Abstract
Background
Direct access to hospital radiology facilities by general practitioner (GP) cooperatives is known to decrease the number of emergency department referrals, but the effects on length of stay (LOS; time from patient arrival at GP cooperative till departure to home) and patient experiences are unclear.
Objectives
To provide insight into the LOS and experiences of trauma patients with an indication for radiology at GP cooperatives with and without access to radiology.
Methods
A multi-methods observational study in April 2014–October 2015 at six GP cooperatives in The Netherlands, covering three organisational models for access to radiology: no direct access, limited access and unlimited access. Patient experiences were measured with a questionnaire. Patient records were analysed for background characteristics, radiology outcomes, referral and LOS.
Results
In total 657 patients were included, 232 no direct access model, 307 limited access model and 118 unlimited access model. The mean LOS was 99 minutes, with a significant difference between GP cooperatives without access to radiology (121 minutes), with limited access (86 minutes), and with unlimited access (90 minutes). The differences were larger for patients without radiological abnormalities. On a ten-point scale, patients rated GP cooperatives with unlimited access to radiology higher (8.62) than those without access (8.36) or with limited access (8.39).
Conclusion
Access to radiology by GP cooperatives seems to reduce the length of stay and is slightly more appreciated by patients. GP cooperatives with unlimited access seem to provide the most efficient and best-valued care, contributing to more patient-centred care.
KEY MESSAGES
Direct access to radiology by the GP cooperative reduces the total LOS of trauma patients who require conventional radiology imaging.
Patients slightly more appreciate GP cooperatives with unlimited access to radiology than those without or with limited access (in restricted time frames).
Introduction
There are various organisational models for out-of-hours primary care in Europe, of which the general practitioner (GP) cooperative is predominant [Citation1]. In these large-scale organisations, GPs take turns being on duty during out of hours for the patient populations of all participating GPs (15–250 GPs per cooperative). In The Netherlands, GP cooperatives are increasingly located on the site of hospital emergency departments (EDs), which creates possibilities for collaboration [Citation2,Citation3]. An example is the triage and treatment of self-referring patients by the GP cooperative instead of the ED [Citation3]. Another possibility is direct access to hospital diagnostics, such as radiology. GPs are often consulted for musculoskeletal trauma, in which conventional radiology may help rule out a fracture or luxation [Citation4]. In The Netherlands, during office hours the GP in the general practice has direct access to the radiology facilities of the hospital. Only in case of radiological abnormalities does the patient receive a referral to the ED; otherwise further treatment is offered by the GP in the general practice. However, during out of hours, patients often need to be referred to the ED, as GP cooperatives often do not have access to conventional radiology facilities [Citation5–7]. A lack of access to hospital diagnostics causes unnecessary contacts with EDs, which are already struggling with overcrowding [Citation8–10]. Moreover, the contribution from the patient’s annual deductible is higher and the total length of stay (LOS) is possibly longer [Citation11,Citation12]. Longer waiting times have been associated with lower patient satisfaction [Citation13].
In past years, several GP cooperatives in The Netherlands have gained direct access to the hospital’s radiology facilities, without the need to refer patients to the ED [Citation5]. Mostly, the access is limited to certain time frames [Citation5,Citation6]. Previous studies into access to radiology by GP cooperatives in The Netherlands have shown that GPs used the radiology facilities adequately [Citation6], more patients were maintained under treatment of the GP [Citation6] and the total number of ED contacts was reduced by 4.5% [Citation7]. It might also positively influence patient satisfaction and LOS. These are indicators of patient centredness, one of the six domains of quality of care [Citation14]. This study aimed to examine the effects of different organisational models of radiology access by the GP cooperative on patient experiences and LOS. We hypothesised that GP cooperatives with unlimited access to radiology would have higher patient satisfaction and shorter LOS than GP cooperatives with limited access (in restricted time frames) and without direct access to radiology.
Methods
Study design and population
We performed an observational study combining patient registration analysis with a survey among trauma patients referred by the GP cooperative for conventional radiology (X-ray) in April 2014–October 2015. The study was carried out in a convenience sample of six GP cooperatives covering three organisational models: one with unlimited access, three with limited access (in restricted time frames) and two without direct access to radiology. The study period in each GP cooperative varied from 3 to 5 months ().
Table 1. Models of access of GP cooperatives to radiology in The Netherlands, study period and background information.
Selection of study subjects
In all three models, all patients with trauma in which the GP and patient decided to take an X-ray were eligible for inclusion. There were no exclusion criteria. The GP informed the patients about the study and asked them to sign an informed consent form.
Procedure
After the GP consultation, included patients were directed to the GP cooperative desk, where a study number was assigned to them. This number was written on the informed consent form and patient questionnaire. Patients were requested to return the form and questionnaire at the GP cooperative desk directly after their treatment. The desk assistant listed the time of emission and return of the questionnaire on the questionnaire form. The informed consent form, the (anonymous) patient questionnaire and study number list with personal data were stored separately by the desk assistant. Forms returned outside the GP cooperative opening hours could be dropped in a closed post box or returned by post addressed to the GP cooperative.
Measurements
The patient questionnaire measured patient experiences with the provided care using a 4-point scale of agreement (1 = not at all; 2 = a little; 3 = largely; 4 = totally) or ten-point scale of quality (1 = very bad; 10 = excellent). The questionnaire was based on the Consumer Quality Index (CQI) [Citation15]. Two questions about the experienced collaboration between GP cooperative and ED were added and filled in only by patients referred to the ED. The questionnaire consisted of 21 questions, which could be answered in less than 5 minutes.
To examine LOS we used the time of start of the consultation at the GP cooperative as registered in the patient record as starting point (A). The questionnaire and informed consent form were handed over to the patient after the GP cooperative consultation (B). The time of return of the questionnaire was used as the endpoint for LOS (C). Questionnaires returned by post or post box (16%) were not used in the LOS analysis.
Data extraction
Routinely registered data were extracted from the GP cooperatives’ electronic registration systems, including age, gender, affected body part, and referral to the ED. The imaging report of the radiologist was obtained from the hospital administration system. For patients who were referred to the ED, the ED file was obtained as well, to verify the diagnosis.
Statistical analyses
Descriptive statistics were used to describe the patient population. Patient characteristics, LOS and patient experiences for the three models were compared with T-tests and chi-square tests. To calculate percentages of agreement on the items measuring patient experiences, the four-point answering scale was dichotomised into agree (‘largely’ plus ‘totally’) and not agree (‘not at all’ plus ‘a little’). Testing, however, was performed on the total scale. The LOS and perceived problems with LOS were calculated for the subgroups of patients with and without radiological abnormalities. For all data analyses IBM SPSS 22 (Statistical Package for Social Sciences) was used. P values less than 0.05 were considered statistically significant.
Ethics
The Ethical Research Committee of the Radboud University Medical Centre Nijmegen was consulted and concluded that this study does not fall within the remit of the Dutch Medical Research Involving Human Subjects Act [Wet Mensgebonden Onderzoek] (2014/219].
Results
Patient characteristics
We included 657 trauma patients within the three organisational varieties for accessibility to conventional radiology (X-ray) by the GP cooperative: 232 patients (35%) in the model without access, 307 patients (47%) in the model with limited access and 118 (18%) in the model with unlimited access (). The mean age was 31.3 years and 55.5% were women. Most injuries concerned extremities (91.0%). The population was similar within the three organisational models regarding age and gender, but differed in the percentage of wrist and foot/toe injuries ().
Figure 1. Patient flow chart per organisational model for general practitioner cooperative access to radiology: no access, limited access (in restricted time frames) and unlimited access (all opening hours). (A) Appointment time of the patient at the GPC (start point). (B) Issue of questionnaire and informed consent form to the patient. (C) Return of questionnaire and informed consent form (endpoint).
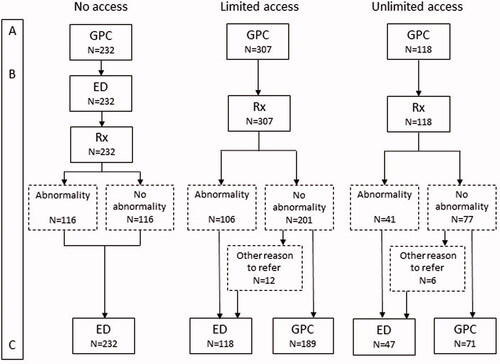
Table 2. Patient characteristics per organisational model with respect to access to radiology by the GP cooperative.
In total, 40.4% of the patients were diagnosed as having a fracture or luxation (N = 263). The outcomes differed significantly between the model without access and models with (limited) access. The percentage of radiological abnormalities (fractures and luxations) was 51.3% in the model without access to radiology, 34.5% in the model with limited access and 34.7% in the model with unlimited access. The ED referral rate for GP cooperatives without access to radiology was (logically) 100%, compared to 38.4% in the case of limited access and 39.8% in unlimited access ().
Length of stay
The mean total LOS for all included patients was 99 minutes. The total LOS in the model without direct access to radiology (121 minutes) differed significantly from the models with limited access (86 minutes) and unlimited access (90 minutes). The difference between the models in mean LOS was the largest for patients without radiological abnormalities. In the model without direct access these patients had to visit the ED and their mean total LOS was 112 minutes. In the (un)limited access models, patients without radiological abnormalities maintained under treatment of the GP cooperative; their mean total LOS was 70 minutes in the limited access model and 63 minutes in the unlimited access model ().
Table 3. Length of stay (in minutes) and patient experiences within the different organisational models with respect to access to radiology by the GP cooperative.
Patient experiences
About half of the total population (47.9%) considered the LOS as problematic. In the models with (un)limited access, patients without radiological abnormalities considered the LOS less often as a problem (38.1% limited access model; 45.8% unlimited access model) than patients who had to visit the ED because of radiological abnormalities (52.0% limited access model; 61.5% unlimited access model). In the model without direct access, there was almost no difference in perceived problems with LOS between patients with and without radiological abnormalities (53.2 vs 51.9%) ().
The mean grade (on a ten-point scale) for care at the GP cooperative was 8.42 (n = 644). For patients who visited the ED the mean grade for care was 8.11 (n = 343). The mean grade for the collaboration between ED and GP cooperative was 7.91 (n = 240, only ED referred patients). The GP cooperative with unlimited access obtained a significantly higher grade (8.62) than GP cooperatives without access (8.36) or with limited access (8.39). Only in the model with unlimited access did none of the respondents give the GP cooperative a grade below 6 (). We did not find a correlation between LOS and patient satisfaction (data not shown).
Most patients indicated that they felt taken seriously by the professionals (GP cooperative 98% and ED 98.3%) and that they had confidence in the medical expertise (GP cooperative 98.6% and ED 98.8%). According to the patients, professionals at the GP cooperative and ED had sufficient time (GP cooperative 98.6% and ED 95.4%) ().
Discussion
Main findings
Our study shows that access to conventional radiology by the GP cooperative is related to a shorter LOS, particularly for patients without radiological abnormalities. The patients were overall satisfied with the delivered care by the GP cooperative, ED and their collaboration. The GP cooperative with unlimited access to radiology had higher satisfaction ratings than those with limited or without access. Patients felt taken seriously and had confidence in the expertise of the professionals working at the GP cooperative and ED.
Strengths and limitations
To our knowledge, this study is the first to investigate the effects of access to radiology by the GP cooperative on LOS and patient satisfaction. It supplements a previously published study of the impacts on referrals [Citation6]. The study was performed in 2014–2015. Since then, more GP cooperatives have gained direct access to radiological facilities. However, we do not believe that repeating the study now would provide other results.
We could not perform an experimental study, but investigated the current situation in a convenience sample of six GP cooperatives. The number of GP cooperatives varied from only one to three per model. Due to the study design, we were not able to demonstrate causal relationships. Organisational differences between the GP cooperatives could have influenced the results. Moreover, the sampling method limits the generalisability of the results to other regions and countries.
The total number of selected patients was not recorded, making it impossible to calculate a response rate. Selection bias could have occurred because patients admitted to the hospital possibly did not return their questionnaires and forms. Furthermore, 16% of all patients were lost to analysis in the calculation of the LOS. For these patients we did not know a LOS endpoint because they returned their questionnaire by post (box). The patient characteristics of these patients were similar to the total study population. We do not believe this loss of patients has influenced the results.
Finally, the time to fill out the questionnaire (less than 5 minutes) was included in the LOS because we used the time of return of the questionnaire as the endpoint of care. The LOS is, therefore, somewhat overestimated. However, this applied to all three models equally, so it has not influenced our comparative analyses.
Interpretation of the study results in relation to existing literature
Thijssen et al. [Citation12] examined the LOS of patients at the ED in The Netherlands and found a mean of 130 minutes per ED visit, which is relatively low compared to other western countries (176–480 minutes). For trauma patients, they reported a mean ED LOS of 91 minutes [Citation12]. In our study, the mean LOS for patients attending both the GP cooperative and ED was 120 minutes in total. The difference in LOS of 29 minutes is understandable because our study included the GP cooperative visit, radiological diagnostic examination and evaluation, ED visit and possible waiting times in between. Despite the relatively short LOS, almost half of the patients in our study considered this problematic.
The patients in our study highly appreciated the care at the GP cooperative and ED in general (mean grades 8.4 and 8.1, respectively). This aligns with previous Dutch patient satisfaction studies at the GP cooperative [Citation16,Citation17] and ED [Citation18]. It has been found that the strongest predictor of ED patient satisfaction is how satisfied the patient is with interpersonal interactions with ED physicians and nurses [Citation13]. Interactions of patients with healthcare providers have not been examined in our study. However, patients reported they felt taken seriously and had high confidence in the expertise of the professionals. This most likely has had positive effects on the relatively high satisfaction grades reported in our study. Waiting time has also been revealed as an important predictor for satisfaction: if these are longer than what patients expect or deem appropriate, dissatisfaction is likely to arise [Citation18]. We did not find any correlation between LOS and patient satisfaction.
Implications for practice and further research
Crowding of EDs is a problem in many western countries [Citation8–10]. Multiple factors have been associated with ED crowding, of which non-urgent ED visits are frequently mentioned. Some of these non-urgent visits are made by self-referred patients presenting at the ED rather than in primary care [Citation19–22]. Increasingly, GP cooperatives and EDs are co-locating and collaborating, giving opportunities to redirect the self-referred patients from ED to GP cooperative [Citation2]. The GP cooperative can safely treat 76% of the redirected self-referrals [Citation2]. The referral rate could be further reduced by giving the GP cooperative access to radiology, which is standard during daytime. GPs with access to radiology use the diagnostics in a restrained way and cause a reduction in ED referrals [Citation5,Citation6]. A reduction of 4.5% of the total ED attendance has been shown even in limited access to radiology [Citation7].
Access to radiology by the GP cooperative should be considered to provide efficient and patient-centred care and to prevent non-urgent care at the ED. On the other hand, initiatives to redirect low-complex care from the ED to primary care settings increase workload. It is advisable to invest in primary care setting to keep this redirection sustainable.
Conclusion
This study shows that access to conventional radiology (X-ray) by the GP cooperative is related to a lower mean LOS and is slightly more highly valued by patients. GP cooperatives with unlimited access seem to provide the most efficient and best-valued care, contributing to patient-centred care.
Disclosure statement
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the paper.
Additional information
Funding
References
- Steeman L, Uijen M, Plat E, et al. Out-of-hours primary care in 26 European countries: an overview of organizational models. Fam Pract. 2020;37(6):744–747.
- Smits M, Rutten M, Keizer E, et al. The development and performance of after-hours primary care in The Netherlands: a narrative review. Ann Intern Med. 2017;166(10):737–742.
- Rutten M, Vrielink F, Smits M, et al. Patient and care characteristics of self-referrals treated by the general practitioner cooperative at emergency-care-access-points in The Netherlands. BMC Fam Pract. 2017;18(1):62.
- Van de Lisdonk EH. Ziekten in de huisartsenpraktijk. [Diseases in General Practice]. Utrecht: Bunge; 2008:380. Dutch.
- Schols AMR, Stevens F, Zeijen CGIP, et al. Access to diagnostic tests during GP out-of-hours care: a cross-sectional study of all GP out-of-hours services in The Netherlands. Eur J Gen Pract. 2016;22(3):176–181.
- Rutten M, Smits M, Peters Y, et al. Effects of access to radiology in out-of-hours primary care in The Netherlands: a prospective observational study. Fam Pract. 2018;35(3):253–258.
- Van den Bersselaar DLCM, Maas M, Thijssen WAMH. Does X-ray imaging by GPC at emergency care access points in the Netherlands change patient flow and reduce ED crowding? A cohort study . Health Sci Rep. 2018;1(2):e26.
- Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52(2):126–136.
- van der Linden C, Reijnen R, Derlet RW, et al. Emergency department crowding in The Netherlands: managers' experiences. Int J Emerg Med. 2013;6(1):41.
- Ramlakhan S, Mason S, O'Keeffe C, et al. Primary care services located with EDs: a review of effectiveness. Emerg Med J. 2016;33(7):495–503.
- Thijssen WA, Wijnen-van Houts M, Koetsenruijter J, et al. The impact on emergency department utilization and patient flows after integrating with a general practitioner cooperative: an observational study. Emerg Med Int. 2013;2013:364659.
- Thijssen W, Kraaijvanger N, Barten D, et al. Impact of a well-developed primary care system on the length of stay in emergency departments in The Netherlands: a multicenter study. BMC Health Serv Res. 2016;16:149.
- Boudreaux ED, O'Hea EL. Patient satisfaction in the emergency Department: a review of the literature and implications for practice. J Emerg Med. 2004;26(1):13–26.
- Expert Group on Health Systems Performance Assessment. SO WHAT? Strategies across Europe to assess quality of care. Publications Office of the European Union; 2016.
- Meeuwissen L, Bakker D. CQ-index huisartsenzorg: meetinstrumentontwikkeling. Kwaliteit van zorg in de huisartsenpraktijk vanuit het perspectief van patiënten. [CQ-index general practice: the development of an instrument. Quality of care in general practice in patients perspective]. Utrecht: NIVEL; 2008. Dutch.
- Smits M, Huibers L, Oude Bos A, et al. Patient satisfaction with out-of-hours GP cooperatives: a longitudinal study. Scand J Prim Health Care. 2012;30(4):206–213.
- Van Uden CJT, Ament AJHA, Hobma SO, et al. Patient satisfaction with out-of-hours primary care in The Netherlands. BMC Health Serv Res. 2005;5(1):6.
- Bos N, van Stel H, Schrijvers A, et al. Waiting in the accident and emergency department: exploring problematic experiences. South Med J. 2015;108(10):613–620.
- Coleman P, Irons R, Nicholl J. Will alternative immediate care services reduce demands for non-urgent treatment at accident and emergency? Emerg Med J. 2001;18(6):482–487.
- de Valk J, Taal EM, Nijhoff MS, et al. Erratum: self-referred patients at the Emergency Department: patient characteristics, motivations, and willingness to make a copayment. Int J Emerg Med. 2015;8:15.
- van der Linden MC, Lindeboom R, van der Linden N, et al. Self-referring patients at the emergency department: appropriateness of ED use and motives for self-referral. Int J Emerg Med. 2014;7:28.
- Kraaijvanger N, Rijpsma D, van Leeuwen H, et al. Self-referrals in the emergency department: reasons why patients attend the emergency department without consulting a general practitioner first-a questionnaire study. Int J Emerg Med. 2015;8(1):46.
