Abstract
Background: Recent evidence indicates that home telemonitoring of chronic patients reduces the use of healthcare resources. However, further studies exploring this issue are needed in primary care.
Objectives: To assess the impact of a primary care-based home telemonitoring intervention for highly unstable chronic patients on the use of healthcare resources.
Methods: A one-year follow-up before and after exploratory study, without control group, was conducted. Housebound patients with heart failure or chronic lung disease, with recurrent hospital admissions, were included. The intervention consisted of patient’s self-measurements and responses to a health status questionnaire, sent daily from smartphones to a web-platform (aided by an alert system) reviewed by healthcare professionals. The primary outcome measure was the number of hospital admissions occurring 12 months before and after the intervention. Secondary outcomes were length of hospital stay and number of emergency department attendances. Primary care nurses were mainly in charge of the telemonitoring process and were assisted by the general practitioners when required.
Results: For the 28 patients who completed the follow-up (out of 42 included, 13 patients died and 1 discontinued the intervention), a significant reduction in hospitalizations, from 2.6 admissions/patient in the previous year (standard deviation, SD: 1.6) to 1.1 (SD: 1.5) during the one-year telemonitoring follow-up (P <0.001), and emergency department attendances, from 4.2 (SD: 2.6) to 2.1 (SD: 2.6) (P <0.001) was observed. The length of hospital stay was reduced non-significantly from 11.4 to 7.9 days.
Conclusion: In this small exploratory study, the primary care-based telemonitoring intervention seemed to have a positive impact decreasing the number of hospital admissions and emergency department attendances.
Key messages
This small-sample exploratory study suggests that primary care-based home telemonitoring of complex chronic patients may be a promising technology that which might reduce hospital admissions and the length of hospital stays.
Moreover, this study suggests a reduction of the number of emergency department attendances while patients were telemonitored.
Introduction
The growing prevalence of chronic health problems and the pressing need for efficient healthcare resources are encouraging the adoption of new effective primary care models. Among such models, home telemonitoring of patients with chronic diseases could offer a possible solution. The telemonitoring of patients in a home setting involves the remote transmission of patient clinical data, allowing subsequent examination by healthcare professionals. Such flow of frequent clinical information may facilitate the patient follow-up and enables decision making which in turn, could lead to faster interventions and avoidance of hospital admissions and use of other healthcare resources. This approach has been most widely applied in heart failure (HF) and chronic obstructive pulmonary disease (COPD).
Several randomized controlled trials (RCT) and systematic reviews with or without meta-analyses [Citation1–10] have been recently published regarding the utility of telemonitoring in reducing hospital admissions and mortality [Citation1,Citation2,Citation4,Citation8,Citation9] in HF, and in decreasing admissions in COPD patients [Citation7,Citation10]. The effect in emergency department attendances has been less explored or there is less evidence regarding this outcome measure. Among the randomized clinical trials, the ‘whole system demonstrator’ (WSD) deserves a special mention, because of its size (3230 patients with diabetes, COPD or HF were included), its practical nature (179 primary care centres were involved) and the impact on mortality, number of emergency department attendances, and number of hospital admissions, showing reductions of 45%, 20% and 11%, respectively [Citation11,Citation12]. However, the telemonitoring experiences managed from primary care are still scarce [Citation13], despite the fact that chronic patients can receive routine care through this level of assistance and implementation of such technology in primary care has been associated with higher efficiency and lower costs compared to the hospital level [Citation14,Citation15].
In the previous TELBIL RCT [Citation14,Citation16], the assessment of a primary care-based telemonitoring intervention showed a significant decrease in healthcare resources use [Citation14]. In 2012, the TELBIL-A study was launched, consisting of an implementation of the previous strategy and further evaluation of the adapted telemonitoring intervention. Marked changes were made seeking to improve the benefits of the remote monitoring and, at the same time, fully integrating the process within actual clinical primary care practice. A high level of acceptance and satisfaction with the TELBIL-A intervention was observed among both patients/relatives and healthcare professionals [Citation17,Citation18].
The objective of the present exploratory study was to assess the influence of a primary care-based home telemonitoring intervention for highly unstable (complex) chronic patients, within routine clinical practice, on healthcare resource use (i.e. hospital admissions and emergency department attendances).
Methods
Study design and setting
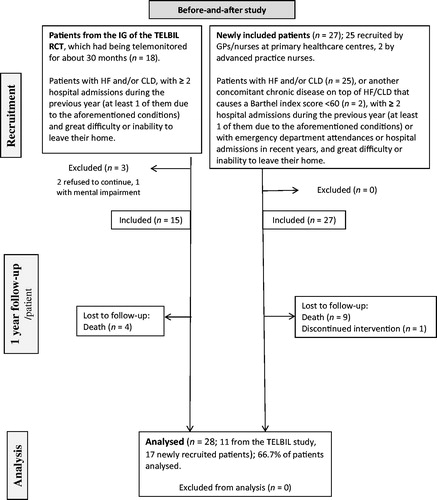
We used a comparative before and after exploratory study, without a control group. The overall length of the study (open recruitment of patients during the first year) was from mid-February 2012 to mid-February 2014, with an individual follow-up per patient of one year, from the inclusion date up to the following year. summarizes the general project design.
Figure 1. Study design and flow of participants through the study. IG: intervention group; RCT: randomized controlled trial; HF: heart failure; CLD: chronic lung disease; GP: General Practitioner.
The study was conducted in the urban-based Bilbao-Basurto Integrated Healthcare Organization (IHO), with a catchment population of around 384 000 people. This IHO included a referral hospital and 25 primary healthcare centres (PHC), with 230 general practitioners (GPs) and 320 nurses.
The study was approved by the Ethics Committee for Scientific Research (Basurto University Hospital, Bizkaia) (19 October 2011) and the Primary Care Research Committee of the Basque Health Service (Osakidetza) (18 October 2011). Patients/relatives gave written informed consent prior to participating in the study.
Selection of study patients
Inclusion criteria. Adult housebound patients (with great difficulty or inability to leave their home) with HF and/or chronic lung disease (CLD) (mainly COPD and a few of them with asthma), with a history of at least two hospital admissions in the previous year (and at least one of them due to the aforementioned conditions) were included in the study. These were also the patient inclusion criteria in the TELBIL RCT.
For newly included patients, those who as well as having HF and/or CLD, had markedly impaired functional status (Barthel index <60) due to concomitant chronic conditions and had two hospital admissions in the previous year or, alternatively, had several emergency department attendances or hospital admissions in recent years could also be included in the study.
Owing to the specific inclusion conditions and complexity of the patients, and based on previous records and lists used in the TELBIL RCT, we estimated that there would be approximately 80 eligible patients in the Bilbao-Basurto IHO. According to the ambulatory care group-predictive modelling (ACG-PM) stratification [Citation19], 27.6% of patients included in our study were labelled as ‘complex patients’ coinciding with the tip of the Kaiser Permanente pyramid. The majority of them, however, were above the aforementioned level, giving an indication of the high complexity and instability of the sample studied.
Exclusion criteria
Patients in residential care, those in terminal phases with a life expectancy of less than six months due to other illnesses unrelated to the inclusion condition (as subjectively judged by their GPs), and those unable to carry out a continuous follow-up using the telemonitoring equipment were excluded.
Patient recruitment process
First, patients belonging to the intervention and control groups of the preceding TELBIL RCT, who wished to continue or start the telemonitoring were recruited. Second, new patients were recruited by nurses and GPs that agreed to participate in the study, once the project was presented at all PHC and collaboration was requested. Additionally, recruitment was conducted by the advanced practice nurses (APN, nurses who specialize in the care of patients with multimorbidity at home). Participants gradually joined the study over a period of one year. Influenced by budget and time limitations, all potentially eligible patients could not be included in the study.
Intervention
The telemonitoring consisted of daily self-monitoring of a patient-specific set of clinical parameters, sent from the patient’s home using smartphones to a specific Web-platform. Additionally, patients/caregivers completed a brief health status questionnaire assessing the patient’s perception of his/her medical and functional condition, together with a series of common and condition-specific questions. The contents of the questionnaire were personalized based on the patient’s clinical characteristics, specific pathology and the criterion of the GP or nurse in charge of the patient. illustrates the default clinical parameters for the patients. When pre-established threshold values were crossed, red or yellow alerts were triggered at the web-platform where the data were transmitted daily.
Table 1. Parameters and initial thresholds.
Study variables
The sociodemographic and clinical baseline information is shown in . The main outcome measure was the number of hospital admissions that occurred during the 12 months before and after the inclusion of each patient in the study. Secondary outcome measures were the length of hospital stay per admission and the total number of emergency department attendances during the year of follow-up compared to the 12-months prior to telemonitoring. The information required for the analysis was obtained from electronic clinical records and discharge clinical reports.
Table 2. Patients’ baseline characteristics.
Sample size and power estimation
A power estimation was calculated considering the 42 patients recruited for the study (constrained by budget and time limitations), using the results obtained in the preceding intervention group (IG) of the TELBIL study [Citation14]. A 25% loss to follow-up was assumed after 12 months, together with a mean of 3.4 all-cause hospital admissions in the year prior to telemonitoring and a standard deviation (SD) of 2.3 in the difference between the before and after rates. Based on these data, the study was estimated to have an 86% statistical power for detecting a 35% decrease in the number of all-cause admissions during the year of follow-up as statistically significant (95% confidence).
Data analysis
Patient’s baseline characteristics were defined as those registered at the end of the telemonitoring-free period. Hence, the baseline values of participants coming from the IG of the TELBIL RCT corresponded to the measurements taken at the beginning of that study. Patients’ baseline characteristics were described using means and SD or frequencies according to the quantitative or qualitative nature of the variables.
Homogeneity between patients lost to follow-up and patients completing the study was analysed. When dealing with quantitative variables the t-test or the non-parametric Mann–Whitney test was performed depending on the fulfilment of the normality assumption. For qualitative variables, the chi-squared test or the Fisher’s exact test was conducted. Homogeneity in baseline characteristics between patients belonging to the IG of the preceding TELBIL RCT and newly recruited patients was checked analogously. A 95% confidence level was established.
To assess the influence on healthcare resources use (total and condition-specific admissions, length of hospital stays and emergency department attendances) a before and after analysis was performed. T-test for paired samples was carried out when the normality assumption was met; otherwise, the Wilcoxon signed-rank test was used.
Results
A total of 42 patients were enrolled, 15 of which belonged to the IG of the TELBIL RCT and 27 were newly recruited (two patients were included by the APN). Two patients, out of the 27 newly recruited participants, had a severely impaired functional status with a Barthel index <60. These two patients had other chronic diseases on top of HF/CLD that caused a serious deterioration of their functional status: one had morbid obesity and HF and the other had had a stroke and COPD. Three patients from the IG of the TELBIL RCT were excluded (two refused to continue and one had advanced mental impairment). Twenty-eight patients completed the 12-month follow-up, 11 of them came from the preceding trial. Fourteen patients were lost to follow-up (13 died and one declined to continue). Out of the 13 deceased patients, five died of heart causes, five of respiratory causes and three as a result of other diseases.
Baseline characteristics
summarises patients’ baseline characteristics, both overall and distinguishing between participants coming from the IG of the TELBIL RCT and those newly recruited. The mean age was 78.9 (SD 7.5) years and 57.8% were women; 14.3% of patients had HF and 23.8% CLD while 57.2% had both conditions concurrently.
No variable showed significant differences among patients lost to follow-up and patients who completed the study (data not shown). Homogeneity between participants coming from the IG of the preceding trial and newly recruited patients was satisfied for all baseline characteristics.
Impact on healthcare resources use
The results of the before and after analysis are shown in . Statistically significant reductions in all-cause and condition-specific hospital admissions and emergency department attendances were found. The mean length of hospital stay was decreased by 3.5 days, though statistical significance was not reached.
Table 3. Results of the before and after analysis on healthcare resources use (n = 28 patients).
Considering the specific pathologies, when both (CLD and HF) coexisted in the same patient who completed the year of follow-up (n = 16), there were significant differences in all-causes of hospital admissions, mean 2.8 (SD: 1.5) versus 1.1 (SD: 1.8) (P = 0.017), and in the emergency department attendances not followed by hospital admissions, 2.3 (SD: 2.1) versus 0.9 (SD: 1.4) (P = 0.009); but not in condition-specific hospital admissions (P = 0.091). Only a very small number of patients had one of the two pathologies exclusively (eight patients had CLD and four had HF).
Discussion
Main findings
Hospital admissions. The results of this small exploratory study appear to show that the impact of the intervention on the reduction of hospital admissions and emergency department attendances seemed to be greater than in the previous TELBIL RCT [Citation14], probably due to the positive influence of the modifications made to the intervention. The before and after analysis, showed a statistically significant decrease in the number of hospital admissions during the 12-month telemonitoring period compared to the previous year. This finding is in agreement with other studies [Citation3,Citation6–10,Citation12,Citation20].
Emergency department attendances. Moreover, a significant decrease in the number of emergency department attendances was observed. Specifically, the mean number of total attendances fell from 4.2 in the 12-month period before telemonitoring to 2.1 during the 12-month follow-up. A similar decrease was also noted in other studies, such as the WSD project, which reported a 20% reduction [Citation12], although there is considerably less published evidence regarding this outcome measure. Nevertheless, the percentage of emergency department attendances without subsequent hospital admissions increased, which could be a positive indicator, since a higher percentage of emergency department attendances could have been solved without the need for admission.
Length of hospital stay. A notable reduction of length of the hospital stays was noticed, which, despite not being statistically significant, was consistent with other telemonitoring studies of patients with HF or COPD [Citation2,Citation12,Citation13]. In the present study, the mean length of stay decreased by 3.5 days after telemonitoring, which could have had a substantial impact both on the quality of life of the patients/relatives and on the costs associated with hospitalization. Such a reduction of hospital stay could be due to the early detection and treatment of exacerbating factors.
Satisfaction of professionals and patients. In addition to the positive impact on the use of healthcare resources, the high level of satisfaction of the healthcare professionals and patients/relatives with the telemonitoring in the TELBIL-A study constitutes a key factor that may influence the successful uptake of such interventions [Citation17,Citation18]. Other studies have also shown that healthcare professionals are generally satisfied with telemedicine activities when they are closely involved [Citation21–23], although results are not consistent [Citation24,Citation25].
Strengths and limitations
Unlike the preceding TELBIL study, a RCT focused on efficacy, this study closely reflects the patient baseline conditions, since telemonitoring was integrated within regular clinical practice. We consider that the complexity of the patients included in the study (which had a high mortality as shown in our previous publications [Citation26]), focussing on the comorbidity and functionality more than on specific pathologies, and the control of telemonitoring by professionals who are usually in charge of these patients, are the main strengths of the TELBIL design.
The main limitations of the present study are those inherent to before and after study designs and the lack of a control group. Another important limitation is the fact that this was an exploratory study with a small sample size. Such limitations should be taken into account when interpreting the impact observed on healthcare resources use.
We included patients coming from the preceding TELBIL RCT, monitored for 2.5 years on average previously, which could bias the results. Nevertheless, the statistical analysis applied considering the events at baseline in patients coming from the TELBIL RCT, the homogeneity analysis at baseline and the subgroup analysis carried out, counteracted this influence showing that the possible bias introduced was not substantial.
Implications for clinical practice
The present exploratory study appears to indicate the utility of a primary care-based telemonitoring intervention for complex chronic patients in reducing healthcare resources use.
Among the key factors for successful implementation of home-care telemonitoring in primary care, we highlight the positive acceptance and adherence to telemonitoring of the primary care professionals in charge of the patients, the promotion of the leading role of nursing, the institutional support for these kind of initiatives, the availability of human and material resources and the reorganization of care processes within a planned diffusion strategy. We believe that telemonitoring of complex chronic patients managed from primary care should be taken further, as the basic means to ensure coordination of the care of these patients across care levels.
Conclusion
In the light of the findings of the present exploratory study, home telemonitoring of patients with HF or CLD implemented in real clinical practice and controlled from primary care seemed to have a positive impact on healthcare resources use, reducing both all-cause and condition-specific hospitalizations and emergency department attendances, and showing a decreasing trend for the length of hospital stay.
Acknowledgements
The authors would like to thank all professionals from the Bilbao-Basurto Integrated Healthcare Organization, Santa Marina hospital and OSAREAN, who participated in this study, as well as the patients themselves and their families for their generous contribution; and to the translation service of Basque Foundation for Health Innovation and Research (BIOEF) and to Anne Sophie Denise Oter for the translation style revision of the manuscript.
Disclosure statement
The authors declare no conflict of interest. The authors alone are responsible for the content and writing of the paper.
Additional information
Funding
References
- Inglis SC, Clark RA, Dierckx R, et al. Structured telephone support or non-invasive telemonitoring for patients with heart failure. Heart. 2017;103:255–257.
- Polisena J, Tran K, Cimon K, et al. Home telemonitoring for congestive heart failure: A systematic review and meta-analysis. J Telemed Telecare. 2010;16:68–76.
- Polisena J, Tran K, Cimon K, et al. Home telehealth for chronic obstructive pulmonary disease: A systematic review and meta-analysis. J Telemed Telecare. 2010;16:120–127.
- Clarke M, Shah A, Sharma U. Systematic review of studies on telemonitoring of patients with congestive heart failure: A meta-analysis. J Telemed Telecare. 2011;17:7–14.
- Bolton CE, Waters CS, Peirce S, et al. Insufficient evidence of benefit: a systematic review of home telemonitoring for COPD. J Eval Clin Pract. 2011;17:1216–1222.
- Conway A, Inglis SC, Chang AM, et al. Not all systematic reviews are systematic: A meta-review of the quality of systematic reviews for non-invasive remote monitoring in heart failure. J Telemed Telecare. 2013;19:326–337.
- McLean S, Liu JL, Pagliari C, et al. Telehealthcare for chronic obstructive pulmonary disease: Cochrane review and meta-analysis. Br J Gen Pract. 2012;62:e739–e749.
- Kitsiou S, Paré G, Jaana M. Effects of home telemonitoring interventions on patients with chronic heart failure: An overview of systematic reviews. J Med Internet Res. 2015;17:e63.
- Kotb A, Cameron C, Hsieh S, et al. Comparative effectiveness of different forms of telemedicine for individuals with heart failure (HF): A systematic review and network meta-analysis. PLoS One. 2015;10:e0118681.
- Cruz J, Brooks D, Marques A. Home telemonitoring effectiveness in COPD: A systematic review. Int J Clin Pract. 2014;68:369–378.
- Bower P, Cartwright M, Hirani SP, et al. A comprehensive evaluation of the impact of telemonitoring in patients with long-term conditions and social care needs: Protocol for the whole system demonstrator cluster randomized trial (study protocol). BMC Health Serv Res. 2011;11:184.
- Steventon A, Bardsley M, Billings J, et al. Effect of telehealth on use of secondary care and mortality: findings from the Whole System Demonstrator cluster randomised trial. Br Med J. 2012;344:e3874.
- Purcell R, McInnes S, Halcomb EJ. Telemonitoring can assist in managing cardiovascular disease in primary care: A systematic review of systematic reviews. BMC Fam Pract. 2014;15:43.
- Martín-Lesende I, Orruño E, Bilbao A, et al. Impact of telemonitoring home care patients with heart failure or chronic lung disease from primary care on healthcare resource use (the TELBIL study randomised controlled trial). BMC Health Serv Res. 2013;13:118.
- Terschüren C, Fendrich K, van den Berg N, et al. Implementing telemonitoring in the daily routine of a GP practice in a rural setting in northern Germany. J Telemed Telecare. 2007;13:197–201.
- Martín-Lesende I, Orruño E, Cairo MC, et al. Assessment of a primary care-based telemonitoring intervention for home care patients with heart failure and chronic lung disease. The TELBIL study. BMC Health Serv Res. 2011;11:56.
- Martín-Lesende I, Recalde E, Reviriego E. Satisfaction of professionals with in-home telemonitoring of chronic patients in primary care, TELBIL-A project (in Spanish). Rev Calid Asist 2013;28:361–369.
- Orruño E, Martín-Lesende I, Mateos M, et al. Telemonitoring of pluripathological patients. Evaluation of its implementation in Primary Care (in Spanish). Ministerio de Sanidad, Servicios Sociales e Igualdad. Servicio de Evaluación de Tecnologías Sanitarias del País Vasco; 2014. Informes de Evaluación de Tecnologías Sanitarias: OSTEBA.
- Weiner JP, Starfield BH, Steinwachs DM, et al. Development and application of a population-oriented measure of ambulatory care case-mix. Med Care. 1991;29:452–472.
- Xiang R, Li L, Lio SX. Meta-analysis and meta-regression of telehealth programmes for patients with chronic heart failure. J Telemed Telecare. 2013;19:249–259.
- Chae YM, Heon Lee J, Hee Ho S, et al. Patient satisfaction with telemedicine in home health services for the elderly. Int J Med Inform. 2001;61:167–173.
- Mc Farland LV, Raugi GJ, Reiber GE. Primary care provider and imaging technician satisfaction with a teledermatology project in rural Veterans Health Administration clinics. Telemed J E Health. 2013;19:815–825.
- Glaser M, Winchell T, Plant P, et al. Provider satisfaction and patient outcomes associated with a statewide prison telemedicine program in Louisiana. Telemed J E Health. 2010;16:472–479.
- Mair F, Whitten P. Systematic review of studies of patient satisfaction with telemedicine. BMJ. 2000;320:1517–1520.
- Terschuren C, Mensing M, Mekel OCL. Is telemonitoring an option against shortage of physicians in rural regions? Attitude towards telemedical devices in the North Rhine-Westphalian health survey, Germany. BMC Health Serv Res. 2012;12:95.
- Martín-Lesende I, Recalde E, Viviane-Wunderling P, et al. Mortality in a cohort of complex patients with chronic illnesses and multimorbidity: a descriptive longitudinal study. BMC Palliat Care. 2016;15:42.
