?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Context: The resistance of bacteria to antibiotics is raising serious concern globally. Asian medicinal plants could improve the current treatment strategies for bacterial infections. The antibacterial properties of medicinal plants used by the Khyang tribe in Bangladesh have not been investigated.
Objective: The present study examines the antibacterial properties of 18 medicinal plants used by the Khyang tribe in day-to-day practice against human pathogenic bacteria.
Materials and methods: Leaves, bark, fruits, seeds, roots and rhizomes from collected plants were successively extracted with hexane, ethyl acetate and ethanol. The corresponding 54 extracts were tested against six human pathogenic bacteria by broth microdilution assay. The antibacterial mode of actions of phytoconstituents and their synergistic effect with vancomycin and cefotaxime towards MRSA was determined by time-killing assay and synergistic interaction assay, respectively.
Results and discussion: Hexane extract of bark of Cinnamomum cassia (L.) J. Presl. (Lauraceae) inhibited the growth of MRSA, Enterococcus faecalis, Escherichia coli, Pseudomonas aeruginosa, Klebsiella pneumoniae and Acinetobacter baumannii with MIC values below 100 µg/mL. From this plant, cinnamaldehyde evoked at 4 × MIC in 1 h an irreversible decrease of MRSA count Log10 (CFU/mL) from 6 to 0, and was synergistic with vancomycin for MRSA with fractional inhibitory concentration index of 0.3.
Conclusions: Our study provides evidence that the medicinal plants in Bangladesh have high potential to improve the current treatment strategies for bacterial infection.
Introduction
The resistance of bacteria to antibiotics has increased to such extend that the World Health Organization (WHO) warns of a ‘post-antibiotic era’ (O’Neill Citation2014; WHO Citation2014). In 1998, 5% of Escherichia coli isolated from hospitals in the Netherlands were resistant to fluoroquinolones (Goettsch et al. Citation2000). In 2014, five out of six WHO regions were affected with 50% or more resistance of Escherichia coli to fluoroquinolone (WHO Citation2014). Carbapenem-resistant Klebsiella pneumoniae has first been reported in Scotland in the late nineties (MacKenzie et al. Citation1997). In 2005, 3.3% Klebsiella pneumoniae isolates were resistant to carbapenem in Brooklyn hospitals (Bratu et al. Citation2005). In 2014, two out of six WHO regions reported 50% or more resistance of Klebsiella pneumoniae to carbapenem (WHO Citation2014). Today Acinetobacter baumannii (Moraxellaceae) resists almost all known antibiotics (Peleg et al. Citation2008). The resistance of Staphylococcus aureus (Staphylococcaceae) to methicillin emerged in 1961 (Jevons Citation1961). Methicillin-resistant Staphylococcus aureus (MRSA) is now resistant to vancomycin and cefotaxime and poses a threat to human health (Fung-Tomc et al. Citation1988; Neu Citation1992; Stryjewski and Corey Citation2014).
In an attempt to control bacterial resistance, WHO recommends ‘to develop the economic case for sustainable investment that takes account of the needs of all countries and to increase investment in new medicines’ (WHO Citation2014). However, approval for new antibacterial agent by the FDA has been decreasing (Charles and Grayson Citation2004; Spellberg et al. Citation2004). According to Alanis (Citation2005), the traditional antibiotic structures have been almost exhausted to the point that antibacterial research is literally crying for new chemical entities that could be found by using fresh and different research approaches. Medicinal plants in Asia have the ability to synthesize a fascinating array of low molecular weight molecules with structures completely unrelated to antibiotics. One example is the alkaloid berberine produced by Tinospora cordifolia (Willd.) Miers ex Hook. f. & Thomson (Menispermaceae), a woody climber used in Bangladesh for the treatment of tuberculosis, cough and fever (Jahan et al. Citation2010). This phytoconstituent not only inhibits the growth of Gram-positive cocci Streptococcus agalactiae (Streptococcaceae) (Peng et al. Citation2015), but enhances the sensitivity of Staphylococcus strains towards antibiotics (Wojtyczka et al. Citation2014). In addition, medicinal plants produce inhibitors of bacterial resistance (Stermitz et al. Citation2000). Essential oil of coriander increases the sensitivity of Acinetobacter baumannii to tetracycline (Duarte et al. Citation2012). During the last few decades, scientists from all over the world are paying much more attention to the studies of an emerging branch of science, ethnobiology, especially to tribal medicine or ethnomedicine. Since 1980s, Bangladesh with 5500 plant species and more than 100 tribal communities belonging to over a dozen linguistic groups residing in various parts of the country with diversified plant species, varied culture, and a rich traditional knowledge system, possess an ethnobotanical emporia. Due to living close to nature, the tribal communities are custodians of an unique traditional knowledge system about ambient flora, fauna, and a rich heritage of phytomedicine or ethnomedicine. Since most of these ethnic communities do not have their written scripts and language, the information about prescriptions, pharmacology, attitude towards diseases, diagnosis, etc., of the age-old tribal medicines is lying unclaimed. The people relating to advanced societies are not aware of this rich knowledge system. A country like Bangladesh has many tropical rainforest plants rich with medicinal values (Rahmatullah et al. Citation2010). The Khyang tribe lives in a remote area and no reports exist on their medicinal plant use. In this context, we examined the antibacterial properties of medicinal plants used by Khyang tribe in Bangladesh by broth microdilution, time-killing and synergistic interaction assay. The aims of our study were: (i) to examine antibacterial properties of 18 medicinal plants of Bangladesh towards a panel of human pathogenic bacteria, (ii) to examine the antibacterial property of at least one major phytoconstituent from the most active plant, (iii) to determine the mode of action (i.e., bacteriostatic or bactericidal) of this phytoconstituent and (iv) and to determine the effect of the phytoconstituent on the sensitivity of MRSA to vancomycin and cefotaxime. The ultimate goal of our study is to contribute to the development of safe, effective and inexpensive plant-based materials to improve the current treatment strategies for bacterial infections.
Materials and methods
Medicinal plants collection
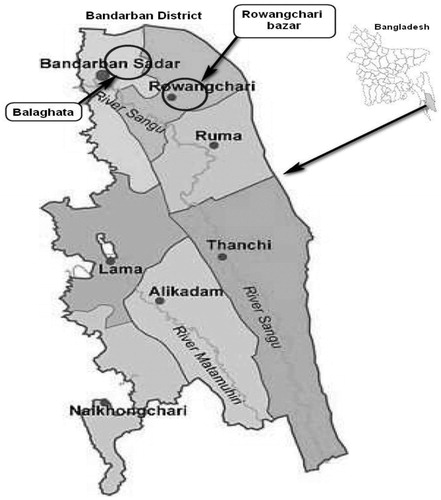
A two-month survey for evaluation and documentation of the use of medicinal plants used for the day-to-day treatment of common diseases by traditional healers in Khyang tribe Bangladesh was performed from 5–30 April 2015 according to ethnopharmacological criteria (Cotton Citation1996). The survey was done on the Khyang tribe residing in villages adjoining Rowangchari bazar and Balaghata village in Bandarban district, Chittagong Hill Tracts, Bangladesh (). Information gathered allowed the collection of 18 medicinal plants (), which were identified by Professor M. Atique Rahman, University of Chittagong. Voucher herbarium specimens with vernacular names, collecting localities, and dates of collections were deposited at the Medicinal Plants Collection Wing, Department of Pharmacy, University of Development Alternative, Dhaka, Bangladesh. After screening of superfluous matter, the collected leaves, bark, roots, rhizomes, seeds or fruits were separated and air-dried at room temperature for 2 weeks. The dried materials were then finely pulverized by grinding using aluminium collection blender (Philips, Shanghai, China) and the powders obtained were weighted with top loading balance (Sartorius AG, Göttingen, Germany).
Table 1. Traditional therapeutic properties of 18 medicinal plants from Bangladesh.
Medicinal plants extraction
The plant powders (20–60 g) were mixed at room temperature sequentially with organic solvents of increasing polarity starting with hexane (Friendemann Schmidt, Parkwood, Australia), ethyl acetate (Friendemann Schmidt, Parkwood, Australia) and 95% (v/v) ethanol (AR grade, John Kollin Corporation, Midlothian, UK) for differential extraction of non-polar, mid-polar and polar extracts, respectively (Harborne Citation1998). Each extraction was performed in triplicate by maceration of plant powder-to-solvent ratio of 1:5 (w/v) for three days at room temperature. The respective liquid extracts were subsequently filtered through qualitative filter papers No. 1 (Whatman International Ltd., Maidstone, UK) using aspirator pump (EW-35031-00, 18 L/min, 9.5 L Bath, 115 VAC), and the filtrates were concentrated to dryness under reduced pressure at 40 °C using rotary evaporator (Buchi Labortechnik AG, Flawil, Switzerland). The dry extracts obtained were weighed with an analytical balance (Sartorius AG, Göttingen, Germany) and stored in tightly closed glass scintillation vials (Kimble, Rockwood, TN) at −20 °C until further use. For stock solutions, each crude extract was dissolved in 100% dimethyl sulphoxide (DMSO) (R&M Chemicals, Chelmsford, UK) to a concentration of 100 µg/µL. A yield for each extract was calculated.
Tested bacterial strains
Stock cultures of bacteria used for this study were kindly provided by the Department of Medical Microbiology, Faculty of Medicine, University of Malaya. The following human pathogenic bacteria were used as tested organisms: Gram positive organisms MRSA (University of Malaya Hospital clinical isolate), Enterococcus faecalis (ATCC 29212) and Gram negative organisms Escherichia coli (ATCC 25922), Pseudomonas aeruginosa (ATCC 15442), Klebsiella pneumoniae (University of Malaya Hospital clinical isolate) and Acinetobacter baumannii (University of Malaya Hospital clinical isolate).
Phytoconstituents and control antibiotics
Cinnamaldehyde, eugenol, gallic acid, rifampicin, vancomycin and cefotaxime were purchased from Sigma-Aldrich (St. Louis, MO, >98% purity).
Broth microdilution assay
Determination of minimum inhibitory concentration (MIC) was performed according to the Clinical and Laboratory Standards Institute guidelines (CLSI Citation2012). Briefly, bacterial strains were grown for 18–24 h at 37 °C. Direct suspension of the colonies were made in cationically adjusted Müeller-Hinton broth (CAMHB) and adjusted to OD625 0.08–0.1 which corresponds to 1–2 × 108 CFU/mL followed by serial 10-fold dilutions to give 1 × 106 CFU/mL. Bacterial suspension (50 µL) was added to 96-well round bottom microtiter plates containing an equal volume of extracts or phytoconstituents at different concentrations and the 96-well plates were incubated for 24 h at 37 °C. The MIC is defined as the lowest concentration of material tested that completely inhibits the growth of bacteria. Minimum bactericidal concentration (MBC) was determined by sub-culturing the test dilutions on to a sterile agar plate and incubated further for 18–24 h. The highest dilution that yielded 0% bacterial growth on agar plates was taken as MBC. Both MIC and MBC values were calculated as the mean of triplicate experiments. Vancomycin and rifampicin were used as positive control antibiotics.
Time-killing assay
Time-killing assay was conducted according to Giacometti et al. (Citation1999). Bacteria (1 × 106 CFU/mL) were incubated with cinnamaldehyde, eugenol, vancomycin or cefotaxime at 1 × MIC in Müeller-Hinton broth (MHB) at 37 °C. Bacterial suspensions (10 μL) were removed at various time intervals (1, 2, 3, 4 and 5 h), serially diluted in PBS, and plated onto Müeller-Hinton agar with 20–24 h at 37 °C to obtain viable colonies. Bacteria count Log10 values were calculated as the mean of triplicate experiments.
Synergistic interaction assay
The ability of the hexane extract of bark of Cinnamomum cassia (L.) J. Presl. (Lauraceae), cinnamaldehyde and eugenol to increase the sensitivity of MRSA towards cefotaxime or vancomycin was measured by fractional inhibitory concentration (FIC) indices (FICIs) (Giacometti et al. Citation1999). Vancomycin was selected because the resistance of Gram-positive bacteria to this glycopeptide is a source of concern for clinicians (Courvalin Citation2006). FICI is the sum of the FIC of compound and FIC of antibiotic calculated according to the following formula (Berenbaum Citation1978):
The FICI results are interpreted as such: ≤0.5 synergistic, 0.5–1 additive, 1–4 indifferent; ≥4 antagonistic (Schelz et al. Citation2006).
Results and discussion
Medicinal plants collection
Survey for evaluation and documentation of the use of medicinal plants used in day-to-day practice by Khyang tribe residing in villages adjoining Rowangchari bazar and Balaghata village in Bandarban district, Chittagong Hill Tracts, Bangladesh () conducted from 5–30 April 2015 afforded the collection of 18 plants from 11 different families (). Twelve medicinal plants out of 18 were used to treat infections and all these belong to families known to accumulate essential oils except Terminalia bellirica (Gaern.) Roxb. (Combretaceae) (Takhtajan Citation2009). The ability of plants to synthesize and accumulate essential oils is not omnipresent in plants but scattered throughout the plant kingdom in certain families (Baser and Buchbauer Citation2015). Kar and Jain (Citation1971) suggested that most of the anti-infectious traditional properties of aromatic plants enlisted in indigenous system of medicine are due to their essential oil contents. Essential oils are antibacterial (Deans and Ritchie Citation1987).
Percentage yields
The yields of extracts were calculated using the following formula:
Dried plant parts were successively extracted with hexane, ethyl acetate and ethanol to obtain lipophilic (non-polar), amphiphilic (mid-polar) and hydrophilic (polar) extracts, respectively (Harborne Citation1998). The average yield values ranged from 2.3 to 10.8% indicating good extraction process (Parthasarathy et al. Citation2008) (). Calculated averages yields for hexane, ethyl acetate and ethanol extracts were 10.8, 3.6 and 2.3%, respectively. Hexane extracts had the highest average extraction yields confirming the predominance of lipophilic natural products in the plant parts extracted (Harborne Citation1998).
Table 2. Percentage yields (w/w).
Broth microdilution assay
We sought to determine the MIC of 54 extracts from the 18 plants collected by broth microdilution method (Reller et al. Citation2009). Results of broth microdilution assay confirmed that Gram-positive bacteria were more susceptible than Gram-negative bacteria (). Rios and Recio (Citation2005) suggested that crude extract with MIC superior to 1000 µg/mL is inactive and proposed interesting activity for MIC of 100 µg/mL and below. Fabry et al. (Citation1998) defined active crude extracts as having MIC values below 8000 µg/mL. Kuete (Citation2010) and Cos et al. (Citation2006) use a stricter endpoint criteria, in which crude extracts with MIC values less than 100 µg/mL are active. Further, Kuete (Citation2010) classifies as weakly active extracts with MIC above 625 µg/mL. Following Cos et al. (Citation2006) and Kuete (2010), three plants had interesting activities with MIC below 100 µg/mL for at least one of the bacteria tested (). The lowest MIC towards MRSA was demonstrated by the hexane extract of Mentha arvensis L. (Lamiaceae) (24.3 µg/mL). According to Krishnan et al. (Citation2010), antibacterial extracts or compounds are categorized into two classes: bacteriostatic (MBC/MIC ratio >4) and bactericidal (MBC/MIC ratio ≤4). Following this classification, hexane extract of Mentha arvensis with MBC/MIC ratio above 61.7 was bacteriostatic for MRSA; this extract was bacteriostatic for E. coli and bactericidal for A. baumannii. A body of experimental evidence demonstrates that it is not unusual for extracts to demonstrate equal MIC and MBC values. For instance, the ethanol extract of galls of Quercus infectoria Olivier (Fagaceae) inhibited the growth of MRSA with MIC and MBC values of 1600 µg/mL (Wan et al. Citation2014). Ethyl acetate extract of Mentha piperita L. (Lamiaceae) inhibited the growth of E. faecalis with MIC and MBC values of 2.5 mg/mL (Shalayel et al. Citation2017). The ethanol extract of Terminalia bellirica was strongly bactericidal for A. baumannii with MIC and MBC of 11.7 µg/mL. Hexane extract of bark of Cinnamomum cassia had the broadest spectrum of activity with notably a bactericidal effect for A. baumannii with MIC of 11.7 µg/mL.
Table 3. Minimum inhibitory concentrations (MIC) by broth microdilution assay.
Cinnamaldehyde is the major constituent of essential oil of Cinnamomum cassia bark (Tisserand and Young Citation2013), which also contains some eugenol (about 10%) (Lockwood Citation1979). Eugenol is also a component of Mentha arvensis (Vivek et al. Citation2009). Gallic acid is a major constituent of Terminalia bellirica (Latha and Daisy Citation2011). The antibacterial potency of these phytoconstituents was quantitatively examined by broth dilution method (). Rios and Recio (Citation2005) suggested that MIC superior to 100 µg/mL for phytoconstituent was to be avoided because it is mildly active and proposed interesting activity with MIC of 10 µg/mL and below. According to Kuete (Citation2010), the antibacterial activity of pure compounds is classified into three categories: MIC < 10 µg/mL: high; MIC between 10 and 100 µg/mL: medium and low for MIC above 100 µg/mL. Following both these classifications, eugenol with an MIC of 11.7 µg/mL and MIC/MBC ratios of 1.0 was strongly bactericidal against E. faecalis, E. coli and K. pneumoniae. Cinnamaldehyde was strongly bactericidal for E. faecalis. Ooi et al. (Citation2006) tested the essential oil of Cinnamomum cassia bark and its major constituent cinnamaldehyde against a panel of bacteria and recorded activity against S. aureus and P. aeruginosa with MIC ranging from 75 to 600 µg/mL. Cinnamaldehyde, eugenol and gallic acid were moderately bactericidal for MRSA. Plant phenols, including eugenol are known for their membrane-disturbing activities (Sikkema et al. Citation1995). This mechanism of activity could at least account for the antibacterial properties of gallic acid (Smith et al. Citation2005; Borges et al. Citation2013). The different spectrum of activity between cinnamaldehyde and eugenol could at least be explained by the fact that polar antibacterial agents can pass the outer membrane through porin channels, whereas the outer membrane serves as a penetration barrier towards macromolecules (like vancomycin) and to non-polar compounds, and it is for this reason that Gram-negative bacteria are relatively resistant to non-polar molecules (Nikaido and Vaara Citation1985).
Table 4. Minimum inhibitory concentrations (MIC) and minimum bactericidal concentrations (MBC) of three phytoconstituents by broth microdilution assay.
Time-killing assay
Cinnamaldehyde and eugenol were tested against MRSA for time-killing assay as this bacterium represents the greatest current medical need (Ling et al. Citation2015). The result of time-killing assay is presented in . A perusal of this table shows that cinnamaldehyde (4 × MIC) and eugenol at both 2 and 4 × MIC evoked at 1 h a fall of Log10 (CFU/mL) bacteria count from 6 to 0. This effect was permanent confirming bactericidal activity. Gill and Holley (Citation2006) made the demonstration that cinnamaldehyde at high concentration was bactericidal on E. coli via inhibition of membrane-bound ATPase activity. This small molecular weight molecule being lipophilic may penetrate and destabilize the cytoplasmic membrane of MRSA leading to nutrients and energy depletion (Sikkema et al. Citation1995). In previous study, cinnamaldehyde was inhibitory for the growth of the enteric bacteria but exhibited neither outer membrane-disintegrating activity nor depletion of intracellular ATP (Helander et al. Citation1998). In addition, aldehyde group conjugated to a carbon to carbon double bond is a highly electronegative arrangement, which may explain the observed activity (Moleyar and Narasimham Citation1986). Such electronegative compounds may interfere in biological processes involving electron transfer and reaction with vital nitrogen components, e.g., proteins and nucleic acids, and therefore inhibit the growth of the microorganisms. Cinnamaldehyde may also bind to amino acids in enzymes via its carbonyl group (Wendakoon and Sakaguchi Citation1993).
Table 5. Time-killing assay of eugenol and cinnamaldehyde against methicillin-resistant Staphylococcus aureus.
Synergistic interaction assay
Cinnamaldehyde has been reported to be synergistic with ampicillin, penicillin, tetracycline or novobiocin against E. coli (Palaniappan and Holley Citation2010). Eugenol is a constituent of Cinnamomum cassia bark. In this context, we sought to determine the synergy effects of the hexane extract of Cinnamomum cassia bark, cinnamaldehyde and eugenol with vancomycin and cefotaxime towards MRSA (). Both extract and cinnamaldehyde did not increase the sensitivity of MRSA to cefotaxime. However, we observed that cinnamaldehyde has a high synergistic effect with vancomycin with an FICI of 0.3. We do not know by which mechanism cinnamaldehyde increases the sensitivity of MRSA to vancomycin. Eugenol with FICI above 4 was antagonistic for both antibiotics. Bacteria resist vancomycin by mutating a gene coding for terminal d-Ala-d-Ala in the peptidoglycan wall resulting in Ala-d-Lac resulting in 1000 decreased affinity of vancomycin (Walsh Citation2000). Wright (Citation2000) proposed to develop agents ‘resisting’ resistance as a strategy to fight superbugs and cinnamaldehyde showing no unreasonable adverse effects to humans (Cocchiara et al. Citation2005) is an exciting candidate. Only with exact knowledge of the mechanisms underlying the synergy effect observed, it will be possible to develop a new generation of safe and standardized with high efficacy (Wagner and Ulrich-Merzenich Citation2009).
Table 6. Fractional inhibitory concentration index (FICI) of different combination of hexane extract of Cinnamomum cassia, cinnamaldehyde or eugenol, and antibiotics against methicillin-resistant Staphylococcus aureus.
Conclusions
Over the past few decades, there has been a dramatic decrease in the number of new antibiotic approved by the FDA. MRSA is a cause for concern due to the small number of antibiotics effective against this organism and resistance associated with their uses. The development of resistant-modifying agents could be a supplemental strategy to overcome resistance. The current result shows that Cinnamomum cassia has a broad-spectrum antibacterial activity. From this plant, cinnamaldehyde is a resistant-modifying agent that decreases the resistance of MRSA to vancomycin. Our study provides evidence that the medicinal plants in Bangladesh have high potential for the development of plant-based material to improve the current treatment strategies for bacterial infections.
Acknowledgements
We are grateful to Professor Atique Rahman, Department of Botany, Biological Science Faculty, University of Chittagong, Chittagong, Bangladesh for identifying the plants.
Disclosure statement
We have no conflict of interest to declare.
Additional information
Funding
References
- Alanis AJ. 2005. Resistance to antibiotics: are we in the post-antibiotic era? Arch Med Res. 36:697–705.
- Baser KHC, Buchbauer G. 2015. Handbook of essential oils: science, technology, and applications. Boca Raton (FL): CRC Press.
- Berenbaum MC. 1978. A method for testing for synergy with any number of agents. J Infect Dis. 137:122–130.
- Borges A, Ferreira C, Saavedra MJ, Simoes M. 2013. Antibacterial activity and mode of action of ferulic and gallic acids against pathogenic bacteria. Microb Drug Resist. 19:256–265.
- Bratu S, Landman D, Haag R, Recco R, Eramo A, Alam M, Quale J. 2005. Rapid spread of carbapenem-resistant Klebsiella pneumoniae in New York City: a new threat to our antibiotic armamentarium. Arch Intern Med. 165:1430–1435.
- Charles PG, Grayson ML. 2004. The dearth of new antibiotic development: why we should be worried and what we can do about it. Med J Aus. 181:549–553.
- Clinical and Laboratory Standards Institute. 2012. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard. 9th ed. CLSI document M07-A9. Wayne (PA): Clinical and Laboratory Standards Institute.
- Cocchiara J, Letizia CS, Lalko J, Lapczynski A, Api AM. 2005. Fragrance material review on cinnamaldehyde. Food Chem Toxicol. 43:867–923.
- Cos P, Vlietinck AJ, Vanden Berghe D, Maes L. 2006. Anti-infective potential of natural products: how to develop a stronger in vitro ‘proof-of concept’. J Ethnopharmacol. 106:290–302.
- Cotton CM. 1996. Ethnobotany: principles and applications. New York: John Wiley & Sons.
- Courvalin P. 2006. Vancomycin resistance in Gram-positive cocci. Clin Infect Dis. 42:S25–S34.
- Deans SG, Ritchie G. 1987. Antibacterial properties of plant essential oils. Int J Food Microbiol. 5:165–180.
- Duarte A, Ferreira S, Silva F, Domingues FC. 2012. Synergistic activity of coriander oil and conventional antibiotics against Acinetobacter baumannii. Phytomedicine. 19:236–238.
- Fabry W, Okemo PO, Ansorg R. 1998. Antibacterial activity of East African medicinal plants. J Ethnopharmacol. 60:79–84.
- Fung-Tomc J, Huczko E, Pearce M, Kessler RE. 1988. Frequency of in vitro resistance of Pseudomonas aeruginosa to cefepime, ceftazidime, and cefotaxime. Antimicrob Agents Chemother. 32:1443–1445.
- Giacometti A, Cirioni O, Barchiesi F, Fortuna M, Scalise G. 1999. In vitro anticryptosporidial activity of ranalexin alone and in combination with other peptides and with hydrophobic antibiotics. Eur J Clin Microbiol Infect Dis. 18:827–829.
- Gill AO, Holley RA. 2006. Inhibition of membrane bound ATPases of Escherichia coli and Listeria monocytogenes by plant oil aromatics. Int J Food Microbiol. 111:170–174.
- Goettsch W, Van Pelt W, Nagelkerke N, Hendrix MGR, Buiting AGM, Petit PL, Sabbe LJM, Van Griethuysen AJA, De Neeling AJ. 2000. Increasing resistance to fluoroquinolones in Escherichia coli from urinary tract infections in the Netherlands. J Antimicrob Chemother. 46:223–228.
- Harborne JB. 1998. Phytochemical methods: a guide to modern techniques of plant analysis. 3rd ed. London: Chapman and Hall.
- Helander IM, Alakomi HL, Latva-Kala K, Mattila-Sandholm T, Pol I, Smid EJ, Gorris LG, von Wright A. 1998. Characterization of the action of selected essential oil components on Gram-negative bacteria. J Agric Food Chem. 46:3590–3595.
- Jahan R, Khatun MA, Nahar N, Jahan FI, Chowdhury AR, Nahar A, Seraj S, Mahal MJ, Khatun Z, Rahmatullah M. 2010. Use of Menispermaceae family plants in folk medicine of Bangladesh. Adv Nat Appl Sci. 4:1–9.
- Jevons MP. 1961. “Celbenin”-resistant staphylococci. Br Med J. 1:124–125.
- Kar A, Jain SR. 1971. Antibacterial evaluation of some indigenous medicinal volatile oils. Qual Plant Mater Veg Food Nutr. 20:231–237.
- Krishnan N, Ramanathan S, Sasidharan S, Murugaiyah V, Mansor SM. 2010. Antimicrobial activity evaluation of Cassia spectabilis leaf extracts. Int J Pharmacol. 6:510–514.
- Kuete V. 2010. Potential of Cameroonian plants and derived products against microbial infections: a review. Planta Med. 76:1479–1491.
- Latha RCR, Daisy P. 2011. Insulin-secretagogue, antihyperlipidemic and other protective effects of gallic acid isolated from Terminalia bellerica Roxb. in streptozotocin-induced diabetic rats. Chem Biol Interact. 189:112–118.
- Ling LL, Schneider T, Peoples AJ, Spoering AL, Engels I, Conlon BP, Mueller A, Schäberle TF, Hughes DE, Epstein S, et al. 2015. A new antibiotic kills pathogens without detectable resistance. Nature. 517:455–459.
- Lockwood GB. 1979. The major constituents of the essential oils of Cinnamomum cassia Blume growing in Nigeria. Planta Med. 36:380–381.
- MacKenzie FM, Forbes KJ, Dorai-John T, Amyes SGB, Gould IM. 1997. Emergence of a carbapenem-resistant Klebsiella pneumoniae. Lancet. 350:783–783.
- Moleyar V, Narasimham P. 1986. Antifungal activity of some essential oil components. Food Microbiol. 3:331–336.
- Neu HC. 1992. The crisis in antibiotic resistance. Science (New York, N.Y.). 257:1064–1074.
- Nikaido H, Vaara M. 1985. Molecular basis of bacterial outer membrane permeability. Microbiol Rev. 49:1–32.
- O’Neill J. 2014. Tackling drug-resistant infections globally: final report and recommendations. UK: HM Government and Welcome Trust.
- Ooi LS, Li Y, Kam SL, Wang H, Wong EY, Ooi VE. 2006. Antimicrobial activities of cinnamon oil and cinnamaldehyde from the Chinese medicinal herb Cinnamomum cassia Blume. Am J Chin Med. 34:511–522.
- Palaniappan K, Holley RA. 2010. Use of natural antimicrobials to increase antibiotic susceptibility of drug resistant bacteria. Int J Food Microbiol. 140:164–168.
- Parthasarathy VA, Chempakam B, Zachariah TJ. 2008. Chemistry of spices. Wallingford (UK): CAB International.
- Peleg AY, Seifert H, Paterson DL. 2008. Acinetobacter baumannii: emergence of a successful pathogen. Clin Microbiol Rev. 21:538–582.
- Peng L, Kang S, Yin Z, Jia R, Song X, Li L, Li Z, Zou Y, Liang X, Li L, et al. 2015. Antibacterial activity and mechanism of berberine against Streptococcus agalactiae. Int J Clin Exp Pathol. 8:5217–5223.
- Rahmatullah M, Hasan ME, Islam MA, Islam MT, Jahan FI, Chowdhury AR, Jamal F, Islam MS, Miajee Z, Jahan R, et al. 2010. A survey on medicinal plants used by the folk medicinal practitioners in three villages of Panchagarh and Thakurgaon district, Bangladesh. Am-Eur J Sustain Agric. 4:291–301.
- Reller LB, Weinstein M, Jorgensen JH, Ferraro MJ. 2009. Antimicrobial susceptibility testing: a review of general principles and contemporary practices. Clin Infect Dis. 49:1749–1755.
- Rios JL, Recio MC. 2005. Medicinal plants and antimicrobial activity. J Ethnopharmacol. 100:80–84.
- Schelz Z, Molnar J, Hohmann J. 2006. Antimicrobial and antiplasmid activities of essential oils. Fitoterapia. 77:279–285.
- Shalayel MHF, Asaad AM, Qureshi MA, Elhussein AB. 2017. Anti-bacterial activity of peppermint (Mentha piperita) extracts against some emerging multi-drug resistant human bacterial pathogens. J Herbal Med. 7:27–30.
- Sikkema J, De Bont JA, Poolman B. 1995. Mechanisms of membrane toxicity of hydrocarbons. Microbiol Rev. 59:201–222.
- Smith AH, Zoetendal E, Mackie RI. 2005. Bacterial mechanisms to overcome inhibitory effects of dietary tannins. Microb Ecol. 50:197–205.
- Spellberg B, Powers JH, Brass EP, Miller LG, Edwards JE. 2004. Trends in antimicrobial drug development: implications for the future. Clin Infect Dis. 38:1279–1286.
- Stermitz FR, Lorenz P, Tawara JN, Zenewicz LA, Lewis K. 2000. Synergy in a medicinal plant: antimicrobial action of berberine potentiated by 5′-methoxyhydnocarpin, a multidrug pump inhibitor. Proc Natl Acad Sci USA. 97:1433–1437.
- Stryjewski ME, Corey GR. 2014. Methicillin-resistant Staphylococcus aureus: an evolving pathogen. Clin Infect Dis. 58:S10–S19.
- Takhtajan A. 2009. Flowering plants. New York: Springer Science & Business Media.
- Tisserand R, Young R. 2013. Essential oil safety: a guide for health care professionals. Edinburgh (UK): Elsevier Health Sciences.
- Vivek S, Nisha S, Harbans S, Devendra SK, Vijaylata P, Bikram S, Raghbir GC. 2009. Comparative account on GC–MS analysis of Mentha arvensis L. (corn-mint) from three different locations of north India. Int J Drug Dev Res. 1:1–9.
- Wagner H, Ulrich-Merzenich G. 2009. Synergy research: approaching a new generation of phytopharmaceuticals. Phytomedicine. 16:97–110.
- Walsh C. 2000. Molecular mechanisms that confer antibacterial drug resistance. Nature. 406:775–781.
- Wan NAW, Masrah M, Hasmah A, Noor IN. 2014. In vitro antibacterial activity of Quercus infectoria gall extracts against multidrug resistant bacteria. Trop Biomed. 31:680–688.
- Wendakoon CN, Sakaguchi M. 1993. Combined effect of sodium chloride and clove on growth and biogenic amine formation of Enterobacter aerogenes in mackerel muscle extract. J Food Prot. 56:410–413.
- Wojtyczka RD, Dziedzic A, Kepa M, Kubina R, Kabala-Dzik A, Mularz T, Idzik D. 2014. Berberine enhances the antibacterial activity of selected antibiotics against coagulase-negative Staphylococcus strains in vitro. Molecules. 19:6583–6596.
- World Health Organization (WHO). 2014. Antimicrobial resistance: 2014 global report on surveillance. Geneva: World Health Organization.
- Wright GD. 2000. Resisting resistance: new chemical strategies for battling superbugs. Chem Biol. 7:R127–R132.