Abstract
Objectives. To test if cardiac computed tomography angiography (CCTA) can be used in the triage of patients at high risk of coronary artery disease. Design. The diagnostic value of 64-detector CCTA was evaluated in 400 patients presenting with non-ST segment elevation myocardial infarction using invasive coronary angiography (ICA) as the reference method. The relation between the severity of disease by CCTA and a combined endpoint of death, re-hospitalization due to new myocardial infarction, or symptom-driven coronary revascularization was assessed. Results. CCTA detects significant (>50%) coronary artery diameter stenosis with a sensitivity, specificity, and positive and negative predictive value of 99%, 81%, 96% and 95%, respectively. CCTA was used to triage patients into guideline defined treatment groups of “no or medical treatment”, “referral to percutaneous coronary intervention” or to “coronary artery bypass graft surgery” and was compared to the index ICA. CCTA correctly triaged patients in 86% of cases. During a median follow-up of 50 months, the presence of an occluded artery by CCTA was associated with adverse outcome. Conclusion. CCTA has high diagnostic and prognostic value in patients with high likelihood of coronary artery disease and could, in theory, be used to triage high risk patients. As many obstacles remain, including logistical and safety issues, our study does not support the use of CCTA as an additional diagnostic test before ICA in an all-comer NSTEMI population.
Introduction
Coronary computed tomography angiography (CCTA) has a high diagnostic accuracy for the detection of obstructive coronary artery disease and has become widely used as a screening tool in patients with non-acute chest pain and low to intermediate likelihood of significant coronary artery disease.[Citation1,Citation2] In these patients, several studies have also demonstrated a high prognostic value of CCTA.[Citation3,Citation4] Recent studies suggest that CCTA may also be useful in patients with acute-onset chest pain and possible acute coronary syndrome (ACS),[Citation5,Citation6] and a recent guideline also suggests the use of CCTA in patients presenting with elevated but inconclusive troponin levels.[Citation7] An expansion of the clinical use of CCTA to include patients with suspected ACS and possible myocardial infarction warrants studies that test the diagnostic accuracy of the method in this clinical setting.
Approximately 60% of patients presenting with ACS are treated with percutaneous coronary intervention (PCI) and the remainder with medication alone or coronary artery bypass graft (CABG) surgery.[Citation8] It is therefore relevant to explore if it is possible to use the widespread CCTA technique in the triage of high risk patients. Finally, CCTA may provide additional information regarding risk stratification.
We tested the applicability of the CCTA technique in a population of high risk patients with confirmed non-ST segment elevation myocardial infarction (NSTEMI) by (1) testing the hypothesis that the diagnostic accuracy of CCTA – especially the high negative predictive values – is preserved in patients with high likelihood of significant coronary artery disease as this is important in order (2) to test if CCTA can be used to stratify high risk patients according to treatment strategy and prognosis.
Material and methods
Study design
Consecutive patients admitted with NSTEMI to the Department of Cardiology, Rigshospitalet, Copenhagen, from December 2006 to January 2009 were screened for participation in the study and examined with CCTA prior to invasive coronary angiography (ICA) in an observational research design to assess the diagnostic accuracy and prognostic value of the method. The CCTA was evaluated on a per coronary segment level and on a per coronary vascular territory level. These datasets were constructed to create the per patient dataset. The coronary segment and vessel analysis were used to test the accuracy of CCTA to categorize patients in the guideline defined anatomical treatment strategy groups as the primary analysis of the paper. Furthermore, the severity of the highest degree diameter stenosis of each patient was used to assess the prognostic value of CCTA.
NSTEMI was defined as symptoms with acute chest pain and/or ECG changes without persistent ST-segment elevation and a characteristic rise and fall in plasma troponin-T in accordance with the European guidelines.[Citation9] Patients with the following contraindications to CCTA were not included: known chronic renal disease or plasma-creatinine >125 μmol/l, cardiac arrhythmias or known allergy to iodine contrast. Furthermore, patients with hemodynamic instability were not enrolled in the study and only patients who provided informed consent were included in the study. Moreover, CCTA was not performed if it was deemed to cause a delay in time-to-ICA. The protocol was approved by the Committees of Biomedical Research for the Capital Region of Denmark (protocol number: KF01318727) and written informed consent was obtained from all patients.
ICA was performed in all patients within two weeks of the clinical NSTEMI diagnosis according to Danish practice during the period of study.[Citation10] Treatment strategy was decided by the interventional cardiologist who was blinded to CCTA findings.
In a random subset of patients (N = 132, 34%), serum creatinine was measured within 96 hours after CCTA and ICA to observe the frequency of contrast induced nephropathy defined as a 25% rise in serum creatinine or a total increase of >44μmol/l. These patients who underwent testing for contrast induced nephropathy were, however, skewed towards those with higher age, higher se-creatinine, lower LVEF as well as higher frequency of 3 vessel disease in comparison to those who were not tested. Long-term clinical outcome was recorded for a minimum of 2 years in all patients. The study endpoint was a composite of death from any cause, non-fatal myocardial infarction and symptom-driven revascularization. Information of the occurrence of an endpoint was obtained from the validated databases in Denmark (Green System, CSC Scandihealth) and the Faroe Islands (COSMIC registry). Non-fatal myocardial infarction was defined as a characteristic rise and fall in cardiac biomarkers.[Citation11] Symptom driven revascularization was defined as invasive treatment due to symptoms of angina pectoris.
Invasive coronary angiography image analysis
ICA was performed according to standard clinical techniques. An expert observer – blinded to the clinical interpretation of the invasive angiograms, clinical presentation and to CCTA findings – analysed the invasive angiograms. All clinically relevant coronary segments were assessed for the presence of an eyeball luminal diameter stenosis of 50–74%, 75–99% and 100%. A 17 segment model of the coronary anatomy described by the Society of cardiovascular computed tomography was used for both ICA and CCTA to make the comparison between modalities easier.[Citation12] Obstructive disease was defined as >50% luminal stenosis. Vessels <2 mm in diameter were considered not clinically relevant and were not evaluated. In addition, coronary segments distal to an occluded coronary artery were not evaluated.
The ICA reading was used to place patients into 3 treatment strategy groups according to guideline defined anatomical criteria, not including any clinical data:[Citation7,Citation13]: (1) Patients with no obstructive disease – likely candidates for no or medical treatment, (2) patients with simple vessel disease: defined as one vessel disease or two vessel disease without involvement of the proximal left anterior descending artery (LAD) territory – likely candidates for percutaneous coronary intervention (PCI) and (3) patients with complex vessel disease: defined as 2-vessel disease which include the proximal LAD and patients with 3 vessel or left main disease – likely candidates for CABG. CCTA findings were subsequently tested against these ICA anatomy defined criteria to categorize the treatment strategy.
CCTA imaging
Patients were scanned with a 64-slice CT-scanner (Toshiba Aquillion, Toshigi, Japan) using a retrospective scanning technique. All patients received beta-blockade unless contraindicated, however no additional beta-blockade was given prior to scanning. The scanner settings were: tube voltage: 120–135 kV, detector collimation: 64 × 0.5 mm and rotation time: 350–500 ms. Depending on expected scan time, 70–100 ml intravenous contrast media Visipaque 320 mgI/ml (GE Healthcare, UK) was infused with a flow rate of 5 ml/s. Image acquisition was initiated by automatic bolus triggering. An automatic raw data motion analysis tool (PhaseXact, Toshiba Medical Systems Corp., Otawara, Japan) was used to determine the optimal motion free phase for reconstruction in addition to reconstructions in mid-diastole (70%, 75% and 80% of the R–R interval). Images were reconstructed with 0.5-mm slice thickness. Image data were transferred to an external workstation (Vitrea, Vital Images, Minnetonka, MN) for analysis.
CCTA image analysis
The CCTA analysis was performed by two experienced observers blinded to ICA findings and treatment strategy. In cases of disagreement between observers, the worst call of coronary stenosis and level of interpretability were used. Coronary segments with stents and calcification were carefully examined for blooming artefacts and all coronary segments were analysed according to current guidelines.[Citation12] Each coronary segment was determined as interpretable or non-interpretable. If two or more coronary segments, assigned to more than one coronary vascular territory, were non-interpretable, the study was regarded as non-evaluable and was excluded from further analysis. Each coronary segment was evaluated for the presence of luminal stenosis according to guidelines.[Citation12] Segments with ≥50% luminal diameter narrowing was considered as obstructive. If a segment was deemed non-interpretable, an intention to diagnose strategy was applied, i.e. the segment was considered as having a ≥50% stenosis. Per vessel analysis was performed in a similar fashion: if a segment was non-interpretable, an intention to diagnose strategy was applied for the target vascular territory. The same strategy was applied in a per patient analysis. In patients with previous CABG, diagnostic accuracy was assessed in the native vessels only. On a per patient analysis, we tested the diagnostic accuracy of CCTA to categorize the treatment strategy according to guideline defined anatomical criteria, as described above.[Citation13]
For risk assessment, patients were grouped according to the coronary artery lesion with the highest degree of severity: Normal (absence of plaque), non-obstructive plaque (diameter stenosis 1–49%), obstructive plaque (diameter stenosis 50–99%) and occluded vessels (diameter stenosis 100%). For risk assessment analysis, non-evaluable coronary segments were regarded as having an occluded coronary vessel.
Statistical analyses
Normally distributed continuous variables were presented as mean ± SD and not normally distributed continuous data were presented as median and interquartile range. Categorical variables were presented as frequencies and percentages.
For statistical comparisons, a two-tailed t-test for independent samples was used for continuous values, and the chi-square test for categorical variables. Continuous variables that were not normally distributed were compared with the Wilcoxon signed-rank test.
The diagnostic value of CCTA to detect a ≥50% coronary artery diameter stenosis was assessed on a segmental, vascular territory and patient level and presented as sensitivity, specificity, negative predictive value and positive predictive value.
The Kaplan–Meier method was used to assess the relation between clinical outcome and categorization according to the diameter stenosis with highest degree of severity assessed by CCTA. The relationship between the CCTA findings, clinical variables, and clinical outcome was assessed using Cox proportional hazards regression. Multivariable regression analysis with forced entry of categorization according to the diameter stenosis with the highest degree of severity was performed with adjustment for established clinical predictors: age, diabetes, previous myocardial infarction, left ventricular ejection fraction, Killip class and actual treatment strategy (no/medical, PCI or CABG). The presence of an occluded vessel was tested for interaction with age and treatment strategy. The proportional hazard assumption was checked through the method of cumulative residuals. Statistical analysis was performed using SAS version 9.2 (SAS Institute, Cary, NC). A p-value < 0.05 was considered statistically significant.
Results
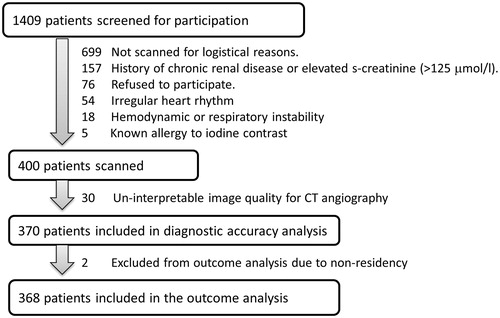
Out of 1409 patients screened for participation, 400 entered the study (). A total of 699 patients could not enter for logistic reasons, mainly because patients were transported from referring hospitals to Rigshospitalet on the evening before the invasive procedure and scheduled for ICA early the next morning before a CCTA examination could be performed. A total of 234 (17%) did not enter the study due to contraindications to CCTA. Thirty (7.5%) CCTA examinations were deemed non-evaluable for clinical CCTA. The mean heart rate during CCTA and the median Agatston score of these patients were significantly higher than in patients with evaluable CCTA (p < 0.001). Demographics of included patients are given in . In two patients, clinical follow-up was not possible because of foreign residence.
Table 1. Demographics, invasive findings and treatment.
Contrast induced nephropathy was found in 5% and all increased levels of se-creatinin returned to normal spontaneously without any clinical manifestation. There were no reports of serious adverse reactions to contrast. Patients received a mean radiation dose of 19 ± 4 mSv.
ICA findings
On a segmental level and on a vascular territory level, 16% (773/4764) and 50% (549/1106) of the evaluated coronary arteries had a ≥50% diameter stenosis according to the ICA, respectively. The ICA diagnosis on a per-patient level is specified in . Among patients with obstructive coronary artery disease, 47% (141/302) had at least one 75–99% coronary stenosis and 40% (122/302) had at least one occluded coronary vessel.
CCTA findings
A total of 7.5% (30/400) of the patients scanned in the study presented with a non-evaluable CCTA and were thus excluded from further analysis. A total of 51 patients out of the included 370 (14%) patients had at least one non-evaluable coronary segment (in one vascular territory: LAD: 12, Cx: 10 RCA: 29). These patients had higher mean heart rate (67 ± 20 bpm vs. 58 ± 10 bpm, p < 0.001) and higher median Agatston score (1058 vs. 268, p < 0.001) compared to patients without non-evaluable segments.
A total of 3.6% (171/4764) of the coronary segments evaluated by ICA were found to be non-evaluable by CCTA analysis due to motion artefacts or the combination of calcium/stent blooming and motion (N = 122), segments with low luminal contrast (N = 41), coronary vessel outside the scan field (N = 6) or artefacts from pacemaker electrode (N = 1).
By categorization of patients according to the highest degree of diameter stenosis, we found 23 (6%) patients without any coronary plaque, 35 (9%) had a 1–49% diameter stenosis, 166 (45%) had a 50% to 99% diameter stenosis, and 146 (40%) had at least one totally occluded vessel.
Diagnostic accuracy of CCTA
The diagnostic accuracy of CCTA to detect coronary artery stenosis on a per segment and per coronary vascular territory is given in . A total of 58 patients were free of significant stenosis on CCTA. Three of these were, however, found to have significant 1 vessel disease on ICA (one in each coronary branch). CCTA correctly identified 110 of 122 totally occluded vessels.
Table 2. Diagnostic accuracy of CCTA for the detection of >50% stenosis by ICA.
The diagnostic accuracy of CCTA for categorizing patients to a treatment strategy group as defined by ICA is given in and . Overall, CCTA categorized patients to the appropriate treatment strategy in 86% of cases. By CCTA, 13% of the participants were placed in a more invasive treatment strategy group (PCI/CABG) than ICA proposed (no or medical/PCI). A total of 13 (19%) patients without disease defined by ICA were placed in the simple disease group by CCTA. These patients had a higher mean heart rate (71 ± 37 vs. 59 ± 11, p < 0.001). A total of 35 (18%) patients with simple disease defined by ICA were placed in the complex disease group by CCTA. These patients had a higher median Agatston score (602 vs. 274, p < 0.02).
Figure 2. Diagnostic performance of coronary cardiac computed tomography (CCTA) for placing patients in anatomical guideline defined treatment groups as determined by invasive coronary angiography (ICA). White: candidates for no or medical treatment, Grey: candidates for percutaneous coronary intervention (PCI) and Black: candidates for coronary artery bypass grafting (CABG).
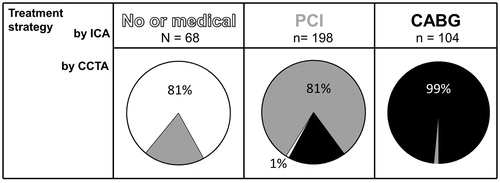
Table 3. Diagnostic accuracy of CCTA for placing patients in treatment groups.
Out of 370 patients, 55 were correctly identified as without significant coronary artery disease by CCTA, thus for every 7 scans, one ICA could be avoided. In contrast 3 patients were wrongfully deemed without significant stenosis on CCTA, thus for every 123 CCTA scans one would wrongfully deny and ICA.
The median time between CCTA and ICA was 4.4 h [interquartile range 2.4 h; 18.5 h]. When patients were divided by median time between CCTA and ICA, no differences in the number of patients that were misplaced in treatment strategy groups by CCTA were found (17% vs. 12%, p = 0.13).
Outcome
The median follow-up time was 50 months (range 27–65). All included patients survived to discharge. During follow-up, 85 (23%) patients reached the composite end-point: 48 (13%) died as their first event, 20 (5%) patients were re-admitted to hospital due to myocardial infarction and 17 (5%) had a symptom-driven revascularization procedure. Patients reaching a study end-point were characterized by higher age (p =0.02), higher prevalence of previous myocardial infarction (p = 0.001), higher Killip class at index myocardial infarction (p = 0.03) and a lower left ventricular ejection fraction (p <0.01).
Events according to patient groups categorized by the highest degree of diameter stenosis on CCTA are presented in . There were no events in the 23 patients without plaque or luminal narrowing. Interestingly, we found no difference in outcome between patients with the worst stenosis of 1–49% compared to 50–99% (log rank between these two groups p = 0.84). Similar findings were found when ICA evaluation was used (log rank p = 0.67).
Figure 3. Kaplan–Meier Plot presenting outcome according to highest degree of coronary diameter stenosis assessed by coronary computed tomography angiography.
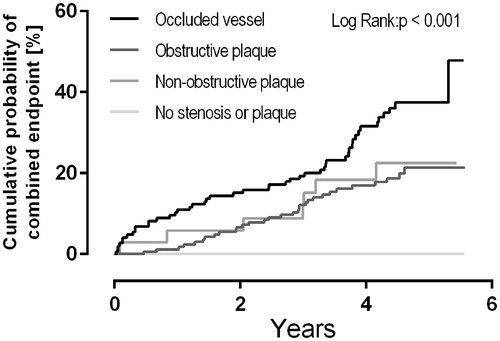
When adjusted for known risk factors and type of post-NSTEMI treatment, the presence of a totally occluded vessel was independently associated with the combined endpoint with an increased hazard ratio of 1.8 (confidence interval 1.1–2.9, p = 0.02). In a subgroup analysis excluding 19 patients with previous CABG, the hazard ratio remained unchanged (hazard ratio: 1.7 (1.03–2.8)).
Discussion
In this study, we demonstrate that the diagnostic accuracy of CCTA to identify and especially to exclude significant coronary artery disease in patients with chest pain and high likelihood of significant CAD (troponin release) is preserved with sensitivity, specificity, positive and negative predictive value of 99%, 81%, 96% and 95%. We found that CCTA could be used to categorize patients into the appropriate treatment strategy in 86% of all cases and, at the same time, improve risk stratification.
Despite our promising findings regarding the diagnostic and prognostic potential of CCTA, it must remembered that the clinical applicability of CCTA in NSTEMI patients could expose many of these patients to unnecessary risk, including radiation and contrast as well as possibly (in a different setting than ours) delay of ICA. Thus, the present study also highlights a number of limitations regarding the use of CCTA in NSTEMI patients that challenge the feasibility of this approach.
Diagnostic accuracy
We found a diagnostic accuracy of CCTA comparable to that of studies in patients with a lower prevalence of disease.[Citation1] A higher number of false negative test results could have been expected in our study due to higher prevalence of disease.[Citation14]. Our findings may partly be explained by the severity of the worst lesion in our population – 87% of the diseased patients had occlusion or severe luminal stenosis (≥75%) as determined by ICA. A priori high-grade stenosis is more likely to be judged to ≥50% on CCTA, compared to borderline narrowing. In part, our results could also be due to the conservative approach used as threshold for obstructive disease on CCTA (≥50% luminal stenosis, worst call of two readers).
A total of 51 (14%) of the patients had at least one non-evaluable segment (with a total of 171 non-evaluable segments). Using a conservative “intention to diagnose strategy” as done in the present study, this will cause false positive findings. This may in turn weaken the use of CT in the triage of patients.
Triage
We introduced the idea of using CCTA for non-invasive triaging of patients with high risk of significant CAD into guideline defined treatment groups. Our study suggests that it may be reasonable to avoid ICA in patients without obstructive disease on CCTA. Interestingly, we found that CCTA had a relatively high sensitivity to detect three-vessel, left main stem or two-vessel disease with proximal LAD involvement. The specificity was however somewhat lower with 35 false positives cases (with 2–3 times higher calcium score). Thus, the current technology should be improved before introducing it as a gatekeeper for CABG.
Further studies should explore the ability for CCTA to triage lower risk patients with possible ACS, preferably using additional pre-medication to lower heart rate and use second generation scanners with higher temporal resolution.[Citation15] These studies should further address the hemodynamic significance of a coronary artery stenosis by computed tomography derived fractional flow reserve or myocardial perfusion analysis. Both techniques have shown to correlate to the hemodynamic properties of coronary stenosis and could potentially improve the choice of treatment strategy.[Citation16–18]
Risk stratification
The group of patients with troponin release without any coronary plaque on CCTA that theoretically could be safely discharged after CCTA was fairly small (6%). The group of patients with non-obstructive plaque was too small to make any definite conclusions; however, they appeared to have the same risk of subsequent events as those with less than occlusive disease. This finding seems to be in contrast to previous studies of patients with suspected coronary artery disease, where patients with non-obstructive plaques had significantly better outcome than those with obstructive plaques.[Citation4] In our high risk population, we found 122 occluded vessels with absence of electrocardiogram determined ST segment elevation. CCTA correctly identified 110 of 122 totally occluded vessels and these patients had the worst prognosis in our study. Whether these patients might benefit from acute invasive treatment remains to be settled.
Patient safety
Patients received a radiation dose comparable to the dose range reported from contemporary CCTA studies performed at the time of study inclusion. This radiation dose is now considered unacceptably high as modern prospective scan techniques results in radiations exposures of 1–3 mSv.[Citation15,Citation19] It could be argued, however, that the radiation dose given in this study may be acceptable in patients with mean age 61, especially if CCTA-based triage results in fewer ICA. It appears likely that modern CCTA technology could provide a similar diagnostic yield, yet with a substantially lower radiation dose, however, this needs to be proven in further studies.
Compared to previous studies of PCI treated patients (without CCTA), we found a low incidence of contrast induced nephropathy.[Citation20] This concurs with previous studies demonstrating that predictors of this condition are known kidney disease, low estimated glomerular filtration rate and hypotension – factors that are not present in our patients scheduled for CCTA – rather than the amount of contrast used. Nevertheless, contrast induced nephropathy may be higher in some angiographic subsets, and it may have been beneficial to obtain a more detailed account rather than the random sample represented in this study.
Logistics and feasibility
The present study demonstrates that when using the logistical CCTA setup that was available at our hospital at the time of study, it was not possible to scan the majority of NSTEMI patients being admitted for ICA. Also, current guidelines recommend that ICA is performed within the first days after myocardial infarction. Therefore, in order to use CCTA in contemporary medical triage of NSTEMI patients, the CCTA has to be performed very early in the course.With a dedicated setup this may, however, be improved.[Citation5,Citation6] A recent study has shown that CCTA, applied early in the work-up of suspected ACS, is possible, safe and associated with less outpatient testing and lower costs compared to standard of care, but does not shorten hospital stay or allow for more direct discharge from the emergency department.[Citation21]
In patients who underwent CCTA, approximately 1 in 5 patients had either non-evaluable scans (7.5%), partly evaluable (4%) scans or incorrect triage result (14%). Under these settings, our study suggests that CCTA may only safely discharge a minority of patients. The results of this study do not support the use of CCTA as an additional diagnostic test before invasive coronary angiography in all-comer NSTEMI populations. It should, however, be appreciated that the target group for this study was patients suitable for CCTA and, therefore excludes patients with abnormal kidney function and hemodynamic instability.
Limitations
Although guidelines roughly outline treatment strategy according to diameter stenosis, many other factors are important in clinical decision-making. These include patient age, body mass index, comorbidity, risk factors, local expertise, cognitive function and compliance/preferences of the patient. Further studies should incorporate these factors in the assessment of the potential role for CCTA in the clinical management of patients with ACS. Moreover, treatment strategy is today most often guided by fractional flow reserve measurements and it is a limitation of the study that this was not assessed.
During ICA, the culprit lesion may often be characterized by special plaque features rather than diameter stenosis; these may include plaque instability, rupture or super-imposed thrombus. This information could be available from CCTA images; however, as NSTEMI patients have not been the clinical target group of CCTA, these signs have not yet been sufficiently elucidated to be implemented in the current investigation. Further studies should investigate the validity of such CCTA findings.
Logistical factors limited the enrolment of consecutive patients. Furthermore, only patients eligible for CT scanning were included in our study, rendering an inherent bias in patient selection highly possible. Accordingly, the fraction of patients with 3 vessels disease in our study group was lower than that of the screened patients.[Citation22] Finally, the results of our study must be interpreted in view of the rather limited size of patient number and events.
The CCTA readers were not blinded to each other’s readings and observer concordance was not assessed.
Conclusion
The high diagnostic accuracy of CCTA to rule out coronary artery disease is preserved in patients with high likelihood of CAD. This may facilitate the use of CCTA in the triage of high risk patients into anatomically defined treatment groups and can be used to place patients into risk groups. Our results show that obstacles remain, especially logistical and safety issues. Our study can, therefore, not support the use of CCTA as an additional diagnostic test before invasive coronary angiography in an all-comer NSTEMI population. Further studies needs to address these problems and should also include investigations of CT plaque characterization and CT derived flow reserve or perfusion in this patient group.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Abdulla J, Abildstrom SZ, Gotzsche O, et al. 64-multislice detector computed tomography coronary angiography as potential alternative to conventional coronary angiography: a systematic review and meta-analysis. Eur Heart J. 2007;28:3042–3050.
- Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the task force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34:2949–3003.
- Hulten EA, Carbonaro S, Petrillo SP, et al. Prognostic value of cardiac computed tomography angiography: a systematic review and meta-analysis. J Am Coll Cardiol. 2011;57:1237–1247.
- Min JK, Shaw LJ, Devereux RB, et al. Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality. J Am Coll Cardiol. 2007;50:1161–1170.
- Litt HI, Gatsonis C, Snyder B, et al. CT angiography for safe discharge of patients with possible acute coronary syndromes. N Engl J Med. 2012;366:1393–1403.
- Hoffmann U, Truong QA, Schoenfeld DA, et al. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med. 2012;367:299–308.
- Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35:2541–2519.
- Navarese EP, Gurbel PA, Andreotti F, et al. Optimal timing of coronary invasive strategy in non-ST-segment elevation acute coronary syndromes: a systematic review and meta-analysis. Ann Intern Med. 2013;158:261–270.
- Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the. European Society of Cardiology (ESC). Eur Heart J. 2016;37:267–315.
- Wallentin L, Lagerqvist B, Husted S, et al. Outcome at 1 year after an invasive compared with a non-invasive strategy in unstable coronary-artery disease: the FRISC II invasive randomised trial. FRISC II Investigators. Fast Revascularisation during Instability in Coronary artery disease. Lancet. 2000;356:9–16.
- Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J. 2012;33:2551–2567.
- Leipsic J, Abbara S, Achenbach S, et al. SCCT guidelines for the interpretation and reporting of coronary CT angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr. 2014;8:342–358.
- Wijns W, Kolh P, Danchin N, et al. Guidelines on myocardial revascularization. Eur Heart J. 2010;31:2501–2555.
- Meijboom WB, van Mieghem CA, Mollet NR, et al. 64-slice computed tomography coronary angiography in patients with high, intermediate, or low pretest probability of significant coronary artery disease. J Am Coll Cardiol. 2007;50:1469–1475.
- Dewey M, Zimmermann E, Deissenrieder F, et al. Noninvasive coronary angiography by 320-row computed tomography with lower radiation exposure and maintained diagnostic accuracy: comparison of results with cardiac catheterization in a head-to-head pilot investigation. Circulation. 2009;120:867–875.
- Norgaard BL, Leipsic J, Gaur S, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J Am Coll Cardiol. 2014;63:1145–1155.
- Kuhl JT, Linde JJ, Kober L, et al. The Transmural Extent and Severity of Myocardial Hypoperfusion Predicts Long-Term Outcome in NSTEMI: an MDCT Study. JACC Cardiovasc Imaging. 2015;8:684–694.
- Rochitte CE, George RT, Chen MY, et al. Computed tomography angiography and perfusion to assess coronary artery stenosis causing perfusion defects by single photon emission computed tomography: the CORE320 study. Eur Heart J. 2014;35:1120–1130.
- Einstein AJ, Moser KW, Thompson RC, et al. Radiation dose to patients from cardiac diagnostic imaging. Circulation. 2007;116:1290–1305.
- Mehran R, Aymong ED, Nikolsky E, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004;44:1393–1399.
- Dedic A, Lubbers MM, Schaap J, et al. Coronary CT angiography for suspected ACS in the era of high-sensitivity troponins: randomized multicenter study. J Am Coll Cardiol. 2016;67:16–26.
- Kuhl JT, Moller JE, Kristensen TS, et al. Left atrial function and mortality in patients with NSTEMI an MDCT study. JACC Cardiovasc Imaging. 2011;4:1080–1087.