Abstract
Background
The countries of the former Yugoslavia have health and education systems with the same tradition but these have changed over the years. Little is known about how family medicine teaching transitioned from face-to-face to distance education during the COVID-19 pandemic.
Objectives
to investigate student/teacher experience in transitioning from face-to-face to distance education.
Methods
A cross-sectional, online survey was conducted among 21 medical schools of the former Yugoslavia between December 2021 and March 2022. Under/postgraduate teachers and students who taught/studied family medicine during the academic year 2020/2021 were invited to participate. Of 31 questions for students and 35 for teachers, all but nine open questions were analysed using descriptive statistics.
Results
Seventeen of 21 medical schools contributed data involving 117 participants representing all countries of the former Yugoslavia. At the beginning of the pandemic, 30%, 26% and 15% of teachers, students and trainees, respectively, received formal preparation in distance education. Of these, 92% of teachers and 58% of students/trainees felt they were not adequately prepared. Synchronous teaching was the main method used, with a third using hybrid methods. All participants were least confident about online assessment. More than 75% of respondents agreed that lectures could be kept online, not patient consultations or practical skills’ classes.
Conclusion
Teachers used various old and new methods to provide learning opportunities despite COVID-19 constraints. Effective technology-based strategies are essential to ensure assessment integrity and enhance the learning environment.
KEY MESSAGES
Despite limited preparedness, teachers and students/trainees transitioned to distance education.
Students/trainees believed synchronous delivery of lectures and small group work can be conducted online but not practical skills’ classes.
Online assessments and practical work with patients were considered the most challenging aspects of distance education.
Introduction
The COVID-19 pandemic profoundly influenced healthcare services worldwide, including the delivery of medical education [Citation1–3]. Several challenges related to providing medical education in pandemic conditions included physical distancing, risks of teaching in the clinical environment with students and trainees as potential infection vectors, and the supply and use of personal protective equipment [Citation4,Citation5].
The most prominent change in medical education was the transition from in-person, face-to-face instruction to blended learning, using online teaching as a predominant teaching model [Citation4,Citation5]. Remote synchronous and asynchronous educational models were rapidly developed, providing students and teachers with opportunities for interaction in real time, as well as accessing and reflecting on learning materials at their own pace [Citation2].
Virtual medical education as a concept is not new. It expanded in the pre-COVID era, with academic institutions adapting their education provision from face-to-face teaching to an online model. This was done in line with advancing technology and a more active role of students in the learning process [Citation6]. Various barriers encountered included time constraints, poor technical skills and inadequate infrastructure. Improved educator skills, improved institutional support and a positive attitude amongst all those involved were suggested as possible solutions [Citation7]. One of the preferred formats was the blended learning model, characterised by combining traditional face-to-face learning and asynchronous or synchronous e-learning. This model demonstrated better effects on knowledge outcomes when compared to conventional learning in health education [Citation8].
During the COVID-19 pandemic, teachers needed to rapidly adapt to new teaching formats, challenged with the burden of providing safe clinical work and maintaining a high standard of medical education [Citation9]. The significant additional effort required to develop and implement distance learning models was recognised by most medical institutions, including the need for additional training related to technical skills and effective online teaching methods [Citation2].
The adaptation of family medicine undergraduate and postgraduate teaching in the countries of the former Yugoslavia seems to have followed a similar transition process from classical education to predominantly online classes [Citation10–11], but little is known about the experience of students and faculty staff involved in this process. A formal collaboration of family medicine teachers in the former Yugoslavia region was established in 2011, due to their common past, similar education and health systems, and shared language [Citation12]. Hence, the seven countries in the region can be treated as a relatively homogenous group.
Most published studies have assessed the experience of distance learning from the perspective of either students or teachers; however, very few have investigated the experience of both groups during the COVID-19 pandemic [Citation13–16]. In addition, most studies have been conducted in single sites, reporting adaptations to distance learning in individual institutions [Citation10,Citation17]. Hence, this study aimed to investigate the experience of both under/postgraduate teachers and students, in the transition from face-to-face to distance education in an international setting and determine the suitability of distance learning for future family medicine education.
Methods
Study design
We used a cross-sectional, multi-centre, descriptive design, using an online survey, containing both closed and open questions exploring the experience of under/postgraduate teachers and students in transitioning from face-to-face to distance education in family medicine. Qualitative methods were used to analyse the open question responses and due to the data volume the findings are reported in a separate paper [Citation18].
Recruitment and data collection
Participant recruitment took place from 11th December 2021 until 1st March 2022 among all 21 medical schools in the region of the former Yugoslavia: Banja Luka, Belgrade, Foča, Kragujevac, Ljubljana, Maribor, Mostar, Niš, Novi Sad, Osijek, Podgorica, Priština, Rijeka, Sarajevo, Skopje, Split, Štip, Tetovo, Tuzla, Zagreb and Zenica.
The link to two online questionnaires, one for teachers and one for students/trainees, was sent to heads of the departments of family medicine or their representatives, with the request to distribute the links to at least two family medicine teachers involved in undergraduate and/or postgraduate distance education during the academic year 2020/2021; and to at least two undergraduate and/or postgraduate students/trainees involved in family medicine distance education in the academic year 2020/2021. This number seemed feasible even for smaller family medicine departments with only a few employed staff.
Two follow-up reminder emails were sent at monthly intervals together with personal contacts to facilitate the return of completed questionnaires. All questionnaires were returned anonymously.
Questionnaire
A semi-structured questionnaire for teachers was created in English (Supplementary files) following a literature search of online teaching experience. This was then adapted to students and refined in repeated consultations with study team members. The questionnaires were then translated into two languages by native speakers, members of the study team: Slovenian (distributed to departments of family medicine in Ljubljana and Maribor) and Croatian (distributed to the other departments of family medicine). The survey was conducted using the 1 Ka survey online tool (Ljubljana, version 12.11.16; 1ka.si)
The four-page questionnaire contained 31 questions for students and 35 for teachers, nine of which were ‘open-ended’. The remaining questions were single- or multiple-answer multiple choice questions and Likert scale questions. The questionnaire was divided into three sections: (1) personal details (students - gender, year of study, university, previous experience with distance learning; teachers - gender, age, university, academic title, student/trainee teacher, previous experience with distance teaching); (2) experience of distance education (preparedness for distance education, confidence in distance education, attitudes towards distance education), and (3) obstacles and facilitators of distance education (open questions). Some statements pertaining to online teaching conditions were adapted from Perron et al. [Citation13]. We piloted the survey on a sample of four medical students from the medical schools in Split and Ljubljana. Student feedback was incorporated into the final version of the questionnaire. In addition, the questionnaire was critically revised by a research methodologist with expertise in medical education. We analysed data only from fully completed and submitted surveys.
Analysis
In this paper, only the quantitative findings are reported. Due to the large volume of data, we present the qualitative findings separately. Descriptive statistics were used to show the quantitative data; sample size (n), percentages (%), frequencies, minimum, maximum and mean values.
Ethics
The study protocol was approved by the Ethics Committee of the University of Split, School of Medicine (Klasa: 003-08/21-03/0003; Ur. br.: 2181-198-03-04-21-0075) on 13th July 2021. All participants were informed of the purpose and content of the survey and, by commencing the survey, gave their voluntary consent to participate.
Results
Participant characteristics
Of the 21 regional medical schools, 17 contributed data to the survey. Foča, Kragujevac and Niš did not respond, and Banja Luka held all their teaching in person during the academic year 2020/2021 (). The total number of participants was 117; among these were 23 students, 54 trainees and 40 teachers. Participant characteristics are shown in . Most of the teachers taught undergraduate students as well as family medicine trainees.
Table 1. Characteristics of participants.
Preparedness for distance education
Previous distance education, prior to the COVID-19 pandemic, was experienced by 65%, 42% and 53% of students, trainees and teachers, respectively (). At the beginning of the pandemic, 30%, 26% and 15% of teachers, students and trainees, respectively, received training/preparation in distance education. Only 8% of teachers and 42% of students and trainees who received training/preparation felt that training prepared them thoroughly for distance education. The group that claimed to have received the least preparation was trainees but the difference between groups was statistically insignificant. During the pandemic, synchronous lectures and seminars were the predominant form of distance education. Students and trainees tended to be more inclined than teachers to keep at least some distance education after the pandemic (p = .080). Practical skills and patient consultations were considered least appropriate for future distance education.
Table 2. Preparation for online classes and opinions about its future use.
Confidence and attitudes towards distance education
Teachers’ and students’/trainee’s confidence and attitudes towards distance education are presented in and . Students/trainees felt most confident when it came to using technology for distance learning (mean 3.93) but they were less optimistic about being assessed online (mean 3.47) (). Teachers were most satisfied in interacting with students/trainees (mean 3.73), and least confident in assessing remotely (mean 3.03). Teachers were generally less confident than students/trainees in all aspects of distance education ().
Figure 1. Teachers’ (T) and students’/trainees’ (St + Tr) confidence in distance education (DE) Absolute values of responders (total no. teachers: 40; total no. students + trainees: 77) Vertical bar represents the median of neutral responses.
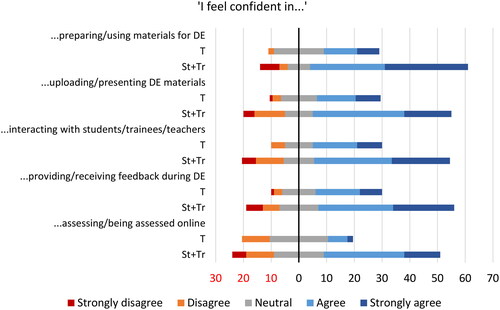
Figure 2. Teachers’ (T) and students’/trainees’ (St + Tr) attitudes towards distance education Absolute values of responders (total no. teachers: 40; total no. students + trainees: 77). Vertical bar represents the median of neutral responses.
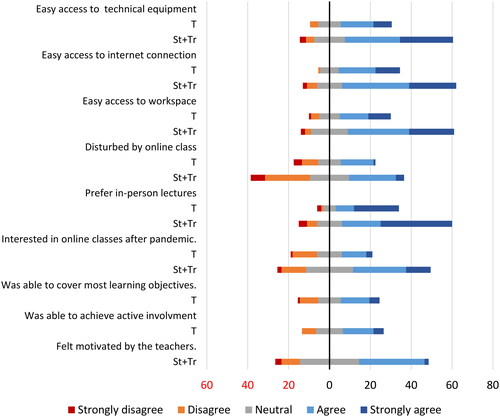
Only a few teachers and students/trainees experienced challenges accessing technical equipment, a suitable workspace or a stable internet connection for distance education – up to 12.5% of teachers and 9.3% of students/trainees ( and ). However, both teachers and students/trainees preferred when lectures/seminars were given in person.
Discussion
Main findings
This multi-centre study provides insight into the experience of students and teachers while transitioning from face-to-face to distance education in family medicine during the COVID-19 pandemic. All countries from the former Yugoslavia were represented, involving both under/postgraduate students and teachers. Less than a third of teachers and only 15% of trainees received formal training/preparation in distance education at the beginning of the COVID-19 pandemic. Synchronous teaching was the main method with only a third experiencing hybrid teaching. Students and teachers felt least confident about online assessment, and only half of the teachers could cover most learning objectives online. Most participants felt that lectures, case scenarios and seminars would be well suited to online education post-pandemic but not practical skills or patient consults.
Preparedness for distance education
Distance education in the pre-COVID-19 era was experienced more often by students/trainees than by teachers in our study. This was also reported in other studies, with most students having some earlier exposure to e-learning, unlike teachers with very limited experience [Citation15]. This will likely affect teachers’ ability to accept and adapt to new, online teaching methods.
Family medicine’s complexity is reflected in various teaching and assessment approaches, including lectures, small group work, one-on-one work with mentors in family medicine practices and self-study [Citation19,Citation20]. Specific learning objectives for family medicine are met if all of these approaches are integrated into different levels of medical education [Citation20]. The results of our study are concordant with other studies in which students rated the online formats as adequate for acquiring theoretical knowledge but less appropriate for learning procedural or clinical skills [Citation21–24]. As suggested by Michels and Windak [Citation3,Citation5], the challenge of transferring to distance family medicine education is to cover the variety of teaching and assessment methods necessary to reach the learning objectives. This is seen in our study, where only half of the teachers felt that most learning objectives had been achieved through online teaching. However, our findings also confirm that some elements of distance education in family medicine, like online lectures, can complement traditional face-to-face learning. Nevertheless, personal experience with patients in family medicine practices is essential for education and cannot be gained online.
Confidence and attitudes towards distance education
In our study, online assessment was found to be the area in which students and teachers felt least confident compared to other aspects of online education. This is probably due to the lack of experience and associated technical complexities. Researchers in Pakistan reported assessment difficulties, including validity, reliability of assessment and (dis)honesty of students [Citation25]. In the literature, several techniques that reproduced traditional methods have been suggested for addressing this challenge [Citation26], such as synchronous online assessments of knowledge based on multiple choice questions, Objectively Structured Practical/Clinical Examinations and video calls for assessing clinical reasoning and decision making in clinical cases or with virtual patients. Moreover, technology offers diverse assessment methods, engaging learners in both feedback and evaluation. It enables tailored knowledge tests, clinical performance assessments, or open-book online testing. While our participants predominantly appraised summative assessments, unrealised potential for online formative continuous assessments persists in the participating universities, possibly due to COVID-19 challenges and time constraints [Citation27].
Results similar to ours were found in the study by Motte-Signoret et al. where less than half of the teachers felt they provided teaching of an equivalent level and quality compared to earlier courses [Citation28]. In the study by Moya-Plana et al., teachers also expressed doubts about the quality of teaching and interaction with students during online teaching [Citation29].
Strengths and limitations
This is the first multinational study to investigate the impact of COVID-19 on teaching family medicine in the former Yugoslavia. Its main strength is that it is a multicentre study, involving both under/postgraduate teachers and students/family medicine trainees. The response from medical schools in the region was high, with 81% of family medicine departments participating. However, the response from individual students and staff was relatively low. Additionally, there is variation in the number of participants from individual countries. This is due to the varying sizes of family medicine departments and the availability of students/teachers. Heads of departments/FM representatives were invited to participate and recruit other teachers and students; those compelled may not represent the general teacher/student population. In addition, recall bias is possible given that students/teachers were surveyed several months after the easing of pandemic restrictions. Finally, most of the questionnaire was newly written for the study due to the lack of availability of a published questionnaire that suited our needs. We have published our questionnaires in full as a Supplementary file to compensate.
Implications for practice
The COVID-19 pandemic highlighted the importance of innovative teaching in family medicine. By combining new methods with traditional ones, educators can improve medical education. Personal experience remains vital; therefore, striking a balance between innovation and personal encounters is essential. To ensure integrity in digital learning and assessments, robust evaluation methods, including plagiarism detection and remote proctoring, are needed. Adapting to these changes enhances the overall quality of family medicine education.
Conclusion
Our study shows that through a combination of traditional and new approaches, teachers were able to provide students with a range of learning opportunities despite the constraints imposed by the COVID-19 pandemic. It also suggests that effective assessment strategies that leverage technology while addressing the possibility of cheating are needed to ensure the integrity of teaching practices and promote a better learning environment.
Acknowledgements
We thank Prof. Ana Marušić for critically reviewing our questionnaire. We are grateful to our esteemed colleagues for assisting with data collection: Olivera Batić-Mujanović, Edita Cerni Obrdalj, Ines Diminić Lisica, Larisa Gavran, Zaim Jatić, Zalika Klemens-Ketiš, Ilir Mencini, Branislava Milenković, Milena Rovčanin Cojić, Katarina Stavrić, Ljiljana Trtica Majnarić, Matilda Vojnović. We want to acknowledge all the medical students, family medicine trainees and teaching staff for contributing to this research.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- World Health Organization. WHO director-General’s opening remarks at the media briefing on COVID-19-11 March 2020 [Internet]. Geneva: Switzerland; 2020. [cited 2023 Nov 12]. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19–-11-march-2020.
- Gordon M, Patricio M, Horne L, et al. Developments in medical education in response to the COVID-19 pandemic: a rapid BEME systematic review: BEME guide no. 63. Med Teach. 2020;42(11):1–8. doi: 10.1080/0142159X.2020.1807484.
- Michels NRM, Scherpbier N, Karppinen H, et al. Do you know how COVID-19 is changing general practice/family medicine education? Educ Prim Care. 2020;31(3):196–197. doi: 10.1080/14739879.2020.1755609.
- Rose S. Medical student education in the time of COVID-19. J A m Med Assoc. 2020;323(21):2131–2132. doi: 10.1001/jama.2020.5227.
- Windak A, Frese T, Hummers E, et al. Academic general practice/family medicine in times of COVID-19– perspective of WONCA Europe. Eur J Gen Pract. 2020;26(1):182–188. doi: 10.1080/13814788.2020.1855136.
- de Nooijer J, Schneider F, Verstegen DM. Optimizing collaborative learning in online courses. Clin Teach. 2021;18(1):19–23. doi: 10.1111/tct.13243.
- O'Doherty D, Dromey M, Lougheed J, et al. Barriers and solutions to online learning in medical education – an integrative review. BMC Med Educ. 2018;18(1):130. doi: 10.1186/s12909-018-1240-0.
- Vallée A, Blacher J, Cariou A, et al. Blended learning compared to traditional learning in medical education: systematic review and meta-analysis. J Med Internet Res. 2020;22(8):e16504. doi: 10.2196/16504.
- Herrmann-Werner A, Erschens R, Zipfel S, et al. Medical education in times of COVID-19: survey on teachers’ perspectives from a German medical faculty. GMS J Med Educ. 2021;38(5):Doc93.
- Petek D, Kolšek M, Petek Šter M, et al. Undergraduate online teaching of family medicine during the epidemic with SARS-CoV-2. ZdravVestn. 2021;90(11–12):575–586. doi: 10.6016/ZdravVestn.3136.
- Puljak L, Čivljak M, Haramina A, et al. Attitudes and concerns of undergraduate university health sciences students in Croatia regarding complete switch to e-learning during COVID-19 pandemic: a survey. BMC Med Educ. 2020;20(1):416. doi: 10.1186/s12909-020-02343-7.
- Zakarija-Grković I, Cerovečki V, Vrdoljak D. Partial adoption of ‘minimal core curriculum’ in undergraduate teaching of family medicine: a cross-sectional study among Central and South-Eastern European medical schools. Eur J Gen Pract. 2018;24(1):155–159. doi: 10.1080/13814788.2018.1464555.
- Junod Perron N, Dominicé Dao M, Rieder A, et al. Online synchronous clinical communication training during the covid-19 pandemic. Adv Med Educ Pract. 2020;11:1029–1036. doi: 10.2147/AMEP.S286552.
- Li W, Gillies R, He M, et al. Barriers and facilitators to online medical and nursing education during the COVID-19 pandemic: perspectives from international students from low- and Middle-income countries and their teaching staff. Hum Resour Health. 2021;19(1):64. doi: 10.1186/s12960-021-00609-9.
- Li S, Zhang C, Liu Q, et al. E-learning during COVID-19: perspectives and experiences of the faculty and students. BMC Med Educ. 2022;22(1):328. doi: 10.1186/s12909-022-03383-x.
- Fitzgerald DA, Scott KM, Ryan MS. Blended and e-learning in pediatric education: harnessing lessons learned from the COVID-19 pandemic. Eur J Pediatr. 2022;181(2):447–452. doi: 10.1007/s00431-021-04149-1.
- Žuljević MF, Jeličić K, Viđak M, et al. Impact of the first COVID-19 lockdown on study satisfaction and burnout in medical students in split, Croatia: a cross-sectional presurvey and postsurvey. BMJ Open. 2021;11(6):e049590. doi: 10.1136/bmjopen-2021-049590.
- Petek D, Zakarija-Grković I, Stepanović A, et al. Transitioning from face-to-face to distance education. Part II: A qualitative study in the Former Yugoslavia during COVID-19. Eur J Gen Pract. 2023;1.
- Simmenroth A, Karppinen H. European education requirements for the undergraduate general practice/family medicine curriculum. 2020. [cited 2023 Nov 12]. https://euract.woncaeurope.org/sites/euractdev/files/documents/publications/others/bmeeducation-requirements-151220finalwith-we.pdf.
- Michels NRM, Maagaard R, Buchanan J, et al. Educational training requirements for general practice/family medicine specialty training: recommendations for trainees, trainers and training institutions. Educ Prim Care. 2018;29(6):322–326. doi: 10.1080/14739879.2018.1517391.
- Khalil R, Mansour AE, Fadda WA, et al. The sudden transition to synchronized online learning during the COVID-19 pandemic in Saudi Arabia: a qualitative study exploring medical students’ perspectives. BMC Med Educ. 2020;20(1):285. doi: 10.1186/s12909-020-02208-z.
- Dost S, Hossain A, Shehab M, et al. Perceptions of medical students towards online teaching during the COVID-19 pandemic: a national cross-sectional survey of 2721 UK medical students. BMJ Open. 2020;10(11):e042378. doi: 10.1136/bmjopen-2020-042378.
- Förster C, Eismann-Schweimler J, Stengel S, et al. Opportunities and challenges of e-learning in vocational training in general practice – a project report about implementing digital formats in the KWBW-Verbundweiterbildungplus. GMS J Med Educ. 2020;37(7):Doc97.
- Joseph JP, Joseph AO, Conn G, et al. COVID-19 pandemic-medical education adaptations: the power of students, staff and technology. Med Sci Educ. 2020;30(4):1355–1356. doi: 10.1007/s40670-020-01038-4.
- Afzal B, Mumtaz N, Shakil Ur Rehman S, et al. Teaching strategies for rehabilitation curriculum: coping with the covid-19 situation. J Pak Med Assoc. 2022;72(5):935–939. doi: 10.47391/JPMA.4220.
- Khan RA, Jawaid M. Technology enhanced assessment (TEA) in COVID 19 pandemic. Pak J Med Sci. 2020;36:S108–S110. doi: 10.12669/pjms.36.COVID19-S4.2795.
- Fuller R, Goddard VCT, Nadarajah VD, et al. Technology enhanced assessment: Ottawa consensus statement and recommendations. Med Teach. 2022;44(8):836–850. doi: 10.1080/0142159X.2022.2083489.
- Motte-Signoret E, Labbé A, Benoist G, et al. Perception of medical education by learners and teachers during the COVID-19 pandemic: a cross-sectional survey of online teaching. Med Educ Online. 2021;26(1):1919042.
- Moya-Plana A, Tselikas L, Lambotte O, et al. Postgraduate oncology educational shifts during the COVID-19 pandemic: results of faculty and medical student surveys. ESMO Open. 2022;7(2):100451. doi: 10.1016/j.esmoop.2022.100451.
