Abstract
Objectives. The Nordic Consortium for Acute Type A Aortic Dissection (NORCAAD) is a collaborative effort of Nordic cardiac surgery centers to study acute type A aortic dissection (ATAAD). Here, we outline the overall objectives and the design of NORCAAD. Design. NORCAAD currently consists of eight centers in Denmark, Finland, Iceland and Sweden. Data was collected for patients undergoing surgery for ATAAD from 2005 to 2014. A total of 194 variables were retrospectively collected including demographics, past medical history, preoperative medications, symptoms at presentation, operative variables, complications, bleeding and blood transfusions, need for late reoperations, 30-day mortality and long-term survival. Results. Information was gathered in the database for 1159 patients, of which 67.6% were male. The mean age was 61.5 ± 12.1 years. The mean follow-up was 3.1 ± 2.9 years with a total of 3535 patient years. Conclusions. NORCAAD provides a foundation for close collaboration between cardiac surgery centers in the Nordic countries. Substudies in progress include: short-term outcomes, long-term survival, time interval from diagnosis until operation, effects of surgical techniques, malperfusion syndrome, renal failure, bleeding and neurological complications on outcomes and the rate of late reoperations.
Introduction
Acute type A aortic dissection involves the ascending aorta and to a varying degree the aortic arch and the descending aorta.[Citation1] It is a life threatening condition, associated with high morbidity and mortality. Death and complications occur due to free rupture of the aorta, pericardial tamponade, acute aortic insufficiency together with critical end-organ malperfusion.[Citation2]
According to the Centers for Disease Control and Prevention, diseases of the aorta and its branches account for 43,000 to 47,000 deaths annually in the United States.[Citation3] Though the precise number of these deaths attributable to thoracic aortic diseases is unclear, the number of patients presenting with ATAAD are estimated to increase, given the longer life expectancy and increased prevalence of risk factors such as high blood pressure.[Citation4] A nationwide population-based study from Sweden showed that the prevalence and the incidence for thoracic aneurysm or dissection increased by 52% in men and 28% in females from 1987 to 2002. During the same period of time, the number of operations for these diseases also increased, as did survival rates of patients undergoing associated surgery.[Citation5] However, it is not clear whether the true incidence of aortic dissection is rising, or if the increase is related to improved diagnostics, increased awareness and/or higher rates of operations for the condition. In Iceland the incidence of thoracic aortic dissections did not change significantly from 1992 to 2013, but an increase in the proportion of patients that underwent an operation for ATAAD was observed.[Citation1]
ATAAD requires immediate surgical intervention since the in-hospital mortality rate is unacceptably high without surgery.[Citation6] Operations for ATAAD are among the most complex surgeries performed and associated complications (e.g. excessive postoperative bleeding, stroke and neurological changes, renal failure, respiratory failure and multiorgan failure) occur at a higher frequency than for elective open-heart operations. ATAAD patients are critically ill and the treatment causes strain on intensive care units (ICU) and hospital resources. Contemporary data from the International Registry of Acute Aortic Dissection (IRAD) shows, however, that the overall hospital mortality has decreased from 31% to 22% from 1995 to 2013, and many other centers have described similar reduction.[Citation6–10]
The objective of this multicenter research project is to collect and combine the surgical outcome of ATAAD of several major cardiac surgery centers in the Nordic countries for the purpose of investigating specific areas of interest related to ATAAD.
Materials and methods
Centers
NORCAAD consists of eight cardiac surgery centers in Denmark, Finland, Iceland and Sweden. These include Aarhus University Hospital, Skejby, Denmark; Tampere University Hospital, Tampere, Finland; Turku University Hospital, Turku, Finland; Landspitali University Hospital, Reykjavik, Iceland; Karolinska University Hospital, Stockholm, Sweden; Örebro University Hospital, Örebro, Sweden; Sahlgrenska University Hospital, Gothenburg, Sweden; Skåne University Hospital, Lund, Sweden. The estimated population covered by participating centers is at least 9,500,000.
Data source
Data were collected independently by each participating center for all patients that underwent an operation for ATAAD from January 1, 2005 to December 31, 2014. ATAAD was defined as disruption of the media layer of the aorta with bleeding or hematoma formation within and along the wall of the ascending aorta resulting in separation of the aortic layers.[Citation3] The operation had to occur within 2 weeks of diagnosis or occurrence of symptoms. Patients that underwent repair of a chronic dissection were excluded. All potential patient identifiers were blinded and each center obtained approval from their corresponding bioethics and data protection committees or commissions. As individual patients were not identified, obtaining individual consent for the study was waived.
Variables
A total of 194 variables were collected () and an additional 53 variables were derived from the collected variables.
Table 1. Variables collected by participating NORCAAD centers.
Statistical methods
Data was collected in Microsoft Excel® (Seattle, WA) from each center and then combined into a single database. Additional statistical analysis was performed in R (R Foundation for Statistical Computing, Vienna, Austria, http://www.R-project.org/) and then made available to participating centers in R, SPSS and STATA format. Continuous variables were expressed as mean ± standard deviation (SD) and categorical variables as percentages. Odds ratio (OR) with 95% confidence interval (CI) were estimated with logistic regression. In NORCAAD substudies, specific statistical methods are applied to address risk factor analysis, short- and long-term survival and related issues.
Results
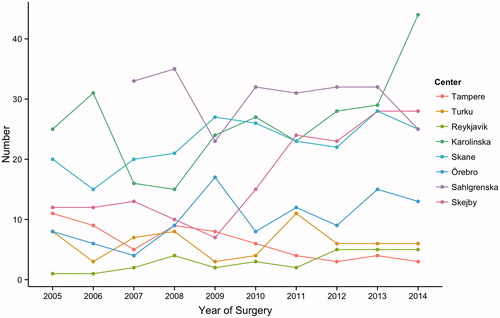
A total of 1159 operations were performed over the 10-year period at the participating institutions with a mean of 116 operations per year (SD 24.2, range 77–150). The total number of operations performed at each center during the study period ranged from 30 to 262 and were as follows: Tampere 62; Turku 62; Reykjavik 30; Karolinska 262; Skåne 227; Örebro 101; Sahlgrenska 243; Skejby 172. Combined number of operations performed at all centers per year increased from 85 in 2005 to 150 in 2014 (OR 1.130, 95%CI 1.103–1.157, p < .001) (). The mean age at time of surgery was 61.5 ± 12.1 years and 67.6% of patients were male. Basic demographics and past medical history including sex, age, hypertension, bicuspid aortic valve, history of stroke and chronic obstructive pulmonary disease (COPD) were similar between different centers. The mean follow-up time was 3.1 ± 2.9 years with a total of 3535 patient years.
Figure 1. Annual number of operations performed for acute type A aortic dissection at each participating center from 2005 to 2014. Data was not available for Sahlgrenska University Hospital for the years 2005–2006.
For the entire combined database of collected variables 20.9% ± 24.7% had missing values. For essential variables the rate of missing values was 8.8% ± 13.8% of which the following had >5% missing values: Time of admission, family history of dissection and aneurysm, smoking, height, weight, hypotension on admission, systolic blood pressure (SBP), diastolic blood pressure (DBP), malperfusion (cardiac, gastrointestinal, renal, extremities, cerebral, spinal), techniques used during hypothermic circulatory arrest (HCA), operative time, cardiopulmonary bypass time, cross-clamp time, HCA time, lowest temperature of HCA, redo sternotomy, acute kidney injury (AKI), bleeding, blood transfusion variable and laboratory tests. For the remaining variables only 1.4% ± 1.3% had missing values.
Discussion
With the launching of NORCAAD, we have now created the third largest database on ATAAD. There are currently two large clinical databases on aortic dissection. The largest is the IRAD, an international registry of 30 centers in 11 countries containing over 3800 cases of acute aortic dissection.[Citation6] The other is the German Registry for Acute Aortic Dissection Type A (GERAADA) that comprises 56 centers in Germany, Austria and Switzerland which started in 2006 and currently has over 3300 ATAAD cases.[Citation11] We are of the opinion that there is a need for a Nordic database on ATAAD and that by combining the results of several Nordic centers we would not only create a large database, but also foster collaboration between Nordic cardiothoracic surgeons. Additional rationales and potential strengths of NORCAAD include similar health care systems in the Nordic countries, homogeneous populations of which long-term follow-up is nearly complete through centralized national identity registry, rather equivalent training systems for cardiothoracic surgeons. In the Nordic countries there are several centers of excellence in cardiac surgery and academic institutions that would provide resources for the different research projects. The weakness of NORCAAD is that of large registry study, and is mostly related to incomplete datasets and the fact that its catchment area includes less than half of the population of all the Nordic countries. Future versions of NORCAAD will involve more centers and thereby increase the number of cases captured significantly.
Despite the large volume of data published on ATAAD, detailed evidence related to operative treatment is still lacking. Registry such as NORCAAD will continue to advance the literature and hopefully contribute to improvement in the management of ATAAD. Clinical decision-making in regards to surgical techniques, related to the proximal and distal extent of the aortic replacement are needed but also conceptual frameworks involving the complex management of patients presenting with severe symptoms of malperfusion; should root-sparing or valve-sparing techniques be used instead of composite root replacement; and should distal anastomosis be performed as open anastomosis using hypothermic arrest or is less extensive repair with aortic cross-clamp sufficient?[Citation12] What type of perfusion techniques should be used during HCA? More extensive operative techniques tend to be more complex and require more training and experience to be successfully performed. For various reasons (operator and team experience, urgency, local treatment traditions) conservative methods are sometimes favored over more extensive and complex approaches. The primary goal of operative treatment for ATAAD is survival of the patient, regardless of the operative technique used. Various aspects of intraoperative and postoperative care affect the high rates of postoperative complications that are observed following surgery for ATAAD. Operative techniques and ICU care has changed markedly over the last decade and contemporary information on temporal changes and actual rates of mortality and complications would aid physicians in the treatment of patients with ATAAD. To address these issues we have initiated several substudies of NORCAAD, led by different participating centers shown in . In some instances, these substudies will address the same issues that other large databases on ATAAD have addressed before, while other substudies will focus on previously less investigated fields. Each substudy is headed by a predefined participating center but will also involve active participation of surgeons, trainees and medial students from other centers to a varying degree. This will ensure active collaboration between participants of NORCAAD.
Table 2. Current NORCAAD research projects.
In the current edition, the cost of data collection is covered by each participating center and surgeons. The future objectives for NORCAAD are to develop a prospective online data collection with expanded collection of operative variables and to include other large Nordic cardiothoracic centers that have not been able to participate at this time. That will require more substantial funding and comes with its unique regulatory challenges to ensure patient confidentiality and data protection. Additional validity checking will also be required to ensure more uniform and complete data collection than the current NORCAAD provided.
In summary, ATAAD remains a highly complex disease, often difficult to diagnose and challenging to treat. Untreated it is highly lethal and even if expeditiously diagnosed and appropriately managed, both short- and long-term morbidity and mortality remain high mandating investigating ways to further improve its outcomes. There still remain numerous unanswered questions related to the management of ATAAD. The recently developed NORCAAD aims to provide contemporary information on the outcomes of the operative treatment of ATAAD with specific interest in the Nordic countries. It will hopefully enhance our knowledge of this complex disease in addition to foster collaboration and collegiality among Nordic cardiothoracic surgeons.
Acknowledgement
The following individuals also contributed to the study: Erik Björklund MD, Josefine Carrell RN, Erik Herou MD, Sigrun H. Lund PhD, Inga H. Melvinsdottir MD, Emily Pan BM and Johan Sjögren MD PhD.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Melvinsdottir IH, Lund SH, Agnarsson BA, et al. The incidence and mortality of acute thoracic aortic dissection: Results from a whole nation study. Eur J Cardiothorac Surg. 2016. [Epub ahead of print]. doi: 10.1093/ejcts/ezw235.
- Anagnopoulos C, Prabhakar M, Kittle C. Aortic dissections and dissecting aneurysms. Am J Cardiol. 1972;30:263–273.
- Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation. 2010;121:e266–e369.
- LeMarie S, Russell L. Epidemiology of thoracic aortic dissection. Nat Rev Cardiol. 2011;8:103–113.
- Olsson C, Thelin S, Stahle E, et al. Thoracic aortic aneurysm and dissection. Increasing prevalence and improved outcomes reported in a nationwide population-based study of more than 14000 cases from 1987-2002. Circulation. 2006;114:2611–2618.
- Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283:897–903.
- Rogers AM, Hermann LK, Booher AM, et al. Sensitivity of the aortic disseciton detection risk score, a novel guideline-based tool for identification of acute aortic dissection at initial presentation. Results from the international registry of acute aortic dissection. Circulation. 2011;123:2213–2218.
- Tsai T, Trimarchi S, Nienaber CA. Acute aortic dissection: perspective from the internationl registry of acute aortic dissection (IRAD). Eur J Vasc Endovasc Surg. 2009;37:149–159.
- Pape LA, Awais M, Woznicki EM, et al. Presentation, diagnosis, and outcomes of acute aortic dissection: 17-year trends from the international registry of acute aortic dissection. J Am Coll Cardiol. 2015;66:350–358.
- Conway BD, Stamou SC, Kouchoukos NT, et al. Improved clinical outcomes and survival following repair of acute type A aortic dissection in the current era. Interact CardioVasc Thorac Surg. 2014;19:971–977.
- Boening A, Karck M, Conzelmann LO, et al. German registry for acute aortic dissection type A: structure, results, and future perspectives. Thorac Cardiovasc Surg. 2016. [Epub ahead of print]. doi: 10.1055/s-0036-1572436.
- Geirsson A, Bavaria JE, Swarr D, et al. Fate of the residual distal and proximal aorta after acute type A dissection repair using a contemporary surgical reconstruction algorithm. Ann Thorac Surg. 2007;84:1955–1964.
- Erbel R, Aboyans V, Boileau C, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases. Eur Heart J. 2014;35:2873–2926.
- Augoustides JG, Geirsson A, Szeto WY, et al. Observational study of mortality risk stratification by ischemic presentation in patients with acute type A aortic dissection: the Penn classification. Nat Clin Pract Cardiovasc Med. 2009;6:1–7.
- Available from: http://www.sts.org/sts-national-database/database-managers/adult-cardiac-surgery-database/data-collection
- Bellomo R, Ronco C, Kellum JA, et al. Acute renal failure: definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204–R212.
