can predict the impact of client suicide on MHPs. Using SEM, results indicate significant short- and long-impact emotional and professional impact of client suicide, as measured by the IES-R, LTEIS, and PPIS. A two-factor model, in which the impact of client suicide was predicted by MHP Characteristics and Exposure to Suicidality explained 43% of the short-term, 69% of the long-term emotional, and 60% of the long-term professional impact. Whereas MHP characteristics did not predict any of the three impact variables (ps > .05), Exposure to Suicidality significantly predicted all three outcome variables. Moreover, an interesting dichotomy was revealed within Exposure to Suicidality, as exposure within a private context (Self and Family/Friends) and lack of exposure within a professional context predict more impact of client suicide. Taken together, the results suggest that (1) MHPs are significantly affected by client suicides and that (2) exposure to suicidality is more informative concerning assessing impact than individual MHPs characteristics. Implications for future research and clinical practice are discussed.
Client Suicide is Traumatic
When MHPs experience a client suicide, they are subject to short- and long-term consequences. Results regarding short-term impact, i.e., the 7 days following a client suicide, reveal on average participants reported symptoms suggestive of partial PTSD, with some reporting full PTSD symptomatology (5%) and others reporting PTSD symptomatology severe enough to suggest long-term impact (27%). Overall, items related to intrusions were endorsed most, suggesting participants often found themselves thinking of it, experienced waves of strong feelings about it, or experienced trouble sleeping and/or ended up dreaming about it. Results regarding long-term impact suggest participants continue to experience increased concern, anxiety, and guilt related to the client's suicide, while at the same time, they find themselves more accepting of and more sensitive to signs of suicidality. Moreover, participants continue to feel more inclined to consult colleagues/supervisors, to remain diligent about note keeping, and to be more attentive to legal matters of the profession. About 5% of participants indicated they now refuse to work with suicidal clients while about 12% are considering leaving the profession as a result of client suicide they experienced.
Overall, these results are in line with previous findings. Previous research suggests about 50% of psychologists and social workers who have experienced client suicide go on to display post-traumatic stress symptoms (Chemtob et al., Citation1988; Dransart et al., Citation2014; Ellis & Patel, Citation2012; Ting et al., Citation2006). Moreover, MHPs are likely to experience long-term consequences like increased feelings of anxiety or helplessness, increased sensitivity to signs of suicidal risk (Alexander et al., Citation2000; Ellis & Patel, Citation2012; Hendin et al., Citation2000; Mitchell et al., Citation2003; Thomyangkoon & Leenaars, Citation2008), more attentiveness to legal matters, increased supervision, and more vigilance and caution when dealing with at-risk patients (Alexander et al., Citation2000; Biermann, Citation2003; Finlayson & Simmonds, Citation2018; Rothes et al., Citation2013; Ting et al., Citation2006). As such, one can conclude that losing a client to suicide should be considered a significant and painful event for most MHPs, with not just short- but long-term consequences.
Predicting Impact of Client Suicide
To investigate whether MHP characteristics like gender, years of experience, and therapeutic background, and exposure to suicidality can predict the impact of client suicide, a SEM analysis was conducted. MHP characteristics including gender, years of experience, and therapeutic background, did not predict impact, whereas Exposure to Suicidality did.
Concerning MHP characteristics previous research has found some, though small, differences: women compared to men (Grad et al., Citation1997; Rothes et al., Citation2013; Wurst et al., Citation2010) and trainees compared to people with more experience (Anderson & Jenkins, Citation2005; Ellis & Patel, Citation2012; Gill, Citation2012; Hendin et al., Citation2000) have been reported to experience more impact following client suicide. Our results suggest that whether MHPs are male or female, had more or less than 10 y of experience, or had a particular therapeutic background or not, did not predict the impact of client suicide. While it may be the case that, depending on the circumstances, MHPs may feel their (lack of) experience or therapeutic training was an important element in their dealing with client suicide, our results do not support previous findings suggesting systematic differences along those lines.
Exposure to Suicidality, whether one has struggled with suicidality themselves, has friends or relatives who have or whether one is often confronted with suicidality at work, did predict the impact of client suicide. Interestingly, results suggest that exposure to suicidality within oneself or related to friends or family and a lack of exposure within a work context predicted more impact of client suicide. Most MHPs deal with suicidality frequently; 30–80% of clinicians have lost one or more clients to suicide—and suicidality of patients, depending on the work setting, can be a daily, weekly, or monthly occurrence (Finlayson & Simmonds, Citation2018; Grad et al., Citation1997; Greenberg & Shefler, Citation2014; Landers et al., Citation2010; Rothes et al., Citation2013). Moreover, many MHPs have also been confronted with suicidality within a personal context, struggling with suicidality themselves, or through friends or relatives who have a history of suicidality (Gilroy et al., Citation2002; CitationPope & Tabachnick, 1994; Swain & Domino, Citation1985). In addition, Swain and Domino revealed that MHPs with lived experience, albeit related to themselves or friend/relatives, were more accepting of suicidality and better able to recognize signs of suicidality (1985). In part, this is in line with our results, suggesting exposure to suicidality is associated with more short- and long-term emotional impact, including but not limited to more “accepting (of the fact) that suicide occurs” and more “sensitive to signs of suicidal risk.”
Implications and Limitations
The current study, which focused on the impact of client suicide and the relevance of MHP characteristics and exposure to suicidality with regard to impact, has implications for both research and clinical practice. As much as we would like to prevent all client suicides, it is unlikely a zero-suicide level will ever be reached. Therefore, it is of particular importance to invest in both intervention and postvention initiatives as well as research what aspects predict both the initial impact and the long-term recovery process (Oordt, Jobes, Fonseca, & Schmidt, Citation2009). The current results justify an investment in training programs for all, men vs. women, new to the profession or not, therapeutic background or not, including both prevention and postvention concerning suicide. These training programs should cover suicidality within a professional and private setting, given exposure and/or lived experience within these domains may have different consequences. Alternatively, these topics should receive particular attention in MHPs personal therapy, allowing the MHP to understand the importance of these events in light of their personal history and particular employment (Moe & Thimm, Citation2021). Interestingly, the suicide survivor movement’s pushes to acknowledge one’s lived experience (Eddie et al., Citation2019) and attempts to reduce stigma within the general public, do not seem to have been mirrored among MHPs as much. While more clinicians are stepping forward to share their stories as suicide survivors, numbers are limited and research as to the importance or impact of lived experience remains limited.
Two limitations need to be acknowledged and considered when interpreting or generalizing the current findings. The first limitation pertains to the way the current data was collected. The current study employed a convenience sample and relied on retrospective self-report data, meaning participants were asked to complete a self-report questionnaire and report on events, thoughts, feelings, and behavior that may have taken place, in some cases, years earlier. While self-report questionnaires and convenience samples are typical for trauma research (e.g., Blaney, Citation1986; Frissa et al., Citation2016; Roemer, Litz, Orsillo, Ehlich, & Friedman, Citation1998; Southwick, Morgan, Nicolaou, & Charney, Citation1997; Wessely et al., Citation2003), they warrant limitations regarding the generalizability of the results. Moreover, data pertaining to the time of the event MHPs reported on was not collected and, as such, the retrospective self-report data may be subject to significant recall bias. A second limitation pertains to the cross-sectional nature of the data. Any analyses based on cross-sectional data rather than longitudinal data remain mostly exploratory in nature. SEM has several important strengths, for instance, one can specify latent variable models that provide separate estimates of relations among latent constructs and their manifest indicators and of the relations among constructs. Moreover, models can be evaluated in terms of global fit and model validity and multiple outcome variables can be investigated within the same model (compared to multiple regression) (Tomarken & Waller, Citation2005). However, as the current SEM model relied on cross-sectional data, we cannot determine cause and effect or assume causal relationships. While it is highly unlikely that experiencing client suicide would impact MHPs’ report of demographic variables, it is (theoretically) possible that experiencing a client suicide made MHPs report differently on their previous exposure to suicide, rather than the other way around. Hence, SEM models that employ a longitudinal design are needed to further investigate these interplays.
AUTHOR NOTE
Ruth Van der Hallen, Department of Psychology, Education & Child Studies, Erasmus University Rotterdam, Rotterdam, 3062 PA, The Netherlands.
ACKNOWLEDGMENTS
I would like to thank Lilli Hahne, Lydia Mazur, Johanna Bernodusson, and Marianna Triantafyllou for their help with the data collection and Brian Godor for his help with the data analysis.
DISCLOSURE STATEMENT
No potential conflict of interest was reported by the author(s).
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Additional information
Notes on contributors
Ruth Van der Hallen
Ruth Van der Hallen, Department of Psychology, Education & Child Studies, Erasmus University Rotterdam, Rotterdam, 3062 PA, The Netherlands.
REFERENCES
- Alexander, D. A., Klein, S., Gray, N. M., Dewar, I. G., & Eagles, J. M. (2000). Suicide by patients: Questionnaire study of its effect on consultant psychiatrists. BMJ, 320(7249), 1571–1574. doi:10.1136/bmj.320.7249.1571
- American Psychological Association (2010). Survey findings emphasize the importance of self care for psychologists. https://www.apaservices.org/practice/update/2010/08-31/survey.
- Anderson, M., & Jenkins, R. (2005). The challenge of suicide prevention. Disease Management & Health Outcomes, 13(4), 245–253. doi:10.2165/00115677-200513040-00003
- Asukai, N., Kato, H., Kawamura, N., Kim, Y., Yamamato, K., Kishimoto, J., … Nishizono-Maher, A. (2002). Reliability and validity of the Japanese-language version of the Impact of Event Scale-revised (IES-R-J): Four studies of different traumatic events. Journal of Nervous and Mental Disease, 190(3), 175–182. doi:10.1097/00005053-200203000-00006
- Beck, J. G., Grant, D. M., Read, J. P., Clapp, J. D., Coffey, S. F., Miller, L. M., & Palyo, S. A. (2008). The impact of event scale-revised: Psychometric properties in a sample of motor vehicle accident survivors. Journal of Anxiety Disorders, 22(2), 187–198. doi:10.1016/j.janxdis.2007.02.007
- Biermann, B. (2003). When depression becomes terminal: The impact of patient suicide during residency. The Journal of the American Academy of Psychoanalysis and Dynamic Psychiatry, 31(3), 443–457. doi:10.1521/jaap.31.3.443.22130
- Blaney, P. H. (1986). Affect and memory: A review. Psychological Bulletin, 99(2), 229–246. doi:10.1037/0033-2909.99.2.229
- Chemtob, C. M., Hamada, R. S., Bauer, G., Kinney, B., & Torigoe, R. Y. (1988). Patients’ suicides: Frequency and impact on psychiatrists. The American Journal of Psychiatry, 145(2), 224–228. doi:10.1176/ajp.145.2.224
- Creamer, M., Bell, R., & Failla, S. (2003). Psychometric properties of the Impact of Event Scale – Revised. Behaviour Research and Therapy, 41(12), 1489–1496. doi:10.1016/j.brat.2003.07.010
- Dransart, D. A. C., Gutjahr, E., Gulfi, A., Didisheim, N. K., & Séguin, M. (2014). Patient suicide in institutions: Emotional responses and traumatic impact on Swiss mental health professionals. Death Studies, 38(1–5), 315–321. doi:10.1080/07481187.2013.766651
- Eddie, D., Hoffman, L., Vilsaint, C., Abry, A., Bergman, B., Hoeppner, B., Weinstein, C., & Kelly, J. F. (2019). Lived experience in new models of care for substance use disorder: A systematic review of peer recovery support services and recovery coaching. Frontiers in Psychology, 10, 1052. doi:10.3389/fpsyg.2019.01052
- Ellis, T. E., & Patel, A. B. (2012). Client suicide: What now? Cognitive and Behavioral Practice, 19(2), 277–287. doi:10.1016/j.cbpra.2010.12.004
- Finlayson, M., & Simmonds, J. G. (2018). Impact of client suicide on psychologists in Australia. Australian Psychologist, 53(1), 23–32. doi:10.1111/ap.12240
- Frissa, S., Hatch, S. L., Fear, N. T., Dorrington, S., Goodwin, L., & Hotopf, M. (2016). Challenges in the retrospective assessment of trauma: Comparing a checklist approach to a single item trauma experience screening question. BMC Psychiatry, 16, 20. doi:10.1186/s12888-016-0720-1
- Gill, I. J. (2012). An identity theory perspective on how trainee clinical psychologists experience the death of a client by suicide. Training and Education in Professional Psychology, 6(3), 151–159. doi:10.1037/a0029666
- Gilroy, P. J., Carroll, L., & Murra, J. (2002). A preliminary survey of counseling psychologists’ personal experiences with depression and treatment. Professional Psychology: Research and Practice, 33(4), 402–407. doi:10.1037/0735-7028.33.4.402
- Grad, O. T., Zavasnik, A., & Groleger, U. (1997). Suicide of a patient: Gender differences in bereavement reactions of therapists. Suicide & Life-Threatening Behavior, 27(4), 379–386. doi:10.1111/j.1943-278X.1997.tb00517.x
- Greenberg, D., & Shefler, G. (2014). Patient suicide. The Israel Journal of Psychiatry and Related Sciences, 51(3), 193–198.
- Gulfi, A., Castelli Dransart, D. A., Heeb, J.-L., & Gutjahr, E. (2010). The impact of patient suicide on the professional reactions and practices of mental health caregivers and social workers. Crisis, 31(4), 202–210. doi:10.1027/0027-5910/a000027
- Hendin, H., Lipschitz, A., Maltsberger, J. T., Haas, A. P., & Wynecoop, S. (2000). Therapists' reactions to patients' suicides. The American Journal of Psychiatry, 157(12), 2022–2027. doi:10.1176/appi.ajp.157.12.2022
- Henry, M., Séguin, M., & Drouin, M.-S. (2004). Les réactions des professionnels en snaté mentale au décès par suicide d’un patient [Mental health professionals’ response to the suicide of their patients]. Revue Québécoise de Psychologie, 25(3), 241–257.
- Horn, P. J. (1994). Therapists’ psychological adaptation to client suicide. Psychotherapy: Theory, Research, Practice, Training, 31(1), 190–195. doi:10.1037/0033-3204.31.1.190
- Kleespies, P. M., Smith, M. R., & Becker, B. R. (1990). Psychology interns as patient suicide survivors: Incidence, impact, and recovery. Professional Psychology: Research and Practice, 21(4), 257–263. doi:10.1037/0735-7028.21.4.257
- Landers, A., O'Brien, S., & Phelan, D. (2010). Impact of patient suicide on consultant psychiatrists in Ireland. The Psychiatrist, 34(4), 136–140. doi:10.1192/pb.bp.109.025312
- Mitchell, A. M., Gale, D. D., Garand, L., & Wesner, S. (2003). The use of narrative data to inform the psychotherapeutic group process with suicide survivors. Issues in Mental Health Nursing, 24(1), 91–106. doi:10.1080/01612840305308
- Moe, F. D., & Thimm, J. (2021). Personal therapy and the personal therapist. Nordic Psychology, 73(1), 3–28. doi:10.1080/19012276.2020.1762713
- Oordt, M. S., Jobes, D. A., Fonseca, V. P., & Schmidt, S. M. (2009). Training mental health professionals to assess and manage suicidal behavior: Can provider confidence and practice behaviors be altered? Suicide & Life-Threatening Behavior, 39(1), 21–32. doi:10.1521/suli.2009.39.1.21
- Pope, K. S., & Tabachnick, B. G. (1994). Therapists as patients: A national survey of psychologists’ experiences, problems, and beliefs. Professional Psychology: Research and Practice, 25(3), 247–258. doi:10.1037/0735-7028.25.3.247
- Roemer, L., Litz, B. T., Orsillo, S. M., Ehlich, P. J., & Friedman, M. J. (1998). Increases in retrospective accounts of war-zone exposure over time: The role of PTSD symptom severity. Journal of Traumatic Stress, 11(3), 597–605. doi:10.1023/A:1024469116047
- Rothes, I. A., Scheerder, G., Van Audenhove, C., & Henriques, M. R. (2013). Patient suicide: The experience of Flemish psychiatrists. Suicide & Life-Threatening Behavior, 43(4), 379–394. doi:10.1111/sltb.12024
- Southwick, S. M., Morgan, C. A., Nicolaou, A. L., & Charney, D. S. (1997). Consistency of memory for combat-related traumatic events in veterans of Operation Desert Storm. The American Journal of Psychiatry, 154(2), 173–177. doi:10.1176/ajp.154.2.173
- Swain, B. J., & Domino, G. (1985). Attitudes toward suicide among mental health professionals. Death Studies, 9(5–6), 455–468. doi:10.1080/07481188508252537
- Thomyangkoon, P., & Leenaars, A. (2008). Impact of death by suicide of patients on Thai psychiatrists. Suicide & Life-Threatening Behavior, 38(6), 728–740. doi:10.1521/suli.2008.38.6.728
- Ting, L., Sanders, S., Jacobson, J. M., & Power, J. R. (2006). Dealing with the aftermath: A qualitative analysis of mental health social workers' reactions after a client suicide. Social Work, 51(4), 329–341. doi:10.1093/sw/51.4.329
- Tomarken, A. J., & Waller, N. G. (2005). Structural equation modeling: Strengths, limitations, and misconceptions. Annual Review of Clinical Psychology, 1(1), 31–65. doi:10.1146/annurev.clinpsy.1.102803.144239
- Wang, S., Chen, C.-C., Dai, C.-L., & Richardson, G. B. (2018). A call for, and beginner’s guide to, measurement invariance testing in evolutionary psychology. Evolutionary Psychological Science, 4(2), 166–178. doi:10.1007/s40806-017-0125-5
- Weiss, D. S., & Marmar, C. R. (1997). The Impact of Event Scale—revised. In J. P. Wilson & T. M. Keane (Eds.), Assessing psychological trauma and PTSD (pp. 399–411). The Guilford Press.
- Wessely, S., Unwin, C., Hotopf, M., Hull, L., Ismail, K., Nicolaou, V., & David, A. (2003). Stability of recall of military hazards over time. Evidence from the Persian Gulf War of 1991. The British Journal of Psychiatry, 183(4), 314–322.
- Wurst, F. M., Mueller, S., Petitjean, S., Euler, S., Thon, N., Wiesbeck, G., & Wolfersdorf, M. (2010). Patient suicide: A survey of therapists' reactions. Suicide & Life-Threatening Behavior, 40(4), 328–336. doi:10.1521/suli.2010.40.4.328