Abstract
Background
Undetected dementia in primary care is a global problem. Since general practitioners (GPs) act as the first step in the identification process, examining their routines could help us to enhance the currently low recognition rates.
Objectives
The study aimed to explore, for the first time in Hungary, the dementia identification practices and views of GPs.
Methods
In the context of an extensive, national survey (February-November 2014) 8% of all practicing GPs in Hungary (n = 402) filled in a self-administered questionnaire. The questions (single, multiple-choice, Likert-type) analysed in the present study explored GPs’ methods and views regarding dementia identification and their ideas about the optimal circumstances of case-finding.
Results
The vast majority of responding GPs (97%) agreed that the early recognition of dementia would enhance both the patients’ and their relatives’ well-being. When examining the possibility of dementia, most GPs (91%) relied on asking the patients general questions and only a quarter of them (24%) used formal tests, even though they were mostly satisfied with both the Clock Drawing Test (69%) and the Mini-Mental State Examination (65%). Longer consultation time was chosen as the most important facet of improvement needed for better identification of dementia in primary care (81%). Half of the GPs (49%) estimated dementia recognition rate to be lower than 30% in their practice.
Conclusions
Hungarian GPs were aware of the benefits of early recognition, but the shortage of consultation time in primary care was found to be a major constraint on efficient case-finding.
KEY MESSAGES
-
Hungarian GPs were aware of the benefits of early dementia recognition.
-
Most GPs do not use cognitive tests for case-finding.
-
Besides providing longer consultation times, the primary way to improve the efficacy of recognition would be to construct a cost- and time-effective dementia identification strategy applicable in GPs’ practices.
Introduction
General practitioners (GPs) are greatly involved in the early stages of the dementia recognition process, as most patients visit them first to have their initial cognitive examination [Citation1]. In Hungary, the estimated number of patients with dementia lies between 150,000 and 300,000 registered cases [Citation2,Citation3]. Due to the rapidly aging population, GPs in primary care are prone to see even more dementia patients in the future.
In Hungary, the dementia identification process depends on multiple professionals. Potential pathways to the identification of dementia could involve the patients’ subjective complaints and/or their family members’ reports on cognitive problems, GPs’ concerns about signs of dementia during patient consultation, targeted case-finding and population screening [Citation4]. If needed, GPs can decide to carry out basic neuropsychological tests (of which the Mini-Mental State Examination (MMSE) and the Clock Drawing Test (CDT) are financially reimbursed) and/or refer potential dementia patients to secondary care (memory clinic, psychiatry, neurology) for further investigation. Establishment of the diagnosis, identification of the etiology based on the International Classification of Diseases – 10th revision (ICD-10) and the prescription of the necessary anti-dementia medications are the tasks of psychiatrists or neurologists. After the diagnostic work-up, the specialists usually schedule patients for regular follow-up as well.
The difficulty of early dementia recognition is a global problem: research suggests that a substantial amount of dementia cases (up to 66%) is missed in primary care [Citation5]. One of the main obstacles towards effective dementia case-finding in primary care is the low use of standardised cognitive tests. Not only is dementia a taboo topic for many GPs [Citation6], some of them also experience ambivalence regarding the advantages of early diagnosis [Citation7], thinking that treatment options are limited or non-existent, while some even believe that nothing could be done for patients with dementia [Citation8].
Apart from an international study with limited sample sizes [Citation9], no extensive research has been conducted on GPs’ routines and views regarding dementia management neither in Hungary nor in many East-Central European countries. To address the lack of research, experts of two Hungarian universities collaborated on a large-scale project to examine several aspects of GPs in dementia care (see Methods section). As part of this project, the present study’s main aim was (1) to identify the methods currently being used by Hungarian GPs for the recognition of dementia; (2) to observe GPs’ satisfaction with the most widespread dementia screening tests; (3) to examine GPs’ views regarding dementia and its management and (4) to explore their ideas about an ideal test for early recognition and those optimal circumstances that could contribute to the establishment of more efficient and effective ways of dementia identification in Hungarian primary care.
Methods
Instrument
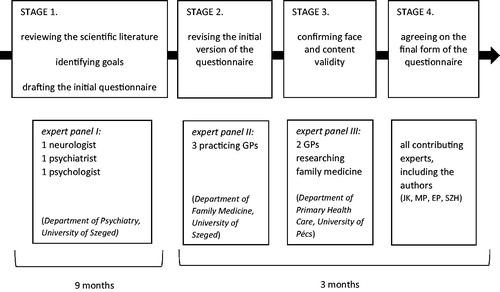
To meet the aims of the project, a self-administered questionnaire was designed specifically to explore a broad range of aspects regarding GPs’ role in dementia detection and management in Hungary. The project investigated several significant topics, including GPs’ routines and perspectives regarding dementia detection in Hungary (which is covered by the present paper); GPs' factual knowledge of dementia [Citation10] and also their attitudes regarding dementia patients and their management [Citation11]. The development and validation of the questionnaire was a multistage process, taking up one year (). The questions analysed in the present paper were fixed-response (single or multiple choice) and Likert-type questions; open-ended questions were not applied. (For the list of questions, refer Supplementary Material).
Participants and data collection
In Hungary, all practicing GPs must participate in a continuous education program, which means attending one professional training course in every 5 year period. Since our aim was to reach as many GPs as possible from every region of the country, the questionnaires were distributed at six major mandatory training courses and at three national conferences within a 10-month time frame, between February and November 2014. In order to avoid the courses’ influence on the results of the study, we selected events that did not provide any specific education about dementia during our recruitment period. Ethical approval was obtained from the Regional and Institutional Research Ethics Committee of the University of Pécs (reference number: 5244).
The questionnaires were distributed on-site among the GP-attendees at the selected trainings and conferences, along with a written informative. Participation was entirely voluntary and anonymous. Completion rate varied for each question (the questions were completed on average by 86% of the respondents); therefore, in Results, the numbers of responses are indicated in brackets for each question.
Data was analysed using the SPSS v.24 statistical analysis software package (SPSS Inc., Chicago, IL, USA). Descriptive statistics (mean, percentage, standard deviation) were applied for all items on the questionnaire. Comparative analysis was executed for one question, using the Wilcoxon signed ranks test (statistical significance was set at the 5% level).
Results
Demographic properties and practice characteristics
Altogether 402 GPs handed back their completed questionnaire, which is more than 8% of all 4,850 GPs practicing in Hungary in 2014 [Citation12]. Demographic information and characteristics of practices are presented in .
Table 1. GPs’ demographics and characteristics of practices.
Ways of dementia evaluation and views on cognitive tests
The vast majority of GPs reported that they ask the patient general questions (91%; n = 355) or they gather information from relatives (64%; n = 253). Only a quarter of them (24%; n = 95) indicated that they utilise cognitive tests and some did not perform any examinations at all to test for the possible occurrence of dementia (5%; n = 22) ().
Table 2. GPs’ ways of dementia evaluation at their practices.
Two of the most widely used tests for dementia evaluation, the MMSE and the CDT, are fairly well-known among respondents: most GPs reported that they knew CDT (89%; n = 307) and fewer people stated familiarity with MMSE (76%; n = 265). One-fifth (18%; n = 63) of the respondents said that they knew Early Mental Test, however, only a few GPs stated they were familiar with Mini-Cog (4%; n = 17) or GPCOG (1%; n = 4). More than two-thirds of respondents indicated they were (completely or mostly) satisfied with the CDT (69%; n = 152) while a slightly lower percentage of them expressed satisfaction with the MMSE (65%; n = 98) ().
Table 3. GPs’ satisfaction regarding the Mini-Mental State Examination (MMSE) and the Clock Drawing Test (CDT).
Views regarding dementia identification and management
Supporting the importance of dementia recognition in the early stages, the vast majority (90%; n = 352) believed that early therapy could slow down symptom progression. GPs also held the view (97%; n = 374) that early detection enhanced both the patients’ and their relatives’ well-being.
Regarding their views on dementia testing and managing, participants were required to mark their answers on a 5-point Likert-type scale (strongly agree/mostly agree and strongly disagree/mostly disagree responses are presented together). Three-fourths (75%; n = 290) of the GPs believed that managing dementia patients and their caregivers took more time than they could afford in their practice. Provided that conditions were suitable, the majority (79%; n = 298) would implement standardised cognitive tests for the early detection. Despite that half of the respondents (56%; n = 210) felt that currently available anti-dementia therapies were ineffective, two-thirds of them (68%; n = 255) still believed that dementia already detected in primary care would lead to more effective outcomes in therapy ().
Table 4. GPs’ views of the detection and management of dementia.
Suggestions for improvement of dementia detection: contributing factors and an optimal instrument
From a list of five contributing factors to a more effective dementia examination routine, GPs marked the items as necessary with the following percentages: more time for patients (81%; n = 311), up-to-date tests (with a maximum of 5 min needed for administration and evaluation) (77%; n = 297), help from assistants (50%; n = 192), more staff (44%; n = 170), and finally, more examination rooms (26%; n = 103). Regarding an optimal, up-to-date instrument, GPs preferred a pen-and-paper test that could be administered by an assistant or the patients themselves and would include information from the patients’ caregivers (detailed results are provided in ).
Table 5. GPs’ ideas about an optimal cognitive screening tool.
Estimated recognition of dementia
Finally, GPs were asked to estimate the recognition rate of dementia in Hungarian primary care and their practice. Regarding primary care, almost two-thirds (62%; n = 226) thought case recognition is under 30% and only very few (7%; n = 27) estimated that dementia is recognised in more than 60% of the cases. However, when asked about their recognition rate, half of them (49%; n = 180) said that they recognise a maximum of 30%, meanwhile, one-sixth (16%; n = 61) reported that they detect more than 60%. Wilcoxon signed ranks test was performed and results suggested that GPs’ estimation of their own dementia recognition rate was significantly higher than their estimations of recognition rate in primary care (Z = –7.806; p < .000).
Discussion
Main findings
Hungarian GPs are generally accepting of the idea of cognitive examinations for signs of possible dementia in primary care and more than two-thirds of them are satisfied with the most commonly used cognitive screening tests (MMSE and CDT). However, only a quarter of them uses standardised cognitive tests in their practices. GPs feel that early detection of dementia leads to more effective outcomes in therapy and serves the well-being of both patients and their families, however they remain ambivalent about the effectiveness of anti-dementia therapies. The most critical barriers towards effective dementia case-finding appear to be the insufficient conditions: mainly lack of time and quickly administrable instruments.
Interpretation of the study results
Our results revealed a discrepancy between GPs’ overall attitudes regarding testing for dementia in primary care versus their actual habits. Even though GPs seem to be aware of the benefits of timely dementia detection and they know the most commonly used cognitive tools, only a quarter of them actually apply these tests for the purpose of dementia detection, while a few do not perform any examinations at all. A similar conflict was found regarding Dutch GPs’ views and habits, who reported taking action at a more progressed stage of dementia, despite that they know the importance of early intervention [Citation13]. The rare application of formal tests has been also observed in other European studies: many (85% of French, 79% of Swiss, 53% of Italian and 33% of Scottish) GPs reported that they did not regularly perform standard procedures in their diagnostic evaluation [Citation14–17], with many preferring the use of non-standardised, general questions [Citation18]. Although there are some exceptions: 92% of Irish GPs self-reported in a survey that they used an appropriate tool to evaluate their patients’ cognition [Citation19] and only 10% of German GPs did not use any screening instrument [Citation20]. Although the trend of not performing formal tests seems to be widespread, missing data, especially from the East-Central European region only provides us with an incomplete image on the topic and raises difficulties with international comparisons.
Since Hungarian GPs seem to be ambivalent regarding the effectiveness of anti-dementia medication, their screening habits may reflect therapeutic nihilism. Some previous studies suggest so: e.g. half of the French GPs felt that it was not worth making a dementia diagnosis because of the ineffective pharmacological treatment [Citation21].
Findings of the present study indicated that the main obstacle to testing for dementia might be short consultation time with patients (which is approximately 6 min in Hungary) [Citation22]. Besides the shortage of time, GPs mentioned the need for quickly administrable cognitive tools and more help from health care staff. All of these concerns are reflected by previous studies (e.g. from the UK and the Netherlands) [Citation23,Citation24]. Despite the time restrictions, current views of scientific literature advocate for the integration of targeted case-finding approach into primary care, prompting early dementia identification [Citation4].
Cultural differences in the attitudes towards age-related memory problems may also affect the success of dementia detection. In Hungary, dementia symptoms (especially in the earlier stages) are often overlooked and thus do not prompt taking steps towards recognition. The tolerance for cognitive decline associated with older age may be higher in Hungary compared to other countries, where elderly people live far from their families and lead a more independent life (e.g. the USA) that would be greatly endangered by a mental illness.
Implications for clinical practice
The underutilisation of validated cognitive tests might be partly due to the lack of agreements on the most effective ways of dementia recognition, leaving the GPs without an unambiguous source of reference. A crucial way to improve recognition rates would be the regular update of international and national dementia guidelines (e.g. the latest Hungarian version was in effect until 2008 and is about to be updated in 2019), which usually give suggestions on the most adequate testing methods for dementia recognition.
The underuse of standardised instruments and the underdiagnoses of dementia in primary care may also be attributed to the prioritisation of somatic diseases over cognitive problems among the elderly. Since more than 65% of people over the age of 65 have multiple chronic conditions [Citation25], the examination of memory functions might end up at the bottom of the priority list [Citation8]. Furthermore, the progression of dementia is a slow process and thus is less obvious than the sudden onset of a somatic, sometimes painful complaint requiring urgent examination.
Strengths and limitations
To the best of our knowledge, this was the first Hungarian study in which GPs were questioned about their routines and views regarding dementia recognition. Our study describes results drawn from a relatively large sample (8% of all practicing GPs in Hungary), with participants from all regions of Hungary.
When interpreting the results, some limitations should be considered. First, as our findings were based on the answers of self-recruited, voluntary participants, the results might represent the views and routines of a more motivated and competent sample of Hungarian GPs. Second, given the sensitive topic of dementia detection practices, the effect of social desirability bias should also be taken into account when interpreting the results. Third, since a pen-and-paper questionnaire was applied, it could not be ensured that all 402 participants filled out all the questions, thus resulting in different numbers of missing responses throughout the survey and limiting the validity of questions with less responses. Regarding future works, it would be useful to recruit a representative sample of Hungarian GPs and also to apply qualitative methods to deepen our understanding on the topic further.
Conclusion
Although GPs in our sample seem to be aware of the benefits of dementia detection in primary care and also the concurrently low recognition rate in the country, the majority does not use formal cognitive tests for case-finding. Besides providing more favourable conditions (e.g. time and professional help), proper education and emphasising the benefits of early identification and treatment, the main way to improve the efficacy of recognition in primary care would be to construct a cost- and time-effective dementia identification strategy applicable in GPs’ practices. With sufficient help, GPs could significantly improve the rate of detected dementias in Hungary, which also corresponds with the goals of international dementia plans.
Author contributions
RB and NI analysed and interpreted all data and also wrote the manuscript. EP and SZH were members of the expert panel that designed the questionnaire and were also responsible for data collection. IK assisted with drafting and critically reviewing the manuscript. KK participated in the expert panel that designed the questionnaire and supervised the development of the paper. FH organised the data collection and also supervised the development of the paper. JK and MP were experts who participated in designing the questionnaire; they also assisted with drafting and critically reviewing the manuscript. All authors read and approved the final manuscript.
Supplemental material: List of analyzed questions
Download MS Word (18.7 KB)Acknowledgments
The authors wish to thank all participating general practitioners for their contribution.
Disclosure statement
The authors report no conflicts of interest.
Additional information
Funding
References
- Wilkinson D , Stave C , Keohane D , et al. The role of general practitioners in the diagnosis and treatment of Alzheimer's disease: a multinational survey. J Int Med Res. 2004;32(2):149–159.
- Érsek K , Kárpáti K , Kovács T , et al. A dementia epidemiológiája Magyarországon [Epidemiology of dementia in Hungary]. Ideggyogy Sz. 2010;63:175–182.
- Takacs R , Ungvari GS , Gazdag G. Demenciában szenvedő páciensek akut pszichiátriai osztályra történő felvételének okai [Reasons for acute psychiatric admission of patients with dementia]. Neuropsychopharmacol Hung. 2015;17:141–145.
- Ranson JM , Kuźma E , Hamilton W , et al. Case-finding in clinical practice: an appropriate strategy for dementia identification? Alzheimers Dement. 2018;4:288–296.
- Boustani M , Peterson B , Hanson L , et al. Screening for dementia in primary care: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2003;138(11):927–937.
- Kaduszkiewicz H , Wiese B , van den Bussche H. Self-reported competence, attitude and approach of physicians towards patients with dementia in ambulatory care: results of a postal survey. BMC Health Serv Res. 2008;8.
- Hansen EC , Hughes C , Routley G , et al. General practitioners' experiences and understandings of diagnosing dementia: factors impacting on early diagnosis. Soc Sci Med. 2008;67(11):1776–1783.
- Boise L , Camicioli R , Morgan DL , et al. Diagnosing dementia: perspectives of primary care physicians. Gerontologist. 1999;39(4):457–464.
- Petrazzuoli F , Vinker S , Koskela TH , et al. Exploring dementia management attitudes in primary care: a key informant survey to primary care physicians in 25 European countries. Int Psychogeriatr. 2017;29(9):1413–1423.
- Imre N , Balogh R , Papp E , et al. Knowledge of general practitioners on dementia and mild cognitive impairment: a cross-sectional, questionnaire study from Hungary. Educ Gerontol. 2019;45(8):495–505.
- Heim S , Busa C , Pozsgai É , et al. Hungarian general practitioners' attitude and the role of education in dementia care. Prim Health Care Res Dev. 2019;20(e92):1–6.
- Hungarian Central Statistical Office . Number of practicing general practitioners in Hungary (2007–2017). [Data base]. [cited 2019 Sept 25]. Available from: http://statinfo.ksh.hu/Statinfo/index.jsp.
- Van Hout H , Vernooij-Dassen M , Bakker K , et al. General practitioners on dementia: task, practices and obstacles. Patient Educ Couns. 2000;39(2-3):219–225.
- Giezendanner S , Monsch AU , Kressig RW , et al. Early diagnosis and management of dementia in general practice – how do Swiss GPs meet the challenge? Swiss Med Wkly. 2018;148:w14695.
- McIntosh IB , Swanson V , Power KG , et al. General practitioners’ and nurses’ perceived roles, attitudes and stressors in the management of people with dementia. Health Bull. 1999;57(1):35–43.
- Somme D , Gautier A , Pin S , et al. General practitioner’s clinical practices, difficulties and educational needs to manage Alzheimer’s disease in France: analysis of national telephone-inquiry data. BMC Fam Pract. 2013;14(1):81.
- Veneziani F , Panza F , Solfrizzi V , et al. Examination of level of knowledge in Italian general practitioners attending an education session on diagnosis and management of the early stage of Alzheimer's disease: pass or fail? Int Psychogeriatr. 2016;28(7):1111–1124.
- Allen M , Ferrier S , Sargeant J , et al. Alzheimer’s disease and other dementias: an organizational approach to identifying and addressing practices and learning needs of family physicians. Educ Gerontol. 2005;31(7):521–529.
- Dyer AH , Foley T , O’Shea B , et al. Dementia diagnosis and referral in general practice: a representative survey of Irish general practitioners. Irish Med J. 2018;111(4):735.
- Thyrian JR , Hoffmann W. Dementia care and general physicians – a survey on prevalence, means, attitudes and recommendations. Cent Eur J Public Health. 2012;20(4):270–275.
- Harmand M-C , Meillon C , Rullier L , et al. Description of general practitioners’ practices when suspecting cognitive impairment. Recourse to care in dementia (Recaredem) study. Aging Ment Health. 2018;22(8):1046–1055.
- Irving G , Neves AL , Dambha-Miller H , et al. International variations in primary care physician consultation time: a systematic review of 67 countries. BMJ Open. 2017;7(10):e017902.
- Chithiramohan A , Iliffe S , Khattak I. Identifying barriers to diagnosing dementia following incentivisation and policy pressures: general practitioners’ perspectives. Dementia (London). 2019;18(2):514–529.
- Prins A , Hemke F , Pols J , et al. Diagnosing dementia in Dutch general practice: a qualitative study of GPs’ practices and views. Br J Gen Pract. 2016;66(647):e416–e422.
- Lehnert T , Heider D , Leicht H , et al. Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev. 2011;68(4):387–420.