Abstract
Objective. Oxygen (O2) have been a cornerstone in the treatment of acute myocardial infarction. Studies have been inconclusive regarding the cardiovascular and analgesic effects of oxygen in these patients. In the SOCCER trial, we compared the effects of oxygen treatment versus room air in patients with ST-elevation myocardial infarction (STEMI). There was no difference in myocardial salvage index or infarct size assessed with cardiac magnetic resonance imaging. In the present subanalysis, we wanted to evaluate the effect of O2 on chest pain in patients with STEMI. Design. Normoxic patients with first time STEMI were randomized in the ambulance to standard care with 10 l/min O2 or room air until the end of the percutaneous coronary intervention (PCI). The ambulance personnel noted the patients´ chest pain on a visual analog scale (VAS; 1-10) before randomization and after the transport but before the start of the PCI, and also registered the amount of morphine given. Results. 160 patients were randomized to O2 (n = 85) or room air (n = 75). The O2 group had a higher median VAS at randomization than the air group (7.0 ± 2.3 vs 6.0 ± 2.9; p = .02) and also received a higher median total dose of morphine (5.0 mg ± 4.4 vs 4.0 mg ± 3.7; p = .02). There was no difference between the O2 and air groups in VAS at the start of the PCI (4.0 ± 2.4 vs 3.0 ± 2.5; p = .05) or in the median VAS decrease from randomization to the start of the PCI (−2.0 ± 2.2 vs −1.0 ± 2.9; p = .18). Conclusion. Taken together with previously published data, these results do not support a significant analgesic effect of oxygen in patients with STEMI.
European Clinical Trials Database (EudraCT): 2011-001452-11.
ClinicalTrials.gov Identifier: NCT01423929
Introduction
Ever since Dr. Charles Steele in 1900 published [Citation1] that one of his patients with angina pectoris was relieved by oxygen (O2) therapy, supplemental O2 has been a cornerstone in the treatment of patients with suspected acute myocardial infarction (AMI) and recommended by many guidelines [Citation2,Citation3]. O2 therapy is believed to reduce ischemia in the myocardium and the risk of arrhythmias [Citation4] and acute heart failure, and to decrease the ischemic chest pain.
Some of the first studies suggested that O2 therapy may have positive circulatory effects in AMI patients [Citation5,Citation6], but many modern studies indicate that O2 therapy is more likely to have negative cardiovascular effects and that it may even increase infarct size [Citation7–9]. Recently, however, both Ranchord et al. [Citation10] and Khoshnood et al. [Citation11,Citation12] found no effect of O2 therapy on infarct size in patients with ST elevation myocardial infarction (STEMI).
The analgesic effect of O2 therapy observed by Steele was also supported by early studies. In 1939 Boothby et al. [Citation13] stated that administration of 100% O2 has a rapid pain-relieving effect in angina pectoris, and in 1940, Boland [Citation5] concluded that O2 therapy effectively decreases chest pain in AMI patients, even when opiates fail to help. A decade later, however, Russek et al. [Citation14] declared that supplemental O2 to patients with angina had no effect on the circulation, AMI development or chest pain. More recent studies suggest that there is no analgesic effect of O2 therapy in patients undergoing elective percutaneous coronary intervention (PCI) [Citation15] or AMI patients and relief of angina [Citation8].
In the present substudy of the Supplemental Oxygen in Catheterized Coronary Emergency Reperfusion (SOCCER) trial, we assessed the effect of O2 therapy vs room air on chest pain in STEMI patients transported to acute PCI.
Methods
The SOCCER study was a dual-center, single blinded randomized controlled trial conducted in Lund and Malmö in Sweden between January 2012 and August 2015. Regarding the design and method, the reader is referred to previous publications [Citation11,Citation12,Citation16]. The trial was approved by both the Regional Ethical Review Board and the Swedish Medical Products Agency (EudraCT No 2011-001452-11). This study is reported in accordance with the CONSORT statement [Citation17].
Patient inclusion and management
In brief, patients with first time STEMI, symptom duration of <6 hours and a normal blood oxygen saturation (≥94%) were, after verbal consent, included in the ambulance and randomized to either 10 L/min supplemental O2 therapy (O2 group) or room air (air group). All patients had an OxyMask fitted and were blinded to the study intervention which lasted until the end of the percutaneous coronary intervention (PCI).
Except for the study intervention, all patients were treated according to local and international guidelines with dual antiplatelet therapy, as well as beta-blockers and morphine as needed. If blood oxygen saturation fell under 94%, the study intervention was terminated and standard care O2 treatment with 10 l/min started. The ambulance personnel used case report forms to note vital parameters and patient management, including medications given.
After the PCI, the patients were informed by a study physician and consented to participation in writing.
This study was a planned secondary analysis of data from the SOCCER trial, and there was no formal sample size calculation.
Visual analog scale
The visual analog scale (VAS) is an easy, reliable, widely used and validated tool to measure the intensity of acute pain [Citation18–20]. The VAS consists of a numeric scale between 0-10 (0-100 mm) on which the patient indicates his or her level of pain. Zero (0) corresponds to “no pain” and ten (10) to the “worst imaginable pain".
In this study, the ambulance personnel reported the patients’ assessment of their chest pain, i.e. their VAS score, on case report forms both at randomization and at arrival at the PCI-center.
Statistical analysis
We compared the study groups with respect to VAS score using a 2-sided Mann-Whitney test because the data were not normally distributed, with a p < .05 considered statistically significant. The null hypothesis was that there was no difference in VAS score between the groups. All data were analyzed using Microsoft Excel and IBM SPSS Statistics V22.
Results
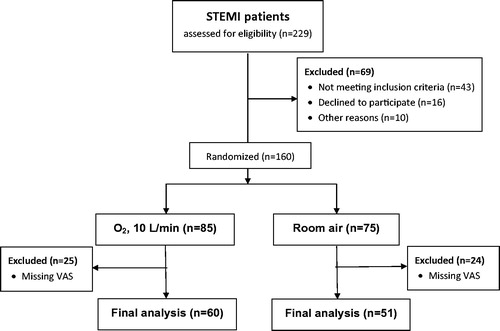
The study profile is outlined in . Of 229 patients assessed for eligibility, 160 were randomized to the O2 group or the air group. After excluding patients with missing VAS values in the two groups, 111 patients were included in the final analysis; 60 patients randomized to the O2 group and 51 randomized to the air group. The missed VAS scores were often because the patients were not able to use the scale for scoring their pain due to language barriers or cognitive difficulties.
The Supplemental Tables 1 and 2 show patient and PCI procedural characteristics for the first 160 patients included. For the 111 patients included in the final analysis, both patient characteristics () and PCI procedural characteristics () were similar. By randomization, patients in the air group were significantly more often treated with diuretics and past smokers than those in the O2 group. Supplemental Tables 3 and 4 outline patient characteristics and PCI procedural characteristics for the excluded patients in the two groups. The excluded patients to a great degree shares the same characteristics as the patients included in the final analysis.
Table 1. Patient characteristics at randomization for those included in the final analysis.
Table 2. Procedural characteristics for those included in the final analysis.
shows both the pain management and VAS for the 111 included patients. A significantly higher amount of the patients included in the O2 group received intravenous morphine in comparison with the air group (81.7% respective 62.7%; p = .026). The median amount of morphine given were also significantly higher in the O2 group compared with the air group (6.0 mg ± 4.6 respective 4.0 mg ± 3.9; p = .007).
Table 3. Pain management and VAS in patients included in the final analyses.
The O2 group had also a significantly higher median VAS in comparison with the air group at randomization (7.0 ± 2.3 respective 6.0 ± 2.9; p = .020) but not at arrival to the PCI-center (4.0 ± 2.4 respective 3.0 ± 2.5; p = .050). When comparing the median difference in VAS from randomization to the beginning of the PCI, between the O2 group and the air group, the difference was not significant (−2.0 ± 2.2 respective −1.0 ± 2.9; p = .183).
Discussion
In this sub-study we aimed to evaluate the effect of O2 therapy on chest pain in STEMI patients undergoing PCI. We found that patients in the O2 group had already before the randomization a significantly higher VAS and most likely because of that, also received significantly more morphine in comparison with the air group.
Although some studies state that O2 therapy diminish chest pain [Citation5,Citation13], other studies have shown no effect of O2 therapy on chest pain [Citation8,Citation14,Citation15]. In a Cochrane review on the effects of O2 therapy in patients with AMI [Citation21], only two studies were identified which discussed the question of pain; Rawles and Kenmure [Citation7] as well as Wilson and Channer [Citation22]. Both these studies reported the use of opiates as a measurement for pain and showed no difference between patients receiving O2 therapy or air. However, the authors of the Cochrane report [Citation21] conclude that the risk of bias were high in these two studies, and that no conclusions should be drawn. Similarly, no effect of O2 therapy on chest pain was observed in the OXYPAIN trial [Citation15], where a total of 305 patients with stable angina or acute coronary syndrome (ACS) undergoing PCI was included. The study measured chest pain during PCI by using the VAS and showed no effect on chest pain in patients being randomized to O2 instead of air. A limitation of this study may have been that it included patients with stable angina who may have had less pain during the PCI compared to STEMI patients who often chest pain also before balloon inflation. Also the AVOID study [Citation8,Citation9], the results of which suggested a larger IS in patients treated with O2 compared to air, did not show any difference between the two arms when discussing pain or the use of analgesics; the median pain scores were equal for the groups.
Our finding of a higher median VAS value for the patients in the O2 group before intervention is probably a play of chance. Because of the higher VAS value, the patients in the O2 group also received significantly more morphine. During the study intervention, the median VAS value fell in both groups, and neither the decrease nor the values at PCI start were significantly different between the groups. Since most patients in both groups received morphine, and since the decreases in VAS values were similar in comparing the two groups, we could not discern a significant effect of O2 on the chest pain. Many studies, e.g. [Citation23–25], describe the analgesic effect of morphine in AMI patients, and we believe that the observed diminished pain was explained by the fact that the majority of our patients were given iv morphine.
Study limitations
As our results include STEMI patients from two university hospitals only, they may not be representative for all STEMI patients. However, the patients included in the present study have similar characteristics and were managed in a similar way as STEMI patients in other studies [Citation26–30]. We believe that the randomization-induced difference in diuretic use and previous smoking between the study groups () was without significant effect on the results.
The patients´ VAS and morphine injections were all managed by the paramedics who were aware of the patient´s group allocation. It is unclear whether this may have influenced the patient management, but with respect to our data and results in our previous publications [Citation11,Citation12], such influence is deemed to be small if at all existent.
Conclusion
Patients in the O2 group had a significantly higher median VAS before randomization, in comparison with patients in the air group. However, this might be the result of play of chance. In discussing the analgesic effect of O2, a major analgesic effect does not seem to exist. Larger studies are needed to fully answer the question of oxygen as an analgesic agent. This present study, taken together with previously published data, do not support a significant analgesic effect of O2 in patients with STEMI.
Suppl.zip
Download Zip (73.9 KB)Disclosure statement
The authors report no conflicts of interest.
References
- Steele C. Severe angina pectoris relieved by oxygen inhalations. BMJ. 1900;2:1568–1568.
- International Liaison Committee on Resuscitation. 2005 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Part 1: introduction. Resuscitation. 2005;67:249–269.
- Pollack CV, Diercks DB, Roe MT, et al. 2004 American College of Cardiology/American Heart Association guidelines for the management of patients with ST-elevation myocardial infarction: implications for emergency department practice. Ann Emerg Med. 2005;45:363–376.
- Ashfield R, Gavey C. Severe acute myocardial infarction treated with hyperbaric oxygen. Report on forty patients. Postgrad Med J. 1969;45:648–654.
- Boland EW. Oxygen in high concentrations for relief of pain: In coronary thrombosis and severe angina pectoris. Jama. 1940;114:1512–1514.
- Ukholkina GB, Kostyanov IY, Kuchkina NV, et al. oxygen therapy in combination with endovascular reperfusion during the first hours of acute myocardial infarction: clinical and laboratory findings. Int J Intervent Cardioangiol. 2005;9:45–51.
- Rawles J, Kenmure A. Controlled trial of oxygen in uncomplicated myocardial infarction. Br Med J. 1976;1:1121–1123.
- Stub D, Smith K, Bernard S, et al. Air versus oxygen in ST-segment elevation myocardial infarction. Circulation. 2015;131:2143–2150
- Nehme Z, Stub D, Bernard S, et al. Effect of supplemental oxygen exposure on myocardial injury in ST-elevation myocardial infarction. Heart. 2016;102:444–451.
- Ranchord AM, Argyle R, Beynon R, et al. High-concentration versus titrated oxygen therapy in ST-elevation myocardial infarction: a pilot randomized controlled trial. Am Heart J. 2012;163:168–175.
- Khoshnood A, Carlsson M, Akbarzadeh M, et al. Effect of oxygen therapy on myocardial salvage in ST elevation myocardial infarction: the randomized SOCCER trial. Eur J Emerg Med. 2016;In press.
- Khoshnood A, Akbarzadeh M, Roijer A, et al. Effects of oxygen therapy on wall motion score index in patients with ST elevation myocardial infarction: results from the randomized controlled SOCCER trial. Echocardiography. 2017;34:1130–1137.
- Boothby WM, Mayo CW, Lovelace WR. One hundred per cent oxygen: indications for its use and methods of its administration. Jama. 1939;113:477–482.
- Russek HI, Regan FD, Naegele CF. One hundred percent oxygen in the treatment of acute myocardial infarction and severe angina pectoris. J Am Med Assoc. 1950;144:373–375.
- Zughaft D, Bhiladvala P, Van Dijkman A, et al. The analgesic effect of oxygen during percutaneous coronary intervention (the OXYPAIN Trial). Acute Cardiac Care. 2013;15:63–68.
- Khoshnood A, Carlsson M, Akbarzadeh M, et al. The effects of oxygen therapy on myocardial salvage in ST elevation myocardial infarction treated with acute percutaneous coronary intervention: the Supplemental Oxygen in Catheterized Coronary Emergency Reperfusion (SOCCER) Study. Cardiology. 2015;132:16–21.
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:1.
- Kelly AM. Does the clinically significant difference in visual analog scale pain scores vary with gender, age, or cause of pain? Acad Emerg Med. 1998;5:1086–1090.
- Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27:117–126.
- Burckhardt CS, Jones KD. Adult measures of pain: the McGill Pain Questionnaire (MPQ), Rheumatoid Arthritis Pain Scale (RAPS), Short‐Form McGill Pain Questionnaire (SF‐MPQ), Verbal Descriptive Scale (VDS), Visual Analog Scale (VAS), and West Haven‐Yale Multidisciplinary Pain Inventory (WHYMPI). Arthritis Care Res. 2003;49:S96–S104.
- Cabello JB, Burls A, Emparanza JI, et al. Oxygen therapy for acute myocardial infarction. Cochrane Library. 2016; CD007160.
- Wilson A, Channer K. Hypoxaemia and supplemental oxygen therapy in the first 24 hours after myocardial infarction: the role of pulse oximetry. J Royal Coll Phys Lond. 1997;31:657–661.
- Everts B, Karlson B, Abdon NJ, et al. A comparison of metoprolol and morphine in the treatment of chest pain in patients with suspected acute myocardial infarction-the MEMO study. J Intern Med. 1999;245:133–141.
- Parodi G. Chest pain relief in patients with acute myocardial infarction. Eur Heart J. 2015;5:277–281.
- Weldon ER, Ariano RE, Grierson RA. Comparison of fentanyl and morphine in the prehospital treatment of ischemic type chest pain. Prehospital Emerg Care. 2016;20:45–51.
- Erlinge D, Götberg M, Lang I, et al. Rapid endovascular catheter core cooling combined with cold saline as an adjunct to percutaneous coronary intervention for the treatment of acute myocardial infarction: the CHILL-MI trial: a randomized controlled study of the use of central venous catheter core cooling combined with cold saline as an adjunct to percutaneous coronary intervention for the treatment of acute myocardial infarction. J Am Coll Cardiol. 2014;63:1857–1865.
- Carlsson M, Ubachs JF, Hedstrom E, et al. Myocardium at risk after acute infarction in humans on cardiac magnetic resonance: quantitative assessment during follow-up and validation with single-photon emission computed tomography. JACC Cardiovasc Imaging. 2009;2:569–576.
- Atar D, Arheden H, Berdeaux A, et al. Effect of intravenous TRO40303 as an adjunct to primary percutaneous coronary intervention for acute ST-elevation myocardial infarction: MITOCARE study results. Eur Heart J. 2014;36:112–119.
- Götberg M, Olivecrona GK, Koul S, et al. A pilot study of rapid cooling by cold saline and endovascular cooling before reperfusion in patients with ST-elevation myocardial infarction. Circ Cardiovasc Interv. 2010;3:400–407.
- Di Lorenzo E, Sauro R, Varricchio A, et al. Randomized comparison of everolimus-eluting stents and sirolimus-eluting stents in patients with ST elevation myocardial infarction: RACES-MI trial. JACC. 2014;7:849–856.