Abstract
Objectives. To ascertain whether extended chest tube drainage decreases the occurrence of late tamponade after cardiac surgery. Design. All patients undergoing cardiac surgery at the Tampere University Heart Hospital, Tampere, Finland, between the 23rd of October 2015 and the 17th of August 2016 were included. The first 260 consecutive patients were treated according to a short drainage protocol, in which the mediastinal chest tubes were removed during the first postoperative day unless producing >50ml/h, and the following 224 consecutive patients by an extended drainage protocol, in which the mediastinal chest tubes were kept at least until the second postoperative day, and thereafter if producing >50ml/4h. The incidence of late tamponade and the length and course of postoperative hospitalization, including the development of complications, were compared. Results. The occurrence of late cardiac tamponade was 8.8% following the short drainage protocol and 3.6% after the extended drainage protocol, p = .018. There were no statistically significant differences in the demographics, medical history, or the procedures performed between the study groups. The in-hospital mortality rate was 3.5%, the stroke rate was 2.1%, and the deep sternal wound infection rate was 1.7%, with no statistically significant differences between the groups. There were no differences in the need for reoperations for bleeding, infection rate, need for pleurocentesis, occurrence of atrial fibrillation, or the length of hospitalization between the groups. Conclusions. Longer mediastinal chest tube drainage after cardiac surgery is associated with a significantly lower incidence of late cardiac tamponade.
Introduction
Pericardial effusions and late cardiac tamponade may complicate patient recovery after cardiac surgery [Citation1–4]. In contrast to early tamponade occurring within the first days postoperatively due to bleeding, late pericardial effusions are thought to be caused by postpericardiotomy syndrome, an inflammatory condition triggered by surgery or other pericardial insult [Citation2,Citation5,Citation6]. Prophylactic therapy with corticosteroids or colchicine has not been shown to reduce the occurrence of late tamponade [Citation7,Citation8]. The incidence of late cardiac tamponade necessitating interventional treatment – either percutaneous procedures or surgical fenestration – ranges from 1.0–6.2% following cardiac operations [Citation1,Citation9–13]. Risk factors include young age, cardiac valve surgery, and anticoagulation [Citation13,Citation14].
We hypothesized that the length of postoperative chest tube drainage impacts the occurrence of late cardiac tamponade. After several years of using a short chest tube protocol, we adopted a more liberal protocol of keeping the chest tubes after cardiac surgery for at least two days. The aim of the study was to evaluate whether our extended chest tube drainage protocol would decrease the occurrence of late cardiac tamponade as compared to our short drainage protocol.
Materials and methods
Study setting
The study was performed as a prospective observational study at Tampere University Heart Hospital, Tampere, Finland, a tertiary referral hospital, and included all consecutive patients operated between the 23rd of October 2015 and the 17th of August 2016. Besides the study intervention, included patients did not take part in any interventional studies, and were otherwise treated according to clinic standards. All adult patients undergoing open heart surgery, including coronary artery bypass grafting, valve surgery, surgery involving the aortic root, ascending aorta, and/or the aortic arch, and combination procedures, as well as redo-operations, were included. If a patient was operated on more than once during the study period, the second operation was included as a new case if performed on during a separate hospital period.
Postoperative chest tube treatment
Two 24Fr mediastinal chest tubes, one placed substernally and one – though subject to surgeon discretion if concomitant inferior wall bypass grafts were present – in the pericardial well, were routinely inserted at the end of each procedure in all patients. Additional pleural drainage with similar chest tubes was performed whenever the pleural space was intentionally or unintentionally opened during the operation, when a pneumothorax was detected intraoperatively, and when excessive pleural effusion was present or anticipated postoperatively. All chest tubes were connected to a single vacuum system set at 10 cm H2O suction level over the study period.
Until and including the 10th of April 2016, the institutional protocol for postoperative chest tube treatment was to remove all mediastinal chest tubes during the morning of the first postoperative day unless producing >50ml/h or leaking air, in which case the removal of said chest tubes were contemplated by the attending surgeon daily afterwards. After and including the 11th of April 2016, mediastinal chest tube drainage was continued at least until the second postoperative day and until the chest tubes produced <50ml/4h in all patients. Postoperative echocardiography was controlled by a cardiologist in all patients, usually on the third postoperative day and in secondary care before hospital discharge, but also whenever needed for clinical decision-making, often several times during the hospitalization. Significant effusions observed in the pericardium were either treated or followed up afterwards. Over the study period, there were no changes in the institutional protocols regarding heparin and protamin use, perioperative cell salvage, anticoagulation, platelet inhibitors, or blood products.
Data collection and analysis
Preoperative patient demographics, medical history, procedural details, length of postoperative hospitalization and mediastinal drainage, the results of relevant laboratory examinations, and clinical data of the postoperative course including the need for reoperations for bleeding within 48 hours, the need for pleurocentesis during the hospitalization, the occurrence of other complications, such as infections or atrial fibrillation, and in-hospital mortality, were recorded. The main study end-point was the occurrence of late cardiac tamponade requiring invasive treatment after the fifth postoperative day and within three months after the hospital discharge following cardiac surgery. The indication for invasive treatment was a pericardial effusion of significant size (>10mm) associated with hemodynamic instability, subjective symptoms such as dyspnea or malaise, signs of cardiac chamber compression in echocardiography, or an effusion significantly increasing in size during follow up. The treatment modality, usually percutaneous drainage or surgical fenestration, was chosen by the attending surgeon.
The study was performed according to the Helsinki Declaration and institutional review board approval was obtained. Statistical analysis was performed using SPSS for Windows version 16.0. Power calculation was set to display the 95% confidence interval and was performed with PowerAndPrecision 4.0 (Biostat, Englewood, NJ). The occurrence of postoperative atrial fibrillation was analyzed in patients without chronic atrial fibrillation preoperatively. Categorical variables were compared using the Chi square and Fisher’s exact tests and the differences between medians in nonparametric variables were compared using the Mann-Whitney U-test and the Kruskal-Wallis H-test. Multivariable analysis including patient demographics, significant comorbidities, type of surgery, and the drainage protocol was performed using binary logistic regression analysis. The association of postoperative weight gain with late postoperative cardiac tamponade was assessed by receiver operating characteristic curve (ROC) analysis. Statistical significance was set at p < 0.05. According to the post-hoc power analysis for the effect size (group means of 0.036 vs. 0.088), standard deviation (0.18 vs. 0.28), patient number (224 and 260), alpha (0.050, 1-tailed), the power for the study was 0.81.
Results
Study population and major outcomes
Altogether 484 consecutive patients were included in the study. Chest tube drainage was performed according to the short protocol in 260 patients and the extended protocol in 224 patients. There were no statistically significant differences in the preoperative characteristics between the study groups and the most common procedures performed were isolated coronary artery bypass and single valve surgeries (). The median actual length of postoperative mediastinal drainage was 1 (IQ range 1–2, range 0–10) day in the short protocol group and 2 (IQ range 2–3, range 1–10) days in the extended protocol group, p < .001 (). There were two cases in the short protocol group in which the chest tubes were accidentally removed by the patient due to confusion or accidental movement on the day of surgery. The major outcomes for the study population were an in-hospital mortality rate of 3.5%, stroke rate of 2.1%, and a deep sternal wound infection rate of 1.7%, with no statistically significant differences between the study groups. Similarly, there were no statistically significant differences in the length of hospitalization, need for pleurocentesis or reoperations for bleeding, or the overall rates of postoperative infections or atrial fibrillation ().
Figure 1. The actual length of mediastinal drainage in study patients when treated according to the short and extended drainage protocol.
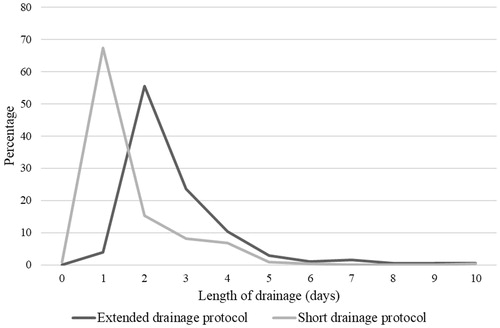
Table 1. Demographics and outcomes.
Late postoperative cardiac tamponade
Late cardiac tamponade occurred in 23 (8.8%) patients with the short drainage protocol vs. eight (3.6%) patients with the extended drainage protocol, p = .018 (). The median delay between surgery and the interventional treatment for late cardiac tamponade was 13 days and did not differ between the study groups. The patients with late tamponade were treated by anterior minithoracotomy and pericardial fenestration in 74%, percutaneous pericardial drainage in 19%, and re-sternotomy or other extended procedures in 6.5% of cases. Of preoperative patient characteristics, coronary disease was associated with a lower incidence of late postoperative pericardial tamponade in the univariable analysis (). The occurrence of late tamponade was low after coronary artery bypass grafting and high after aortic surgery, while multiple valve surgery showed a non-significant trend towards higher incidence (). The need for early reoperations for bleeding or the development of infectious complications were not associated with the occurrence of late cardiac tamponade. The incidence of postoperative atrial fibrillation was, however, significantly higher in patients who subsequently developed late cardiac tamponade, 61% vs. 39%, p = .016, respectively. The patients’ median maximum weight gain within seven days postoperatively varied according to the procedure performed and was 6.2kg after coronary surgery, 7.0kg after single valve surgery, 7.8kg after valve and bypass surgery, 9.1kg after multiple valve surgery, and 6.9kg after aortic surgery, p = .014. The median maximal weight gain was significantly higher in patients who developed late cardiac tamponade when compared to other patients, 10 vs. 6.7kg, p = .001. ROC analysis showed that postoperative weight gain is associated with late postoperative cardiac tamponade (AUC 0.688; S.E. 0.062; p = .001; 95% confidence interval 0.566–0.810, ). In subgroup analysis according to the type of procedure performed, the difference remained statistically significant in patients with single valve surgery, 9.6 vs. 6.8kg, p = .017, and was near-significant in multiple valve surgery, 11.3 vs. 7.8kg, p = .053. The preoperative blood hemoglobin or serum creatinine levels, the lowest blood hemoglobin concentration or the amount of hemoglobin decrease with seven days postoperatively, or the highest serum C-reactive protein concentration within seven days postoperatively were not associated with the development of late cardiac tamponade. In the multivariable analysis including preoperative patient characteristics and the type of surgery planned, the extended drainage protocol remained independently associated with a lower risk of late cardiac tamponade ().
Figure 2. Late cardiac tamponade according to the drainage protocol (SDP = Short drainage protocol, EDP = Extended drainage protocol) in all patients and according to the type of procedure performed. Aortic surgery includes operations for the aortic root, ascending aorta, aortic arch, with or without concomitant coronary and/or valve procedures.
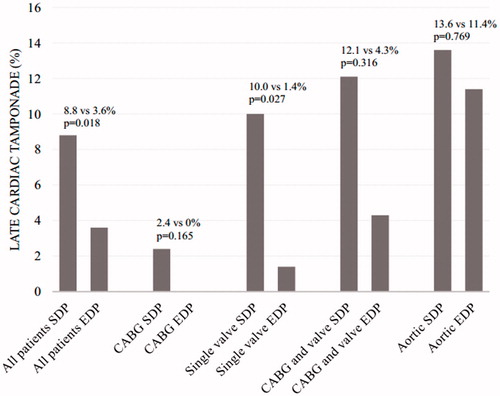
Figure 3. According to ROC analysis, the maximal weight gain during the first seven postoperative days was associated with late cardiac tamponade (AUC 0.688; S.E. 0.062; p = .001; 95% confidence interval 0.566–0.810).
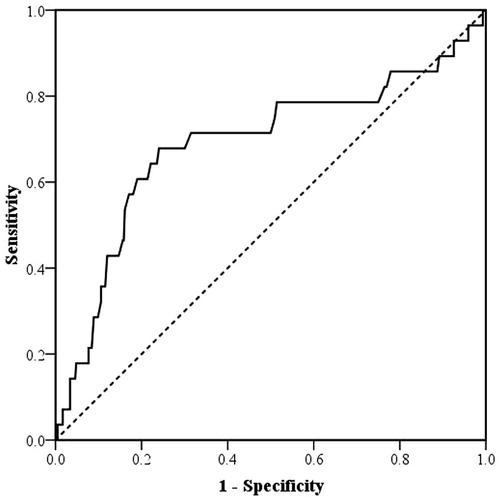
Table 2. The occurrence of late cardiac tamponade according to preoperative factors and the type of surgery.
Table 3. Risk factors for late cardiac tamponade in multivariable analysis. Preoperative factors, the type of surgery, and the drainage protocol were included.
Discussion
Late postoperative cardiac tamponade due to postpericardiotomy syndrome is an infrequent but serious complication of cardiac surgery. In this study, we compared short and long chest tube drainage protocols and report a significantly lower incidence of late cardiac tamponade in patients treated according to an extended drainage protocol. The optimal duration of postoperative chest tube drainage remains controversial in the literature and many authors suggest early removal of chest tubes [Citation15–17], while some studies imply that residual effusions in the pericardium may predispose to the development of late tamponade and therefore longer mediastinal drainage may be beneficial. Posterior pericardiotomy seems to reduce the incidence of late cardiac tamponade, probably owing to increased drainage of mediastinal effusions through the pleural spaces [Citation18]. Even a small amount of pericardial fluid observed during the first days after cardiac surgery is associated with late cardiac tamponade [Citation14] and early chest tube removal may increase its risk [Citation19].
The median duration of mediastinal drainage in patients treated according to the extended protocol in our series was two days. It is tempting to speculate that an even longer chest tube treatment in some patients would have further decreased the occurrence of late tamponade. The risk was lower in patients undergoing coronary surgery when compared to valve, aortic, and combination procedures, as in earlier studies. As complex procedures are becoming more frequent, the prevention of late cardiac tamponade is increasingly important, as is patient follow-up because the diagnosis is often obtained after hospital referral or discharge. The association of late cardiac tamponade with higher postoperative weight gain reflects its association with extended and combination procedures with long perfusion and cross-clamp times, and increased need for transfusions, but may also suggest a separate pathophysiological mechanism that should be addressed in future studies. There was no increase in the overall length of hospitalization, in the rates of postoperative infections or other adverse events in patients treated by the extended drainage protocol, and the chest tubes were well tolerated in most patients. Additional pleural drainage may play a role in the development of late tamponade, but was excluded from this analysis due to the multitude of possible confounding factors. For example, pleural drainage, uni- or bilateral, might have been initiated before, during, or after the operation, for accidental or intentional pleural opening, for actual or anticipated need, for air leakage or effusions, for one or several episodes, and so forth. Importantly, according to the power calculation in comparing the frequency of late tamponade in patients with extended drainage vs. short drainage, 81% of studies were expected to yield a significant effect, rejecting the null hypothesis that the two group means were equal.
The main limitations of the study include the single-center setting, limited statistical power in detecting differences between patient subgroups and in other complications, such as the need for pleurocentesis, and, most importantly, the non-randomized design of the study. While the re-referral of these patients is strongly advocated, it is possible that some patients might have been treated at other hospitals. However, keeping the chest tubes in place until definitive cessation of postoperative fluid secretion led to an outstanding – up to 5.2% – decrease of late cardiac tamponade. The limitations of the study warrant some caution, but the observation clearly merits further investigation.
In conclusion, the occurrence of late cardiac tamponade was significantly lower in patients treated according to an extended drainage protocol after cardiac surgery. Longer drainage was not associated with an increased risk for other complications. Postoperative weight gain seems to be associated with the development of late tamponade.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Pepi M, Muratori M, Barbier P. Pericardial effusion after cardiac surgery: incidence, site, size, and haemodynamic consequences. Br Heart J. 1994;72:327–331.
- Ikäheimo M, Huikuri H, Airaksinen K, et al. Pericardial effusion after cardiac surgery: incidence, relation to the type of surgery, antithrombotic therapy, and early coronary bypass graft patency. Am Heart J. 1988;116:97–102.
- Weitzman L, Tinker W, Kronzon I, et al. The incidence and natural history of pericardial effusion after cardiac surgery-an echocardiographic study. Circulation. 1984;69:506–511.
- Adler Y, Charron P, Imazio M, et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The task force for the diagnosis and management of pericardial diseases of the European Society of Cardiology (ESC) endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2015;36:2921–2964.
- Alraies M, Al Jaroudi W, Shabrang C, et al. Clinical Features associated with adverse events in patients with post-pericardiotomy syndrome following cardiac surgery. Am J Cardiol. 2014;114:1426–1430.
- Lehto J, Gunn J, Karjalainen P, et al. Incidence and risk factors of postpericardiotomy syndrome requiring medical attention: The Finland postpericardiotomy syndrome study. J Thorac Cardiovasc Surg. 2015;149:1324–1329.
- Imazio M, Brucato A, Ferrazzi P, et al. Colchicine for prevention of postpericardiotomy syndrome and postoperative atrial fibrillation: the COPPS-2 randomized clinical trial. JAMA. 2014;312:1016
- Bunge J, van Osch D, Dieleman J, et al. Dexamethasone for the prevention of postpericardiotomy syndrome: A DExamethasone for cardiac surgery substudy. Am Heart J. 2014;168:126–131.
- Meurin P, Weber H, Renaud N, et al. Evolution of the postoperative pericardial effusion after day 15: the problem of the late tamponade. Chest. 2004;125:2182–2187.
- Aksöyek A, Tütün U, Ulus T, et al. Surgical drainage of late cardiac tamponade following open heart surgery. Thorac Cardiovasc Surg. 2005;53:285–290.
- Russo AM, O'Connor WH, Waxman HL. Atypical presentations and echocardiographic findings in patients with cardiac tamponade occurring early and late after cardiac surgery. Chest. 1993;104:71–78.
- Bucekova E, Simkova I, Hulman M. Postpericardiotomy syndrome – post-cardiac injury syndrome. Bratisl Lek Listy. 2012;113:481–485.
- Khan NK, Järvelä KM, Loisa EL, et al. Incidence, presentation and risk factors of late postoperative pericardial effusions requiring invasive treatment after cardiac surgery. Interact Cardiovasc Thorac Surg. 2017;24:835–840.
- You S, Shim C, Hong G-R, et al. Incidence, predictors, and clinical outcomes of postoperative cardiac tamponade in patients undergoing heart valve surgery. PLoS One 2016;11:e0165754.
- Gercekoglu H, Aydin N, Dagdeviren B, et al. Effect of timing of chest tube removal on development of pericardial effusion following cardiac surgery. J Card Surg. 2003;18:217–224.
- Mirmohammad-Sadeghi M, Etesampour A, Gharipour M, et al. Early chest tube removal after coronary artery bypass graft surgery. N Am J Med Sci. 2009;1:1333–1337.
- Moss E, Miller C, Jensen H, et al. A randomized trial of early versus delayed mediastinal drain removal after cardiac surgery using silastic and conventional tubes. Interact Cardiovasc Thorac Surg. 2013;17:110–115.
- Gozdek M, Pawliszak W, Hagner W, et al. Systematic review and meta-analysis of randomized controlled trials assessing safety and efficacy of posterior pericardial drainage in patients undergoing heart surgery. J Thorac Cardiovasc Surg. 2017;153:865–875.
- Andreasen J, Sørensen G, Abrahamsen E, et al. Early chest tube removal following cardiac surgery is associated with pleural and/or pericardial effusions requiring invasive treatment. Eur J Cardiothorac Surg. 2016;49:288–292.
