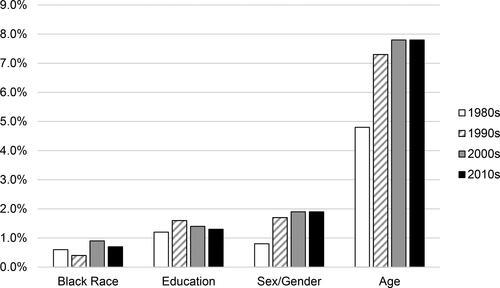
The racial strife that was exacerbated by the murder of George Floyd in the Spring of 2020 prompted many of us to reflect on race as a social justice issue in clinical neuropsychology. As a specialty in which White Americans have historically been over-represented (Sweet et al., Citation2021), how much do Black lives really matter to clinical neuropsychology? Of course, the broader Civil Rights movement has been active for decades and the racial inequities in psychological science, training, and practice have existed for even longer (Guthrie, Citation2004). Importantly, they are inextricably linked and relevant to clinical neuropsychology. Black Americans experience marked health disparities and are over-represented in many of the clinical populations that neuropsychologists serve (e.g. vascular disease, dementia, and infectious disease). And yet, fewer than 1% (n = 75) of the nearly 11,000 articles published in our field’s six major journals since 1985 focus specifically on Black Americans. As seen in , the limited emphasis on Black Americans in our neuropsychological research has not improved meaningfully in 35 years, as publication frequencies fall reliably below studies focused on other sociodemographic factors such as age, sex/gender, and education/literacy (ps < .0001). A majority of the neuropsychological articles on Black Americans emphasize race-based test score discrepancies, psychometrics, and norms (e.g. Heverly et al., Citation1986). Although such psychometric studies have value, they are nevertheless fraught with thorny interpretive issues (e.g. Manly & Echemendia, Citation2007; Possin et al., Citation2021) and represent only a small part of the brain health needs of Black Americans. Moreover, race is a social, rather than biological, construct, and the issues associated with race and brain health are tremendously complex and cannot be resolved with an exclusive psychometric focus.
Figure 1. Percentage of 10,531 article titles that focus on specific demographic issues in six major clinical neuropsychology journals between 1985 and 2020 (NB. data were drawn from the sample of articles detailed in Matchanova et al., in press).
Inspired by the Black Lives Matter academic strike (Nature, Citation2020), this special issue was a call to action for clinical neuropsychologists to use their platform as clinician-scientists to promote the brain health and quality of life of Black Americans. The special issue begins with two systematic reviews examining the representation of Black Americans in neuropsychological studies. Historically, well over half of articles in clinical neuropsychology journals fail to include even basic descriptive data on race/ethnicity (Medina et al., Citation2021). And even when race/ethnicity data are reported, they are commonly ignored or treated as a “nuisance” confounding variable, rather than as a thoughtful focus of prospective investigation. In this special issue, Pugh et al. (Citation2022) estimated that Black Americans – who represent 13.4% of the U.S. population – comprise only 10.7% of the participants in neuropsychological research published over the last decade. The under-representation of Black Americans is particularly evident in studies of older adults, chronic medical conditions, and neurological disorders. In a parallel review, Ray et al. (Citation2022) observed that two-thirds of neuropsychological studies that reported race/ethnicity did not include a sufficient epidemiological representation of Black Americans. A staggering 39% of those studies do not include a single Black participant. These data underscore the importance neuropsychologists moving beyond simplistic checklist recruitment approaches. Modern inclusion science approaches are needed to emphasize community engagement and genuine partnership in developing research questions, designing study measures, recruiting and retaining participants, and integrating the study findings back into the community (George et al., Citation2014).
The other 13 articles in this special issue provide new insights on Black Americans living with different clinical conditions that affect brain structure and function. Two of the studies in this special issue focus specifically on Black children. Miller et al. (Citation2022) describe the benefits of educational decision-making empowerment in caregivers of children with sickle cell disease. Wexler et al. (Citation2022) present data on the importance of informant source in interpreting symptom ratings of Black children being evaluated for Attention-Deficit/Hyperactivity Disorder (Wexler et al., Citation2022). Four articles report on issues related to the diagnosis (Graves et al., Citation2021; Salo et al., Citation2022), trajectory (Johnson et al., Citation2022), and care (Pereira et al., Citation2022) of older Black American adults with neurocognitive disorders. Three additional papers describe the neurocognitive aspects of human immunodeficiency virus (HIV) disease in Black Americans, focusing on health literacy (Beltran-Najera et al., Citation2022), comorbid conditions (Thames et al., Citation2022), and associations with daily functioning (Thompson et al., Citation2022). The final four studies help emphasize the “psychology” in clinical neuropsychology by exploring psychological factors that can affect the brain health of Black Americans, including vascular depression (Bogoian & Dotson, Citation2022), illness representation (Gupta et al., Citation2022), gendered racism (Hill-Jarrett & Jones, Citation2022), and stereotype threat (Van Landingham et al., Citation2022).
The publication of this special issue during Black History Month in the United States was intended to encourage clinical neuropsychologists to reflect on historical issues related to race and to foster creative thinking about brain health equity for Black Americans. Although the content of this special issue represents some progress in increasing the representation of Black Americans in neuropsychological research, we have a long way to go on the road toward brain health equity. We call for organized research efforts and funding to evaluate important questions, such as: (1) What are the presentations, clinical features, and needs of Black Americans with central nervous system disease? (2) How can we develop and use brain-behavior assessments in ways that mitigate racial bias and better reflect the needs of underserved groups? (3) How does race interface with health literacy and psychological factors (e.g. discrimination) to affect the engagement of Black Americans with neuropsychological services and their uptake? (4) How does race influence “established” phenomena in clinical neuropsychology (e.g. the inter-relationships between neuropsychological functions and well-known factors such as other demographics or self-report of cognitive symptoms)? We call on researchers to move beyond comparing Black Americans to White Americans as the “gold standard” of inclusive research. We call on publishers, editors, reviewers, and authors to normalize the full reporting and thoughtful consideration of race as a potential factor in their work. We call on clinical neuropsychologists to engage with underserved communities and listen carefully to their needs. Finally, we call for concerted efforts to better engage, attract, and retain Black Americans in neuropsychological training programs and professional leadership positions.
Acknowledgements
We are grateful to the thousands of participants who contributed their time and effort to these studies, to the outstanding research teams that responded to this call to action, to the many new and seasoned reviewers who provided helpful critiques of these studies, and to Dr. Yana Suchy and the TCN editorial team for their support and efforts behind the scenes. Thank you all!
Disclosure statement
No potential conflict of interest was reported by the authors.
Funding
The author(s) reported there is no funding associated with the work featured in this article.
References
- Beltran-Najera, I., Thompson, J. L., Matchanova, A., Sullivan, K. L., Babicz, M. A., & Woods, S. P. (2022). Neurocognitive performance differences between black and white individuals with HIV disease are mediated by health literacy. The Clinical Neuropsychologist, 36(2), 414–430. https://doi.org/https://doi.org/10.1080/13854046.2021.1953147
- Bogoian, H. R., & Dotson, V. M. (2022). Vascular depression in Black Americans: A systematic review of the construct and its cognitive, functional, and psychosocial correlates. The Clinical Neuropsychologist, 36(2), 431–461. https://doi.org/https://doi.org/10.1080/13854046.2021.1933188
- George, S., Duran, N., & Norris, K. (2014). A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. American Journal of Public Health, 104(2), e16–e31. https://doi.org/https://doi.org/10.2105/AJPH.2013.301706
- Graves, L. V., Edmonds, E. C., Thomas, K. R., Weigand, A. J., Cooper, S., Stickel, A. M., Zlatar, Z. Z., Clark, A. L., & Bondi, M. W. (2022). Diagnostic accuracy and differential associations between ratings of functioning and neuropsychological performance in non-Hispanic Black and White older adults. The Clinical Neuropsychologist, 36(2), 287–300. https://doi.org/https://doi.org/10.1080/13854046.2021.1971766
- Gupta, S. K., Margolis, S. A., Grant, A. C., Gonzalez, J. S., & Nakhutina, L. (2022). Relationships among illness representations and depressive symptom severity in predominantly African-American and Caribbean-American people with epilepsy. The Clinical Neuropsychologist, 36(2), 462–468. https://doi.org/https://doi.org/10.1080/13854046.2021.1923802
- Guthrie, R. V. (2004). Even the rat was white: A historical view of psychology. Pearson/Allyn and Bacon.
- Heverly, L. L., Isaac, W., & Hynd, G. W. (1986). Neurodevelopmental and racial differences in tactile-visual (cross-modal) discrimination in normal black and white children. Archives of Clinical Neuropsychology: The Official Journal of the National Academy of Neuropsychologists, 1(2), 139–145.
- Hill-Jarrett, T. G., & Jones, M. K. (2022). Gendered racism and subjective cognitive complaints among older black women: The role of depression and coping. The Clinical Neuropsychologist, 36(2), 479–503. https://doi.org/https://doi.org/10.1080/13854046.2021.1923804
- Johnson, E. E. H., Alexander, C., Lee, G. J., Angers, K., Ndiaye, D., & Suhr, J. (2022). Examination of race and gender differences in predictors of neuropsychological decline and development of Alzheimer’s disease. The Clinical Neuropsychologist, 36(2), 327–352. https://doi.org/https://doi.org/10.1080/13854046.2021.1940299
- Manly, J. J., & Echemendia, R. J. (2007). Race-specific norms: Using the model of hypertension to understand issues of race, culture, and education in neuropsychology. Archives of Clinical Neuropsychology, 22(3), 319–325. https://doi.org/https://doi.org/10.1016/j.acn.2007.01.006
- Matchanova, A. M., Avci, G., Babicz, M. A., Thompson, J. L., Johnson, B., Ke, I. J., Rahman, S., Sullivan, K. L., Sheppard, D. P., Morales, Y., Tierney, S. M., Kordovski, V. M., Beltran-Najera, I., Ulrich, N., Pilloff, S., Yeates, K. O., & Woods, S. P. (in press). Gender disparities in the author bylines of articles published in clinical neuropsychology journals from 1985 to 2019. The Clinical Neuropsychologist, 1–18. https://doi.org/https://doi.org/10.1080/13854046.2020.1843713
- Medina, L. D., Torres, S., Gioia, A., Ochoa Lopez, A., Wang, J., & Cirino, P. T. (2021). Reporting of demographic variables in neuropsychological research: An update of O’Bryant et al.’s trends in the current literature. Journal of the International Neuropsychological Society, 27(5), 497–507. https://doi.org/https://doi.org/10.1017/S1355617720001083
- Miller, M., Landsman, R., Scott, J. P., & Heffelfinger, A. K. (2022). Fostering equity in education and academic outcomes in children with sickle cell disease. The Clinical Neuropsychologist, 36(2), 245–263. https://doi.org/https://doi.org/10.1080/13854046.2021.1945147
- Nature. (2020). Thousands of scientists worldwide to go on strike for Black lives. Nature. https://doi.org/https://doi.org/10.1038/d41586-020-01721-x
- Pereira, C., LaRoche, A., Arredondo, B., Pugh, E., Disbrow, E., Reekes, T. H., Brickell, E., Boettcher, A., & Sawyer, R. J. (2022). Evaluating racial disparities in healthcare system utilization and caregiver burden among older adults with dementia. The Clinical Neuropsychologist, 36(2), 353–366. https://doi.org/https://doi.org/10.1080/13854046.2021.1951844
- Possin, K. L., Tsoy, E., & Windon, C. C. (2021). Perils of race-based norms in cognitive testing: The case of former NFL players. JAMA Neurology, 78(4), 377–378. https://doi.org/https://doi.org/10.1001/jamaneurol.2020.4763
- Pugh, E., Robinson, A., De Vito, A. N., Bernstein, J., & Calamia, M. (2022). Representation of U.S. Black Americans in neuropsychology research: How well do our reporting practices show that Black lives matter? The Clinical Neuropsychologist, 36(2), 216–226. https://doi.org/https://doi.org/10.1080/13854046.2021.1958923
- Ray, C., Anderson, K., Hudson, M., George, E., Bisignano, N., & Montgomery, V. (2022). Current status of inclusion of Black participants in neuropsychological studies: A scoping review and call to action. The Clinical Neuropsychologist, 36(2), 227–244. https://doi.org/https://doi.org/10.1080/13854046.2021.2019314
- Salo, S. K., Marceaux, J. C., McCoy, K., & Hilsabeck, R. C. (2022). Removing the noose item from the Boston Naming Test: A step toward antiracist neuropsychological assessment. The Clinical Neuropsychologist, 36(2), 311–326. https://doi.org/https://doi.org/10.1080/13854046.2021.1933187
- Sweet, J. J., Klipfel, K. M., Nelson, N. W., & Moberg, P. J. (2021). Professional practices, beliefs, and incomes of U.S. neuropsychologists: The AACN, NAN, SCN 2020 practice and "salary survey". The Clinical Neuropsychologist, 35(1), 7–80. https://doi.org/https://doi.org/10.1080/13854046.2020.1849803
- Thames, A. D., Nunez, R., Slavich, G. M., Irwin, M. R., & Senturk, D. (2022). Racial differences in health and cognition as a function of HIV among older adults. The Clinical Neuropsychologist, 36(2), 367–387. https://doi.org/https://doi.org/10.1080/13854046.2021.1967449
- Thompson, J. L., Beltran-Najera, I., Johnson, B., Morales, J., & Woods, S. P. (2022). Evidence for neuropsychological health disparities in Black Americans with HIV disease. The Clinical Neuropsychologist, 36(2), 388–413. https://doi.org/https://doi.org/10.1080/13854046.2021.1947387
- Van Landingham, H., Ellison, R. L., Laique, A., Cladek, A., Khan, H., Gonzalez, C., & Dunn, M. R. (2022). A scoping review of stereotype threat for BIPOC: Cognitive effects and intervention strategies for the field of neuropsychology. The Clinical Neuropsychologist, 36(2), 503–522. https://doi.org/https://doi.org/10.1080/13854046.2021.1947388
- Wexler, D., Salgado, R., Gornik, A., Peterson, R., & Pritchard, A. (2022). What’s race got to do with it? Informant rating discrepancies in neuropsychological evaluations for children with ADHD. The Clinical Neuropsychologist, 36(2), 264–286. https://doi.org/https://doi.org/10.1080/13854046.2021.1944671
