Abstract
Our new double patch technique for repairing posteroinferior ventricular septal ruptures (VSRs) offers placement of patches in both the left and right ventricle, avoids ventriculotomies and gives good access and complete control of both AV-valves during implantation. We have treated two patients with this technique. Both survived with unremarkable status upon leaving the hospital.
Introduction
Surgical repair of posterior septal ruptures in acute myocardial infarction is hampered by a number of technical difficulties, and the prognosis for these patients is dubious even in the best of hands Citation1,2. The surgical repair is complicated with bleeding problems, non-patency of patch placements, distorted ventricular geometry in the repair process and trauma to an already infarcted left ventricle. No technique is perfect when repairing these severely damaged ventricles.
There are two dominant principles used in most clinics: the Daggett left ventricular patching Citation3 and the David infarct exclusion technique Citation1,4. Both these techniques demand a left ventriculotomy adding damage to the infarcted left ventricle. A transatrial approach with patch placement in the right ventricle has been proposed Citation5,6, but this “downstream” patch is prone to failure caused by the left-to-right pressure gradient. Finally, a double patch technique demanding two ventriculotomies has been proposed Citation7, but this technique is hampered by a high incidence of low output failure due to ventricular damage.
We have recently treated an 82-year-old woman and a 70-year-old man with a posterior postinfarct ventricular septal rupture (VSR) with a double patch repair through a biatrial approach. The technical aspects and rationale for the procedure are described in this paper.
Patients and surgical procedure
The first patient, an 82-year-old woman, was admitted after having had chest pain for several days at home. On admittance, the ECG was remarkable for having new Q-waves in the inferior leads (aVF, II and III). Nine days after being admitted, she developed orthopnoea and a new murmur. Echocardiography revealed a large posteroinferior ventricular setal rupture with a concomitant left-to-right shunt. She rapidly developed pulmonary oedema in the prone position and was transferred to our institution for surgery. On admittance she was markedly dyspnoeic and dependent on oxygen supplement, but had diuresis and a blood pressure of 110/70 mmHg. She was accepted for surgery without cardiac catheterization.
Surgical technique
During surgery, both atria were opened using the standard transseptal incision and opening the roof of the left atrium. By exposing the two ventricles through the AV-valves, the rupture in the proximal third of the posterior septum could easily be delineated and exposed using a cotton band ( and ). A large bovine pericardial patch intended for the left ventricular septal wall was sown in by placing the sutures through the patch and VSR from the right ventricular side. Using this technique, the sutures could be accurately placed by retracting and avoiding all of the tricuspid and mitral apparatuses. The patch was then pulled/pushed through the VSR from the right to the left side and positioned all the way from the base of the mitral valve to the mid-ventricular wall (). The inferior sutures placed on the diaphragmatic surface were anchored through the wall on a felt strip (). A new patch was then sown into the right wall of the septum using the same double armed pledgeted 2-0 sutures anchoring the left ventricular patch (). The tricuspid valve apparatus was retracted and the patch placed all the way to the right sided AV-plane. A total of 15 double armed sutures were used around the circumference. Three single vein grafts were placed on the LAD, circumflex and right coronary artery. The atria were then closed, the heart deaired and reperfused.
Figure 1. Location of the septal rupture. The septal rupture was found in the proximal part of the interventricular septum towards the inferior wall in both patients.
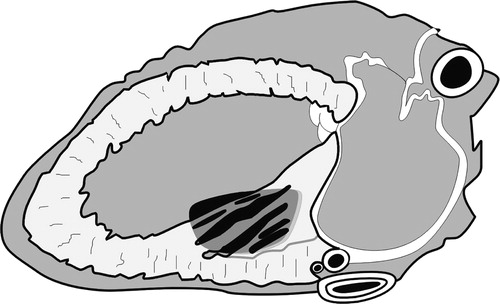
Figure 2. In order to delineate the extent of the defect and its exact location, a cotton band was pulled through the defect from the right to the left atrium.
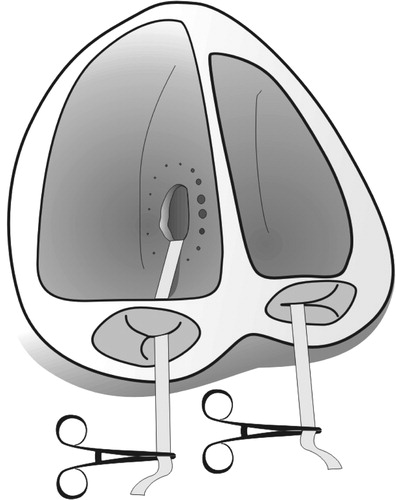
Figure 3. The figure illustrates the placement of all sutures and both patches through the tricuspid annulus and right ventricle (see text).
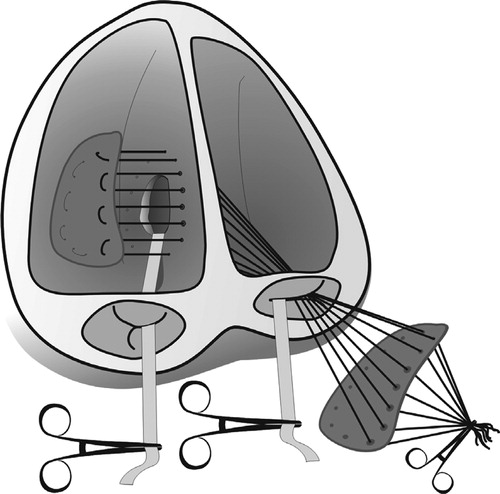
Figure 4. In the inferior part, the sutures were taken out of the ventricle and supported by Teflon felt on the diaphragmatic surface of the ventricle.

Control echocardiography demonstrated a patent patch and a globally contracting left ventricle. An aortic balloon pump was placed prophylactically. The recovery was remarkable for a day 2 reoperation due to a venous bleeding from the abdominal wall induced by drain removal. The patient made a slow recovery over the ensuing 3 weeks with a total ventilator time of 16 d and weaning via a tracheotomy.
Follow-up echocardiography on day 2 after the operation showed a small apical Doppler jet but no shunt fraction. After 6 months, the jet is unchanged and the patient has no symptoms and is at home and self-supportive. She is presently under observation for an abdominal aortic aneurysm.
The second patient was admitted with dyspnoea at rest 5 weeks after an episode of chest pain. He did not seek medical consultation during the period of chest pain. On admittance, his blood pressure was 90/60 mmHg, ECG showed an inferior myocardial infarction (Q-waves in lead aVF, II and III). A work up demonstrated a large posterior VSR with a shunt fraction of 66%, a main stem stenosis and triple-vessel coronary disease. He was operated with the described technique, quadruple vein bypasses and the left mammary artery to the LAD. His recovery was uneventful as he was extubated 2 h postoperatively and transferred to the floor on day 1 after the operation.
Discussion
The rationale for using this approach in these patients was primarily motivated from the desire to avoid a ventriculotomy in a patient with a small well-contracting left ventricle and an infarct mostly confined to the septum and right ventricle with less damage to the inferior left ventricular wall (echocardiography). In addition, the approach through both AV-valves allowed an excellent exposure of the proximal septum and therefore a precise definition of the VSR and extent of the infarcted muscle. The transatrial biventricular approach also allowed complete control of both valvular apparatuses and therefore we could avoid possible hooking of chordae, papillary muscles or valves. The double patch gave a secure and robust repair, and it is our proposal that the “self-anchoring” of two patches to an extent keeps the closure in spite of areas with progressive muscular necrosis or bad suture hold. The geometry of the ventricles is easy to maintain with the technique avoiding a possible restrictive effect from using a not-large-enough infarct-exclusion patch (“small-ventricular syndrome”) or crowding with flow problems in the outflow tract if the patch gets too big. Most importantly, the technique avoids additional ventricular damage; low-output failure is the most troublesome problem after both the Daggett and David techniques Citation2,7.
It should be noted that this technique is developed for posterior or basal VSRs. An apical VSR will be too far off from the AV-plane to allow an easy placement of patches using this approach.
References
- David TE, Armstrong S. Surgical repair of postinfarction ventricular septal defect by infarct exclusion. Semin Thorac Cardiovasc Surg 1998; 110: 105–10
- Barker TA, Ramnarine IR, Woo EB, Grayson AD, Aw J, Fabri BM, Bridgewater B, Grotte GJ. Repair of post-infarct ventricular septal defect with or without coronary artery bypass grafting in the northwest of England: A 5-year multi-institutional experience. Eur J Cardiothorac Surg 2003; 24: 940–6
- Daggett WM, Guyton RA, Mundth ED, Buckley MJ, McEnany MT, Gold HK, Leinbach RC, Austen WG. Surgery for postinfarct ventricular septal defect. Ann Surg 1977; 203: 269–71
- David TE, Dale L, Sun Z. Postinfarction ventricular septal rupture: Repair by endocardial patch with infarct exclusion. J Thorac Cardiovasc Surg 1995; 110: 1315–22
- Rousou JA, Engelman RM, Breyer RH, Whitteredge P, Schnider R. Transatrial repair of postinfarction ventricular septal defect. Ann Thorac Surg 1987; 43: 665–6
- Filgueira JL, Battistessa SA, Estable H, Lorenzo A, Cassinelli M, Scola R. Delayed repair of an acquired posterior septal defect through a right atrial approach. Ann Thorac Surg 1986; 42: 208–9
- Labrousse L, Choukron E, Chevalier LM, Madonna F, Robertie F. Surgery for post infarction ventricular septal defect (VSD): Risk factors for hospital death and long term results. Eur J Cardiothorac Surg 2002; 21: 725–31