Abstract
The significant risk of cerebral embolism during cardiopulmonary bypass (CPB) makes monitoring of embolic events advisable already when developing new operation and coagulation management strategies for example in CPB animal models. The present study therefore evaluated in a porcine CPB model the feasibility of bilateral epicarotid Doppler signal recording and the quality of manual or automatic emboli detection. A total of 42 recordings (e.g. right carotid artery (n =20), left carotid artery (n =22)) were evaluated. The frequency of emboli counts was comparable for both carotid arteries. Automatic emboli detection, however, found significantly more embolic events per pig than did post-hoc manual off-line analysis of the recordings (172±217 vs. 13±10). None of the brains, however, showed any emboli or infarction area either in cross-examination or in histological evaluation. In conclusion, the present study showed the feasibility of using an epicarotid Doppler device for bilateral emboli detection in a porcine CPB model. Automatic on-line emboli detection, however, reported more embolic events than did post hoc, off-line manual analysis. Possible reasons for this discrepancy are discussed.
During cardiopulmonary bypass (CPB) the risk of cerebral embolism is always imminent Citation1–3. Solid emboli originating from atherosclerotic lesions or thrombotic material but also gaseous emboli due to air entrapment put the patient at risk for perioperative stroke Citation4–6. Intraoperative emboli detection by continuous transcranial Doppler sonography (TCD) of the middle cerebral arteries or the carotid arteries has lately become possible Citation7, Citation8. Changes in operation strategy but also in coagulation management have a potential impact on the risk for emboli during CPB. Therefore, it is of utmost importance to monitor occurrence of emboli already when developing such new management strategies in CPB animal models. Emboli detection can be based either on manual off-line evaluation of the Doppler signal or on implemented automatic detection algorithms. The feasibility and above all quality of manual or automatic emboli detection have not been evaluated in CPB animal models to date. The present study, therefore, evaluated the feasibility and compared manual off-line with automatic on-line emboli detection in a porcine CPB model. In addition, all pigs were histologically screened for morphologic alterations due to cerebral embolism.
Materials and methods
Animals
The study protocol was approved by the Austrian Federal Animal Investigation Committee (GZ 66.011/68–BrGT/2003), and pigs (German/Pietrain; n = 34; 15–18 wk old; 36–55 kg body weight) were managed in accordance with the guidelines of the National Institutes of Health. Animals were fasted overnight but had free access to water. Pigs were premedicated with azaperone (4 mg/kg intramuscular) and atropine (0.01 mg/kg intramuscular) one hour before surgery. Following induction of anesthesia with ketamine (20 mg/kg intramuscular) and propofol (2–4 mg/kg intravenous) and tracheal intubation, pigs were normoventilated (fraction of inspired oxygen (FiO2), 0.4; endtidal carbon dioxide concentration (EtCO2), 40 mmHg). Anesthesia was maintained with propofol (6–8 mg/kg/h) and boli of piritramid (30–45 mg). Ringer's solution (10 mL/kg/h) was administered throughout the experiment. No paralyzing agent was used. Monitoring included a standard lead II electrocardiogram and invasive blood pressure measurement in the femoral artery (diameter: 1.2 mm; Leader Cath, Vygon GmbH, Aachen, Germany). Furthermore, the jugular vein was cannulated with a 7 Fr Swan-Ganz thermodilution catheter (Edwards Life Sciences, Unterschleissheim, Germany).
Experimental protocol
Pigs (n = 22) underwent bilateral carotid artery monitoring for emboli detection during 120 minutes CPB before being sacrificed for histological evaluation of the brain.
Bilateral, eEpicarotid Doppler recordings for emboli detection
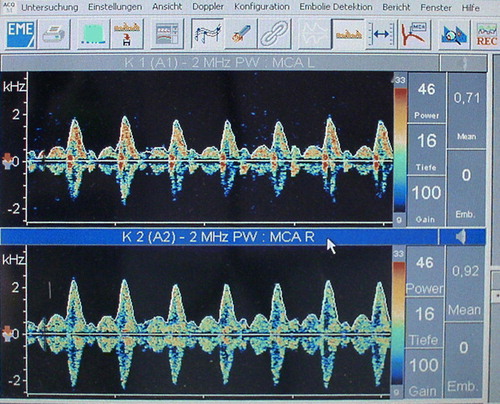
Epicarotid Doppler probes (2 MHz) (Nicolet Companion III, WIN TCD transcranial Doppler, EME-Nicolet GmbH, Langenfeld, Germany) were surgically placed bilaterally for continuous recording of high-intensity transient signals (HITS) from 15 minutes before to 15 minutes after CPB. Suture fixation kept the probes to the carotid artery at the angle giving the strongest Doppler signal (). To optimize the filter setting in respect to artefact-elimination we tapped against the probe, the cardiopulmonary bypass (CPB) cannula and the sternal retractor. For automatic on-line emboli recording power was set to 46, depth to 16 mm and gain to 100. Subsequently, recordings with artefacts were excluded. Thereafter, the recorded carotid flow-signal quality was visually scored (1 (poor quality) to 10 (excellent quality)). Only recordings scoring 5 or higher were accepted for manual off-line analysis of emboli counts by a blinded investigator (G.G.). Any short-lived, high-intensity (e.g. signal intensity above 7 dB) signals (e.g. click, chirp, whistle, bloop) in the Doppler flow spectrum occurring randomly during the cardiac cycle indicated an embolus Citation9–12.
Surgical preparation and Cardiopulmonary Bypass (CPB)
Surgical preparation for CPB was performed as described: Briefly, the heart and ascending aorta were exposed through a median sternotomy, with the pig in supine position. The thymus was removed and the pericardium opened. Purse string sutures were placed in the right atrium and the ascending aorta. Following heparinization and ACT measurement the ascending aorta (Medtronic® 22 Fr cannula, Medtronic Inc., Minneapolis, U.S.A.) and the right atrium (DLP® right-angled 34 Fr cannula, Stöckert Instrumente GmbH, Munich, Germany) were cannulated and CPB was started. During CPB flow was approximately 100 mL/kg/min. Saline (0.9%, 900 mL) was used for priming, and any fluid loss during CPB was substituted with lactated Ringer's solution. Acid-base management was adjusted to the alpha-stat regime Citation13. After a total CPB time of 120 minutes mechanical ventilation was resumed, the heart was defibrillated if needed and CPB was terminated. As soon as hemodynamics had stabilized, the aortic and the right atrial cannulae were removed and protamine sulfate (1:1) was administered to antagonize heparin. Approximately 60 minutes later, the pigs were sacrificed for histological evaluation by intravenous injection of potassium chloride (60 mM) and the brain was removed.
Histological evaluation
Brain tissue was fixed in formalin (4%). Following state-of-the-art pathological practice for cross-examination of the brain to detect emboli and infarct area the brain was cut in 2-mm slices. Furthermore, representative samples were taken from bilateral frontal, parietal, occipital and cerebellar regions. Slices were embedded in paraffin following routine histological techniques. Sections (1 µm) were stained with hemotoxylin-eosin.
Statistical analysis
Descriptive statistics were used for data analysis. Data are presented as mean (± SD) and range. Moreover, Spearman's rho between automatically and manually detected embolic counts was calculated. A p ≤ 0.05 was considered statistically significant. The statistical computer package SPSS ® 11.0.0 for Windows XP Professional (Chicago, IL, USA) was used for statistical analysis.
Results
All pigs (n = 22) completed the study without complication. A total of 42 recordings (right carotid artery (n = 20), left carotid artery (n = 22)) were evaluated. Frequency of counts was comparable in both carotid arteries. Automatic emboli detection, however, found significantly more embolic events per pig than did post-hoc manual off-line analysis of the recordings (172±217 vs. 13±10) (). A significant correlation between automatic and manual emboli detection was found only for the left carotid artery ().
Table I. A summary of the number of left (left carotid artery), right (right carotid artery) and total (total) carotid artery emboli counts continuously recorded from 15 minutes before to 15 minutes after 120 min cardiopulmonary bypass (CPB) in pigs (n = 22).
None of the brains showed any emboli or infarction area either in cross-examination or in histological evaluation.[JC1]
Discussion
Bilateral epicarotid Doppler recordings were successfully used for on-line emboli detection in a porcine CPB model. Frequency of embolic events was comparable in both carotid arteries. On-line automatic emboli detection, however, registered approx. ten times more embolic events than did post-hoc, manual off-line analysis.
Since cerebral emboli detection by human experts was previously shown to correlate well with that by specific algorithms Citation14, the present study's discrepancy between the number of emboli detected by automatic or manual analysis of the Doppler signal deserves further attention. To a certainly not irrelevant degree this discrepancy can be explained by the fragility of the epicarotid probe fixation and the sensitivity of the automatic detection algorithm to slightest motion artefacts caused, for example, by pulsation of the extracorporeal perfusion device. The Nicolet Doppler device can differentiate between artefacts and real emboli although it lacks multigating, which would allow echoes to be traced at various depths along the ultrasound beam, thus improving embolus but also artefact recognition Citation15. Furthermore, the algorithm of the present study's Doppler device (Nicolet Companion III, WIN TCD transcranial Doppler, EME-Nicolet GmbH, Langenfeld, Germany) is clearly optimized for transcranial surveillance of the arteria cerebri media, so that epicarotid application may contribute to the found discrepancy.
Although for reasons of anatomy one might expect more counts in the right carotid artery, the present study's emboli count for both carotid arteries was comparable (). This finding is in accordance with Sungurtekin et al. who could not show a side preference for microshperes injected in an animal embolization CBP model Citation16. Similarly, cardiosurgical patients showed no side preference for intraoperative emboli Citation17, Citation18. Comparing, however, a conventional ascending aortic cannulation site with a less commonly used but also less emboligenic descending aortic cannulation site yielded a higher rate of left hemispheric emboli Citation19. In contrast, postoperative CT scans in cardiosurgical patients showed a predominance of right hemispheric lesions Citation20. Since it can well be assumed that solid emboli with possibly noxious biological effects are directed towards the brachiocephalic trunk because of their greater mass, as compared to gaseous emboli, the conflicting results concerning a possible side preference of emboli are most likely caused by the nature of the embolus and the CPB flow rate.
In respect to its nature an embolus can basically be either solid or gaseous, which however cannot be discriminated by the used Doppler device (Nicolet Companion III, WIN TCD transcranial Doppler, EME-Nicolet GmbH, Langenfeld, Germany). By contrast, multifrequency Doppler devices (EMBO-DOP®) were initially shown to reliably discriminate solid and gaseous emboli Citation21. Although the multifrequency approach in contrast to the present study's intensity threshold approach gives improved discrimination of solid and gaseous emboli, a more recent study reported the method's positive predictive value to be only 0.5 Citation22. Refinements of software settings applied for reevaluation of the data by the same authors yielded an increased sensitivity (74.2%) for solid emboli Citation23, Citation24. This, however, at the cost of a moderate loss of specifity (85.4%) and exclusion of approximately a third of solid emboli Citation25. Accordingly, Schoenburg-M et al. reported a false negative value of 40.4% for the emboli detection by the EMBO-DOP® equipment Citation26. Since unambiguous identification of microembolic signals and sufficient artifact rejection are basic requirements before a differentiation between solid and gaseous particle can be performed these findings have put the clinical usefulness of the EMBO-DOP® equipment somewhat into question.
However, not finding solid thrombi or even an infarcted area in the histological evaluation of brain sections indicates two things. Firstly, the present study's detected emboli were most likely exclusively gaseous. Secondly, since infarcted areas were not found in any of the brain sections it can be assumed that for the present porcine CPB model there is only a very weak correlation between the quantity of detected emboli and damage to the brain. This finding stands in contrast to that of other authors who in cardiosurgical patients reported a positive correlation between the number of intraoperative microembolic signals (MES) and postoperative neurological deficits Citation27. A neurological deficit generally combines with histopathological findings, which can either be reversible or irreversible. The time required for development but also resolution of such histopathological changes is variable, but generally cannot fall below a tissue-specific minimum. Since the brain was removed at approx. one hour following the end of CPB, it is probable that the minimum time necessary for the development of histopathological changes had simply not yet elapsed. Aortic atherosclerotic lesions are known to be a good breeding ground for intraoperative cerebral embolism in patients undergoing CPB procedures. The fact that atherosclerotic lesions were absent in the present study's pigs confirms the above-postulated predominantly gaseous nature of the emboli. The assumption that gaseous emboli have less potential to cause brain damage than do solid emboli Citation28 would at any rate be in accordance with the absence of histopathological findings in the present study's pigs. Moreover, a surprising tolerance of the brain for microembolization in the acute setting, which was previously reported by Rapp et al. Citation29, could further explain the lack of histopathological changes despite numerous recorded embolic events in our porcine CPB model.
In conclusion, the present study showed the feasibility of using an epicarotid Doppler device for bilateral emboli detection in a porcine CPB model. A side preference for emboli occurrence was not found. Automatic on-line emboli detection, however, reported an approx. 10 times higher number of embolic events than did post hoc, off-line manual analysis.
Acknowledgements
The Doppler device was kindly supplied by VIASYS Healthcare, Langenfeld, Germany.
References
- Hogue CW, Jr, Sundt TM, 3rd, Goldberg M, et al. Neurological complications of cardiac surgery: The need for new paradigms in prevention and treatment. Semin Thorac Cardiovasc Surg. 1999; 11: 105–15
- Utley JR. Techniques for avoiding neurologic injury during adult cardiac surgery. J Cardiothorac Vasc Anesth. 1996; 10: 38–43; quiz 43–34
- Utley JR. Cardiopulmonary bypass surgery. Curr Opin Cardiol. 1992; 7: 267–75
- Menkis AH. Management of the ascending aorta in routine cardiac surgery. Semin Cardiothorac Vasc Anesth. 2004; 8: 19–24
- Bar-Yosef S, Anders M, Mackensen GB, et al. Aortic atheroma burden and cognitive dysfunction after coronary artery bypass graft surgery. Ann Thorac Surg. 2004; 78: 1556–62
- Fearn SJ, Pole R, Burgess M, et al. Cerebral embolisation during modern cardiopulmonary bypass. Eur J Cardiothorac Surg. 2001; 20: 1163–7
- Newell DW. Transcranial Doppler ultrasonography. Neurosurg Clin N Am. 1994; 5: 619–31
- Markus HS, Tegeler CH. Experimental aspects of high-intensity transient signals in the detection of emboli. J Clin Ultrasound. 1995; 23: 81–7
- Spencer MP, Thomas GI, Nicholls SC, Sauvage LR. Detection of middle cerebral artery emboli during carotid endarterectomy using transcranial Doppler ultrasonography. Stroke. 1990; 21: 415–23
- Spencer MP. Detection of cerebral artery emboli. Transcranial Doppler, DW Newell, R Aaslid. Ravan Press, New York 1992; 216–30
- Ringelstein EB, Droste DW, Babikian VL, et al. Consensus on microembolus detection by transcranial Doppler ultrasound. Stroke. 1998; 29: 725–9
- Consensus committee of the 9th International Cerebral Hemodynamics Symposium. Basic identification criteria of Doppler microembolic Signals. Stroke. 1995; 26: 1123
- Swan H. The importance of acid-base management for cardiac and cerebral preservation during open heart operations. Surg Gynecol Obstet. 1984; 158: 391–414
- Cullinane M, Reid G, Dittrich R, et al. Evaluation of new online automated embolic signal detection algorithm, including comparison with panel of international experts. Stroke. 2000; 31: 1335–41
- Georgiadis D, Goeke J, Hill M, Konig M, Nabavi DG, Stogbauer F, et al. A novel technique for identification of doppler microembolic signals based on the coincidence method: In vitro and in vivo evaluation. Stroke. 1996; 27: 683–6
- Sungurtekin H, Plochl W, Cook DJ. Relationship between cardiopulmonary bypass flow rate and cerebral embolization in dogs. Anesthesiology. 1999; 91: 1387–93
- Droste DW, Reisener M, Kemeny V, et al. Contrast transcranial Doppler ultrasound in the detection of right-to-left shunts. Reproducibility, comparison of 2 agents, and distribution of microemboli. Stroke. 1999; 30: 1014–8
- Kaps M, Hansen J, Weiher M, et al. Clinically silent microemboli in patients with artificial prosthetic aortic valves are predominantly gaseous and not solid. Stroke. 1997; 28: 322–5
- Mullges W, Franke D, Reents W, et al. Brain microembolic counts during extracorporeal circulation depend on aortic cannula position. Ultrasound Med Biol. 2001; 27: 933–6
- Hedberg M, Boivie P, Edstrom C, et al. Cerebrovascular accidents after cardiac surgery: An analysis of CT scans in relation to clinical symptoms. Scand Cardiovasc J. 2005; 39: 299–305
- Russell D, Brucher R. Online automatic discrimination between solid and gaseous cerebral microemboli with the first multifrequency transcranial Doppler. Stroke. 2002; 33: 1975–80
- Markus HS, Punter M. Can transcranial Doppler discriminate between solid and gaseous microemboli? Assessment of a dual-frequency transducer system. Stroke. 2005; 36: 1731–4
- Russell D, Brucher R. Embolus detection and differentiation using multifrequency transcranial Doppler. Stroke. 2005; 36: 706
- Russell D, Brucher R. Embolus detection and differentiation using multifrequency transcranial Doppler. Stroke. 2006; 37: 340–1
- Markus HS. Embolus detection and differentiation using multifrequency transcranial Doppler. Stroke. 2006; 37: 340–1, author reply 341–2
- Schoenburg M. Embolus detection and differentiation using multifrequency transcranial Doppler. Stroke. 2006; 37: 340–1, author reply 341–2
- Braekken SK, Reinvang I, Russell D, et al. Association between intraoperative cerebral microembolic signals and postoperative neuropsychological deficit: Comparison between patients with cardiac valve replacement and patients with coronary artery bypass grafting. J Neurol Neurosurg Psychiatry. 1998; 65: 573–6
- Balacumaraswami L, Abu-Omar Y, Anastasiadis K, et al. Does off-pump total arterial grafting increase the incidence of intraoperative graft failure?. J Thorac Cardiovasc Surg. 2004; 128: 238–44
- Rapp JH, Pan XM, Sharp FR, et al. Atheroemboli to the brain: Size threshold for causing acute neuronal cell death. J Vasc Surg. 2000; 32: 68–76