Abstract
Background
The shortage of family physicians is a considerable challenge in Hungary. The number of vacant practices is increasing and the rural and deprived areas are more affected.
Objectives
This study aimed to investigate medical students’ attitudes towards rural family medicine.
Methods
The current study used a cross-sectional design with a self-administered questionnaire. Each of the four Hungarian medical universities was represented by their medical students from December 2019 to April 2020.
Results
The response rate was 67.3% (n = 465/691). Only 5% of the participants plan to be a family doctor, 5% of the students plan to work in rural areas. On a 5-point Likert scale (1 = ‘surely not’, 5 = ‘surely yes’), half of the participants answered 1 or 2 to choose rural medical work, while 17.5% answered 4 or 5. There was a significant relationship between rural working plans and rural origin (OR = 1.97; p = 0.024), and the plan to work in family practice (OR = 4.90; p < 0.001).
Conclusion
Family medicine is not a popular career option among Hungarian medical students and rural medical work is even less attractive. Medical students with a rural origin and an interest in family medicine are more likely to plan to work in rural areas. More objective information and experience need to be given to medical students about rural family medicine to increase the attractiveness of the speciality.
KEY MESSAGES
Very few medical students think about rural family medicine as a career option.
It is crucial to find effective strategies to stop the tendency of vacancies in practices.
More emphasis should be put on students with rural backgrounds and rural training places to promote rural family medicine.
Introduction
Access to the full range of essential health services is a fundamental human right but currently, there are significant inequalities and rural communities often have a disadvantage in this field [Citation1,Citation2]. Strong primary care is key in providing universal health coverage and contributes to an equitable, efficient and cost-effective health care system [Citation3].
The specific characteristics of ‘Rural medicine’ vary from country to country. The differentiation between rural and urban contexts is based on various factors, such as geographic, environmental, economic, cultural, social and other characteristics [Citation4]. The current survey did not use strict definitions, and the participants could decide what they considered to be rural, but in Hungary, for medical students, rural medicine means medical services in the countryside. In Hungary, about 30% of the population lives in rural settings. Hungary does not have geographically separated areas and an extensive territory (93,030 km2); economic and financial aspects play a role in regional disparities [Citation5].
In July 2022, 677 family practices were not filled out of the 6460 (10.5%) and 516 vacant practices (76.2%) were situated in areas with fewer inhabitants than ten thousand. It means that rural areas are mostly affected by the problem of vacant practices. In parallel, this negative trend has reached the big cities; 45 vacant practices are in the capital city, Budapest [Citation6]. The number of vacant practices has grown steadily in recent years, almost tripled in 2010–2017. There is a strong association between deprived areas and unfilled practices [Citation7]. The number of new entrants into the GP resident training programme is insufficient to stop this trend [Citation8].
Career choice is a multifactorial decision in medical students’ lives. The medical school, the student’s personality and preferences, the ideas about the preferred speciality and the current life situation significantly impact the decision [Citation9]. In this article, we focus only on the impact of their attitude towards rural family medicine on career choice. Medical education plays a significant role in medical students’ lives through knowledge transfer and by shaping their attitudes. The hidden curriculum strongly influences the students’ career decisions [Citation10]. EURACT (European Academy of Teachers in General Practice/Family Medicine) suggests that every medical faculty should have a department or unit of family medicine with a family doctor as chair and family medicine should be part of the undergraduate core curriculum [Citation11]. There is strong evidence that the quantity of practical GP curriculum is directly correlated with medical students’ willingness to choose family medicine as a future career [Citation12]. Rural medicine is in the same situation. EURIPA (European Rural and Isolated Practitioners Association) and EURACT state that specific rural medicine programmes must be part of medical education to increase the popularity of pastoral work [Citation13].
The movement of family physicians from more deprived areas to developed areas causes an unequal distribution of physicians. This process also exists between countries. Since 2004, when Hungary became an EU member, healthcare professionals’ migration has become an increasing problem [Citation7,Citation14,Citation15].
This study aims to describe the attitudes and motivations of Hungarian medical students towards family medicine and rural medical work and to explore the influencing factors. There were two hypotheses underlying this research: medical students of a rural origin are likelier to work in rural areas. Medical students interested in family medicine are more likely to work in rural settings.
Methods
Study design and participants
It was a cross-sectional survey with a self-administered paper-based questionnaire. Participation was voluntary and anonymous. Four Hungarian medical universities (Budapest, Debrecen, Szeged, and Pécs) were represented by their fourth and fifth-year medical students who attended face-to-face family medicine lectures. Because the four universities have different curricula and family medicine is included in different years, we involved the appropriate years everywhere (). Data collection was carried out from December 2019 to April 2020. After this time, it had to be stopped due to the COVID-19 pandemic. This step primarily affected the University of Pécs, where we reached a lower response rate. After receiving appropriate information about the study, 465 students decided to participate.
Table 1. The presence of family medicine in Hungarian universities in 2020.
Questionnaire
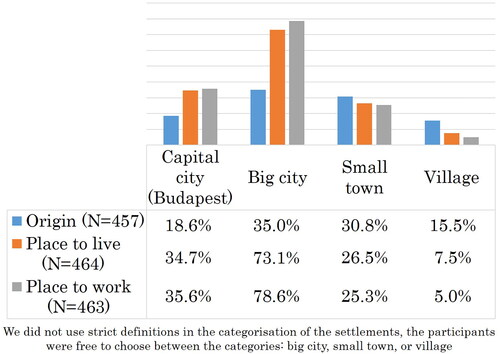
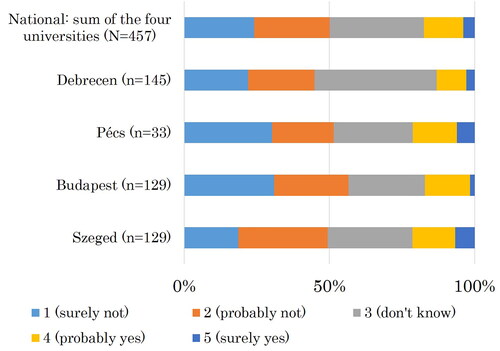
Data were collected with a self-developed questionnaire. There were nine questions about sociodemographic data, such as gender, age, place of origin and family role model (higher education, medical degree or family physician in the family?). Three questions were concerned with future career plans and preferred specialities. Students were asked about their planned future living place and workplace. The likelihood of rural work among participants was assessed. The first variable was ‘Do you plan to work in a rural area in the future?’ with two answer options: ‘yes’ or ‘no.’ The second variable was: ‘Do you consider it likely that you will work in a rural area in the future?’ Answers were assessed with a 5-point Likert scale (1: surely not, 2: probably not, 3: do not know, 4: probably yes, 5: surely yes). In the multivariate analysis, the categories were merged: answers 1 and 2 became ‘no,’ answers 4 and 5 became ‘yes’ and answer 3 was not used. We did not use strict definitions in the categorisation of the settlements. The capital city is Budapest but the participants could choose between the other categories. (big city, small town, or village).
Data analyses
Data analysis was done by STATA (version 13.0, Stata Corp, College Station, TX). Descriptive statistics were performed using chi-square tests. Multivariate logistic regression models (MVA) were used to identify which factors might influence students’ future career plans focusing on the rural environment, where goodness-of-fit tests were also executed. The multivariate models consisted of two outcomes (‘X’,‘Z’). Descriptive data are presented by means/medians and standard deviations/interquartile ranges (IQR) in the case of continuous variables and as percentages in the case of categorical variables. Odds ratios describe the multivariate model results. The results were considered significant if the p-values derived from the statistical tests were below 0.05.
Ethics approval
Ethics approval was received from the National Medical Research Council, Hungary, reference number 51983-2/2019/EKU.
Results
In the relevant years, 1057 medical students studied at the four universities. In the given period, 691 participated in family medicine lectures. Of these students, 465 completed our questionnaire (67.3%). The response rate was 86.8% (n = 145/167) in Debrecen, 23% (n = 38/165) in Pécs, 63% (n = 131/208) in Budapest and 73.3% (n = 151/206) in Szeged. Sociodemographic characteristics of the sample are presented in .
Table 2. Sample characteristics.
Only 5% of the respondents (n = 23/462) plan to work as a family doctor in the future, 72% (n = 333/462) of them have other speciality preferences and 23% (n = 106/462) have not chosen their preferred speciality yet, 15.5% of the students have a rural origin. The vast majority of the participants plan to live in urban environments. The ratio of students who plan to work in rural settings is 5% ().
There was a significant positive relationship between a rural origin and rural working plans (UVA: p = 0.018; MVA: OR = 1.97; p = 0.024). The rural working plans had a significant correlation with family medicine as a first choice speciality (UVA: p < 0.001) and with the intention to work in family practice in the future (UVA: p < 0.001; MVA: OR = 4.90; p = 0.014) (); 51.5% of the students plan to work abroad after their graduation. On a 5-point Likert scale, 50.1% of the participants answered that they would ‘surely not’ or ‘probably not’ (together: ‘no’) choose rural medical work, while 17.5% answered ‘probably yes’ or ‘surely yes’ (together: ‘yes’) ().
Table 3. Results of the univariate and of the multivariate analysis (UVA and MVA).
There was a significant correlation between the probability of rural work and a rural origin (UVA: p = 0.001; MVA: OR = 3.24; p < 0.001), between the probability of rural work and family medicine as a first-choice speciality (UVA: p = 0.001) and between the probability of rural work and the plan to work in family practice in the future (UVA: p = 0.002; OR = 4.99; MVA: p < 0.018).
Discussion
Main findings
Our study found that only a few medical students think about family medicine as a career option (5%). The analysis of the reasons for low interest in family medicine is out of the scope of this work. Rural work is not attractive for students; only 5% think about a rural medical career. About one-quarter of the students would not work in rural areas in any case. However, half of the students were uncertain or showed more or less willingness towards rural work. The job is to focus on this group, give them opportunities to understand the characteristics of rural medical work better and motivate them to choose this career. The results confirmed our first hypothesis: medical students of a rural origin are more likely to plan to work in rural areas. There was a strong correlation between rural career plans and willingness to work in family practice and our second hypothesis was confirmed. Our results support that migration remains a key issue in family physicians’ recruitment. Half of the students plan to work abroad.
Strengths and limitations
This is the first study that examined Hungarian medical students’ attitudes towards rural medical work as a career option among medical students from all four Hungarian medical universities. The sample size and response rate are acceptable and allow us to draw general conclusions about the Hungarian situation. Because of the Covid-19 Pandemic, a lower response rate was reached than initially expected. However, based on the nature of this limiting factor, we can assume that the characteristics of the participant group of students and the non-participant group of students are not different. The gender ratio supports our assumption: 62.1% (288/464) in the participant group and 63.9% (379/593) in the non-participant group. The fourth and fifth year students were at different stages of their medical studies and may have different perceptions and experience, which could be a limiting factor. The lack of a strict definition of 'rural’ can be a limiting factor. Cross-sectional data cannot be used to infer causality. Only a few of the medical students are interested in family medicine and rural medical work as a future career option; therefore we could not describe the unique characteristics of this group.
Comparison with existing literature
In our previous studies, 0–3.9% of medical students planned to be a family doctor definitely and 12.1–19.2% thought about it [Citation16]. Worldwide, healthcare systems face similar challenges and the popularity of primary care work is not high enough among medical students. Naimer et al. found that 19% of Israeli students are interested in family medicine [Citation17]. In Germany, 12.3% of the students plan to opt for family medicine [Citation18]. Girasek et al. found that in 2008, only 0.8% of Hungarian resident doctors planned to work in places with fewer inhabitants than 10,000 [Citation19]. In our previous research in 2016, students with primary care orientation were 28 times more likely to work in rural areas than the students who would have liked to work in secondary care [Citation16], 21% of Argentinians, 44% of the Indians and 42% of the Australian medical students want to work in rural areas. In these countries, rural medicine gets more emphasis during medical education, students get more impulses and experience from this field and undergraduate rural is significantly associated with long-term rural work [Citation20–23]. Studies show that financial and economic incentives and rural practice experience during the medical years could drive these students to rural pathways. However, not only financial aspects but also lifestyle factors play an essential role in the decision [Citation24,Citation25]. The Hungarian government supports rural employment with different tender opportunities but it does not seem to be motivating enough for doctors or medical students. A meta‑analysis from 2020 states that rural exposure during medical education increases the likelihood of future rural practice by more than four times on average [Citation26]. In the case of complex educational programmes, the background of medical students, their interactions with rural communities and many other factors also play an important role. The rural community-based medical education programme in Thailand and the many Australian rural education programmes are successful examples of initiatives to solve the rural human resource crisis [Citation27,Citation28]. Győrffy et al. found that in 2016 almost 40% of the participating fifth and sixth-year medical students planned to work abroad as a doctor. Based on these, we can state that the tendency did not change significantly. [Citation14].
Implications for practice and policy
Undergraduate education has a crucial role in specialisation. Different career choice-supporting resources and programmes could positively impact students’ engagement with career planning [Citation29]. It seems worthwhile to handle the challenges of the rural human resource crisis and human resource recruitment in family medicine together. Training more general practitioners could be important in addressing the rural doctor shortage. We recommend increasing the presence of family medicine and rural medical work in the curriculum. Creating strategies to involve more rural students in medical universities should be considered. Furthermore, it is vital to recognise what factors determine urban students, who are in the majority, to choose rural medical work. Moreover, the universities, medical organisations, government, and the media are also responsible for authentic informing of medical students about their career choice. The shortage of rural family physicians is not an exclusively Hungarian issue. Awareness of different countries’ challenges or solution proposals could trigger better local initiatives in every country or international cooperation.
Conclusion
Human resource recruitment in rural primary care is an unsolved problem. It is crucial to find enough highly qualified medical professionals with primary care orientation and it needs young doctors who are interested in rural medical work. Only a few medical students consider rural family medicine as a career option in Hungary. Implementing international programmes and adapting them to local conditions would be beneficial. To promote rural medical work and family medicine as a career, more emphasis should be put on medical students with rural backgrounds and rural training places.
Ethical approval
Ethics approval was received from the Medical Research Council, Hungary, reference number 51983-2/2019/EKU. Informed consent was obtained from all subjects. All experimental protocols for involving human data was per the Declaration of Helsinki.
Authors’ contributions
AM and TP contributed to the conception and design, questionnaire development, data analysis, interpretation of the results and the first draft of the manuscript. GSz contributed to data analysis and interpretation. LK, JR, AV, MKM and CsH contributed to data and literature collection and critically revised the manuscript. All authors read and approved the final version of the manuscript.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Data availability statement
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- World Health Organization. Increasing Access to health workers in remote and rural areas through improved retention. Global policy recommendations. Geneva (Switzerland): World Health Organization; 2010. [cited 2021 March 24]. Available from: http://whqlibdoc.who.int/publications/2010/9789241564014_eng.pdf
- World Health Organization. Declaration of Astana. Geneva: World Health Organization; 2018. [cited 2021 March 24]. Available from: https://www.who.int/primary-health/conference-phc/declaration
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502.
- Reid S, Worley P, Strasser RP, et al. ’What brings us together’: the values and principles of rural medical education. In: Chater AB, Rourke J, Couper ID, Strasser RP, Reid S, editors. WONCA Rural medical education guidebook. Bangkok (Thailand): World Organization of Family Doctors (WONCA): WONCA Working Party on Rural Practice. [cited 2021 March 24]. Available from: https://www.globalfamilydoctor.com/site/DefaultSite/filesystem/documents/ruralGuidrural/RMEG.pdf
- Magyarország: a népesség – demográfiai helyzet, nyelvek, vallások [Hungary: population – demographic situation, languages, religions. Eurydice.]. Hungarian. [cited 2021 March 24]. Available from: https://eurydice.eacea.ec.europa.eu/national-education-systems/hungary/population-demographic-situation-languages-and-religions
- Háziorvosi szolgálatok. Nemzeti Egészségbiztosítási Alapkezelő [Family practice services. National health insurance fund of Hungary.]. Hungarian. [cited 2021 March 24]. Available from: http://www.neak.gov.hu/felso_menu/lakossagnak/szerzodott_szolgaltatok/haziorvosi_szolgalatok.html.
- Papp M, Kőrösi L, Sándor J, et al. Workforce crisis in primary healthcare worldwide: Hungarian example in a longitudinal follow-up study. BMJ Open. 2019;9:e024957.
- Rurik I. Alapellátás, alapellátók Magyarországon, 2018 [Primary care and providers in Hungary, 2018.]. Orv Hetil. 2019;160(24):926–935. Hungarian.
- Querido SJ, Vergouw D, Wigersma L, et al. Dynamics of career choice among students in undergraduate medical courses. A BEME systematic review. Med Teach. 2016;38(1):18–29.
- Sarikhani Y, Shojaei P, Rafiee M, et al. Analyzing the interaction of main components of hidden curriculum in medical education using interpretive structural modeling method. BMC Med Educ. 2020;20(1):176.
- Simmenroth A, Carelli F, Vallersnes OM, et al. European education requirements for the undergraduate general practice/family medicine curriculum. EURACT/WONCA EUROPE; 2020. [cited 2021 March 26]. Available from: https://euract.woncaeurope.org/sites/euractdev/files/documents/publications/others/bmeeducation-requirements-151220finalwith-we.pdf
- Alberti H, Randles HL, Harding A, et al. Exposure of undergraduates to authentic GP teaching and subsequent entry to GP training: a quantitative study of UK medical schools. Br J Gen Pract. 2017;67(657):e248–e252.
- Lopez-Abuin JM, Kersnik J. EURIPA—EURACT: medical education in rural practice improves quality of care and can attract more physicians to enter rural practice. Eur J Gen Pract. 2013;19(2):133–134.
- Zs G, Zs S. Magyarországi orvostanhallgatók külföldi munkavállalási szándékai [Willingness to work abroad among Hungarian medical students.] Orv Hetil. 2018;159(1):31–37. Hungarian
- Kovács E, Girasek E, Kozák A, et al. Helyzetkép az elvándorlásban érintett orvosi szakterületek hazai humánerőforrás-ellátottságáról. Orv Hetil. 2019;160(31):1223–1230. Hungarian.
- Mohos A, Varga A, Markó-Kucsera M, et al. A családorvoslás mint karrier. Orvostanhallgatók pályaválasztással kapcsolatos vélekedései és motivációi [Family medicine as a career. Medical students’ attitudes and vocational choice motivations]. LAM. 2019;29(12):627–634. Hungarian
- Naimer S, Press Y, Weissman C, et al. Medical students’ perceptions of a career in family medicine. Isr J Health Pol Res. 2018;7:1.
- Deutsch T, Lippmann S, Frese T, et al. Who wants to become a general practitioner? Student and curriculum factors associated with choosing a GP career - a multivariable analysis with particular consideration of practice-orientated GP courses. Scand J Prim Health Care. 2015;33(1):47–53.
- Girasek E, Edit Eke E, Szócska M. Analysis of a survey on young doctors’ willingness to work in rural Hungary. Hum Res Health. 2010;8:13.
- Borracci R, Arribalzaga EB, Couto JL, et al. Factors affecting willingness to practice medicine in underserved areas: a survey of Argentine medical students. RRH. 2015;15:3485.
- Jain M, Gupta SA, Gupta AK, et al. Attitude of would-be medical graduates toward rural health services: an assessment from Government Medical Colleges in Chhattisgarh. J Fam Med Prim C. 2016;5(2):440–443.
- Walker J, DeWitt D, Pallant J, et al. Rural origin plus a rural clinical school placement is a significant predictor of medical students’ intentions to practice rurally: a multi-university study. RRH. 2012;12:1908.
- Playford D, Masi L, Rowe A, et al. Factors associated with Australian female doctors’ long-term, as opposed to short-term, rural Family Medicine work. Fam Pract. 2022;39(4):633–638.
- Budhathoki SS, Zwanikken PAC, Pokharel PK, et al. Factors influencing medical students’ motivation to practise in rural areas in low-income and middle-income countries: a systematic review. BMJ Open. 2017;7(2):e013501.
- Javorská K, Halata D, Štolfa J, et al. What are the main motivating factors for young general practitioner trainees to work in rural areas in the Czech Republic? Eur J Gen Pract. 2022;28(1):200–202.
- Holst J. Increasing rural recruitment and retention through rural exposure during undergraduate training: an integrative review. Int J Envir Res Publ Health. 2020;17:6423.
- Somporn P, Walters L, Ash J. Expectations of rural community-based medical education: a case study from Thailand. Rural Remote Health. 2018;18(4):4709.
- Sullivan BGO, Matthew R, McGrail MR, et al. A review of characteristics and outcomes of Australia’s undergraduate medical education rural immersion programs. Hum Res Health. 2018;16(1):8.
- Gyekye-Mensah H, Watkins A, Wenden J, et al. An evaluation of a student-led career profiling project to support the exploration of a career in general practice and other specialities. BJGP Open. 2022;6(3):BJGPO.2022.0002.