Abstract:
Objectives. Over the past decade, the number of patients on dialysis and with cardiovascular diseases has steadily increased. This retrospective analysis compares the postoperative mortality after cardiac surgery between patients on hemodialysis and peritoneal dialysis. Methods. Between 1998 and 2015, 136 patients with end-stage renal disease initiating dialysis more than one month before surgery underwent cardiac surgery. Demographics, preoperative hemodynamic and biochemical data were collected from the patient records. Vital status and date of death was retrieved from a national register. Results. Hemodialysis was undertaken in 73% and peritoneal dialysis in 22% of patients aged 59.7 ± 12.9 years, mean EuroSCORE 8.6% ± 3.5. Isolated coronary artery bypass graft was performed in 46%, isolated valve procedure in 29% and combined procedures in 24% with no significant statistical difference between groups. The 30-day mortality was 14% for hemodialysis patients and 3% for peritoneal dialysis patients (p = .056). One-year and 5-year mortality were, 30% and 59% in the hemodialysis group, 30% and 57% in the peritoneal dialysis group (p = .975, p = .852). Independent predictors of total mortality were age (p = .001), diabetes (p = .017) and active endocarditis (p = .012). Conclusion. No statistically significant difference in mortality was found between patients in hemo- or peritoneal dialysis. However, we observed that patients with end-stage renal disease on dialysis have two times higher mortality rate than estimated by EuroSCORE.
Introduction
An increased number of patients with ESRD receive dialysis by peritoneal (PD) and hemodialysis (HD), and they have a reduced life span compared to the general population [Citation1]. This difference may be due to an increased incidence of hypertension, diabetes, smoking and hypercholesterolemia [Citation2,Citation3], which are the risk factors for cardiovascular disease. Causes of the increased incidence of cardiovascular diseases includes accelerated atherosclerosis genesis, disturbed calcium-phosphate metabolism, lipid derangement, endothelia dysfunction and inflammation [Citation4].
Despite these risks and a 30 times higher cardiovascular mortality in dialysis patients compared to the general population [Citation3,Citation5,Citation6] patients on PD and HD demonstrated improved survival during the last decade [Citation7–9]. From 1988 to 2003 the incidence of coronary revascularization procedures in patients with ESRD doubled from 2.5 to 5 per 1000 patient years [Citation7]. Previous studies [Citation7,Citation8,Citation10–12] have reported that need for dialysis preoperatively is a significant risk factor for mortality and postoperative complications after cardiac surgery. In addition, some of the these studies examined the effect of dialysis modality (HD and PD) on survival in ESRD patients. However, the results are conflicting. Both HD and PD accelerates the process of vascular diseases such as coronary artery disease and cardiac events [Citation9].
The question that remains is whether dialysis modality have an influence on mortality and postoperative complications after cardiac surgery. In this study we wanted to compare the postoperative complications and mortality between patients on HD and PD and to identify preoperative predictors of mortality.
Material and methods
All patients in the Capital and Sealand region of Denmark with ESRD treated with dialysis and undergoing cardiac surgery from 1998 to 2015 were included in this retrospective analysis. Cardiac surgery was performed in 199 patients. After review of the patient records, 63 patients were excluded as dialysis was started less than one month before surgery indicating potentially reversible acute kidney failure and not ESRD.
Data collection
Patients were identified in the Cardiothoracic Departments’ clinical database (PATS®, Oregon, USA). All cardiac surgical procedures performed at Rigshospitalet are registered in the database and preoperative dialysis is specifically noted in this database.
Patients’ demographics, risk factors for morbidity and mortality, surgical clinical data, preoperative hemodynamics and biochemical as well as postoperative outcome data were collected from the patient records. Vital status and date of death was retrieved from The Danish Civil Registration System, latest search November 31, 2015.
Statistical analysis
Continuous data was studied as mean ± standard deviations or median with range and compared using Student´s t-test. Categorical data was collected as numbers and percentages and compared using chi square test.
Statistical significance was defined as p-values ≤.05 and all p-values reported were two-sided.
Overall survival rate of the patients was outlined as the time from surgery until the time of death or censored at the last time of follow-up. Mortality curves were generated using Kaplan-Meier plots and compared using log-rank test. Furthermore, the use of a Cox regression model assessed the impact of independent variables on the primary outcome, all-cause of death. Independent variables as age, gender, type of procedure, diabetes, endocarditis, type of dialysis and time on dialysis were analyzed. Statistical analysis was performed using SPSS 22 software (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp).
Results
During the study period 136 patients with ESRD on chronic renal replacement therapy underwent cardiac surgery, 99 (73%) patients were on HD and 30 (22%) on PD, and in 7 patients the type of dialysis could not be identified. Baseline demographics were not statistically different in the two groups (). The mean age was 59.7 ± 12.9 years, 22% (30) were females and mean EuroSCORE was 8.6% ± 3.5. The median time on dialysis was 36 (1–396) months.
Table 1. Baseline characteristics of patients*.
The ethology of ESRD was mostly due to diabetic nephropathy (25%) (). Twenty (15%) patients had previously been kidney transplanted, with no graft function. Left ventricular ejection fraction (LVEF) exceeded 50% in 40% of the patients ().
Table 2. Renal history/status of patients*.
The majority of patients underwent an isolated coronary artery bypass graft (CABG) procedure, followed by an isolated valve procedure and a combined CABG and valve procedure ().
The median length of stay in the intensive care unit (ICU) was 1 day, (range 1–48 days) and the median length of stay in the hospital was 8 days, (range 1–52) days with no difference between HD and PD patients (). There was an in-hospital mortality of 10%, only 35% of the patients were discharged directly to the home, while 54% were discharged to another hospital (2% with missing data). Reoperations were performed in 15% of the patients primarily due to bleeding (13%). During hospitalization, 5% had pleurocentesis performed, 43% had cardiac arrhythmias, 8% had a stroke, 5% sternal infection and multiple organ failure occurred in 5% of the population.
Table 3. Postoperative data*.
Postoperative intubation beyond 48 hours occurred in 18% of the patients.
Re-hospitalization (all departments apart from Nephrology department included) occurred in 42% of the patients.
The 30-day mortality rate was 14% (N = 14) for HD patients and 3% (N = 1) for PD patients (p = 0.069). However, at one year the mortality rate increased to 30% (N = 30) for HD patients and 30% (N = 9) for PD patients.
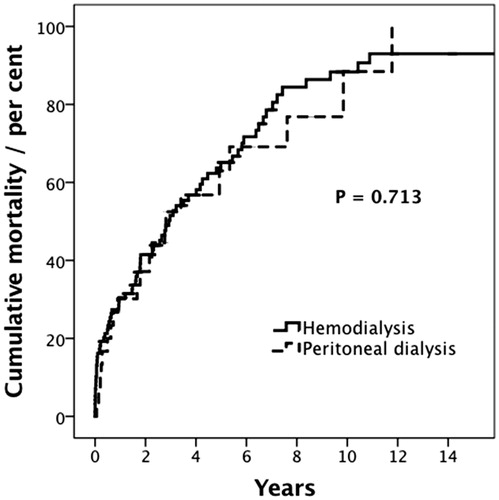
Mean time of follow-up in our cohort was 3 ± 3.3 years. At 5 year the mortality rate was 65% (N = 58) for HD and 63% (N = 17) for PD (p = .713) (, Kaplan Meier).
Figure 1. Mortality curve comparing hemodialysis and peritoneal dialysis. There was no statistical difference between the two groups (p = 0.713). (solid line hemodialysis, dashed line peritoneal dialysis).
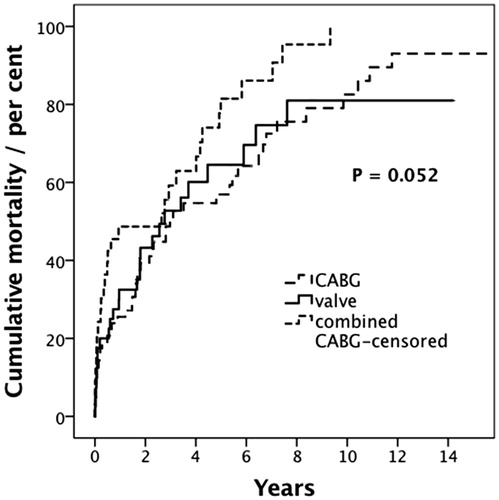
A multivariate Cox´s proportional hazard regression model, identified age (HR= 1.03, 95% CI 1.014–1.055, p = .001), patients with diabetes (HR = 1.75, 95% CI 1.11–2.767, p = .017), and active endocarditis (HR = 2.21, 95% CI 1.188–4.094, p = .012) as independent predictors of mortality. As we found no difference between HD and PD, we did a post hoc analysis of mortality between the different surgical procedures. The 30-day mortality rate was 11% for CABG, 12% for valve surgery and 21% for combined surgery. At one year and 5-year the mortality rate was 25% and 57% for CABG, respectively and 32% and 64%, for valve surgery, and 49% and 81%, for combined surgery (p = .052) ().
Discussion
In our study we found no statistically significant difference in survival after cardiac surgery between patients in hemo- or peritoneal dialysis. Patients on dialysis with their fragile condition have an increased risk of mortality and complications after major surgical trauma such as cardiac surgery. In our study, we found a 30-day mortality as high as 14% for HD and 3% for PD. Similar results were reported recently with a 30 days mortality of 16.4% of 483 patients on dialysis undergoing cardiac surgery [Citation13]. This high mortality rate and numeric differences between HD and PD makes it important to gain a deeper understanding of the difference in short term mortality. It is also important due to the increasing number of patients with ESRD undergoing cardiac surgery. Some studies showed no survival difference between HD and PD, and others demonstrated an advantage to either HD or PD. The difference which has long been known is that patients treated with hemodialysis are older and have more comorbidities and studies demonstrating a benefit for patients on PD are due to younger age and a reduced burden of cardiovascular risk factors [Citation14]. But there are also studies where patients receiving peritoneal dialysis with cardiovascular disease have poorer survival [Citation15].
The studies that examined the difference in mortality between HD and PD found conflicting results. Heaf [Citation16] looked at the influence of dialysis modality on prognosis in 4921 dialysis patients and showed that PD patients have better survival during the first 2 years. In contrast, Jaar [Citation15] who compared risk of death among patients receiving dialysis (1041 patients), showed that patients with PD had twice the risk of death during the second year of follow-up and that patients with cardiovascular diseases and PD had a poorer survival during the first years. In our study we found no difference in one and five year mortality. Similar to our study Kumar [Citation17], did not find any difference in survival rates between patients on HD and PD after cardiac surgery. Not only the type of dialysis have been studied with conflicting results. The influence of dialysis duration on the survival and postoperative complications have also showed conflicting results. In our study, dialysis duration influenced survival in patients treated with PD. Patients on PD had lower survival the longer duration on dialysis. This is in accordance with some other studies after adjustment of background profiles of HD vs PD [Citation14].
Jaar [Citation15] found no differences in survival during the first year, however after two years a statistically significant higher mortality in PD patients was observed.
Heaf [Citation16] found that PD patients had better survival during the first two years and subsequent similar to HD. Ganesh [Citation9] found that PD patients on dialysis for less than 6 months had a better survival (RR = 1.15 p < .001). This was partly in accordance with our study where patients on PD had lower survival the longer dialysis duration. Hemodialysis duration had no statistically effect on survival even when we analyzed all patients regardless dialysis modality. The explanation for this may be that patients who undergoes cardiac surgery are older and have been on dialysis for an average of 4 years. This is consistent with poor outcome since average survival after initiating dialysis are approximately 4 years.
The question is why patients with ESRD on dialysis have this short survival, apart from increased risk factors. One could speculate that volume overload, electrolyte abnormalities, metabolic acidosis and anemia, which advances with declining kidney function as well as increased bleeding tendency could be attributing factors to the poor prognosis in patients on dialysis. This could also be the explanation why patients on dialysis have increased postoperative complications. In the present study we found an increased frequency of major complications after surgery, especially a high number of bleeding episodes. The number of reoperations for bleeding, sternal infection and stroke were up to 5 times as high as in patients not on dialysis as known from data from the Danish Heart Registry [Citation18]. The reason for increased bleeding complications is unknown but may be related to the impaired coagulation system seen in patients with reduced kidney function [Citation19]. Anyhow, reoperations for bleeding after cardiac surgery in patients on dialysis opens to an array of other complications also due to the need for multiple transfusions [Citation20]. These complications include prolonged time in the intensive care unit due to need for intubation and ventilation, septicemia and organ failure etc.
However in our study we did not find any differences in postoperative complications between HD and PD. In contrast to our findings, Kumar [Citation17] did find higher rate of some postoperative complication (including prolonged intubation time, postoperative infections or death), in patients treated with HD versus PD (50% versus 28%). This underlines the difficulty in comparing the different groups due to the differences in dialysis characteristics at baseline.
Risk score estimation for patients undergoing cardiac surgery is mainly based on EuroSCORE or STS score. In the present study the EuroSCORE predicted a 30-day mortality rate of 8%, which proved to be low compared to our result of a 14% 30-day mortality rate. These numbers indicates that the existing predictive algorithms such as EuroSCORE and STS are unable to predict the risk of postoperative mortality in this group of patients after cardiac surgery. The explanation could be that existing risk scores do not include variables describing the biological status of the patient. The biological status, or frailty, seems to have a great influence in these patients, as patients with ESRD on dialysis are reported to be significant more frail than the general population [Citation21,Citation22] Different types of risk scores exist to measure the outcomes in patients with ESRD when starting treatment with dialysis [Citation23]. A systematic determination of frailty in ESRD patients before cardiac surgery could be a tool to predict and possibly reduce the risk in these patients. Considering the high rate of mortality and postoperative complications, several studies have investigated if any predictor exists for mortality in ESRD patients on dialysis undergoing cardiac surgery [Citation11,Citation24–26]. Horst [Citation10] found time on dialysis and combined surgery as predictors. In our study we did not find time on dialysis to have any influence, except patients on PD. However we found a numeric difference, with a higher mortality in patients undergoing combined surgery.
Patients with ESRD and on dialysis undergoing cardiac surgery have a high 30-day mortality as well as poor long-term survival. The majority of patients are on hemodialysis. However, we found no difference in mortality or postoperative complications between patients on hemodialysis compared to peritoneal dialysis.
Disclosure statement
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Additional information
Funding
References
- The Danish nephrology visions report. 2020. Available from: http://www.nephrology.dk/Publikationer/accept260413Visionsrapport2020.pdf
- Levey A, Beto J, Coronado B, et al. Controlling the epidemic of cardiovascular disease in chronic renal disease: what do we know? What do we need to learn? Where do we go from here? National Kidney Foundation Task Force on Cardiovascular Disease Am J Kidney Dis. 1998;32:853–906.
- Sarnak MJ, Levey AS, Schoolwerth AC, et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Hypertension. 2003;42:1050–1065.
- Wanner C, Amann K, Shoji T. The heart and vascular system in dialysis. Lancet. 2016;388:276–284.
- Foley RN. Clinical epidemiology of cardiac disease in dialysis patients: left ventricular hypertrophy, ischemic heart disease, and cardiac failure. Semin Dial. 2003;16:111–117.
- Levin A. Clinical epidemiology of cardiovascular disease in chronic kidney disease prior to dialysis. Semin Dial. 2003;16:101–105.
- Parikh DS, Swaminathan M, Archer LE, et al. Perioperative outcomes among patients with end-stage renal disease following coronary artery bypass surgery in the USA. Nephrol Dial Transplant. 2010;25:2275–2283.
- Rahmanian PB, Adams DH, Castillo JG, et al. Early and late outcome of cardiac surgery in dialysis-dependent patients: single-center experience with 245 consecutive patients. J Thorac Cardiovasc Surg. 2008;135:915–922.
- Ganesh SK, Hulbert-Shearon T, Port FK, et al. Mortality differences by dialysis modality among incident ESRD patients with and without coronary artery disease. J Am Soc Nephrol. 2003;14:415–424.
- Horst M, Mehlhorn U, Hoerstrup SP, et al. Cardiac surgery in patients with end-stage renal disease: 10-year experience. Ann Thorac Surg. 2000;69:96–101.
- Yamamura M, Mitsuno M, Tanaka H, et al. Risk factors for open heart surgery in hemodialysis patients. Gen Thorac Cardiovasc Surg. 2009;57:235–238.
- Bechtel JFM, Detter C, Fischlein T, et al. Cardiac surgery in patients on dialysis: decreased 30-day mortality, unchanged overall survival. Ann Thorac Surg. 2008;85:147–153.
- Leontyev S, Davierwala PM, Gaube L-M, et al. Outcomes of dialysis-dependent patients after cardiac operations in a single-center experience of 483 patients. Ann Thorac Surg. 2017;103:1270–1276.
- Termorshuizen F, Korevaar JC, Dekker FW, et al. Hemodialysis and peritoneal dialysis: comparison of adjusted mortality rates according to the duration of dialysis: analysis of The Netherlands Cooperative Study on the Adequacy of Dialysis 2. J Am Soc Nephrol. 2003;14:2851–2860.
- Jaar BG, Coresh J, Plantinga LC, et al. Comparing the risk for death with peritoneal dialysis and hemodialysis in a National Cohort of Patients with Chronic Kidney Disease. Ann Intern Med. 2005;143:174
- Heaf JG, Løkkegaard H, Madsen M. Initial survival advantage of peritoneal dialysis relative to haemodialysis. Nephrol Dial Transpl. 2002;17:112–117.
- Kumar VA, Ananthakrishnan S, Rasgon SA, et al. Comparing cardiac surgery in peritoneal dialysis and hemodialysis patients: perioperative outcomes and two-year survival. Perit Dial Int. 2012;32:137–141.
- The Danish Heart Registre: Annual Report. 2015. Available from: www.si-folkesundhed.dk/upload/dhr_a%CC%8Arsberetning_2015.pdf
- Kaw D, Malhotra D. Platelet dysfunction and end-stage renal disease. Semin Dial. 2006;19:317–322.
- Bhaskar B, Dulhunty J, Mullany DV, et al. Impact of blood product transfusion on short and long-term survival after cardiac surgery: more evidence. Ann Thorac Surg. 2012;94:460–467.
- Alfaadhel TA, Soroka SD, Kiberd BA, et al. Frailty and mortality in dialysis: evaluation of a clinical frailty scale. Clin J Am Soc Nephrol. 2015;10:832–840.
- Drost D, Kalf A, Vogtlander N, et al. High prevalence of frailty in end-stage renal disease. Int Urol Nephrol. 2016;48:1357–1362.
- Painter P, Marcus R. Physical function and gait speed in patients with chronic kidney disease. Nephrol Nurs J. 2013;40:529–538.
- Zhong H, David T, Zhang AH, et al. Coronary artery bypass grafting in patients on maintenance dialysis: is peritoneal dialysis a risk factor of operative mortality? Int Urol Nephrol. 2009;41:653–662.
- Thourani VH, Sarin EL, Kilgo PD, et al. Short- and long-term outcomes in patients undergoing valve surgery with end-stage renal failure receiving chronic hemodialysis. J Thorac Cardiovasc Surg. 2012;144:117–123.
- Cooper WA. Impact of renal dysfunction on outcomes of coronary artery bypass surgery: results from the society of thoracic surgeons national adult cardiac database. Circulation. 2006;113:1063–1070.