Abstract
Background
Although insomnia is a very common disorder, few people seek medical help.
Objectives
To determine the proportion of people who consult a healthcare professional about insomnia and examine reasons for help seeking.
Methods
Descriptive study of 99 patients diagnosed with insomnia following a telephone survey of 466 adults assigned to a primary healthcare unit in Majorca (Spain). Data were obtained from interviews and subsequent review of electronic medical records.
Results
Thirty-nine patients (39.8%) consulted at least once with one health care professional; 36(92.2%) consulted a general practitioner. Only 12.2% had an insomnia diagnosis registered in their medical record. Insomnia consultation was not associated with any sociodemographic variables analysed, anxiety, depression or comorbidities. Also, there was no association with sleep quality, duration, and sleep efficiency. Patients with clinical insomnia (OR, 2.48; 95% CI, 1.03–5.94), those who were more worried (OR, 2.93; 95% CI 1.08–7.95) or felt that others noticed the impact of insomnia on their quality of life (OR, 2.48; 95% CI, 1.02–19.08) are more likely to seek medical help. Patients taking sleep medication were 21.54 (95% CI, 7.34–63.20) times more likely to have asked for medical assistance.
Conclusion
Insomnia is an under-reported problem for both patients and doctors. When patients decide to consult for insomnia problems, they first go to the GP, and the vast majority take medications for their sleep problem. Those who consult most are people with more severe insomnia and those who are more worried.
Key messages
Although insomnia is a very common disorder, less than half of patients consult a physician; when they consult, patients contact their general practitioner
Presence of clinical insomnia is the main trigger for help seeking
Most of the patients who have consulted are taking insomnia medication
Introduction
Insomnia is the most common sleep disorder, with prevalence rates ranging from 5 to 48% depending on the definitions and diagnostic criteria used by the different studies [Citation1–6]. Insomnia can have significant daytime consequences, such as irritability, depression, concentration problems and chronic illness, and is associated with increased health services use, drug and alcohol consumption, work absenteeism, and accidents [Citation7–9]. Nevertheless, even though effective cognitive-behavioural and pharmacological treatments exist [Citation10,Citation11], just 27–48% of insomniacs seek help from healthcare professionals [Citation1,Citation12,Citation13].
The most common reason for patients not seeking medical help is the perception of insomnia as a benign and unimportant condition, as they need to deal with on their own [Citation14], and asking for medical help is often their last option [Citation15]. Other common barriers to help-seeking are a lack of awareness of available treatments and a belief that existing treatments are ineffective or unattractive [Citation14]. By contrast, factors found to be associated with help-seeking behaviour are consequences of more severe forms of insomnia such as fewer hours of sleep at night and interference with daytime functioning [Citation12,Citation16], and expectations of a prescription that could relieve patient's insomnia symptoms [Citation15,Citation17].
The primary care setting is a critical venue for identification and early intervention to manage insomnia effectively but patients who do decide to seek medical help for insomnia have greater faith in specialists such as psychiatrists and psychologists than in general practitioners (GPs) or nurses [Citation18]. A common perception is that GPs’ knowledge about insomnia is limited to offering advice on sleep hygiene and prescribing drugs while specialists are seen as more knowledgeable and have a better understanding of the nature of the problem and treatment approaches [Citation19].
This study aimed to investigate how many patients with insomnia sought help from a professional, to know which professional they initially contacted and compare sociodemographic characteristics, comorbidities and sleep quality between those who contact a primary care health professional and those who did not.
Methods
Study design
The present study forms part of a broader descriptive cross-sectional survey, investigating the prevalence of insomnia and patient characteristics in the primary care health centre of Calviá (Majorca, Spain) with a population of 23,200 inhabitants registered.
The study was carried out during 2010–2011 and insomnia prevalence results have already been published [Citation6]. The study was developed through two phases. Phase 1 was a telephone insomnia screening survey to detect the population with persistent insomnia. Participants were a random sample generated with Epidat v3.1 of 1563 individuals, aged between 18 and 80 years, registered in the health centre for more than two years. Exclusion criteria were pregnancy, restless legs syndrome, sleep apnoea, narcolepsy, attention-deficit/hyperactivity disorder, palliative care, severe cognitive deficit, psychosis and major depression. Diagnosis of insomnia was based on the Insomnia Severity Index (ISI) score of ≥8.
Participants with detected insomnia were invited to participate in a second phase based on an interview in the health centre. These individuals formed the sample for the present study. This study received the approval of the Majorca Primary Care Ethical Research Committee PI11/15.
Measures
The survey participants with insomnia detected get an appointment at the health centre with a trained nurse or GP. During the interview, all participants were given oral and written information about the study and provided signed consent. The following data were collected: (a) sociodemographic data, (b) the presence of comorbidities, using the list of the Spanish Health Survey [Citation20], (c) any visit to a GP or other healthcare professional about insomnia, (d) use of sleep medication, (e) anxiety and depression measured with the 14-item Spanish version of the Hospital Anxiety and Depression Scale (HADS) [Citation21], (f) insomnia duration, (g) insomnia severity; measured with the Spanish version of the Insomnia severity Index (ISI) [Citation22], which elicits 0–4 severity ratings (‘none’ to ‘very’/’very much’) for recent problems with sleep. A composite score is obtained by adding ratings given to the different items (total possible score, 0–28). Higher scores indicate more severe insomnia [Citation22,Citation23]. According to the ISI scores, patients were classified as sub threshold 8–14 and clinical insomnia >14, and h) Quality of sleep was measured using the Spanish version of the Pittsburgh Sleep Quality Index (PSQI) [Citation24,Citation25], which contains 19 items that assess seven self-reported clinically relevant components of sleep quality in the preceding month: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction. The first four items are answered by free entry, while the rest are rated with a score ranging from 0 to 3, where 0 indicates no problems and 3 indicates a severe problem. A cut-off of 5 discriminates between good and bad sleepers.
After the interviews, the patients’ electronic medical records were reviewed to collect the following information registered during five years before patient inclusion in the study: (a) any visit with a GP or practice nurse about insomnia; (b) any visit with a mental health specialist (psychologist or psychiatrist) about insomnia; (c) a diagnosis of insomnia registered in the patient’s medical record; (d) prescription of pharmacological treatment for insomnia.
Statistical analysis
A descriptive analysis was performed using frequencies and percentages to describe categorical variables. The participants’ rate who had sought medical help for insomnia was calculated. Associations between sociodemographic variables, number of comorbidities (grouped as 0–2 or ≥3), sleep quality, and insomnia consultations were estimated using the χ2 test and calculation of odds ratios with 95% CIs. Statistical significance was considered at a p value < 0.05. Analyses were performed with SPSS v. 23.
Results
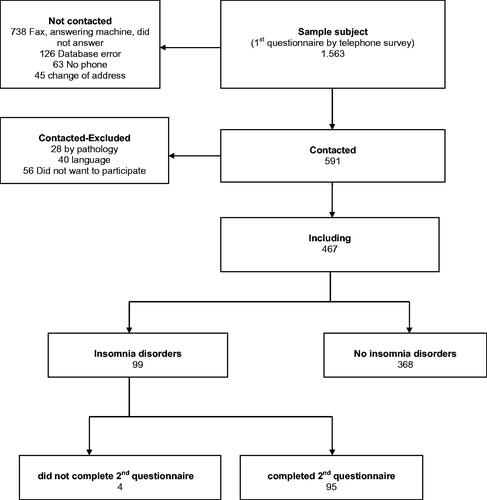
The flowchart of inclusion of the study population is shown in . Of the 467 who answered the first phase, 99 patients were diagnosed with insomnia (ISI score ≥8) and 31 (31.3%) of them were classified as having clinical insomnia (ISI >14). We were unable to access the medical record of one patient who had moved out of Majorca. Patients’ characteristics with insomnia have already been published [Citation6]. These were predominantly women, patients with a stable partner, primary school education, those who had a job, and those younger than 65 years ().
Table 1. Sociodemographic characteristics of sample with insomnia (n = 99).
Help-seeking behaviour
Based on the review of the medical records, 39 patients (39.8%, 95% CI 29.5–48.9%) had discussed their insomnia with a healthcare professional. The vast majority (n = 36, 92.2%) had consulted a GP; 8 (20.6%) had consulted a psychologist and 3 (7.8%) a psychiatrist. None had consulted a practice nurse. Of those who visited a health professional, four patients (10.3%) had discussed their insomnia with at least two healthcare professionals while 3 (8%) had consulted three (GP, psychologist, and psychiatrist). Forty-five patients (45.9%) had been prescribed sleep medication. Just 12 patients (12.2%) had a diagnosis of insomnia registered in their medical record.
Characteristics of people looking for help
More women than men sought medical help for their insomnia, although the difference was not significant (). No significant differences were observed either for age, civil status, or level of education. Help-seeking behaviours were more common in patients with anxiety (but not statistically significant) than in those with depression or more medical conditions.
Table 2. Association between help seeking for insomnia and sociodemographic factors, number of comorbidities, and the presence of anxiety and depression.
Results of ISI and PSQI are summarised in according to whether patients consulted or not about their insomnia. Patients with clinical insomnia (ISI ≥14), those who were worried about their insomnia, and those who felt that the effects of their insomnia on quality of life were noticeable to others were significantly more likely to consult a healthcare professional.
Table 3. Association between help seeking for insomnia and insomnia severity and sleep quality.
Patients who had been prescribed sleep medication formed the largest proportion of patients who sought medical help for their insomnia (84.6%) and they were over 20 times more likely than patients not on prescribed medication (OR, 21.54; 95% CI, 7.34–63.20). A Kappa value of 0.49, indicating moderate agreement, was observed between self-reported medication use and sleep prescription records in clinical notes.
Discussion
Main findings
Our results show that just four of every 10 people with insomnia seek help for their problem from healthcare professionals. Help-seeking behaviour in our population was significantly associated with clinical insomnia (ISI >14). Patients were also more likely to seek professional help if they were worried about their insomnia or if they felt that its impact on their quality of life was noticeable to others. People in these situations have probably come to recognise that their insomnia is a relevant health problem. Most of the patients who consulted a healthcare professional about their insomnia were taking sleep medication. This could be because doctors frequently are more prone to prescribe pharmacological drugs to treat insomnia or because patients’ main reason for visiting their doctor is to request medication that may relieve their insomnia symptoms. Most help seekers in our study had consulted a GP, but this could be due to the nature of the Spanish public healthcare system, where patients can only gain access to other specialists through their GP. It is therefore likely that GPs only referred more complicated cases to mental health specialists.
Strengths and limitations
This was a population-based study where information on insomnia prevalence was obtained by telephone interviews with a random sample of the population assigned to a healthcare centre [Citation6]. We think it would provide a more reliable estimate of the prevalence of insomnia in the general population than studies that calculate prevalence based on members of the population who consulted with a primary healthcare professional. This approach has also been problematic since we had many difficulties in contacting patients, resulting in a low response rate in the prevalence survey and in consequence a low sample size of population with insomnia. We estimated percentages of consultation through medical records that could be affected by information bias, as sleep problems are often not the main reason for consultation and as such might be underreported. Our results show that most GPs have recorded insomnia symptoms declared during a medical consultation as text notes but not as a diagnosis. This fact could result in a lesser follow-up of the problem and less probability of the sleeping disorder being solved.
Comparison with existing literature
Overall, 39.8% of the patients with insomnia sought medical help for their problem; this figure is similar to others reported in the literature (40–48%) [Citation12,Citation26,Citation27], which also showed more than half of patients with insomnia did not receive any help from a professional. Even some of those patients with clinical insomnia and interference in daily functioning did not reach clinical attention. All studies analysed, reported that patients with insomnia were much more likely to consult a GP rather than another specialist, although the rate in our study population, 92.2%, is somewhat higher than rates reported by Morin et al., (82.7%) [Citation27], Stinson et al., (72.9%) [Citation14] and Cheung et al., (65%) [Citation19]. This could be because in Spain, access to psychiatrists and psychologists is through GP referral. We observed that insomnia in our population was under-registered and under-diagnosed by GPs as observed by others studies probably because it was considered as a trivial or temporary problem or because it has been reported to the GP together with other conditions. It was not given priority in the patient agenda [Citation18,Citation28]. As the review of Araujo et al., highlights [Citation29], there is a mismatch between patients’ and health care professionals’ points of view on the experience of insomnia, as well as the complexity and extent of the phenomenon. Health professionals tend to give less attention to the subjective experience of insomnia resulting in under-diagnosis of the insomnia complaints [Citation28].
Women were more likely to seek help from a healthcare professional than men but the difference was not significant, as also seen by Liu et al., and Morin et al., [Citation26,Citation27]. Discrepancies were also noted for sociodemographic variables. While significant associations have been reported between insomnia consultations and older age [Citation30], some college education [Citation12] and unemployment [Citation27], these factors were not significant in our participants.
Our results for anxiety and depression also differ from those reported in the literature. Patients with anxiety were more likely to consult a professional about their insomnia (although not statistically significant), but this was not the case for those with depression, contrasting with findings by other authors who have reported a significant association between consultations and depression [Citation30] and psychiatric disorders in general [Citation26,Citation31]. Also in contrast to other studies [Citation12,Citation26], patients with more medical conditions were not significantly more likely to seek help for their insomnia.
One of the most consistent reasons for seeking help is the severity of insomnia and how it affects daily life activities. In agreement with Liu et al., [Citation26], we found that patients with clinical insomnia (ISI >14) and sleep medication users were more likely to have consulted about their problem. Also, patients more worried about insomnia and those with daily life impact noticeable to others were more prone to seek medical help. Findings of Cheung et al., in specialist care [Citation19], show that daytime symptoms arising from insomnia serve as important illness cues for patients to seek medical help. Others found that non-restorative sleep and difficulties initiating sleep were the factors most strongly associated with a self-reported need for the treatment of sleeping difficulties [Citation31].
Implications for clinical practice
Despite the considerable impact of insomnia on the quality of daily life of those suffering, it is still an under-reported health problem. Those who seek medical help mainly contact their primary care physician. Continuity of care in primary care is a unique opportunity to recognise insomnia during clinical interviews. Being more active and asking more assertive sleep-related questions in patients with sleep complaints during a consultation for other conditions could be a helpful approach in detecting insomnia. Since many persons who have insomnia do not consult, it would be advisable to design strategies aimed at community care, either to detect insomnia or for its management. Other studies are needed in this field, especially with a qualitative approach to explore both professionals and patients’ perspectives on insomnia as a health disorder and beliefs around its management.
Conclusion
Insomnia is an under-reported problem for both patients and doctors. When patients decide to consult for insomnia problems, they first go to the GP, and the vast majority of them take medications for their sleep problem. Half of the patients do not request medical help and consequently, a vital percentage that have clinical insomnia or who are worried about the disorder miss the opportunity to receive a treatment that could benefit them.
Acknowledgement
We thank all general practitioners who facilitated our contact with the patients who participated in this study. We thank Leighton Jones for editing the revision.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Additional information
Funding
References
- Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111.
- Ohayon MM, Sagales T. Prevalence of insomnia and sleep characteristics in the general population of Spain. Sleep Med. 2010;11(10):1010–1018.
- Léger D, Partinen M, Hirshkowitz M, EQUINOX (Evaluation of daytime QUality Impairment by Nocturnal awakenings in Outpatient's eXperience) Survey Investigators, et al. Characteristics of insomnia in a primary care setting: EQUINOX survey of 5293 insomniacs from 10 countries. Sleep Med. 2010;11(10):987–998.
- Cañellas Dols F, Ochogavia Cánaves J, Llobera Cánaves J, et al. ITC. Trastornos del sueño y consumo de hipnóticos en la isla de Mallorca [sleep disorders and the consumption of hypnotics on the island of Mallorca]. Rev Clin Esp. 1998;198:719–725.
- Vela-Bueno A, de Iceta M, Fernández C. Prevalencia de los trastornos del sueño en la ciudad de Madrid [prevalence of sleep disorders in Madrid, Spain]. Gac Sanit. 1999;13(6):441–448.
- Torrens I, Argüelles-Vázquez R, Lorente-Montalvo P, et al. Prevalencia de insomnio y características de la población insomne de una zona básica de salud de Mallorca (España) [Prevalence of insomnia and characteristic of patients with insomnia in a health area of Majorca (Spain)]. Aten Primaria. 2019;51(10):617–625.
- Daley M, Morin CM, LeBlanc M, et al. Insomnia and its relationship to health-care utilization, work absenteeism, productivity and accidents. Sleep Med. 2009;10(4):427–438.
- Léger D, Partinen M, Hirshkowitz M, EQUINOX (Evaluation of daytime QUality Impairment by Nocturnal awakenings in Outpatients eXperience) survey investigator group, et al. Daytime consequences of insomnia symptoms among outpatients in primary care practice: EQUINOX international survey. Sleep Med. 2010;11(10):999–1009.
- Chung KF, Yeung WF, Ho FYY, et al. Predictors of daytime consequences of insomnia: the roles of quantitative criteria and nonrestorative sleep. Psychopathology. 2018;51(4):262–268.
- Morin CM, Bootzin RR, Buysse DJ, et al. Psychological and behavioral treatment of insomnia: update of the recent evidence (1998–2004). Sleep. 2006;29(11):1398–1414.
- Riemann D, Baglioni C, Bassetti C, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675–700.
- Aikens JE, Rouse ME. Help-Seeking for insomnia among adult patients in primary care. J Am Board Fam Pract. 2005;18(4):257–261.
- Hayward RA, Jordan KP, Croft P. The relationship of primary health care use with persistence of insomnia: a prospective cohort study. BMC Fam Pract. 2012;13:8.
- Stinson K, Tang NKY, Harvey AG. Barriers to treatment seeking in primary insomnia in the United Kingdom: a cross-sectional perspective. Sleep. 2006;29(12):1643–1646.
- Dyas JV, Apekey TA, Tilling M, et al. Patients’ and clinicians’ experiences of consultations in primary care for sleep problems and insomnia: a focus group study. Br J Gen Pract. 2010;60:180–200.
- Morin CM, Barlow DH. Insomnia: psychological assessment and management. Guilford Press; 1993.
- Bjorvatn B, Meland E, Flo E, et al. High prevalence of insomnia and hypnotic use in patients visiting their general practitioner. Fam Pract. 2017;34(1):20–24.
- Sake FTN, Wong K, Bartlett DJ, et al. Insomnia management in the Australian primary care setting. Behav Sleep Med. 2019;17(1):19–30.
- Cheung JMY, Bartlett DJ, Armour CL, et al. Insomnia patients' help-seeking experiences. Behav Sleep Med. 2014;12(2):106–122.
- MINSAL. Encuesta Nacional de Salud [National Health Survey]. Vol. 68, Revista de sanidad e higiene publica. 2011 [cited 2020 Nov 20]. Available from: https://www.mscbs.gob.es/estadEstudios/estadisticas/encuestaNacional/encuestaNac2011/Cuestionario_Adultos.pdf.
- Quintana JM, Padierna A, Esteban C, et al. Evaluation of the psychometric characteristics of the Spanish version of the hospital anxiety and depression scale. Acta Psychiatr Scand. 2003;107(3):216–221.
- Sierra JC, Guillén-Serrano V, Santos-Iglesias P. Insomnia severity index: some indicators about its reliability and validity on an older adults sample. Rev Neurol. 2008;47:566–570.
- Gagnon C, Bélanger L, Ivers H, et al. Validation of the insomnia severity index in primary care. J Am Board Fam Med. 2013;26(6):701–710.
- Buysse DJ, Reynolds CF, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
- Royuela Rico A, Macías Fernández JA. Propiedades clinimétricas de la versión castellana del cuestionario de Pittsburgh [Clinometric properties of the spanish version of the Pittsburgh questionnaire]. Vigilia-sueño. 1997;9(2):81–94.
- Liu Y, Zhang J, Lam SP, et al. Help-seeking behaviors for insomnia in Hong Kong Chinese: a community-based study. Sleep Med. 2016;21:106–113.
- Morin C, Leblanc M, Daley M, et al. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7(2):123–130.
- Tubtimtes S, Sukying C, Prueksaritanond S. Sleep problems in out-patient of primary care unit. J Med Assoc Thai. 2009;92(2):273–278.
- Araújo T, Jarrin DC, Leanza Y, et al. Qualitative studies of insomnia: current state of knowledge in the field. Sleep Med Rev. 2017;31:58–69.
- Bartlett DJ, Marshall NS, Williams A, et al. Predictors of primary medical care consultation for sleep disorders. Sleep Med. 2008;9(8):857–864.
- Sandlund C, Westman J, Hetta J. Factors associated with self-reported need for treatment of sleeping difficulties: a survey of the general Swedish population. Sleep Med. 2016;22:65–74.