Abstract
Background: Care transitions between general practice and hospital are hazardous regarding patient safety. For developing an improvement strategy adjusted to local settings, understanding of type and potential causes of transitional safety incidents (TSIs) is needed.
Objectives: To provide a broad overview of the nature of TSIs reported by patients and healthcare professionals.
Methods: We collected data (2011–2015) from three hospitals and 56 affiliated general practitioners (GPs) in two Dutch regions (one urban, one rural). We collected data from patients through a survey, interviews and incident reporting weeks, and from GPs and hospital specialists through incident reporting systems, surveys, interviews and focus group discussions. We classified reported TSIs according to type, cause and severity.
Results: In total, 548 TSIs were reported by 411 patients and 137 healthcare professionals; 368 of 548 TSI reports contained sufficient information for classification into aspects of the care transition process, 191 of 548 for cause, and 149 of 548 for severity. Most TSIs concerned handover correspondence from hospital to GP (26%), referral (14%) and communication/collaboration (14%). Concerning cause, reported TSIs could be attributed to organizational (48%) and human factors (43%). Twenty-four percent concerned unsafe situations, 45% near misses and 31% adverse events. Patients and healthcare professionals reported differently on referral (17% vs 9%), repeated diagnostic testing (20% vs 1%), and uncertainty about assigned responsible physician (10% vs 3%).
Conclusion: Reported TSIs typically concerned informational discontinuity. One third caused harm to the patient. Patients report different TSIs than healthcare professionals, suggesting a different view.
KEYMESSAGES
Most transitional safety incident reports concern informational discontinuity, such as missing handover correspondence from hospital to general practitioner or inadequate communication or collaboration.
One-third of the reports on transitional safety incidents were harmful for the patient.
Patients report on different transitional safety incidents than healthcare professionals, suggesting a different view on transitional patient safety.
Introduction
During the numerous transitions in healthcare between general practitioners (GPs) and hospital, patients are known to be at increased risk for safety incidents because of several hazards across the interface [Citation1–4]. Examples are inadequate transfer of medical information to the next care level, such as diagnoses, test results, or changes in medication [Citation5]. Internationally, research has shown that many transitional safety incidents (TSIs) were linked to miscommunication during the discharge process [Citation6]. Furthermore, after referral from the GP to the hospital, information needs to be up-to-date and complete to guarantee a safe transition. However, hospital specialists consider only a minority of referral letters to be adequate [Citation7]. Moreover, the electronic medical records of primary and hospital care are not linked, which impedes direct electronic information transfer between settings.
In the Netherlands, little is known either about number or nature of TSIs. While knowledge on exact incidence may spur a sense of urgency for change, understanding ‘what goes wrong’ is vital too. Indeed, profound knowledge about the content of incidents will guide future solutions and help to prioritize action. In addition, feedback to stakeholders on both parts will create a sense of urgency necessary for improvement [Citation8].
The current study is conducted within the context of the Transitional Incident Prevention Programme (TIPP) study, which aimed to evaluate a multifaceted intervention programme to prevent TSIs in the Netherlands [Citation9]. We aimed to explore type, causes and severity of TSIs as reported by Dutch patients or healthcare professionals and describe differences between patients and professionals.
Methods
We purposefully collected TSIs through different methods, as safety incident reports differ depending on source as well as reporting method [Citation10, Citation11]. Using both qualitative and quantitative methods, we collected reports on TSIs from healthcare professionals in primary and hospital care, as well as from patients.
According to literature, we defined a TSI as: ‘any unintended or unexpected event in patient care between different healthcare organizations (in our case between GP and hospital) which could have led or did lead to harm to a patient’ [Citation12]. Furthermore, we defined a transition as ‘all movements of patients or patient information between GP and hospital (that is, referral from the GP to the outpatient clinic or medical department of the hospital, discharge from the outpatient clinic or medical department of the hospital back to the GP, and simultaneous treatment by both the hospital specialist and the GP.’
Ethics
According to Dutch law, the TIPP study was exempted from formal medical ethical approval by the medical ethical committee University Medical Center Utrecht, The Netherlands (METC decision 13/142).
Setting and study population
Between 2011 and 2015 we collected data on TSIs from three hospitals and 56 affiliated general practices from two regions in the Netherlands. In the urbanized area of Utrecht, data was collected in the departments of cardiology and gastroenterology of two hospitals, the University Medical Center Utrecht and the Diakonessenhuis Utrecht. In the rural region of Hardenberg, data was collected in the departments of cardiology, gastroenterology and internal medicine of the Röpcke-Zweers Hospital.
Data collection
See for all different data sources. Current overview applied an observational approach. We collected retrospective data from the incident reporting systems in the three hospitals. In addition, we prospectively collected patient data, using the Transitional Risk and Incident Questionnaire (TRIQ), and through interviews. For healthcare professionals, we prospectively collected data through a case report form and through focus group discussions. Finally, we collected data on TSIs reported by patients or healthcare professionals in the participating hospitals and general practices during so-called ‘incident reporting weeks.’ Exclusion from analysis occurred when the incident was not related to a transition between GP and hospital. We now provide detailed information on data collection per data source.
Table 1. Flowchart of data sources and number of reported TSIs by patients and healthcare professionals.
Incident reporting systems
We retrospectively collected safety incidents that were reported through the existing internal ‘incident reporting systems’ of the participating hospitals and general practices between 2011 and 2014 and assessed whether these concerned TSIs or not.
Patient survey
Between November 2014 and January 2015, patients visiting the outpatient clinics of participating hospital departments were asked to digitally (through internet questionnaire) fill in the TRIQ questionnaire, which is a validated questionnaire developed to measure experienced TSIs as well as perceptions of patients on transitional patient safety [Citation13]. For the current overview, we only used the data collected with the TRIQ questions whether patients experienced a TSI (dimension C ‘information exchange’ (items C1, C2, C4, C6–C9) and dimension D ‘collaboration between GP and hospital physician’ (items D1–D8). We asked patients to explain the background and details of the event. The research team subsequently assessed these reported events, and classified them as TSI or not.
Patient interviews
We used a convenience sampling strategy to recruit participants that either had experienced a TSI or reported to have been at risk. Semi-structured interviews were conducted between October 2013 and June 2014. Patients were approached for the interview by their treating physician. After patients consented, they were approached by phone by a nurse to receive additional information and given an interview date. The interviews were conducted by one of three researchers (IM, LR, MM), took 36–104 min, and were taped, typed out verbatim and subsequently analysed by two researchers (IM, LR). The interviews focused on patients’ experiences during their transitional patient journey that preceded the TSI. These interviews were originally used to assess concordance with medical records, as published before [Citation12].
Case reports by GPs and hospital care professionals
In April 2014, GPs and hospital care professionals from both regions were asked via email to report one recently experienced TSI and provide additional information on the circumstances preceding the TSI, using a digital anonymous incident reporting system.
Focus group discussions of GPs and hospital specialists
We asked all GPs and hospital specialists in our two regions to participate in focus group discussions. In April and May 2014, focus group discussions were held with GPs and hospital specialists, which were taped and typed out verbatim. Key themes were individual experiences and perceptions of transitional patient safety, perceived cultural differences between primary and secondary care regarding the safety climate as well as suggestions for improvement. For the current study, we extracted the examples of TSIs brought up by participants during these discussions.
Incident reporting weeks
During two separate weeks in November 2014 and March 2015, patients and healthcare professionals were asked to report any TSIs they encountered, prospectively. Patients could report incidents on paper forms, which were available in waiting rooms of the participating general practices and outpatient clinics of hospitals. Healthcare professionals were asked to report incidents through their existing (hospital) or specially designed (GPs) electronic incident reporting system.
Classification of reported TSIs
Two researchers (MM, VS) independently classified all reported TSIs according to aspects of the transitional process in which the TSI occurred, cause and severity. In case of disagreement, the incident was discussed with three members of the research team (VS, MM, DZ) until consensus was reached.
We classified TSIs according to aspects of care transition process in an existing safety taxonomy of the World Health Organization adjusted to transitional patient safety (Supplementary Table S1) [Citation14].
If sufficient information was available, causes of reported TSIs were determined and systematically classified using the Eindhoven Classification Model (ECM) (Supplementary Table S2) [Citation15]. This method classifies root causes in five separate categories: technical, organizational, human, patient-related, and others.
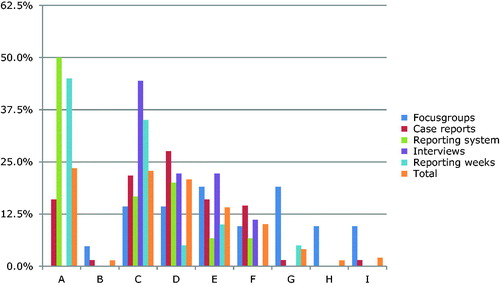
To classify the severity of harm, we used the categories of the National Coordinating Council for Medication Error Reporting and Prevention (NCC-MERP) index () [Citation16]. This index distinguishes four main categories of severity, from an unsafe situation and near miss to adverse event.
Figure 1. Classification by severity of transitional safety incidents according to NCC-MERP index. Category A: unsafe situation (no error); these concern events that have the capacity to cause error. Category B: near miss (error, no harm); an error occurred but did not reach the patient. Category C: near miss (error, no harm); an error occurred that reached the patient but no harm was caused. Category D: near miss (error, no harm); an error occurred, reached the patient and required monitoring/intervention to preclude harm. Category E: adverse event (error and harm); error that may have contributed/resulted in temporary harm and required intervention. Category F: adverse event (error and harm); error that may have contributed to or resulted in temporary harm and required initial or prolonged hospitalization. Category G: adverse event (error and harm); error that may have contributed to or resulted in permanent harm. Category H: adverse event (error and harm); error that required intervention necessary to sustain life. Category I: adverse event (error and death); error that may have contributed to or resulted in patient’s death.
Data analysis
The TSIs were extracted from the different data sources and listed. For each TSI we then determined type, causes and severity of harm, but only if enough information on the TSI was available necessary for classification. In case of doubt, we excluded the TSI from classification. Subsequently, we performed descriptive analyses for type, cause and severity per data source in SPSS. Concerning the qualitative data from the focus groups, we extracted and analysed the reported TSIs similar to other data sources.
Results
In total, 548 TSI reports were collected: 470 patients reported 411 incidents, and 233 healthcare professionals reported 137 incidents. See for numbers of TSIs per data source.
Classification of TSIs
For 368 out of 548 (67%) reported TSIs sufficient information was available for classification according to aspects of the care transition process. In particular, data from the patient survey (TRIQ) often missed sufficient information: 180 of 399 (45%) TSIs reported through TRIQ contained insufficient information for classification. The 368 TSI reports often could be classified to more than one aspect of the care transition process, resulting in 672 classifications. In total, 171 of 672 TSIs (26%, range 22–50% within different data sources) were attributed to a problem in either handover of information from hospital to GP, or vice versa in 97 of 672 TSIs (14%, range 0–19%), or failing communication/collaboration between healthcare professionals in 93 of 672 TSIs (14%, range 0–22%) ().
Table 2. Classification of 368 of 548 TSIs into aspects of the care transition process, stratified per data source.
Healthcare professionals (n = 223) reported flaws in ‘handover of correspondence to GP’ as the most frequent background of a TSI (30%), followed by flaws in ‘communication/collaboration’ (16%) and in ‘medication prescription’ (16%) (). Patients’ reported TSIs (n = 449) concerned incidents in ‘handover of correspondence to GP’ (24%) followed by ‘repeated diagnostic testing’ (20%) and ‘referral’ (17%).
Table 3. Classification of 368 of 548 TSIs into aspects of care transition process, stratified for patients and healthcare providers.
Compared to healthcare professionals, patients more often reported ‘omission of referral information’ (17% vs 9%) and ‘repeated diagnostic testing’ (20% vs 1%) (). Alternatively, healthcare professionals reported TSIs that more often concerned problems with medication (16% vs 8%).
In total, 191 of the 548 (35%) TSI reports contained sufficient information for identifying at least one cause, using the ECM criteria (). ‘Organizational factors’ (48%) and ‘human factors’ (43%) were the two most frequently identified categories for causes.
Table 4. Classification of 191 of 548 TSIs by cause according to the Eindhoven Classification Model (ECM), stratified for the different data sources.
Of the 548 TSIs, 149 (27%) could be classified according to the NCC-MERP (). In total, 35 of 149 (24%) TSI reports were classified as unsafe situations (category A), 45% as near misses (category B to D) and 31% as adverse events (categories E to I).
Different data sources revealed different severity. The focus group discussions revealed the most harmful incidents with two thirds being adverse events, as opposed to the incident reporting weeks and the reporting systems, in which half were classified as unsafe situations.
Three of 149 incidents (2%) had fatal consequences (category I), of which two were from focus group discussions and one was a case report. One concerned a hip fracture not recognized during the diagnostic process and one concerned a carcinoma diagnosed after failure of follow-up of a suspicious test result. Both regarded vulnerable patients (elderly or cognitively impaired). The third concerned a patient with a newly diagnosed abdominal aneurysm, of whom the hospital had provided no handover correspondence to the GP and when the patient presented with symptoms, those were not linked by the GP to an aneurysm and the patient died.
Discussion
Main findings
We identified a total of 548 TSIs reported by patients or healthcare professionals through seven different data sources. Correspondence and communication between hospital and GP, during referral, discharge, and simultaneous care at the outpatient hospital care were the most vulnerable aspects of the care transition process, and TSIs were mainly caused by organizational factors.
Furthermore, whereas healthcare professionals noted more medication discrepancies, patients noted redundant testing and uncertainty about the first responsible physician more frequently. Although most reported TSIs did not cause patient harm, one-third did, of which a minority with fatal consequences. Many of the reported TSIs provide opportunities for prevention of adverse health outcomes.
Strengths and limitations
Our large sample of TSIs with its rich and heterogeneous spectrum using all the different data sources, each with their own logistics and methodology, engendered some limitations. Concerning generalizability, undoubtedly the presented overview is an underrepresentation of the actual occurrence of TSIs, as underreporting of safety issues is common. For instance, patients are unlikely to report unsafe situations that they do not notice and healthcare professionals are known to underreport minor incidents [Citation17]. In addition, patients tend to be quite forgiving to their healthcare professionals because of their dependent relationship [Citation13, Citation18]. Although possibly not all types of TSIs are equally represented in our study, we believe our results provide a valid and moreover broad overview of TSIs as occurring in clinical practice and can guide future steps towards improvement. Of course, we cannot draw any conclusions on the incidence of subtypes of TSIs, as our methods were not suited for judgment on frequencies.
Additionally, often we could not classify the TSIs because of insufficient details reported. This mainly concerned patient-reported TSIs from the TRIQ survey, which should be interpreted with caution.
Notwithstanding these limitations concerning our choice of data sampling, we believe this approach was worthwhile since we optimally used information that sometimes was already available, as well as assuring this broader view as explained above.
Interpretation of study results
Inadequate information exchange between general practice and hospital was most frequently mentioned as a cause of TSIs. This is in line with the literature: a survey among 4720 physicians demonstrated that only 35% of hospital specialists always received referral information, and only 62% of GPs received handover correspondence [Citation19]. Kripalani et al. reported that in the US 51–77% of the discharge summaries were not received by GPs within four weeks [Citation5].
Interestingly, in our study, 20% of patients reported that diagnostic testing was repeated in the hospital while only 1% of healthcare professionals mentioned this. Although possibly difficult for patients to assess whether repeated testing is truly redundant, the patient is the only one present in all phases of the healthcare process. Therefore, patients might be able to reveal issues that healthcare professionals are simply unaware of [Citation10, Citation20]. Little is known on repeated diagnostic testing. One study demonstrated that a 50% reduction in redundant laboratory testing was possible with better sharing of information [Citation21]. Scrutinizing patients’ reports on redundant testing may be another fruitful source to uncover unnecessary diagnostics threatening transitional safety.
As to the causes of TSIs, we mainly identified organizational and human factors. This is in contrast to a large Dutch medical record review study, which found 43% of all in-hospital incidents were patient related, followed by 32% due to human factors [Citation22]. Smits et al. found human factors (61%) were the main cause in adverse events in the hospitalized patients, followed by 39% by patient-related factors [Citation23]. The discrepancy might be caused by the different processes involved in transitional safety as compared to in-hospital patient safety. In transitional patient safety, well-organized and documented communication within the medical record between settings is vital. Current, frequently occurring flaws can, therefore, be seen as organizational flaws, although no definite causal effect can be concluded from the current analysis. The low percentage of patient-related causal factors is probably explained by the fact that the patient often has a fairly inactive and inexplicit role in transitional patient safety [Citation24, Citation25].
Our distribution of reported TSIs was in line with the literature. Forster et al. found adverse events in 19% of the patients after discharge [Citation26]. The TSIs reported in our focus group discussions were more severe than those identified through other data sources. A focus group setting is likely to provoke discussion on events that have had a major impact on the physician. These are inherently those with severe patient harm. The same is true for the case reports. Lastly, we identified many unsafe situations that can cause harm; however, literature on these minor TSIs is scarce. Tam et al. demonstrated unsafe situations in 10–67% of patients related to incomplete medication histories on hospital admission [Citation27]. Although these unsafe situations may seem harmless and futile, they require time and effort of healthcare professionals to be corrected and may escalate to patient harm in the presence of other risk factors [Citation28].
Interpretation for clinical practice
This broad overview of different types of TSIs can be used as feedback information to assess current transitional patient safety. Results suggest TSIs are often occurring, implying urgency to improve. Our results also indicate improvement strategies should focus on exchange of information between hospitals and general practices. Other countries might benefit from our study, as most have healthcare systems where inpatient care and primary care are separate worlds [Citation29].
Conclusion
TSIs typically occur in the processes of information continuity such as discharge from hospital to general practice, referral vice versa or other communication. One-third of TSIs cause harm to the patient. Patients report different TSIs than healthcare professionals, suggesting a different view on transitional patient safety.
Acknowledgements
The authors thank all of the participating patients and healthcare providers for their reported incidents. The authors thank Vera Stegmann, Carmen Erkelens, Ineke Mol, Sofie Diepenbroek, Kate Murphy and Antoinette de Bont for their contribution in collecting data.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- https://www.cbs.nl/nl-nl/onze-diensten/methoden/onderzoeksomschrijvingen/korte-onderzoeksbeschrijvingen/ziekenhuisopnamen (in Dutch)
- Wiegers T, Hopman P, Kringos D, et al. De. Overzichtstudies: De eerste lijn. Utrecht; 2011;1:7–112.
- Vereniging VZN. Zorg Loont. Utrecht 2013;1:44–45. https://www.nvz-ziekenhuizen.nl/_library/11481/Zorg%20loont%20-%20brancherapport%202013.pdf (in Dutch)
- Coleman E, Berenson R. Lost in transition: Challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141:533–536.
- Kripalan S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians. JAMA. 2007;297:831–841.
- Williams H, Edwards A, Hibbert P, et al. Harms from discharge to primary care: mixed methods analysis of incident reports. Br J Gen Pract. 2015;65:e829–e837.
- Martinussen PE. Referral quality and the cooperation between hospital physicians and general practice: the role of physician and primary care factors. Scand J Public Health. 2013;41:874–882.
- Kotter JP, Leading Change. Boston, MA: Harvard Business Press; 1996.
- Van Melle MA, Zwart DLM, de Bont AA, et al. Improving transitional patient safety: research protocol of the transitional incident prevention programme (TIPP). Saf Health. 2015;1:13.
- Weingart SN, Pagovich O, Sands DZ, et al. What can hospitalized patients tell us about adverse events? Learning from patient-reported incidents. J Gen Intern Med. 2005;20:830–836.
- Zwart DL, Van Rensen EL, Kalkman CJ, et al. Central or local incident reporting? A comparative study in Dutch GP out-of-hours services. Br J Gen Pract. 2011;61:183–187.
- van Melle MA, Erkelens DC, van Stel HF, et al. Pilot study on identification of incidents in healthcare transitions and concordance between medical records and patient interview data. BMJ Open. 2016;6:e011368.
- Van Melle MA, van Stel HF, Poldervaart JM, et al. The Transitional Risk and Incident Questionnaire (TRIQ) was valid and reliable for measuring transitional patient safety from the patients’ perspective. J Clin Epidemiol. 2019;105:40–49.
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems. Geneva: World Health Organization; 2004;2:109.
- Van Vuuren W, Shea CE, van der Schaaf TW. The development of an incident analysis tool for the medical field. Eindhoven. 1997;1:1–25.
- NCC MERP index for categorizing medication errors algorithm. Natl Coord Counc Medicat Error Report. 2001:2001. [cited 2018 October 18]. Available from: http://www.nccmerp.org/sites/default/files/indexColor2001-06-12.pdf.
- Noble DJ, Pronovost PJ. Underreporting of patient safety incidents reduces health care’s ability to quantify and accurately measure harm reduction. J Patient Saf. 2010;6:247–250.
- Keller AC, Bergman MM, Heinzmann C, et al. The relationship between hospital patients’ ratings of quality of care and communication. Int J Qual Health Care. 2014;26:26–33.
- O’Malley AS, Reschovsky JD. Referral and consultation communication between primary care and specialist physicians: finding common ground. Arch Intern Med. 2011;171:56–65.
- Waibel S, Henao D, Aller M-B, et al. What do we know about patients’ perceptions of continuity of care? A meta-synthesis of qualitative studies. Int J Qual Health Care. 2012;24:39–48.
- Hebel E, Middleton B, Shubina M, et al. Bridging the chasm: Effect of health information exchange on volume of laboratory testing. Arch Intern Med. 2012;172:517–519.
- Langelaan M, de Bruijne MC, Baines RJ, et al. Medical record study in Dutch hospitals on patient harm due to healthcare 2011/2012 [Monitor Zorggerelateerde Schade 2011/2012. Dossieronderzoek in Nederlandse ziekenhuizen.] 2018. [cited October 16]. Available from: https://www.nivel.nl/sites/default/files/bestanden/monitor_zorggerelateerde_schade_2011_2012.pdf
- Smits M, Zegers M, Groenewegen PP, et al. Exploring the causes of adverse events in hospitals and potential prevention strategies. Qual Saf Health Care. 2010;19:e5
- Flink M, Öhlén G, Hansagi H, et al. Beliefs and experiences can influence patient participation in handover between primary and secondary care—a qualitative study of patient perspectives. BMJ Qual Saf. 2012;21:i76–i83.
- Johnson JK, Arora VM, Barach PR. European HANDOVER Research Collaborative. What can artefact analysis tell us about patient transitions between the hospital and primary care? Lessons from the HANDOVER project. Eur J Gen Pract. 2013;19:185–193.
- Forster AJ, Murff HJ, Peterson JF, et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161–167.
- Tam VC, Knowles SR, Cornish PL, et al. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ. 2005;173:510–515.
- Reason J. Human error: models and management. Bmj. 2000;320:768–770.
- Hesselink G, Vernooij-Dassen M, Pijnenborg L, et al. European HANDOVER Research Collaborative. Organizational culture: an important context for addressing and improving hospital to community patient discharge. Med Care. 2013;51:90–98.
