Abstract
Objective. Current guidelines for treatment of intermittent claudication (IC) do not include a specific recommendation for the intensity of exercise therapy. Thus, the purpose of this study was to determine the relative effectiveness of high versus low intensity exercise for patients with IC, and further to study the effect of such training on blood flow to the legs during exercise. Design. The effect of eight weeks of supervised endurance training was examined in 16 patients with IC. The patients were randomly assigned to training at intensities corresponding to either 60% or 80% of their peak oxygen consumption (VO2peak), respectively. Results. VO2peak and time to exhaustion increased significantly (9% and 16%, respectively) more in the high intensity group (p<0.05). Blood flow to the legs did not change after training in any of the groups. Conclusion. High intensity training gave larger improvements in VO2peak and time to exhaustion than low intensity training. As blood flow did not change after the exercise program, it is likely that the observed different increase of VO2peak was due to changed mitochondrial oxidative capacity and/or skeletal muscle diffusive capacity.
Intermittent claudication (IC) denotes pain that develops in the affected limb with exercise and is relieved with rest Citation1. A recent epidemiological study showed that the prevalence of symptomatic IC was about 4% in men and 2% in women aged 65 years or older. Peripheral artery disease (Ankle/Brachial Index <0.9) had a prevalence of 18%, and carried significant cardio- and cerebrovascular co-morbidity Citation2. Patients with IC have a lower maximal oxygen consumption (VO2max) Citation3 and a higher O2 consumption at submaximal work rates Citation4 than healthy individuals. Over the last decades several studies have shown that physical exercise at a wide range of intensities improves VO2peak Citation5–7 and work economy Citation7 in patients with IC. High intensity training has been shown to be more effective than low or moderate intensity training for improving VO2max in healthy subjects and in patients with stable coronary artery disease Citation8–10. However, for patients with IC the most effective training regime and the underlying mechanisms remain yet unknown Citation11. Thus, the primary aim of the present study was to evaluate the relative effectiveness of exercise with high and low intensity for improving VO2peak and time to exhaustion in patients with IC.
In unfit subjects there is probably a demand limitation in the oxygen transport, while in athletes exercising with large muscle mass; a supply limitation has been demonstrated Citation12. Thus, the fact that IC patients are characterised as unfit indicates a demand limitation, and this is supported by studies showing limitations in muscle energy metabolism Citation13, Citation14 and lack of change in blood flow after training Citation15. However, significant arterial stenoses reduce blood flow and give ischemic symptoms and this indicates that their exercise capacity is supply limited. Consequently, it is not clear whether oxygen transport in patients with intermittent claudication is demand or supply limited. Thus, the secondary aim of this study was to assess the contribution of regional blood flow to the training-induced improvement in exercise capacity.
Material and methods
Nineteen patients participated in the study after reviewing and signing consent forms. The study was approved by the ethical committee at the Norwegian University of Science and Technology and performed in accordance with the Declaration of Helsinki. The inclusion criteria were an ankle-brachial index (ABI) ≤0.9 in one or both of the lower extremities, and that claudication pain was limiting exercise capacity. Eight patients had unilateral and eleven patients had bilateral claudication pain. Patients were excluded if their walking capacity was limited by other factors than claudication, or if they were not able to walk on a treadmill at 4 km h−1. The patients were assigned to two groups by computer generated random numbers (block randomization) before the patients where seen by the study investigators. Three patients withdrew from the study due to personal reasons. The physical characteristics of the patients are shown in .
Table I. Physical and physiological characteristics of patients at pre-test.
Ankle Brachial Index (ABI)
ABI was measured within a month before pre-test, and within 2 days after post-test using a custom made device which recorded blood pressure simultaneously in the posterior tibial and the brachial artery. Systolic pressure was recorded as the pressure at the first detected flow during cuff deflation using ultrasound Doppler flow probes.
Treadmill Testing
Resting values of blood lactate ((La−)b) (YSI 1500 Sport Lactate Analyser, Yellow Springs Instrument Co, USA), heart rate (HR) (Polar Sport Tester, Polar Electro Oy, Finland) and blood pressure in the brachial artery were recorded in the sitting position. Blood pressure was measured using an oscillometric vital signs monitor (Scholar™ II/507E Series, Criticare systems, inc., USA), which also included an oxygen saturation (SaO2) recorder. VO2peak was measured using a treadmill (Woodway, USA) stepwise rank protocol consisting of 2 minute work periods at a speed of 4 km h−1 separated by 5 minute breaks. The treadmill inclination at start was 0%, and increased by 3% for every work period. If the patients reached an inclination of 18%, the next and maximum inclination was 20%. If patients still continued work, speed was increased by 0.5 km h−1 for every work period. The test was stopped when the patients could no longer complete a full two minute work period. The treadmill was calibrated for speed and inclination before the study. VO2 was measured continuously during all work periods using a Vmax 29 (Vmax series, SensorMedics Co, USA) which analysed expired air and calculated the average O2-uptake over 30 second intervals. VO2peak was recorded as the highest value obtained during the work periods. The procedure for measuring VO2max and HRmax has previously been described by Helgerud et al. Citation16. In the present study we also used VO2 values in the units of mL kg−0.75 min−1 to take dimensional scaling into account when comparing the subjects’ different body weights Citation17. HR and SaO2 were measured during the last 10 seconds of the work periods. Immediately after each work period the patients assessed work load on the Borg self-perceived exertion scale, and blood pressure was recorded simultaneously. (La−)b was measured if the patients evaluated the exertion to be ≥4 on the Borg scale. The patients then sat down and rested until the next work period began. Work economy was calculated as VO2 divided by the calculated work (in Watts) during submaximal treadmill walking.
Ultrasound Measurements and Strength Test
Blood flow was measured in the popliteal artery during supine one-leg ankle plantar flexion exercise. The lower extremity with the lowest ABI was chosen for all measurements. The patients were lying in prone position and mean blood velocity (MBV) and arterial diameter (da) were recorded with a flat phased array probe placed in the popliteal fossa (centre frequency 6 MHz, Doppler frequency 3.65 MHz) and a System FiVe scanner (GE Vingmed Ultrasound, Horten, Norway). A cable pulley was connected with a static rope to a pedal attached to the patient's foot. One kg weights were used for the cable pulley. Obstacles secured standardised movements and stabilised the calf. After obtaining resting values, the pedal from the cable pulley was attached to the patient's foot, and 1 repetition maximum (1RM) for plantar flexion was measured. Thereafter patients performed three two minute work periods with weight loads of ∼20%, 30%, and 50% of 1RM, respectively, separated by five minute breaks. The work frequency was set by a metronome to yield 25 contraction/relaxation cycles per minute. The same absolute loads were used in the post-test. Popliteal blood flow was measured during the last 30 seconds and immediately after (within 30 seconds) each period. Details of the ultrasound measurements have been described previously by Amundsen et al. Citation18.
Training Intervention
The training program consisted of three guided treadmill walking exercise sessions per week for eight weeks, giving a total of 24 sessions. The intensity level was set to 60% of VO2peak in the low intensity group and 80% of VO2peak in the high intensity group. In the high intensity group the patients walked eight periods of two minutes, separated by three minutes sit-down breaks. In the low intensity group the patients either walked continuously for 30 minutes or until the pain was so severe that further walking were impeded. For the latter, patients took breaks of five minutes and continued work until a 30 minute work period was completed. The exercise time in the low intensity group was matched to that of the high intensity group, to ensure that only intensity differed between the groups. Speed and inclination during training were set to the values that yielded the desired level of VO2 in the treadmill test. HR was recorded during all sessions. Intensities of 60% and 80% of VO2peak correspond to approximately 70% and 90% of HRpeak, respectively Citation17, Citation19. Since VO2peak and work economy adapt to training, the work load had to be adjusted during the training period to maintain the relative intensity level. All patients therefore underwent two maximal work tests after 1/3 and 2/3 of the training period to adjust work load.
Statistical Analysis
Non-parametric statistics were used due to small groups. The Mann-Whitney U test was used to compare the changes in the two intensity groups from pre- to post-test. Wilcoxon signed rank test was used to compare pre- and post-test values. A difference was considered significant if the p-value was <0.05. Statistical analysis included only patients with values from both pre- and post-test. Values are given in mean±SD.
Results
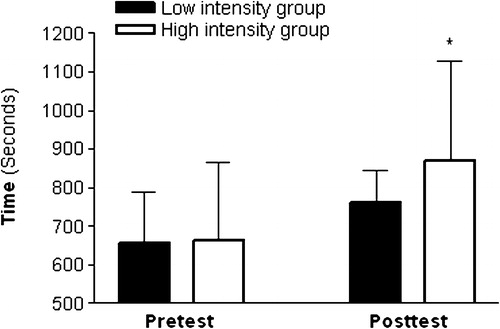
The low intensity group completed 98%, and the high intensity group 96%, of all planned training sessions. The increase of VO2peak after training was larger in the high intensity group compared to the low intensity group (16% vs. 9%, p<0.05; ). At submaximal workloads both groups increased work economy by 14% with no significant difference between the groups. The increase of time to exhaustion was larger in the high intensity group compared to the low intensity group (31.4% vs. 15.7%, p<0.05; ).
Figure 1. Peak oxygen uptake (mean + SD) for both groups at pre-test and post-test. *Significant difference between groups (p<0.05).
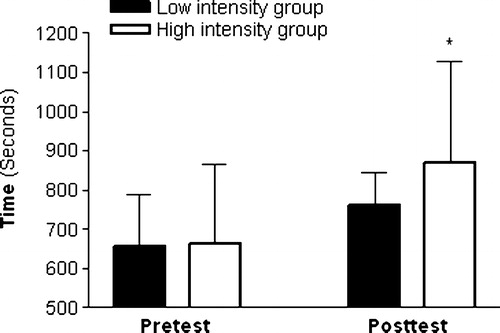
Figure 2. Time to exhaustion (mean + SD) for both groups at pre-test an post-test. *Significant difference between groups (p<0.05).
There were no differences between the low and high intensity groups in mean blood velocity, arterial diameter, or blood flow after training (). One repetition maximum increased by 22.6% in the low intensity group and 28.7% in the high intensity group. There was no significant difference between groups. The changes of HRpeak; HR; ((La−)b); SaO2; experience of exhaustion and ABI were not different between groups, neither were there any changes within each group after training.
Table II. Blood flow in the popliteal artery during plantar flexion exercise at increasing loads.
Discussion
The major finding in the present study was that high intensity training was more effective than a matched volume of low intensity training for improving VO2peak and time to exhaustion in patients with intermittent claudication. This confirms that adaptations to physical exercise follow the same pattern in IC patients as in healthy subjects, even though their VO2peak may have other limitations Citation8, Citation9, Citation20. This study underscores the importance of not only recommending physical training for the treatment of IC, but also to include recommendations on the intensity level of training.
Time to exhaustion increased significantly more in the high intensity group than in the low intensity group. This is expected as VO2peak increased only after high intensity training, in accordance with previous studies Citation21–26. Since no improvement was observed in VO2peak in the low intensity group, the 16% improvement in time to exhaustion was likely caused by improved work economy. Thus, we conclude that adaptations in VO2peak are intensity-dependent in patients with IC, while improvements in work economy are not. Improved work economy in this patient group after training has been found previously Citation7.
VO2peak values for the patients in this study were approximately 20 mL kg−1 min−1, while in other studies measurements range from 13–18 mL kg−1 min−1 Citation3, Citation5–7, Citation27. The breaks during the test protocol in the present study allowed restitution for the hypoxic muscles, with the effect that the patients were able to work at a steeper inclination and achieve a larger VO2peak than they would have with a continuous protocol Citation5–7, Citation27. Measuring too low VO2peak values will lead to miscalculation of training intensity and the effect of the training intervention.
The two exercise groups did not show any training induced difference in blood flow, MBV, or da, in accordance with previous studies Citation15. Thus, the increase in VO2peak could not be explained by an adaptation in the oxygen-supplying cardiovascular system. In previous studies a lack of increased maximal blood flow has been ascribed to insufficient training intensity Citation28, but this is not supported by the present study where intensity was high and VO2peak increased.
During exercise patients with IC are limited by the muscles in the lower extremities, distal to the atherosclerotic lesions. This is a relatively small amount of muscle, and Shephard et al. Citation29 showed that as working muscle mass decreased, there was a shift in limitation of VO2peak from central oxygen supply to local muscle limitation. Also, patients with IC are unfit, and a metabolic demand limitation has been shown in healthy unfit subjects when working with a large muscle mass Citation12. Limitations in oxygen supply factors for VO2max are first seen when healthy subjects become fit Citation30. It is possible that a longer training intervention than in the present study would have caused a shift in limitation from diffusive capacity or metabolic rate to central oxygen supply as the patients had become fit. If not caused by a change in blood flow, the increase of VO2peak could have been due to an increased number of capillaries or redistribution of flow leading to a better oxygen perfusion in the muscles. However, a relation between number of capillaries and VO2max has only been shown in healthy subjects Citation31, Citation32. Previously several mitochondrial abnormalities have been found in patients with IC Citation13, Citation14, Citation33, Citation34, possibly indicating a defective energy metabolism in the mitochondria of the claudicating muscle. Training might have corrected such a defect.
Conclusion
High intensity interval training at 80% of VO2peak was more effective in improving VO2peak and time to exhaustion than low intensity training at 60% of VO2peak for patients with IC. Work economy improved similarly in both groups. No significant differences between groups were observed in changes of blood pressure, regional blood flow, 1RM, HRpeak, SaO2, experience of exhaustion, or ABI. Since no differences were found in the latter parameters, a change in oxygen demand in the exercising muscles is suggested.
We wish to thank Elin A. Amundsen for help with recruiting patients to the study.
References
- Weitz JI, Byrne J, Clagett GP, Farkouh ME, Porter JM, Sackett DL, et al. Diagnosis and treatment of chronic arterial insufficiency of the lower extremities: A critical review. Circulation 1996; 94: 3026–49
- Diehm C, Schuster A, Allenberg JR, Darius H, Haberl R, Lange S, et al. High prevalence of peripheral arterial disease and co-morbidity in 6880 primary care patients: cross-sectional study. Atherosclerosis 2004; 172: 95–105
- Bauer TA, Regensteiner JG, Brass EP, Hiatt WR. Oxygen uptake kinetics during exercise are slowed in patients with peripheral arterial disease. J Appl Physiol. 1999; 87: 809–16
- Gardner AW, Skinner JS, Vaughan NR, Bryant CX, Smith KL. Comparison of three progressive exercise protocols in peripheral vascular occlusive disease. Angiology 1992; 43: 661–7
- Hiatt WR, Regensteiner JG, Hargarten ME, Wolfel EE, Brass EP. Benefit of exercise conditioning for patients with peripheral arterial disease. Circulation 1990; 81: 602–9
- Izquierdo-Porrera AM, Gardner AW, Powell CC, Katzel LI. Effects of exercise rehabilitation on cardiovascular risk factors in older patients with peripheral arterial occlusive disease. J Vasc Surg. 2000; 31: 670–7
- Womack CJ, Sieminski DJ, Katzel LI, Yataco A, Gardner AW. Improved walking economy in patients with peripheral arterial occlusive disease. Med Sci Sports Exerc. 1997; 29: 1286–90
- Pollock ML, Gaesser GA, Butcher JD, Després JP, Dishman RK, Franklin B, et al. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory fitness, and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 1998; 30: 975–91
- Wenger HA, Bell GJ. The interactions of intensity, frequency and duration of exercise training in altering cardiorespiratory fitness. Sports-Med. 1986; 3: 346–56
- Rognmo O, Hetland E, Helgerud J, Hoff J, Slørdahl SA. High intensity aerobic exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur J Cardiovasc prev Rehabil. 2004; 11: 216–22
- Thompson PD, Buchner D, Pina IL, Balady GJ, Williams MA, Marcus BH, et al. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: a statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity). Circulation 2003; 107: 3109–16
- Wagner PD. New ideas on limitations to VO2max. Exerc Sports Sci Rev. 2000; 28: 10–14
- Hiatt WR, Wolfel EE, Regensteiner JG, Brass EP. Skeletal muscle carnitine metabolism in patients with unilateral peripheral arterial disease. J Appl Physiol. 1992; 73: 346–353
- Lundgren F, Dahllof AG, Schersten T, Byllund-Fellenius AC. Muscle enzyme adaptation in patients with peripheral arterial insufficiency: spontaneous adaptation, effect of different treatments and consequences on walking performance. Clin Sci. 1989; 77: 485–93
- Stewart KJ, Hiatt WR, Regensteiner JG, Hirsch AT. Exercise training for claudication. N Engl J Med. 2002; 347: 1941–51
- Helgerud J, Ingjer F, Strømme SB. Sex differences in performance-matched marathon runners. Eur J Appl Physiol. 1990; 61: 433–9
- Helgerud J. Maximal oxygen uptake, anaerobic threshold and running economy in women and men with similar performances level in marathons. Eur J Appl Physiol. 1994; 68: 155–61
- Amundsen BH, Wisløff U, Helgerud J, Hoff J, Slørdahl SA. Ultrasound recorded axillary artery blood flow during elbow-flexion exercise. Med Sci Sports Exerc. 2002; 34: 1288–93
- Franklin BA, Hodgson J, Buskirk ER. Relationship between percent maximal O2 uptake and percent maximal heart rate in women. Res Q Exerc Sport. 1980; 51: 616–24
- Helgerud J, Engen LC, Wisløff U, Hoff J. Aerobic endurance training improves soccer performance. Med Sci Sports Exerc. 2001; 33: 1925–31
- Regensteiner JG. Exercise in the treatment of claudication: assessment and treatment of functional impairment. Vasc med. 1997; 2: 238–42
- Brandsma JW, Robeer BG, van den Heuvel S, Smit B, Wittens CHA, Oostendorp RAB. The effect of exercises on walking distance of patients with intermittent claudication: A study of randomized clinical trials. Phys Ther. 1998; 78: 278–88
- Brendle DC, Joseph LJO, Coretti MC, Gardner AW, Katzel LI. Effects of exercise rehabilitation on endothelial reactivity in older patients with peripheral arterial disease. Am J Cardiol. 2001; 87: 324–9
- Carter SA, Hamel ER, Paterson JM, Snow CJ, Mymin D. Walking ability and ankle systolic pressures: Observations in patients with intermittent claudication in a short-term walking exercise program. J Vasc Surg. 1989; 10: 642–9
- Gardner AW, Katzel LI, Sorkin JD, Killewich LA, Ryan A, Flinn WR, et al. Improved functional outcomes following exercise rehabilitation in patients with intermittent claudication. J Gerontology. 2000; 55: M570–577
- Gardner AW, Katzel LI, Sorkin JD, Bradham DD, Hochberg MC, Flinn WR, et al. Exercise rehabilitation improves functional outcomes and peripheral circulation in patients with intermittent claudication: A randomized controlled trial. J Am Geriatr Soc. 2001; 49: 755–62
- Hiatt WR, Wolfel EE, Meier RH, Regensteiner JG. Superiority of treadmill walking exercise versus strength training for patients with peripheral arterial disease. Circulation. 1994; 90: 1866–74
- Remijnse-Tamerius HCM, Duprez D, De Buyzere M, Oeseburg B, Clement DL. Why is training effective in the treatment of patients with intermittent claudication?. Int Angiol. 1999; 18: 103–12
- Shephard RJ, Bouhlel E, Vanderwalle H, Monod H. Muscle mass as a factor limiting physical work. J Appl Physiol. 1988; 64: 1472–9
- Bassett DR, jr, Howley ET. Limiting factors for maximum oxygen uptake and determinants of endurance performance. Med Sci Sports Exerc. 2000; 32: 70–84
- Ingjer F. Maximal aerobic power related to the capillary supply of the quadriceps femoris muscle in man. Acta Physiol Scand. 1978; 104: 238–40
- Ingjer F. Effects of endurance training on muscle fibre ATP-ase activity, capillary supply and mitochondrial content in man. J Physiol. 1979; 294: 419–32
- Bath HK, Hiatt WR, Hoppel CL, Brass EP. Skeletal muscle mitochondrial DNA injury in patients with unilateral peripheral arterial disease. Circulation. 1999; 99: 807–12
- Pipinos II, Shepard AD, Anagnostopoulos PV, Katsamouris A, Boska MD. Phosphorus 31 nuclear magnetic resonance spectroscopy suggests a mitochondrial defect in claudicating skeletal muscle. J Vasc Surg. 2000; 31: 944–52