Abstract
Objectives. In a nationwide cohort, we analyzed long-term outcome following coronary artery bypass grafting, using the combined strategy of left internal mammary artery to the left anterior descending artery and saphenous vein as secondary graft to other coronary targets. Methods. 1,507 consecutive patients that underwent myocardial revascularization during 2001–2012 in Iceland. Mean follow-up was 6.8 years. Major adverse cardiac and cerebrovascular events were depicted using the Kaplan-Meier method. Cox-regression was used to define risk factors. Relative survival was estimated by comparing overall survival to the survival of Icelanders of the same age and gender. Results. Mean age was 66 years, 83% were males, mean EuroSCOREst was 4.5, and 23% of the procedures were performed off-pump. At 5 years, 19.7% had suffered a major adverse cardiac or cerebrovascular event, 4.5% a stroke, 2.2% myocardial infarction, and 6.2% needed repeat revascularization. Overall 5-year survival was 89.9%, with a relative survival of 0.990. Independent predictors of major adverse cardiac and cerebrovascular events were left ventricular ejection fraction ≤30%, a previous history of percutaneous coronary intervention, chronic obstructive lung disease, chronic kidney disease, diabetes, and old age. The same variables and an earlier year of operation were predictors of long-term mortality. Conclusions. The long-term outcome following myocardial revascularization, using the left internal mammary artery and the great saphenous vein as conduits, is favourable and improving. This is reflected by the 5-year survival of 89.9%, deviating minimally from the survival rate of the general Icelandic population, together with a freedom from major adverse cardiac and cerebrovascular events of 80.3%.
Introduction
Coronary artery bypass grafting (CABG) remains the most effective treatment for multivessel coronary artery disease and left main stem disease [Citation1,Citation2]. Since its introduction over five decades ago, improvements in perioperative care and surgical techniques, including the use of the left internal mammary artery (LIMA) and advances in cardioplegia techniques, have resulted in better early and long-term outcomes [Citation3,Citation4].
Traditionally, both arterial and venous conduits have been used for CABG [Citation4]. Numerous studies have supported the excellent long-term patency of LIMA to the left anterior descending coronary artery (LAD), which is the standard conduit for LAD disease [Citation5,Citation6]. In the last decade, there has been growing interest in the use of multiple arterial grafts, especially the right internal mammary artery (RIMA) and radial artery to replace saphenous vein grafts as secondary conduits to different coronary targets. The rationale is improved patency of arterial grafts as compared to venous conduits [Citation7,Citation8]. Some retrospective studies have shown improved long-term survival when using multiple arterial grafts [Citation9,Citation10]. However, the recently published randomized controlled Arterial Revascularization Trial (ART) showed no significant survival benefit of bilateral IMA (BIMA) grafts compared to single IMA grafts (SIMA) in a 5-year follow-up [Citation11]. With saphenous vein grafts being easily accessible, their use as secondary grafts is still the leading approach, both in the US and Europe [Citation3,Citation12,Citation13].
Short-term complications after CABG, such as new-onset atrial fibrillation, wound infections, and bleeding, together with 30-day mortality, have been thoroughly reported in the literature, including results from our group [Citation3,Citation14]. The long-term outcomes, however, are equally important when choosing a treatment modality. To date, studies on long-term outcomes after CABG have focused more on survival than on long-term adverse events. In addition, these studies have often been based on selected patient cohorts, while there are few data from whole populations [Citation15]. Furthermore, comparisons between CABG patients and the general population (relative survival) have seldom been reported.
The use of the LIMA for the LAD with a saphenous vein graft as a secondary conduit has been the standard technique for myocardial revascularization in Iceland for the past two decades. Centralized databases in Iceland provide an opportunity to collect nationwide data from a well-defined population receiving well-documented follow-up after CABG. Thus, the objective of this study was to determine the outcome of CABG surgeries in Iceland, where the LIMA was used for the LAD with a saphenous vein graft as a secondary conduit. We concentrated on long-term complications and survival, including relative survival, using the Icelandic population as a reference.
Materials and methods
Study design and study group
This was a retrospective nationwide study that included all patients who underwent first-time isolated CABG at Landspitali University Hospital in Reykjavik, Iceland, during the period 1 January 2001 to 31 December 2012. The hospital is the only centre performing cardiac surgery in Iceland. To maximize the homogeneity of the study group, we only included operations with the LIMA to the LAD and with saphenous vein grafts to the right and circumflex branches, and excluded operations where the RIMA or only venous grafts were used.
Data collection
Patients were identified by searching for digital operation codes in a computerized diagnostic and operation registry, in addition to reviewing a centralized cardiac surgery database for CABG operations in that period. Clinical information, including patient demographics, perioperative variables, and postoperative variables, was collected retrospectively from hospital charts at Landspitali. Information on PCI was collected from a centralized percutaneous coronary intervention (PCI) registry at Landspitali, the only hospital in Iceland performing PCI. To achieve complete long-term follow-up, medical records were reviewed from all hospitals in Iceland providing services for patients with cardiovascular diseases. Thus, seven hospitals covering all parts of Iceland provided data. Information on survival was collected from the centralized registry Statistics Iceland.
Patient preoperative demographics registered included age, gender, BMI, history of diabetes, hypertension, chronic obstructive pulmonary disease (COPD), smoking history, and history of previous myocardial infarction (MI), arrythmia, and/or PCI. Chronic kidney disease (CKD) was staged according to the Kidney Disease Outcome Quality Initiative (KDOQI) classification [Citation16]. Estimated glomerular filtration rate (eGFR) was calculated from serum creatinine mesurements using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [Citation17], and CKD was defined as eGFR ≤60 mL/min/1.73 m2 (stage 3–5). The Canadian Cardiovascular Society (CCS) Grading System score was used to grade angina, and standard EuroSCORE [Citation18] was calculated for all patients to estimate predictive operative mortality. Data on the severity of coronary artery disease (CAD) was collected from angiography reports, preoperative left ventricular ejection fraction (LVEF) from echocardiographic reports, and information on medical therapy â including statins, beta-blockers, and aspirin â from hospital records.
Operative variables included the use of cardiopulmonary bypass (CPB), total operative time, CPB and cross-clamp time, the number of distal anastomoses, chest-tube output during the first 24 postoperative hours, number of transfused units of packed red cells (PRCs), and whether the operation was emergent (within 24 hours of admission), semi-emergent (within the same admission period), or elective. Length of total hospital stay and time in the intensive care unit (ICU) were also registered.
Outcome parameters
Major adverse cardiac and cerebrovascular events (MACCE) were registered as long-term endpoints and included MI, stroke, need for PCI or repeated CABG, and death. Stroke was defined as neurological signs that persisted for more than 24 hours. Long-term MI was defined as the diagnosis of MI more than 30 days after surgery, excluding perioperative MIs. A diagnosis of MI was made if an elevation of cardiac biomarkers was seen in addition to one of the following: new significant ST segment changes, new left bundle branch block or development of Q-waves on electrocardiogram, symptoms of ischemia, diagnostic imaging showing new wall motion abnormalities, or identification of intracoronary thrombus. The estimate of stroke and MI incidence included patients who received those diagnoses and died during the follow-up period.
Follow-up
Follow-up was completed for all patients, and the end of follow-up was 1 July 2014. Mean length of follow-up was 6.8 years (range: 0–13.5 years).
Statistical methods
Descriptive statistics were calculated using Microsoft Excel, while further statistical analysis was performed using R version 3.2.3 (R Foundation for Statistical Computing, Vienna, Austria) using the survival, epitools, MASS, dplyr, tidyr, ggplot2, mice, and relsurv packages. Any P-values less than .05 were considered significant.
The Kaplan-Meier method was used to calculate the complication rate for each of the long-term endpoints: MI, stroke, PCI, repeat CABG, and death â and also the total rate of the composite endpoint, MACCE.
Cox regression analysis was used to identify preoperative risk factors for death and MACCE. A univariate Cox regression analysis was carried out for all preoperative variables. The significant variables, in addition to variables of clinical importance and/or previously known to be risk factors, were then included in multivariate Cox regression models, both for death and MACCE. A semi-automated stepwise backwards and forwards method was used to find the best model, for death and MACCE. The severity of coronary artery disease (one-, two-, or three-vessel disease) and EuroSCORE were adjusted by strata and included in both of the final models. All variables in the final models (see Results) met the requirements of proportional hazards [Citation19]. The area under the receiver operating characteristic (ROC) curve was calculated to show the predictive abilities of the final models. The unadjusted hazard ratios (HR) from the univariate analysis, the adjusted HRs from the final analysis, p-values, and confidence intervals are reported.
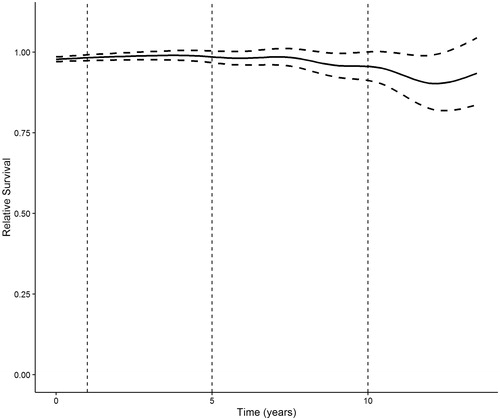
Relative survival of the population was estimated with relative survival ratios (RSR) [Citation20], comparing the ratio of the observed survival of the patient cohort with the estimated survival of an age- and gender-matched cohort from the same population.
The study was approved by the Icelandic National Bioethics Committee and the Data Protection Commission. As individual patients were not identified, the need to obtain individual consent was waived.
Results
Altogether, 1,622 patients underwent first-time isolated CABG at Landspitali during the 12-year study period, with the annual number of operations ranging from 110 in 2012 to 164 in 2008. Ninety-three operations (5.7%) were excluded where only venous grafts were used, and 22 cases (1.4%) were excluded where RIMA was used. This left 1,507 operations for further analysis, where the LIMA was used for the LAD with saphenous vein grafts for the right coronary artery and circumflex branches.
The patient demographics are shown in . The mean age was 65.9 years (range: 32–87), 82.5% were males, 16.4% had diabetes, 64.4% had hypertension, 7.1% had COPD, and 13.1% had a CKD KDOQI stage 3–5. More than two-thirds of the patients had a history of smoking, with 25.3% being current smokers. The mean BMI was 28.3 kg/m2 (range: 17–64), 25.2% had a history of a previous MI, and 20.8% had a history of PCI, with more than half of them having received a coronary stent. The mean preoperative LVEF was 55%, with 4.1% of the patients having an LVEF of ≤30%. The mean EuroSCORE was 4.5 and the mean CCS score was 3.2. Over 90% of the patients had a three-vessel CAD (83.0%) and/or left mainstem coronary stenosis (41.8%). Before surgery, 78.3% of patients had been taking aspirin, 77.5% had been taking lipid-lowering statins, and 70.3% were on beta-blockers.
Table 1. Preoperative patient demographics.
lists the operative and postoperative variables. Beating-heart (OPCAB) technique was used in 23.0% of the patients. Mean CPB time was 90 minutes and mean cross-clamp time 46 minutes. Around half of the operations were elective, 46.6% were performed as semi-emergent, and 3.8% were defined as emergent operations. The median number of distal anastomoses was 3 (mean 3.5). The median chest-tube output during the first 24 hours after surgery was 800 mL, and 63.0% of patients received transfusion with PRC, with a median of one unit. The median total hospital stay was 9 days (range: 0–96), 1 day of which was in the ICU (range: 0–35).
Table 2. Operative and postoperative variables.
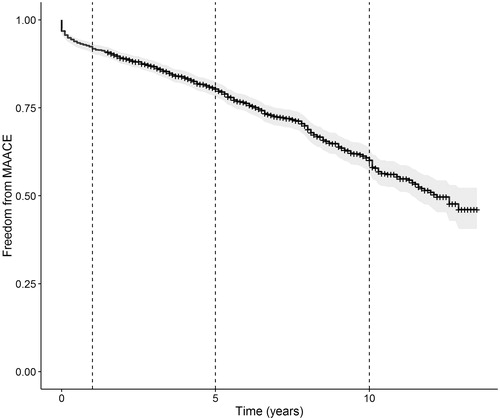
The rate of freedom from MACCE 1, 5, and 10 years from surgery is shown in . The total rate of freedom from MACCE was 91.8% at 1 year, 80.3% at 5 years, and 60.1% at 10 years. shows Kaplan-Meier estimated freedom from MACCE up to 10 years from surgery. The survival was 96.5% at 1 year, 89.9% at 5 years, and 75.0% at 10 years. One year from the operation 2.1% of the patients had suffered stroke, 5 years from the operation 4.5% had suffered stroke, and 7.5% had suffered stroke by 10 years. The rate of MI was 0.5% at 1 year, 2.2% at 5 years, and 7.5% at 10 years after the operation. The need for PCI increased with time from operation, the rate being 2.5% at 1 year, 5.9% at 5 years, and 12.7% at 10 years from surgery. Only three patients required re-CABG at 1 year (0.2%), and at 5 and 10 years the numbers were four patients (0.3%) and eight patients (0.9%), respectively.
Table 3. Freedom from MACCE, calculated with the kaplan-meier method, at 1, 5, and 10 years from the operation.
Independent predictors of MACCE and death are given in . LVEF ≤30%, a history of PCI before CABG surgery, a history of COPD, CKD, diabetes, and advanced age were significant risk factors for MACCE (). Independent risk factors for long-term mortality were the same, in addition to an earlier year of operation (). A previous history of coronary stent implantation was included in both of the models, but turned out not to be significant. In addition, BMI, gender, and the use of statins preoperatively were included in the final long-term mortality model, but they were not significant. The area under the ROC curve analysis to assess the abilities of the finalized Cox models to predict risk factors for MACCE and death revealed that these variables were able to correctly classify 65% and 68% of the patients into groups―with or without MACCE and alive or not alive, respectively.
Table 4a. Cox regression analysis predicting risk factors for MACCE, showing all variables included in the final model with the unadjusted and adjusted HRs, CI, and p-value.
Table 4b. Cox regression analysis predicting risk factors for death, showing all variables in the final model with the unadjusted and adjusted HRs, CI, and p-value.
shows the relative survival of the patients compared to the survival of the Icelandic population of the same age and gender, with the survival of the Icelandic population of the same age and gender being 1.0. The relative survival was 0.995 (95% confidence interval (CI): 0.992–0.999) at 1 year, 0.990 (95% CI: 0.984–0.995) at 5 years, and 0.984 (95% CI: 0.978–0.991) at 10 years after surgery.
Discussion
The main aim of this whole-nation study was to examine long-term survival and cardiovascular event rates in patients undergoing CABG, where the strategy of LIMA to LAD and the greater saphenous vein to other coronary targets was used. Our findings show 5-year survival of 89.9%, which is favourable, and a 5-year freedom-from-MACCE rate of 80.3%. Furthermore, the patients had comparable survival to that of the general population of Iceland, with overall relative survival rates of 0.990 and 0.984 at 5 and 10 years, respectively.
Contemporary studies of long-term survival following CABG with a single IMA graft have reported 5-year survival of 85–93% [Citation7,Citation10,Citation11,Citation21]. In both the SYNTAX trial [Citation1] and the FREEDOM trial (with only diabetic patients) [Citation2], a 5-year survival of 89% was reported, which is only slightly lower than the 89.9% found in the present study. Our 10-year survival is also in line with the literature ― being 75% as compared to 70%–79% in other studies [Citation7,Citation9,Citation10,Citation21].
Even more favourable long-term survival rates have been reported in some retrospective studies with the use of multiple arterial conduits, of around 94–96% at 5 years and 83–84% at 10 years [Citation7,Citation10,Citation22]. However, a shortcoming of most of these studies has been that selected patient cohorts were analyzed, and registration of long-term complications other than mortality was often lacking. Furthermore, the comorbidity profiles of patients often vary, setting the stage for selection bias: patients who receive multiple arterial grafts often have less comorbidities than patients who receive a single IMA graft [Citation7,Citation9,Citation10]. Complication rates may increase in conjunction with the use of multiple arterial grafts, e.g. sternal wound infections with the use of BIMAs, especially in diabetic patients [Citation23]. Furthermore, arterial graft spasm in the radial artery conduits is often a problem, even causing lethal cardiac hypoperfusion [Citation24]. The recently published multi-centre randomized ART trial found no difference in survival at 5 years between patients receiving SIMA or BIMA grafts but, importantly, it found an increased rate of sternal wound complications with BIMA grafting [Citation11].
Our study shows that favourable outcome of CABG can be achieved using the classical technique of LIMA to the LAD in addition to saphenous vein grafts. This even applies to a single centre that treats all patients in the country and where sicker patients can´t be referred to another hospital. It emphasizes that further evidence from RCTs with longer follow-up and subgroup analysis is needed to increase the rate of multiple arterial grafting.
The total rate of MACCE at 5 years after surgery was 19.7% in the present study, which is considerably lower than the 26.9% in the SYNTAX trial [Citation1]. For comparison, the freedom-from-MACCE survival for CABG patients at 5 years in the Arterial Revascularization Therapies Study (ARTS) was 78% [Citation25]. Both studies used the same definition of MACCE, but randomized controlled trials inherently capture more adverse events than a retrospective study like ours. Our freedom-from-MACCE rate also compares favourably with that in other studies such as the one by Deb et al. (2016), which had a 5-year freedom-from-MACCE rate of around 84% [Citation26].
Importantly, the total rate of repeat revascularization was only 6.2% at 5 years (84 patients). The majority of these patients (80 patients) underwent PCI, and only four (0.3%) needed to undergo a repeat CABG at this time point. Similar results were reported recently in the ART trial, 6.5% in the BIMA group and 6.6% in the SIMA group [Citation11]. A recent Italian study showed a 5-year PCI rate of 6.5% for male patients and 8% for female patients, and repeat CABG in only 0.1–0.2% [Citation27]. For comparison, the rate of repeat revascularization at 5 years was 13.7% in the SYNTAX trial and 8.8% in the ARTS trial [Citation1,Citation25].
The 5-year long-term rate of stroke in the present study was 4.5%, which is similar to the 2.5–5.4% previously reported [Citation1,Citation2,Citation11,Citation25,Citation27]. Interestingly, the 5-year rate of MI was only 2.2% in the present study, which compares favourably with the figures of 3.5% and 3.8% in the ART and SYNTAX trials, and to a more than twofold higher rate in the FREEDOM trial (5.2%) and the ARTS trial (5.6%) [Citation1,Citation2,Citation25]. The low rate of long-term MI in our study is probably explained by the definition of MI, since in the studies mentioned, perioperative and short-term MIs were included in the analysis, while in the present study only MIs occurring more than 30 days from the operation were defined as being long-term.
By Cox regression analysis, low LVEF, COPD, and CKD, a previous history of PCI or diabetes, and old age were all independent predictors of death and MACCE. These have all been recognized previously as negative predictors of long-term survival after CABG [Citation28–31]. Similar predictors of long-term MACCE have also been reported [Citation26,Citation31]. Interestingly, a later calendar year of operation was a significant predictor of more favourable survivalâ indicating an improvement in outcome after CABG in Iceland. However, we cannot exclude the possibility that this improvement in survival was caused by some differences in population characteristics occurring during the study period. Furthermore, the long-term survival of our cohort was similar to the survival of a matched cohort from the Icelandic population, further underscoring the favourable long-term results of the operation.
Limitations and strengths
The main limitation of this study was its retrospective design. Thus, data on factors such as freedom from angina or other cardiac symptoms were not registered in sufficient detail for inclusion in our analysis. Furthermore, graft patency was not routinely examined, since angiography was only performed upon recurrence of symptoms. A clear strength was the use of several centralized registries in a population-based cohort, with a complete survival follow-up up to 13.5 years. This included access to centralized CABG and PCI registries and availability of hospital records from all the hospitals in Iceland that treat patients with cardiovascular diseases, thereby covering the whole country. In addition, the 1,507 patients were operated by only eight senior surgeons at a single centre.
Conclusions
The long-term outcome following CABG in our nationwide cohort is favourable, and improving. This is reflected by a very favourable 5-year survival rate (89.9%) closely mimicking the survival of the general population of the same age and gender, and a high 5-year freedom-from-MACCE rate (80.3%). Our findings reflect modern CABG and confirm the favourable long-term outcome of CABG with the strategy of using the LIMA and the great saphenous vein as conduits.
Acknowledgements
We thank Hannes Sigurjonsson and Saemundur Oddsson from the Cardiothoracic Research Team at Landspitali for helping with data collection and Gunnhildur Johannesdottir for secretarial help.
Disclosure statement
The authors report no conflicts of interest.
This work was supported by grants from the Landspitali University Hospital Research Fund, the University of Iceland Research Fund, and the Helga Gudmundsdottir and Sigurlidi Kristjansson Memorial Fund.
Additional information
Funding
References
- Mohr FW, Morice M-C, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet. 2013;381:629–638.
- Farkouh ME, Domanski M, Sleeper LA, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012;367:2375–2384.
- Elbardissi AW, Aranki SF, Sheng S, et al. Trends in isolated coronary artery bypass grafting: An analysis of the Society of Thoracic Surgeons adult cardiac surgery database. J Thorac Cardiovasc Surg. 2012;143:273–281.
- Diodato M, Chedrawy EG. Coronary artery bypass graft surgery: the past, present, and future of myocardial revascularisation. Surgery Res Pract. 2014;2014:726158.
- Loop FD, Lytle BW, Cosgrove DM, et al. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med. 1986;314:1–6.
- Cameron A, Davis KB, Green G, et al. Coronary bypass surgery with internal-thoracic-artery grafts–effects on survival over a 15-year period. N Engl J Med. 1996;334:216–219.
- Tranbaugh RF, Dimitrova KR, Friedmann P, et al. Radial artery conduits improve long-term survival after coronary artery bypass grafting. Ann Thorac Surg. 2010;90:1165–1172.
- Chow MS, Sim E, Orszulak TA, et al. Patency of internal thoracic artery grafts: comparison of right versus left and importance of vessel grafted. Circulation. 1994;90:Ii129–Ii132.
- Lytle BW, Blackstone EH, Sabik JF, et al. The effect of bilateral internal thoracic artery grafting on survival during 20 postoperative years. Ann Thorac Surg. 2004;78:2005–2014.
- Locker C, Schaff HV, Dearani JA, et al. Multiple arterial grafts improve late survival of patients undergoing coronary artery bypass graft surgery: analysis of 8622 patients with multivessel disease. Circulation. 2012;126:1023–1030.
- Taggart DP, Altman DG, Gray AM, et al. Randomized Trial Of Bilateral Versus Single Internal-Thoracic-Artery Grafts. N Engl J Med. 2016;375:2540–2549.
- Swedeheart Annual report 2015 [cited 2016 19/10]. Available from: http://www.ucr.uu.se/swedeheart/index.php/arsrapport-2015.
- Bridgewater BKB, Kinsman R, Walton PK. on behalf of the Society for Cardiothoracic Surgery in Great Britain and Ireland. Sixth National Adult Cardiac Surgical Database Report 2008. London, UK: Dendrite Clinical Systems Ltd; 2009 [cited 2016].
- Helgadottir S, Sigurdsson MI, Ingvarsdottir IL, et al. Atrial fibrillation following cardiac surgery: risk analysis and long-term survival. J Cardiothorac Surg. 2012;7:87.
- Yi G, Shine B, Rehman SM, et al. Effect of bilateral internal mammary artery grafts on long-term survival: a meta-analysis approach. Circulation. 2014;130:539–545.
- National Kidney Foundation. KDOQI Clinical Practice Guideline for Diabetes and CKD: 2012 Update. Am J Kidney Dis. 2012;60:850–886.
- Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612.
- Roques F, Nashef SA, Michel P, et al. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg. 1999;15:816–822. Discussion 22–3.
- Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81:515–526.
- Pohar M, Stare J. Relative survival analysis in R. Comput Methods Programs Biomed. 2006;81:272–278.
- Grau JB, Ferrari G, Mak AW, et al. Propensity matched analysis of bilateral internal mammary artery versus single left internal mammary artery grafting at 17-year follow-up: validation of a contemporary surgical experience. Eur J Cardiothorac Surg. 2012;41:770–775. Discussion 6.
- Lytle BW, Blackstone EH, Loop FD, et al. Two internal thoracic artery grafts are better than one. J Thorac Cardiovasc Surg. 1999;117:855–872.
- Savage EB, Grab JD, O’Brien SM, et al. Use of both internal thoracic arteries in diabetic patients increases deep sternal wound infection. Ann Thoracic Surg. 2007;83:1002–1006.
- He GW, Taggart DP. Spasm in Arterial Grafts in Coronary Artery Bypass Grafting Surgery. Ann Thorac Surg. 2016;101:1222–1229.
- Serruys PW, Ong AT, van Herwerden LA, et al. Five-year outcomes after coronary stenting versus bypass surgery for the treatment of multivessel disease: the final analysis of the Arterial Revascularization Therapies Study (ARTS) randomized trial. J Am Coll Cardiol. 2005;46:575–581.
- Deb S, Tu JV, Austin PC, et al. Impact of south asian ethnicity on long-term outcomes after coronary artery bypass grafting surgery: a large population-based propensity matched study. J Am Heart Assoc. 2016;5:e003941.
- Nicolini F, Vezzani A, Fortuna D, et al. Gender differences in outcomes following isolated coronary artery bypass grafting: long-term results. J Cardiothorac Surg. 2016;11:144.
- O'Boyle F, Mediratta N, Fabri B, et al. Long-term survival after coronary artery bypass surgery stratified by EuroSCORE. Eur J Cardiothorac Surg. 2012;42:101–106. Discussion 6–7.
- Wu C, Camacho FT, Wechsler AS, et al. Risk score for predicting long-term mortality after coronary artery bypass graft surgery. Circulation. 2012;125:2423–2430.
- Volzke H, Henzler J, Menzel D, et al. Outcome after coronary artery bypass graft surgery, coronary angioplasty and stenting. Int J Cardiol. 2007;116:46–52.
- Dalen M, Ivert T, Holzmann MJ, et al. Coronary artery bypass grafting in patients 50 years or younger: a Swedish nationwide cohort study. Circulation. 2015;131:1748–1754.