Abstract
Background
The implementation of eHealth applications in primary care remains challenging. Enhancing knowledge and awareness of implementation determinants is critical to build evidence-based implementation strategies and optimise uptake and sustainability.
Objectives
We consider how evidence-based implementation strategies can be built to support eHealth implementation.
Discussion
What implementation strategies to consider depends on (potential) barriers and facilitators to eHealth implementation in a given situation. Therefore, we first discuss key barriers and facilitators following the five domains of the Consolidated Framework for Implementation Research (CFIR). Cost is identified as a critical barrier to eHealth implementation. Privacy, security problems, and a lack of recognised standards for eHealth applications also hinder implementation. Engagement of key stakeholders in the implementation process, planning the implementation of the intervention, and the availability of training and support are important facilitators. To support care professionals and researchers, we provide a stepwise approach to develop and apply evidence-based implementation strategies for eHealth in primary care. It includes the following steps: (1) specify the eHealth application, (2) define problem, (3) specify desired implementation behaviour, and (4) choose and (5) evaluate the implementation strategy. To improve the fit of the implementation strategy with the setting, the stepwise approach considers the phase of the implementation process and the specific context.
Conclusion
Applying an approach, as provided here, may help to improve the implementation of eHealth applications in primary care.
eHealth in primary care
KEY MESSAGES
-
To successfully implement eHealth in primary care, context-specific implementation strategies are essential.
-
Identifying potential barriers (e.g. costs) and facilitators (e.g. support) to eHealth implementation is necessary to develop the right implementation strategy.
-
The provided tool helps to define the implementation problem and desired implementation behaviour and develop evidence-based implementation strategies.
This background paper discusses the implementation of eHealth in primary care. The primary purpose of this paper is to discuss strategies to optimise the implementation of eHealth and to provide a practical, step-by-step approach to develop evidence-based implementation strategies that fit the specific context. What implementation strategies to consider, however, depends on (potential) barriers and facilitators in a given situation. Therefore, after an introduction on the implementation of eHealth interventions in primary care, we give a brief overview of key barriers and facilitators to eHealth implementation. Knowing what potential barriers and facilitators can be at play, could help researchers, clinicians, and policymakers develop the right implementation strategy.
Implementation of interventions in primary care
A translational gap between research and practice exists, meaning that proven effective healthcare innovations often do not reach practice or only after a significant length of time. Moreover, the implementation of new interventions into healthcare is not always successful [Citation8]. This is alarming as it can affect the quality of care being delivered [Citation8]; it may, for example, harm the effectiveness and safety of healthcare. This highlights that there is room for improvement. Implementation research is specifically focussed on methods to promote the uptake of research findings and other evidence-based practices into routine practice and thereby aims to improve the quality of healthcare [Citation9].
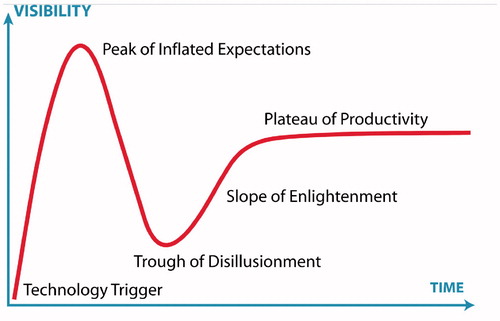
The hype cycle of Gartner can be used to determine at what stage of uptake an eHealth application is at any given point in time [Citation10]. As shown in , the visibility or use of technological innovation rapidly increases after the introduction because of inflated expectations about the innovation. Next, there is a decline in uptake as the real-world challenges with the implementation come to light (i.e. Trough of Disillusionment). When, at this stage, the shortcomings or obstacles to successful implementation are addressed, the uptake of the innovation can be boosted (i.e. Slope of Enlightenment) and reach a stable level. As mentioned in the first article of this series [Citation6], it is essential to take the interaction between end-user demands, technology, and context into account to sustain the use of the eHealth innovation.
Figure 1. Hype cycle of Gartner. Source: https://en.wikipedia.org/wiki/Hype_cycle.
The success rate of eHealth implementation is unknown; however, many examples of eHealth implementation failures have been described [Citation11]. Next to the translational gap between research and practice, there also seems to be an evidence gap. Many new eHealth applications are not yet investigated on effectiveness [Citation6,Citation12]. For example, a scoping review on eHealth applications for people with COPD showed that most eHealth applications were not thoroughly investigated on effectiveness [Citation13]. The evidence of effectiveness is, however, a basic requirement for implementation [Citation14,Citation15]. The phase between adopting an eHealth application and the routine use of the application is multidimensional and complex [Citation15]. It is therefore vital to gain knowledge on which factors impact eHealth implementation, and how we can effectively target these factors. Several different barriers and facilitators that can influence the implementation success have been identified. The framework for non-adoption, abandonment, scale-up, spread and sustainability (NASSS) of healthcare technologies posits that the implementation of eHealth applications will only succeed when the different interacting domains are acknowledged and addressed (e.g. characteristics of the technology, end-user, organisation and outer setting) [Citation16]. When effective eHealth applications are successfully implemented in routine care, this may benefit the quality of healthcare.
An implementation framework
The Consolidated Framework for Implementation Research (CFIR) is widely used to categorise barriers and facilitators to implementation [Citation17]. The CFIR is a theory-driven model and comprises five domains: (1) the intervention characteristics, (2) the outer setting, (3) the inner setting, (4) the characteristics of the individuals involved in the intervention, and (5) the implementation process. In Supplementary Appendix 1, we describe each domain and list critical barriers and facilitators to eHealth implementation that were reported in the literature and give examples of how barriers and facilitators can affect the implementation of eHealth. The appendix does not provide an exhaustive list of all potential barriers and facilitators but offers insight into the most essential and changeable implementation factors. This inventory will help to determine what obstacles need to be overcome and how we might optimise eHealth implementation in primary care. It is important to realise that certain factors can be considered both a facilitator and a barrier. For example, financial costs are frequently mentioned as a factor affecting eHealth implementation [e.g. Citation15,Citation18,Citation19,Citation20]. When there are high costs and there is no or limited funding, financial cost is a barrier; however, low costs and the availability of funding can be considered a facilitator. presents an overview of the domains and the key factors influencing eHealth implementation.
Implementation strategies
To enable the successful implementation of eHealth applications in practice, the correct implementation strategies must be chosen. Implementation strategies refer to the ‘methods or techniques used to enhance the adoption, implementation, and sustainability of a clinical programme or practice’ [Citation21]. A comprehensive list of 73 implementation strategies is provided by Powell et al. [Citation22] (e.g. promote adaptability, centralise technical assistance, identify and prepare champions). Strategies can be used individually or combined into a multi-component implementation approach, which allows users to target the different relevant domains simultaneously (e.g. organisational, individual, or policy level). When choosing implementation strategies, it is crucial to ensure that they fit the phase of the implementation process (i.e. adoption phase vs implementation phase) and the specific context (e.g. characteristics of the GP practice and stakeholders involved). More specific, certain implementation strategies may be better suited for the adoption phase of implementation (e.g. developing a formal implementation blueprint). In contrast, other strategies can better be applied when implementation has already started (e.g. identifying early adopters).
To facilitate healthcare professionals and researchers who are in the process of implementing an eHealth intervention, we have provided a practical worksheet to effectively target expected or experienced barriers and facilitators (Supplementary Appendix 2; ). The worksheet is based on the Action, Actor, Context, Target, Time (i.e. AACTT) framework, which helps to specify what behaviour needs to change and how to define this particular behaviour [Citation23]. The worksheet contains the following steps: (1) specify the eHealth application, (2) define the problem, (3) specify the desired implementation behaviour, i.e. describe ‘who does what; to, for or with whom; when; where?’ [Citation23], (4) choose the implementation strategy from the overview provided by Powell et al. [Citation22], and (5) evaluate the implementation strategy. A description of each step is given in and examples are given in Supplementary Appendix 2. The barriers and facilitators to eHealth implementation that are described in Supplementary Appendix 1 may be used to fill in the worksheet. More specifically, the determinants may be used to help define the problem in step 2 of the worksheet and they may guide the choice of the implementation strategy in step 4. For example, a problem may be that professionals were not adequately trained to work with a new eHealth application (see domain 3: Inner setting). Conducting ongoing training may be an implementation strategy to help overcome this problem. The worksheet can be a practical tool to facilitate the development and application of evidence-based implementation strategies. The worksheet takes into account the phase of the implementation process and the specific context in which the eHealth application is implemented, and this may improve the fit of the implementation strategy with the setting. Besides developing evidence-based implementation strategies, it is important to be aware of the ethical implications of the implementation of eHealth in primary care (e.g. questions related to roles and responsibilities). This topic is further discussed in the second article of this series [Citation24].
Table 1. A stepwise tool to build an evidence-based implementation strategy.
Conclusion
The implementation of eHealth applications in primary care is challenging. Broadening knowledge on barriers and facilitators that influence the implementation of eHealth applications is essential to promote successful uptake and maintenance. Cost, privacy, security problems, and a lack of recognised standards for eHealth applications were identified as important barriers, whereas engaging stakeholders, planning the implementation, and the availability of training and support were considered facilitators. To allow eHealth applications to be successfully implemented, it is important that context-specific implementation strategies are applied that are in line with the phase of the implementation process. The step-by-step worksheet provided may help researchers and healthcare professionals who are implementing an eHealth application, to develop and apply evidence-based implementation strategies.
Supplemental Material - Appendix 1
Download PDF (180.9 KB)Supplemental Material - Appendix 2
Download PDF (268.3 KB)Acknowledgements
The following individuals, working at the department of Public Health and Primary Care of the Leiden University Medical Center, contributed to the manuscript: Jiska J. Aardoom, Marise J. Kasteleyn, Tobias N. Bonten, Frederike L. Büchner, Isa E.J.F. Houwink, Esther P.W.A. Talboom-Kamp, Jens H. van Dalfsen, Annelieke H.J. Petrus, and Sanne C. van Kampen.
Disclosure statement
David Mohr has accepted consulting fees and honoraria from Apple Inc, Otsuka Pharmaceuticals, the One Mind Foundation, and has an ownership interest in Adaptive Health, Inc. The other authors declare no conflict of interest.
Additional information
Funding
References
- Fisher RF , Croxson CH , Ashdown HF , et al. GP views on strategies to cope with increasing workload: a qualitative interview study. Br J Gen Pract. 2017;67:e148–e156.
- Eysenbach G. What is e-health? J Med Internet Res. 2001;3:e20.
- Meier CA , Fitzgerald MC , Smith JM. eHealth: extending, enhancing, and evolving health care. Annu Rev Biomed Eng. 2013;15:359–382.
- Anderson JG , Balas EA. Computerization of primary care in the United States. Int J Healthc Inf Syst Inform. 2006;1:1–23.
- Tan SSL , Goonawardene N. Internet health information seeking and the patient-physician relationship: a systematic review. J Med Internet Res. 2017;19:e9.
- van der Kleij RM , Kasteleyn MJ , Meijer E , et al. SERIES: eHealth in primary care. Part 1: Concepts, conditions and challenges. Eur J Gen Pract. 2019;25:179–189.
- Shaw T , McGregor D , Brunner M , et al. What is eHealth (6)? Development of a conceptual model for eHealth: qualitative study with key informants. J Med Internet Res. 2017;19:e324.
- Eccles M , Grimshaw J , Walker A , et al. Changing the behavior of healthcare professionals: the use of theory in promoting the uptake of research findings. J Clin Epidemiol. 2005;58:107–112.
- Eccles MP , Mittman BS. Welcome to implementation science. Implementation Sci. 2006;1:3.
- Dedehayir O , Steinert M. The hype cycle model: a review and future directions. Technol Forecast Soc Change. 2016;108:28–41.
- Berg M. Patient care information systems and health care work: a sociotechnical approach. Int J Med Inform. 1999;55:87–101.
- Black AD , Car J , Pagliari C , et al. The impact of eHealth on the quality and safety of health care: a systematic overview. PLoS Med. 2011;8:e1000387.
- Hallensleben C , van Luenen S , Rolink E , et al. eHealth for people with COPD in the Netherlands: a scoping review. Int J Chron Obstruct Pulmon Dis. 2019;14:1681.
- Mair FS , May C , O'Donnell C , et al. Factors that promote or inhibit the implementation of e-health systems: an explanatory systematic review. Bull World Health Organ. 2012;90:357–364.
- Ross J , Stevenson F , Lau R , et al. Factors that influence the implementation of e-health: a systematic review of systematic reviews (an update). Implement Sci. 2016;11:146.
- Greenhalgh T , Wherton J , Papoutsi C , et al. Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J Med Internet Res. 2017;19:e367.
- Damschroder LJ , Aron DC , Keith RE , et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50.
- Anderson JG. Social, ethical and legal barriers to e-health. Int J Med Inform. 2007;76:480–483.
- Peeters JM , Krijgsman JW , Brabers AE , et al. Use and uptake of eHealth in general practice: a cross-sectional survey and focus group study among health care users and general practitioners. JMIR Med Inform. 2016;4:e11.
- Granja C , Janssen W , Johansen MA. Factors determining the success and failure of eHealth interventions: systematic review of the literature. J Med Internet Res. 2018;20:e10235.
- Proctor EK , Powell BJ , McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci. 2013;8:139.
- Powell BJ , Waltz TJ , Chinman MJ , et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10:21.
- Presseau J , McCleary N , Lorencatto F , et al. Action, actor, context, target, time (AACTT): A framework for specifying behaviour. Implement Sci. 2019;14:102.
- Boers SN , Jongsma KR , Lucivero F , et al. SERIES: eHealth in primary care. Part 2: exploring the ethical implications of its application in primary care practice. Eur J Gen Pract. 2020;26:26–32.

