Abstract
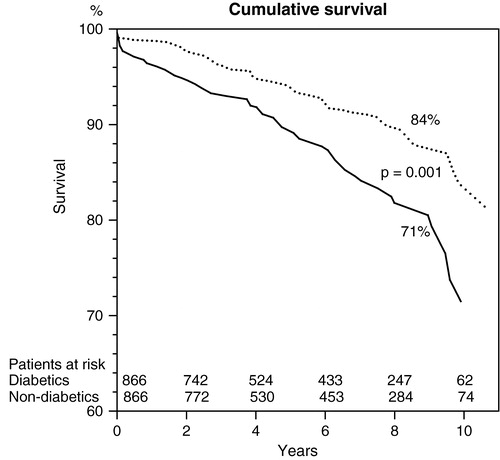
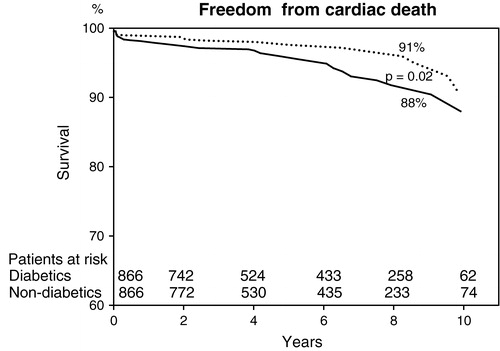
Objective. To determine the impact of diabetes on outcome after coronary artery bypass surgery. Design. We matched 866 diabetic patients with non-diabetic controls in regards to gender, age, left ventricular ejection fraction, body mass index, presence of unstable angina and history of myocardial infarction, and day of surgery. The 30-d mortality and morbidity were evaluated with univariate analysis and survival and freedom from cardiac death were assessed with the Kaplan–Meier method. Results. Follow-up time was 69±37 months. The 30-d mortality was 2.0% in the diabetic group and 1.0% in the non-diabetic group (p=0.15). Postoperative morbidity did not differ between groups. Cumulative 5- and 10-year survival rates were 89 and 71% in diabetics and 94 and 84% in non-diabetics (p=0.001). During follow-up, there was no difference between groups in regards to repeat revascularization. Conclusions. The 30-d mortality was equally low in diabetic and non-diabetic patients with severe coronary artery disease. However, long-term survival was significantly lower in the diabetic group than in the non-diabetic group.
Introduction
Diabetes mellitus is a major risk factor for cardiovascular disease, and coronary heart disease is the leading cause of death among adult diabetics. The frequency of acute myocardial infarction is higher, there are more complications during treatment, and the prognosis is poorer among diabetic than non-diabetic patients Citation1,2. In general, around 20% of patients undergoing coronary artery bypass surgery (CABG) suffer from diabetes mellitus. In the BARI trial, coronary artery bypass grafting (CABG) was found to provide superior long-term survival in diabetics with multivessel disease as compared to percutaneous coronary intervention (PCI) Citation3. Previous studies have demonstrated the adverse effect of diabetes mellitus on long-term survival after CABG Citation4–6. In a recently published study involving more than 146 000 patients, diabetes mellitus appeared to be an independent risk factor of 30-d mortality Citation7.
This case–control study was conducted to determine the effect of diabetes mellitus on short- and long-term outcome after CABG.
Material and methods
All relevant preoperative, perioperative and postoperative data of patients undergoing cardiac operations at Kuopio University Hospital were prospectively collected and stored in the cardiac surgical database used in this study. Between the beginning of 1992 and the end of 2001, 6113 patients underwent isolated first CABG at Kuopio University Hospital, 1084 of whom had diabetes mellitus. The diagnosis of diabetes was obtained from the patient information and clinical data of previously diagnosed diabetes or from patients undergoing drug treatment due to diabetes mellitus. In order to evaluate the effect of diabetes mellitus with the outcome after CABG, 1084 diabetic patients were individually matched to control patients in the non-diabetic group. The patients were matched regarding gender, age (±3 years), left ventricular ejection fraction (±5%), body mass index (±1 kg/m2), presence of unstable angina, history of myocardial infarction, and day of surgery (±2 months). The matching process was performed by one investigator blinded to the postoperative course of the patients. At the end of the matching process, no suitable match was found for 218 diabetic CABG patients. Thus, 866 pairs formed the final study population.
The data of cause and date of death were obtained from the National Causes-of-Death Register of Finland in March 2003. The information concerning PCI and REDO CABG performed after the primary CABG was obtained from the Finnish Social and Health Ministry registry. This study was approved by the ethical committee of Kuopio University Hospital.
Statistical analysis
The difference in continuous variables was analysed using the paired samples Student's t-test. Ordinal variables were analysed using the paired samples Marginal homogeneity test and dichotomized variables with the McNemar test. Survival curves were obtained with the Kaplan–Meier method. Statistical significance was calculated with the log-rank test. The continuous variables are presented as mean±standard deviation in the tables. Values of p<0.05 were regarded as statistically significant. All statistical procedures were performed with a statistical program SPSS for Windows, Release 11.5.1 (SPSS Inc., Chicago, IL, USA).
Results
The average follow-up time was 68.6±36.6 months (range 15–137 months). The clinical characteristics of the study groups are shown in . However, the proportion of current or ex-smokers was lower in diabetics than in non-diabetics. Fifty-five patients (6.4%) had type 1 diabetes and 811 (93.6%) had type 2 diabetes. There was no difference between the groups concerning the Canadian Cardiovascular Society angina (CCS) class, history of claudication, history of stroke or transient ischemic attack (TIA), or preoperative serum creatinine level. Three-vessel disease was more common in the diabetic group than in the non-diabetic group (92.0% vs 84.5%, respectively, p<0.001). The number of distal anastomoses was higher in the diabetic group than in the non-diabetic group (4.42±1.12 vs 4.25±1.17, respectively, p=0.001). Use of an internal thoracic artery graft was uniform in both groups (97.9%). Four diabetic and 10 non-diabetic patients had bilateral internal thoracic artery grafts; seven diabetic and five non-diabetic patients had either radial artery or right gastroepiploica artery grafts; and the rest of the bypasses were performed using saphenous vein grafts. Cross-clamp time was longer in the diabetic group than in the non-diabetic group (93±30 min vs 88±29 min, respectively, p=0.002).
Table I. Preoperative patient characteristics and operative data.
Mortality and morbidity
Morbidity and postoperative data are presented in . The 30-d mortality was 2.0% in the diabetic group and 1.0% in the non-diabetic group (p=0.15). There was also no difference between the groups concerning postoperative data listed in . The length of stay in the intensive care unit (ICU), length of hospital stay and readmission rate to ICU were similar between groups.
Table II. Mortality and postoperative data.
Survival and freedom from cardiac death
During the follow-up period, 125 (14.4%) diabetic and 71 (8.2%) non-diabetic patients died (p=0.00002). Cumulative 5- and 10-year survival rates were 89 and 71% in diabetics and 94 and 84% in non-diabetics (p=0.001, ). Cumulative 5- and 10-year freedom from cardiac death rates were 96 and 88% in diabetics and 97 and 91% in non-diabetics (p=0.02, ). Cumulative survival and cumulative freedom from cardiac death did not differ between type 1 and type 2 diabetics (p=0.54 and 0.96, respectively).
Re-interventions
There was no difference between the groups in the incidence of re-interventions during the follow-up period. New PCI was performed on 14 (1.6%) diabetic and 11 (1.3%) non-diabetic patients (p=0.69). Nine patients (1.0%) in the diabetic group and seven (0.8%) in the non-diabetic group underwent REDO CABG during follow-up (p=0.84).
Discussion
In our study, the short-term mortality after CABG was 2% in diabetic patients with severe coronary artery disease. Mortality was not higher than that among non-diabetic patients after matching with the relevant clinical factors for coronary heart disease. However, during 5 or 10 years of follow-up, the mortality was higher in diabetic patients than in non-diabetic patients demonstrating the deleterious effect of diabetes on the cardiovascular system.
Several studies have reported the influence of diabetes on the short- and long-term outcome after CABG Citation4–12, with somewhat conflicting results. We studied the influence of diabetes per se on outcome after CABG by matching a large number of diabetic and non-diabetic patients regarding seven important clinical characteristics, to make the study groups as comparable as possible. The study groups had statistically significant differences in a few preoperative or intraoperative variables. Three-vessel disease was more common in diabetic patients than in non-diabetics (92% vs 84.5%, respectively) and diabetic patients had 0.2 distal anastomoses more than non-diabetic patients and 5 min longer cross-clamp time than non-diabetic patients. These differences reached statistical significance because of the large number of patients in the study groups, but the clinical importance of these minor differences remains low. In addition to very comparable study groups, other strengths of our study are the completeness of survival data, prospective data collection and the large number of patients in the study groups.
In agreement with other reports Citation5,10 we did not find differences in 30-d mortality between diabetic and non-diabetic patients. Some studies have found diabetes to be an independent predictor for early postoperative death Citation4,7,8,11,12, but all are retrospective, and did not match diabetic and non-diabetic groups, nor are they comparable with regard to other factors. In a recently published study by Carson et al. Citation7 including 146 786 patients undergoing isolated CABG, mortality was higher in both diabetic and non-diabetic patients (3.7 and 2.7%, respectively) than in our study and they found diabetes to be an independent predictor of 30-d mortality (odds ratio 1.23). Importantly, in their analysis cardiac mortality was lower in diabetics than in non-diabetics, suggesting that excess short-term mortality in diabetics is due to non-cardiac causes. On the other hand, Calafiore et al. Citation8 reported in their retrospective study that diabetes was an independent risk factor only for early cardiac death and not for death of any cause.
Diabetic patients have been reported to have higher incidence of peri- and postoperative neurological complications Citation4, but the incidence of postoperative stroke was similar in both groups in our study. There are reports demonstrating increased risk of postoperative wound infections in diabetic patients Citation7,13,14. Only four diabetic patients had bilateral internal thoracic artery grafts in our study. It has been clearly demonstrated that adequate glucose control lowers the risk of postoperative wound infection in diabetic patients Citation15–17. Since the report by Zerr et al. in 1997 Citation15, we took continuous insulin infusions in diabetic patients in clinical practice, so around half of the patients in the diabetic group had continuous insulin infusion postoperatively. These two factors might explain the low incidence of deep sternal wound infection in the diabetic patients.
Our study confirmed that diabetics have worse long-term survival and lower freedom from cardiac death after CABG than non-diabetics. The poorer survival of diabetics than non-diabetics is due to both non-cardiac deaths and excessive cardiovascular mortality. This is in agreement with most of the published studies Citation4–6, Citation9–11. In one retrospective report, long-term survival in patients who survived the first 30 d was not statistically significantly different for diabetic and non-diabetic patients Citation8. Reports have shown a better long-term outcome in diabetic patients if one or two internal thoracic artery grafts were used Citation18, Citation19. Almost all (97.9%) of the diabetic patients in our study group had left internal thoracic artery to left anterior descending artery, but long-term outcome of diabetic patients compared with controls was still impaired. Recently Endo et al. Citation20 demonstrated the benefit of using the bilateral internal thoracic artery in diabetic patients with left ventricle ejection fraction greater than 40%: the 10-year survival rate was 88% in patients who received a bilateral thoracic artery graft, compared with 75% in patients who received a single internal thoracic artery graft. The 10-year survival rate did not differ in patients with left ventricle ejection fraction less than 40% in their analysis.
Although cardiac death was more common in diabetics than in non-diabetics, diabetic patients did not have more revascularizations during follow-up. In general, diabetic patients have more severe coronary artery disease and rapid progression of atherosclerosis, due to hyperglycaemia, and an unfavourable serum lipid profile and a hypercoagulable state. In addition, diabetes has deleterious effects on myocardial metabolism leading to increased risk of heart failure and excessive cardiovascular mortality. In our study it is not possible to evaluate the effect of diabetic metabolism on long-term mortality, because due to our study setting we did not separately determine the glycosylated haemoglobin A1 level.
In conclusion, in our study diabetic and non-diabetic patients had similar low short-term morbidity and mortality after CABG. In contrast long-term survival was markedly impaired in diabetic patients, due to an excess of both cardiac and non-cardiac mortality. Aggressive treatment of risk factors and adequate diagnosis and treatment of recurrent ischemia after CABG is required in order to improve long-term survival in diabetic patients.
This study was financially supported by Kuopio University Hospital.
References
- Stone PH, Muller JE, Hartwell T, York BJ, Rutherford JD, Parker O, Turi ZG, Strauss HW, Willerson JT, Robertson T. The effect of diabetes mellitus on prognosis and serial left ventricular function after acute myocardial infarction: Contribution of both coronary disease and diastolic left ventricular dysfunction to the adverse prognosis: The MILIS study group. J Am Coll Cardiol 1989; 14: 49–57
- Herlitz J, Malmberg K, Karlson BW, Ryden L, Hjalmarson A. Mortality and morbidity during a five-year follow-up of diabetics with myocardial infarction. Acta Med Scand 1988; 224: 31–8
- BARI investigators. Influence of diabetes on 5-year mortality and morbidity in a randomized trial comparing CABG and PTCA in patients with multivessel disease. Circulation 1997; 96: 1761–9
- Herlitz J, Wognsen GB, Emanuelsson H, Haglid M, Karlsson BW, Karlsson T, Albertsson P, Wesberg S. Mortality and morbidity in diabetic and nondiabetic patients during a 2-year period after coronary artery bypass grafting. Diabetes Care 1996; 19: 698–703
- Risum O, Abdelnoor M, Svennevig JL, Levorstad K, Gullestad L, Bjornerheim R, Simonsen S, Nitter-Hauge S. Diabetes mellitus and morbidity and mortality risks after coronary artery bypass surgery. Scand J Thorac Cardiovasc Surg 1996; 30: 71–5
- Barzilay JI, Kronmal RA, Bittner V, Eaker E, Evans C, Foster ED. Coronary artery disease and coronary artery bypass grafting in diabetic patients aged ≥65 years: Report from the coronary artery surgery study registry. Am J Cardiol 1994; 74: 334–9
- Carson JL, Scholz PM, Chen AY, Peterson ED, Gold J, Schneider SH. Diabetes mellitus increases short-term mortality and morbidity in patients undergoing coronary artery bypass graft surgery. J Am Coll Cardiol 2002; 40: 418–23
- Calafiore AM, Di Mauro M, Di Giammarco G, Contini M, Iaco AL, Canosa C, Dalessandro S. Effect of diabetes on early and late survival after isolated first coronary bypass surgery in multivessel disease. J Thorac Cardiovasc Surg 2003; 125: 144–54
- Barsness GW, Peterson ED, Ohman EM, Nelson CL, DeLong ER, Reves JG, Smith PK, Anderson D, Jones RH, Mark DB, et al. Relationship between diabetes mellitus and long-term survival after coronary bypass and angioplasty. Circulation 1997; 96: 2551–6
- Szabo Z, Håkanson E, Svedjeholm R. Early postoperative outcome and medium-term survival in 540 diabetic and 2239 nondiabetic patients undergoing coronary artery bypass grafting. Ann Thorac Surg 2002; 74: 712–9
- Thourani VH, Weintraub WS, Stein B, Gebhard SSP, Craver JM, Jones EL, Guyton RA. Influence of diabetes mellitus on early and late outcome after coronary artery bypass grafting. Ann Thorac Surg 1999; 67: 1045–52
- Cohen Y, Raz I, Merin G, Mozes B. Comparison of factors associated with 30-day mortality after coronary artery bypass grafting in patients with versus without diabetes mellitus. Am J Cardiol 1998; 81: 7–11
- Fietsam RJ, Basset J, Glover J. Complications of coronary artery surgery in diabetic patients. Am J Surg 1991; 57: 551–7
- Tavolacci MP, Merle V, Josset V, Bouchart F, Litzler PY, Tabley A, Bessou JP, Czernichow P. Mediastinitis after coronary artery bypass graft surgery: Influence of mammary grafting for diabetic patients. J Hosp Infect 2003; 55: 21–5
- Zerr KJ, Furnary AP, Grunkemeier GL, Bookin S, Kanhere V, Starr A. Glucose control lowers the risk of wound infection in diabetics after open heart operations. Ann Thorac Surg 1997; 63: 356–61
- Furnary AP, Zerr KJ, Grunkemeier GL, Starr A. Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures. Ann Thorac Surg 1999; 67: 352–62
- Lazar H, Chipkin S, Fitzgerald CA, Bao Y, Cabral H, Apstein CS. Tight glycemic control in diabetic coronary artery bypass graft patients improves perioperative outcomes and decreases recurrent ischemic events. Circulation 2004; 109: 1497–502
- Hirotani T, Kameda T, Kumamoto T, Shirota S, Yamano M. Effects of coronary artery bypass grafting using internal mammary arteries for diabetic patients. J Am Coll Cardiol 1999; 34: 532–8
- Pick AW, Orszulak TA, Anderson BJ, Schaff HV. Single versus bilateral internal mammary artery grafts: 10-year outcome analysis. Ann Thorac Surg 1997; 64: 599–605
- Endo M, Tomizawa Y, Nishida H. Bilateral versus unilateral internal mammary revascularization in patients with diabetes. Circulation 2003; 108: 1343–9