Abstract
Objective: To investigate early auditory prerequisites in relation to the use of canonical babbling (CB) and early consonant production in a heterogeneous group of children with hearing impairment (HI) and in comparison to controls with normal hearing (NH).
Methods: Five children with unilateral or bilateral HI who used hearing aids (HA) (0;9–1;7 years) and six children with cochlear implants (CI) (0;10–2;0 years) were compared to data from 22 children with NH (0;10–1;6 years). Hearing age, type of HI and daily use of hearing technology (hours) was investigated in relation to CB ratio and consonant production. Analysis of babbling from video recordings during verbal interaction between a parent and child was independently performed by two observers. Intra- and inter-agreement were calculated.
Results: Children with HI used less CB compared to children with NH. Less CB utterances and occurrences of dental/alveolar stops were found in children with HA who had a hearing age of 5 months and who used their hearing technology 5 h per day. The children with CI reached an expected CB ratio and consonant production after 8.5 months with daily fulltime use of CI.
Conclusions: Even a mild hearing loss in early childhood may affect and delay the onset of important linguistic milestones like canonical babbling and consonant production. It was indicated that children with CI or HA might receive different attention and intervention services. Longer hearing age and full-time use of hearing technology may influence positively on CB ratio and consonant production in children with HI.
Introduction
Hearing ability and listening skills such as auditory feedback, are necessary underlying factors in the process of developing linguistic milestones like canonical babbling (CB), defined as well-formed syllables consisting of a consonant and a vowel with a rapid transition between the two [Citation1,Citation2]. The CB is well established around 9 months in typically developing children [Citation3]. Previous studies of children with hearing impairment (HI) have shown that CB onset is depending on factors such as age at diagnosis as well as type of HI and degree of hearing loss (HL) [Citation1,Citation4,Citation5]. Better hearing ability post-op with cochlear implant(s) (CI) has also proven to have a positive impact on the CB development [Citation2]. Children with CI use temporal cues for phonetic identification to a greater extent than children with hearing aids (HA) who rely more on spectral cues similar to children with normal hearing (NH) [Citation6]. However, neither HA and/or CI do fully compensate for a HI in all listening situations, which may affect the CB onset and listening development negatively.
Babbling and early consonant production
The onset of CB is typically from 6 months of age and seems to be robust, even in the presence of factors such as low socioeconomic status, prematurity and exposure to more than one language [Citation7]. The consonant production in CB prepares the child for word production [Citation8] and the consonant sounds in CB correspond largely with the speech sounds that are used in the early spoken words [Citation9]. Anterior place of articulation (labial and dental/alveolar) in consonant production and oral stops (b, d), nasals (m, n) and approximants (j, w) with) are most commonly used [Citation10].
A delayed onset of CB and consonant production could be a predictor of difficulties in speech and language development later on. It has been found to be associated with delayed onset of meaningful speech [Citation11], a smaller expressive vocabulary at 18, 24 and 30 months [Citation12,Citation13], less accurate articulation at 36 months [Citation14,Citation15], and later difficulties with literacy [Citation16].
Children with hearing impairment
Today it is possible to screen for deafness and HL when infants are born at the maternity hospital [Citation17]. The introduction of Universal Newborn Hearing Screening (UNHS) has led to earlier identification of HL and deafness in infancy, resulting in earlier ages at first fitting of hearing aids (HAs) and/or CI(s) [Citation18]. Children who are born with a mild-moderate/severe hearing loss (26–70 dB HL) can potentially make use of some natural acoustic hearing, when amplified with well-adjusted HA(s), while young deafborn children with a moderate/severe-profound HL (56–91+ dB HL) have no or very little benefit of HA(s), and therefore need electrical stimulation through a CI. It is expected that children with HA have access to suprasegmental cues in their surrounding speech, and that most of them learn spoken language spontaneously, despite possible limitations in the audibility of speech [Citation19]. The perceived speech signals with HA might be distorted because of for instance background noise, and the spectral speech information might be limited, especially if the child has a worse degree of hearing loss [Citation19]. Hearing aids can only amplify the speech sounds within the individual’s particular hearing range, while a CI replaces the non-functional acoustic hearing with direct electronic stimulation of the auditory nerve, which is the link to the auditory cortex. Due to relatively good temporal resolution of the CI, it is possible for recipients to perceive segmental speech information and for example discriminate between oral stops. One drawback of the CI technology is a reduced spectral resolution, and limitations to convey suprasegmental cues and especially low-frequency speech signals [Citation20]. This might contribute to difficulties of i.e. understanding speech in noise, identify prosodic features like intonation, and to discriminate between nasal consonants (m, n). For children with HA it is common to have a reduced ability to percieve speech signals within the high-frequency area, which can lead to deficient recognition of consonants and less accurate discrimination between oral stops.
The criteria for being a candidate for CI have changed gradually over the years, primarily as a consequence of better understanding the impact of early intervention with CI [Citation18]. Children who need a CI are nowadays implanted simultaneously or sequentially with bilateral CIs or unilaterally from approximately 5 months of age in many countries. Also, children with better pre-implant hearing may be a CI-candidate. This has resulted in a higher number of children who benefit from having one CI at an early age together with contralateral HA use on the other ear, the so-called bimodal approach. Furthermore, the degree of HL might change over time for children with progressive HL, and some of these children who use HA might eventually become CI candidates.
In the literature, the two groups of children (HA and CI) are often studied separately. They are partly viewed as different subgroups, for reasons like their different initial auditory background and acoustical or electrical listening experiences with their hearing devices. However, today when the deaf-born children are implanted in infancy some of the age-related differences between groups (HA and CI) have diminished (that is, age at diagnosis, and age at 1st fitting of hearing devices). In addition, many children with HI use the bimodal approach from early ages and all children with a HA are potential candidates for a CI, in the near or later future. One important difference that has been found between groups (HA vs. CI) is their daily amount of hearing device use. It seems like children with CI use their devices full-time to a higher degree than children who use HA [Citation21]. Use of hearing technology was explored in a longitudinal study of 290 children with mild-to-severe hearing loss [Citation22]. Parents estimated across visits that children used their HAs for around 10.63 h (SD = 3.29) per day on average while data logging values of their HAs were around 8.44 h (SD = 4.06). This finding indicates that parents overestimated their child’s daily HA use [Citation22]. Maternal education level was a predictor of HA use over time, both in infancy and school age [Citation22]. Moreover, it has been found that not only the age at initial fitting of the HAs and amount of daily HA use, but also the optimal level of stimulation and audibility with the HA must be reached for children with mild-to-moderate HL, to avoid deficiencies in speech and language development [Citation23]. In a study of 146 children with CI the objective was to measure daily CI use by objective datalogging, and to explore which factors that affected consistent device use [Citation24]. The result showed that 64% (n = 93) used their devices more than nine hours per day. The mean use time in the whole cohort was 9.86 h (SD = 3.43). More hearing experience promoted consistent CI use, and higher frequency of coil-off time during the day was a negative factor leading to fewer hours with CI use [Citation24].
Babbling and consonant production in children with hearing impairment
It is well known that children with a severe degree of HL who use HA have a deviant early speech production with a restricted consonant production in babbling [Citation1,Citation14,Citation15]. Later onset of canonical babbling, smaller consonant inventories including lack of dentals/alveolars, and less accurate consonants compared with normally hearing children have been demonstrated in children with HA. Significant relationships between late onset of CB and small size of particularly expressive vocabulary [Citation12] and between lack of predictive consonants in CB and articulation proficiency at 3 years of age have been shown in children with cleft palate [Citation25,Citation26]. Although similar observations have been done in children with HI [Citation27] there seem to be within-group differences related to use of HA or CI [Citation2]. Eilers and Oller [Citation1] demonstrated that children with HA had a delayed onset of CB regardless of their chronological age while Schauwers et al. [Citation5] found that deaf children with a CI caught up and had typical CB after only four months of listening experiences with a CI [Citation5]. Interestingly, age at CI did not affect the number of months of exposure to spoken language with CI required, for babbling to occur [Citation5]. These authors concluded that a child implanted with a CI at 6 months as well as a child who received a CI in the second year of life needed approximately the same amount of time with auditory exposure to start babbling [Citation5]. This was confirmed by Fagan [Citation2] who explored the nature of transition from non-linguistic to linguistic vocalizations (from vocalizations before emergence of words to vocalizations with combinations consistently with specific meaning) by evaluating use of CB in infants with CI who had a mean age at implantation of 9.9 months and in comparison to children with NH. Canonical babbling were rare before CI activation but after 4 months of consistent CI use the infants born deaf had caught up and used repetitive vocalizations in similar ways as the children with NH. In summary, these findings indicate that optimal auditory requisites are essential for a natural development of CB in deaf-born children, as well as the child’s own active exploration of speech sounds towards an adequate consonant inventory, proficiency and expressive vocabulary.
Considering what is known about CB as predictor of later spoken language development it is continuously warranted to explore the use of CB in children with HI, in order to design valid and individualized intervention options from infancy, for optimal speech and language development. According to previous findings, children with a HI may establish CB and typical consonant production later than children with NH and there seem to be differences within the population that can be related to type of hearing technology (HA vs. CI) [Citation1,Citation5].
Aim
The aim of the pilot study was to explore the presence of CB and consonant production in a heterogenous group of children with HI with different type of hearing technology and in comparison to previously collected data of age-matched children with NH.
The research questions and hypotheses of the study were:
What is the CB ratio in children with HI compared with age-matched. Children with NH, and is there a difference related to type of hearing technology (CI and HA)? The hypothesis was that children with a HI would have CB similar to NH controls, if they had used their hearing technology for more than four months or had received an early HL diagnosis (before 3 months) respectively.
Are there any relationships between quantitative and qualitative use of babbling in children with HI and hearing age (time period with hearing technology), or daily use of hearing technology? The hypothesis was that factors like lower degree of HL and longer time period with hearing technology (HA or CI), including daily use in hours, would affect CB outcome positively in children with HI.
What is the prevalence of predictive consonant variables, such as oral stops, anterior placement in stops and specifically dental/alveolar placement in stops, in children with HI compared to controls? The hypothesis was that these consonant variables would be present also in children with HI if they were older.
Materials and methods
Participants
Selection
Children with HI using a HA or CI (0;9–2;0 years) who were followed-up at the Karolinska University Hospital, either at the Auditory Implant Center or Hearing and Balance Clinic, were invited to take part in the pilot study. At the time of recruitment there were 40 children with mild-to-moderate HL (30–70 dB) and 15 children with CI(s), who met the inclusion criteria of having at least one native Swedish-speaking caregiver and no diagnosed neurodevelopmental disability. There were seven families, each with a child with a HA, who accepted to participate. However, two children were later excluded because it turned out that neither of their parents spoke Swedish. Twenty-two families with a child who had a HA did not reply at all and eleven families replied that they would not like to be enrolled in the study. In the group of children with CI there were four families who did not reply to the study invitation and one family did not accept to be enrolled in the study. Ten families out of 15 with children who had CI agreed to participate. However, three families did not have the possibility to attend at the time of observation and one child was excluded because neither of the parents spoke Swedish with the child during the observation. Video recordings and observation data of 22 age-matched children with typical development and NH from a previous study were included for group comparisons [Citation28].
Study group
Eleven children with HI participated in the study (5 with HA and 6 with CI). Each participant with HI was sex and age matched to two children with NH (n = 22). All participants were identified with a bilateral HI at birth (UNHS). Three children had a conductive HI and seven children had a sensorineural HI, which contributes to the heterogeneity within the sample. Swedish was their native language and at least one parent of each child spoke Swedish as their mother tongue. See for information of individual hearing characteristics (HA and CI). There was no significant difference on chronological age (median) between children with CI; 19.5 months (range: 12–21) and children with HA; 10 months (range: 9–19) (p > .05). Children with CI had a significantly longer median hearing age (time with hearing technology since 1st fitting until the test occasion); 8.5 months (range: 4–13) compared to children with HA with a median hearing age; 5 months (range: 0–8) (t = –2.61, df = 9, p = .03). Children with CI used their devices every waking hour which was significantly more compared to children with HA who used their devices part-time with a median of 5 h (range: 0–8). (t = –5.23, df = 9, p < .01).
Table 1. Subject characteristics and Medians (Md); children with HA (n = 5) and children with CI (n = 6).
Procedure
The study was approved by the Regional Ethical Committee in Stockholm (Dnr: 2013/1989-32). Parents signed a written consent before participation. Participating children with HI and their parents were then scheduled for one test occasion at the Auditory Implant Center, Karolinska University Hospital. The family first met an audiologist who performed a hearing test before the babbling observation. Then four observers, divided in two different pairs, responsible for either observation of children with HA or children with CI, introduced and observed parent-child interactions. Four of the six participating children with CI were observed in conjunction with their regular follow-up visits at the clinic. The other two children with CI, and all five children with HA, and their parents came specifically for taking part in the study.
Material
Previously validated variables (i.e. occurrence of CB, oral stops, anterior placement and specifically dental/alveolar placement, and total number of different consonants) were used to evaluate babbling by standardised observation [Citation29]. The hearing ability was evaluated with a pure-tone average test and a parental evaluation form of the child’s current listening skills was also filled in the same day. Information regarding the child’s age-related hearing background like age at HA fitting or age at CI was gathered from medical records.
Audiometry
Hearing ability was tested with the Visual Reinforcement Audiometry test (VRA), calculated for the best ear, for ten of the eleven children with HI, with pure-tone average of four test points; 0.5, 1, 2 and 4 kHz. One child did not participate in the audiometry test because of unknown reasons. There was no significant difference between groups (HA and CI) on the pure-tone average test (p > .05).
Listening skills – parent questionnaire
The subjective form LittlEARS was used as a complement to the VRA hearing test [Citation30]. LittlEARS is a parental questionnaire that can be used to estimate listening skills both in children with NH and children with HI. The form consists of 35 questions that parents have to answer yes or no to. The form can be used to assess auditory development from 0 up to 2 years of age in children with NH or in children with HA or CI with up to 2 years of hearing experience [Citation30]. LittlEARS has been translated and recently validated for Swedish [Citation31]. There was no significant difference between groups (HA and CI) on listening ability measured with LittlEARS (p > .05).
Observation of babbling
The observation method was used for assessment of babbling [Citation29]. The parent was told to play and communicate with the child Parents received instructions to play and talk, as they would do at home during 30–40 min. The two examiners were in the same room and video and audio recorded the play situation. The recordings were made with a video camera (Sony HDR-CX250E), an external microphone (Sony ECM-909) and a portable audio recorder for backup audio recording (TASCAM DR-07MKII). A fixed set of toys that were age-appropriate were used for eliciting spoken communication during parent-child interactions. During the session, the two observers independently notified if vocalizations and CB occurred on a 100 mm VAS, where the occurrence was estimated from “no “to “much”. The potential occurrence of high-pressure oral consonants/oral stops and anterior placement was noted by the response options “yes”, “no” or “do not know”. Based on the Swedish consonant system, which contains 18 phonemes (6 oral stops, 7 fricatives, where 3 usually are pronounced as approximants, 3 nasals, 1 lateral and the/r/phoneme, the observers noted consonant sounds that were heard at least twice during the observation. From this set-up a calculation of total number of different consonants and total number of oral stops were made. After each video recorded observation the parents were asked if the child’s utterances during the session were representative for how the child usually sounded. Two of the observers then analysed the data of all children with HA including video recorded material of their matched controls with NH. The other two observers analysed the data of children with CI and video recorded material of their matched children with NH.
Training
The four observers prepared their observation skills before data collection by practicing to use the observation method by jointly observing and listening to video recordings of six typical developed children with NH aged 10–18 months. This was followed by pilot observations of two typically developing children aged 18 months where the use of forms, equipment and other approaches were tested. After each recording and pilot observation the results were discussed in the small group of observers. The purpose was to increase common judgments of observations and to reach agreement on how the observation points would be used.
Reliability of the observational analysis
Observation analysis was made at all test occasions by the two responsible observers in each pair and independently of each other. For additional control of reliability, re-observations were made after two weeks using the video recordings from all observations. Reliability was calculated with the Intra-class Correlation Coefficient (ICC) for number of utterances, number of CB utterances, different consonants and oral stops. Percentage agreement, point by point, was calculated for the dichotomous variables high-pressure consonants, anterior consonants, oral stops and anterior oral consonants. The results from the calculation should be as close to 1.0 as possible and a result above .9 is considered to be high [Citation32] and over .8 is good [Citation33]. Intra-observer reliability varied between .82 and .99 for all variables and the agreement was 100% for all observers. The inter-observer ICC-values were over .8 and varied between .81 and .98. The agreement values were 83% for anterior consonants and 100% for the other variables.
Validity of the observational analysis
The number of utterances was counted from the video recordings independently by all four observers and used for calculation of CB ratio. To be classified as an utterance, the vocalization had to be separated by breaths or pauses, which potentially include a breath [Citation34]. An utterance was not counted if the production was simultaneous with an adult’s production. Only speech-like utterances were counted, that is non-speech-like vocalizations (e.g. crying, yelling, laughing, coughing, burps) were excluded. A mark was made for each speech-like utterance and one more if it was canonical, that is, included at least one vowel and one consonant/consonant-like sound with smooth and fast transition between the two sounds, as in speech [Citation12]. The number of canonical utterances was divided by the total number of utterances for calculation of a CB ratio. The threshold of ≥ 15% for having CB was recently validated for this simplified CB ratio (CBRUTTER) [Citation35]. The ICC-value between the four observers for number of utterances was .98 and for number of CB utterances .99. The observation of CB was compared with CB ratio in the two subgroups showing good or high agreement (ICC = .85 and .91).
Then the consonant production was phonetically transcribed of up to 100 utterances for each child (lowest number was 78). The transcriptions of the children with CI were performed by observers who collected data of children with HA and vice versa. Reliability of the transcriptions was controlled for by comparison of transcriptions from two children for each observer. Broad transcription using the International Phonetic Alphabet (IPA) and the extended IPA (extIPA) was performed according to the following procedure and order. It was first decided if the sound was a consonant or vowel. A vowel was notified with a V. For consonants the manner of articulation, and then place was decided.
The transcriptions were categorized into the same variables as in the observation and compared. The comparisons between observed consonant variables and transcription showed good or high agreement with ICC-values for the two sub-groups of .81 and .96.
Statistical analysis
Because of small groups and skewed distribution of the data, only nonparametric statistics were used. For examining differences between the group with HI and children with NH we used the Mann Whitney U test. The Fischer’s exact test was used for calculating differences of dichotomous data. Correlation between CB and hearing status were tested with Spearman’s rank correlation coefficient. Significance level was set to <.05.
Results
CB ratio in children with HI related to type of hearing technology (CI or HA)
Three of five children with HA and four of six children with CI had established CB according to the observation and a CB ratio ≥ 15%. All children with NH except for one with CB ratio of 14%, had CB (≥15%). Individual results for children with HI are presented in .
Table 2. Individual child characteristics and results in children with HA (n = 5) and children with CI (n = 6) including test age (months), hearing age (months with NH, HA or 1st CI), CB ratio (%), total number of utterances, occurrence of oral stops; anterior stops; dental-alveolar stops (yes = 1, no = 0) and number of different consonants and number of different oral stops.
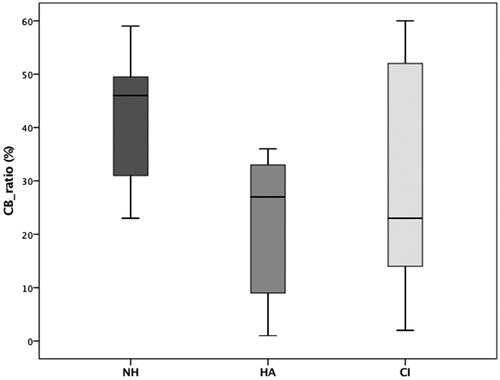
The difference for CB ratio between children with NH and children with HI was close to be statistically significant (Z = –2.00; p = .05). There was a larger variance within the group of children with HI compared to controls. The difference between children with NH and children with HA was statistically significant (Z = –2.16; p = .03), whereas no such difference was found between controls with NH and children with CI (Z = –1.16; p = .25) ().
CB and consonant use related to hearing age and time with hearing technology (CI or HA)
A significant positive correlation was found between the amount of CB and the child’s time with 1st CI (rs = .94, p <.01) while this was not the case in children with HA (time with HA). The two children with the shortest period with 1st CI were also the children who had not yet established CB. All children with a CI used their device(s) more than 12 h per day according to the parent estimation and children with HA used their devices around five hours per day (median). A close to significant negative correlation was found between use of HA (hours per day) and number of CB (rs = –.87, p=.05). Children with CI produced close to significantly more utterances than children with HA (Mann–Whitney U-test, Z = –2.01; p = .05).
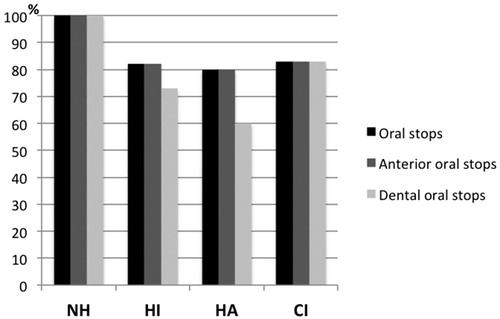
Consonant variables in children with HI and CI or HA compared to controls
The proportion of children with of oral stops was 100% in the NH group and approximately 80% in children with HI. The difference was a close but not statistically significant (Z = –2.49; p = .05). Fewer children with HA had anterior or specifically dental placement of oral stops than children with CI and NH () but none of these differences were statistically significant. The three children with a conductive HL had higher percentage of CB use and higher numbers of different consonants compared to the other two children with HA who had a sensorineural HL. There was no obvious association with degree of HL, however.
Discussion
The aim of this explorative pilot study was to investigate canonical babbling and consonant production in a heterogeneous group of toddlers with HI who used different hearing technology (HA and/or CI) by using previously validated variables for CB observation of children with NH and children with cleft palate [Citation28]. Children who were born deaf had somewhat better CB outcome than children with mild to moderate or severe HL. Children who relied on their hearing with HA, only used their hearing technology part-time, had fewer utterances and a more limited consonant repertoire compared to children with CI. Longer time with hearing technology (hearing age) and consistent use of a CI were possibly beneficial factors for CB use and production of different consonants in children with CI.
In accordance with previous findings deaf children with CI caught-up and reached age-equivalent levels of babbling and used different consonant types after only a relatively short period of consistent CI use. Schauwers et al. [Citation5] found similar results in their study of ten infants with CI and suggested that the fast babbling development in infants with CI is the result of a “trigger effect” rather than a maturation effect [Citation5]. Seemingly, a CI quickly becomes a natural part of the deaf-born child’s everyday life. Although a CI functions as an artificial hearing device compared to HA, the benefits of electrical stimulation for promoting listening skills in infancy have previously been proven to be beneficial for deaf toddlers to develop consonant sounds and CB fairly quickly [Citation36]. Even though the children with a HA in the present study were neuromotorically prepared for CB use, they were at higher risk of lacking detailed acoustic information important for consonant acquisition because they had a shorter hearing age and deviant speech perception compared to children with NH. Potentially, the “trigger effect” that was found in the pilot study could therefore be less pronounced in the sample of children with HA. Maternal education level has previously been found to be an important predictor of HA use in infancy [Citation10]. In the current study, mothers’ had a high education level but children still had a low level of HA use. This indicates that caregivers in this subgroup were less aware about HA use effects.
The deaf-born children with a CI and with at least eight months of full-time use of their first CI device had CB, confirming our initial hypothesis and previous reported results for children with a CI [Citation2,Citation4]. Moreover, there was one child with a CI who had a close to reference CB ratio, which was confirmed by the parent opinion. In the group of children with a HA it was the two children (9 and 10 months old) with the most severe HL and lowest scores on LittlEARS who had a low CB ratio. According to parent estimations of HA use these two children used their hearing devices around 8 h per day, which was the highest scores within the group of children with a HA, similar compared to previous reports of HA use [Citation22] and children with CIs in the current study. Nevertheless, they did not reach the reference CB ratio level. One possible explaining factor could have been their short time period with HAs (3–4 months).
Group mean of the hearing assessment indicated that children in both groups (CI and HA) functioned on an expected level for children with mild-to-moderate HL (PTA results, ). Longer time with hearing technology was beneficial for CB use and prevalence of different types of consonants in children with HI. Children with a HA did not use their HAs consistently, which might have explained why they used fewer CB utterances and less consonant types [Citation22,Citation36]. Considering that children with severe-profound HL with a CI, who used their devices full-time, caught up after only a short period of listening time also point to the importance of consistent usage of hearing device in this group. Parents of children with HA have previously reported that there are both practical and emotional challenges of promoting their child’s consistent HA use [Citation36]. An influencing factor in the level of satisfaction and empowerment was the timing and amount of guidance that parents had received from their audiologist and Speech-Language Pathologist (SLP) in managing the hearing technology and promoting full-time use [Citation36]. There are few Swedish parents of children with mild to moderate HL who receive regular, and individual Family-Centered Early Intervention (FCEI) options. Families who have deaf children with CI, are usually prioritized and have access to more specialized habilitation services. This factor might have explained some of the between-groups differences in the current study. There could also be differences in access of services within the two subgroups, including children with CI, that depend on where the family lives in Sweden.
Although not significantly different, children with a CI seemed to produce a less amount of oral stops than controls, whereas the prevalence of different oral stops was similar for both groups (CI and NH). On the other hand, children with a HA seemed to produce even lesser occurrences of oral stops and especially with dental/alveolar placement. Children with a HA who did not produce oral stops and anterior placement also had the most severe HL. This finding showed that the degree of HL may affect the development of oral stops and anterior placement in children who use a HA, which has been found in previous studies [Citation12]. Besides from having less specific auditory and acoustic information of consonant sounds in a phase of life when CB usually develops, it may also lead to fewer experiences of CB use and opportunities of beneficial self-training, which are both essential parts of the acquisition of vocabulary [Citation14]. Moeller et al. [Citation14] found that phonetic and phonological delays negatively influenced on vocabulary growth in children with mild-to-profound HL [Citation14].
The observation method of babbling and a parental questionnaire of listening abilities may together serve as useful clinical tools for early identification of precursors for typical, delayed or atypical spoken language development in young children with HI. The study was limited in different ways, however. The sample size was small and the findings are not generalizable. In particular, few families who had children with a HA agreed to participate in the study. This could be explained by that parents in this subgroup are less worried and aware about their child’s development and thereby not interested or motivated enough to participate in research studies.
In summary, deaf children with a CI used their devices fulltime according to their parents and showed CB results that were similar to age and sex matched controls with NH. Children with a HA also had CB, although fewer utterances with CB than controls, because of yet unexplained factors. Despite the small sample, results showed significant and close to significant differences in the subgroup of children with mild to moderate HL with less utterances and occurrences of different consonant sounds, especially dental/alveolar stops. This means that even a mild to moderate HL could negatively affect spoken language development, also previously suggested by Moeller et al. [Citation37]. Findings from the present study need to be interpreted with caution but point towards the need for longitudinal population-based studies for verification and in-depth exploration of hearing-related factors in relation to linguistic mile-stones like babbling in young children with HI and its effects of later language development. Factors that are related to clinical accessibility of FCEI services, regardless of type and degree of HL and environmental aspects such as parent level of knowledge and engagement in audio-verbal communication with their child should be investigated in relation to CB usage and development of consonant sounds.
Conclusions
Even a mild hearing loss in early childhood may affect and delay the onset of important linguistic milestones like canonical babbling and consonant production. Furthermore, it was indicated that children with CI or HA might receive different attention and service, which needs to be further explored. All parents of children with HI should be educated about the importance of full-time use of hearing technology and taught how they can promote their child’s own speech and CB development.
Acknowledgements
We thank Maria Drott and Erica Billermark for their help in audiological assessment procedure and especially the families for participating in the study. In addition, we thank Jeremy Wales for proofreading of the manuscript.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Additional information
Notes on contributors
Ulrika Löfkvist
Ulrika Löfkvist is Associate professor at the University of Oslo, Norway, and Research Coordinator at the Auditory Implant Center Karolinska Institute, Stockholm, Sweden. She has previously worked as clinician (CCC-SLP, LSLS cert. AVEd) at the Karolinska University Hospital, Sweden. Her research is focusing on language development and skills in individuals with hearing loss.
Kristin Bäckström
Kristin Bäckström is a Speech and Language Pathologist with a clinical position at the Habilitation and Care in the Stockholm County Council. She previously completed her MSc at Karolinska Institutet.
Malin Dahlby-Skoog
Malin Dahlby-Skoog is a Speech and Language Pathologist with a clinical position at the Haninge Rehab in the Stockholm County Council. She previously completed her MSc at Karolinska Institutet.
Sofia Gunnarsson
Sofia Gunnarsson is a Speech and Language Pathologist with a clinical position at the Södermanland County Council in Nyköping. She previously completed her MSc at Karolinska Institutet.
Malin Persson
Malin Persson is a Speech and Language Pathologist with a clinical position at the Stocksunds RE/Speech and Language in the Stockholm County Council.
Anette Lohmander
Anette Lohmander is Professor in Speech and Language Pathology at Karolinska Institutet and Head of Division of Speech and Language Pathology, Department of Clinical Science, Intervention and Technology, Karolinska Institutet. She is also a Speech and Language Pathologist at the Karolinska University Hospital. Her research is currently focused on early speech and language development and difficulties associated with adverse conditions such as cleft palate and hearing impairment.
References
- Eilers RE, Oller DK. Infant vocalizations and the early diagnosis of severe hearing impairment. J Pediatr. 1994;124(2):199–203.
- Fagan MK. Why repetition? Repetitive babbling, auditory feedback, and cochlear implantation. J Exp Child Psychol. 2015;137:125–137.
- Nathani S, Ertmer D, Stark RE. Assessing vocal development in infants and toddlers. Clin Ling Phon. 2006;20(5):351–369.
- Vohr B, Topol D, Girard N. Language outcome and service position of preschool children with congenital hearing loss. Early Hum Dev. 2012;88(7):493–498.
- Schauwers K, Gillis S, Govaerts PJ. Babbling in early implanted CI children. Int Congr Series. 2004;1273:344–347.
- Winn MB, Won JH, Moon IJ. Assessment of spectral and temporal resolution in cochlear implant users using psychoacoustic discrimination and speech cue categorization. Ear Hear. 2016;37(6):e377–e390.
- Oller D, Eilers RE, Steffens M, et al. Speech-like vocalizations in infancy: an evaluation of potential risk factors. J Child Lang. 1994;21(1):33–58.
- Stoel-Gammon C. Relationships between lexical and phonological development in young children. J Child Lang. 2011;38(1):1–34.
- McCune L, Vihman M. Early phonetic and lexical development: a productivity approach. J Speech Lang Hear Res. 2001;44(3):670–684.
- Vihman MM, Greenlee M. Individual differences in phonological development: ages one and three years. J Speech Lang Hear Res. 1987;30(4):503–521.
- Stoel-Gammon C. Prelinguistic vocalizations of hearing-impaired and normally hearing subjects. J Speech Hear Dis. 1988;53(3):302–315.
- Oller DK, Eilers RE, Neal AR, et al. Precursors to speech in infancy: the prediction of speech and language disorders. J Comm Dis. 1999;32(4):223–245.
- Fasolo M, Majorano M, D'Odorico L. Babbling and first words in children with slow expressive development. Clin Ling Phon. 2008;22(2):83–94.
- Moeller MP, Hoover B, Putman C, et al. Vocalizations of infants with hearing loss compared with infants with normal hearing: part 1-phonetic development. Ear Hear. 2007;28(5):605–627.
- Moeller MP, Hoover B, Putman C, et al. Vocalizations of infants with hearing loss compared with infants with normal hearing: part II-transition to words. Ear Hear. 2007;28(5):628–642.
- Lieu JE. Unilateral hearing loss in children: speech-language and school performance. B-ENT. 2013;21:107–115.
- Alford RL, Arnos KS, Fox M, et al. American college of medical genetics and genomics guideline for the clinical evaluation and etiological diagnosis of hearing loss. Gen Med. 2014;16:347–355.
- Peterson NR, Pisoni DB, Miyamoto RT. Cochlear implants and spoken language processing abilities: review and assessment of the literature. Rest Neuro Neurosci. 2010; 28:237–250.
- McCreery RW, Walker EA. Pediatric amplification: enhancing auditory access. San Diego, CA: Plural Publishing; 2017.
- Most T, Harel T, Shpak T, et al. Perception of suprasegmental speech features via bimodal stimulation: cochlear implant on one ear and hearing aid on the other. J Speech Lang Hear Res. 2011;54(2):668–678.
- Anmyr L, Olsson M, Larson K, et al. Children with hearing impairment – living with cochlear implants or hearing aids. Int J Pediatr Otorhinolaryngol. 2011;75(6):844–849.
- Walker EA, McCreery RW, Spratford M, et al. Trends and predictors of longitudinal hearing aid use for children who are hard of hearing. Ear Hear. 2015; 36:38S–47S.
- Tomblin JB, Oleson JJ, Ambrose SE, et al. The influence of hearing aids on the speech and language development of children with hearing loss. JAMA Otolaryngol Head Neck Surg. 2014;140(5):403–409.
- Easwar V, Sanfilippo J, Papsin B, et al. Factors affecting daily cochlear implant use in children: datalogging evidence. J Am Acad Audiol. 2016;27(10):824–838.
- Klintö K, Salameh EK, Olsson M, et al. Phonology in Swedish-speaking 3-year-olds born with cleft lip and palate and the relationship with consonant production at 18 months. Int J Lang Com Dis. 2014;49(2):240–254.
- Willadsen E. Lexical selectivity in Danish toddlers with cleft palate. Cleft Palate Craniofac J. 2013;50(4):456–465.
- Walker E, Bass-Ringdahl S. Babbling complexity and it’s relationship to speech and language outcomes in children with cochlear implants. Otol Neurotol. 2008;29(2):225–229.
- Lieberman M, Lohmander A. Observation is a valid way of assessing common variables in typical babbling and identifies infants who need further support. Acta Paediatr. 2014;103(12):1251–1257.
- Lohmander A, Holm K, Eriksson E, et al. Observation method identifies that a lack of canonical babbling can indicate future speech and language problems. Acta Paediatr. 2017;106(6):935–943.
- Coninx F, Weichbold V, Tsiakpini L, et al. Validation of the LittleEARS®Auditory Questionnaire in children with normal hearing. Int J Pediatr Otorhinolaryngol. 2009;73(12):1761–1768.
- Persson A, Miniscalco C, Lohmander A, et al. Validation of the Swedish version of the LittlEARS® Auditory Questionnaire in children with normal hearing – sa longitudinal study. Int J Audiol. 2019;58:635–642.
- Atkinson G, Nevill AM. Statistical methods for assessing measurement error (reliability) in variables relevant to sports medicine. Sports Med. 1998;26(4):217–238.
- Weir JP. Quantifying test-retest reliability using the intra-class correlation coefficient and the SEM. J Strength Cond Res. 2005;19(1):231–230.
- Nathani S, Oller D. Beyond ba-ba and gu-gu: challenges and strategies in coding infant vocalizations. Beh Res Meth Instr Comput. 2001;33(3):321–330.
- Nyman A, Lohmander A. Babbling in children with neurodevelopmental disability and a simplified way of measuring canonical babbling ratio. Clin Ling Phon. 2018;32(2):114–127.
- Schramm B, Bohnert B, Keilmann A. The prelexical development in children implanted by 16 months compared with normal hearing children. Int J Pediatr Otorhinolaryngol. 2009;73(12):1673–1681.
- Moeller MP, McCleary E, Putman C, et al. Longitudinal development of phonology and morphology in children with late identified mild-moderate sensorineural hearing loss. Ear Hear. 2010;31(5):625–635.