Abstract
Objectives. Stroke is a common condition after a transient ischemic attack (TIA) or minor ischemic stroke (IS). Adding clopidogrel to aspirin may yield more beneficial outcomes than aspirin mono-therapy; meanwhile, the risk of bleeding in the acute phase remains poorly understood. Therefore, there is increasing emphasis on the risks and benefits of clopidogrel with aspirin compared with aspirin mono-therapy in an effort to treat TIA/IS. Design. We searched several electronic databases, including PubMed, Cochrane, and Embase, to identify eligible randomized controlled trials (RCTs) based on the index words comparing dual-antiplatelet therapy to aspirin mono-therapy for secondary stroke prevention updated to December, 2018. Results. A total of 11 RCTs met our inclusion criteria. The pooled analysis showed that clopidogrel plus aspirin was associated with a trend toward a reduction in recurrent IS (RR = 0.72, 95%CI = 0.65–0.81, p < .001), but not the recurrent stroke rate (RR = 0.81, 95% CI = 0.63‐1.03, p = .09) than aspirin mono-therapy. There were differences in bleeding episodes (RR = 1.81, 95%CI = 1.65–1.99, p < .001), moderate-severe major bleeding (RR = 1.64, 95% CI = 1.24‐2.16, p = .0005), or mild bleeding (RR = 2.25, 95%CI = 1.54–3.31, p < .001) between the study groups. Meanwhile, no benefit of reducing the risk of intracranial hemorrhage with dual-antiplatelet therapy was found in TIA/IS patients (RR = 1.44, 95% CI = 0.95–2.19, p = .09). Conclusions. The addition of clopidogrel to aspirin for patients with TIA or IS appeared to significantly reduce the risk of IS recurrence with a possible increase in the risk of bleeding compared with aspirin alone.
Introduction
Transient ischemic attack (TIA) and acute minor ischemic stroke (IS) are common conditions caused by loss of blood flow and often lead to unstable clinical symptoms. In addition, patients are at higher risk of recurrent stroke in the immediate aftermath of TIA/IS. This may reflect temporary instability of the symptomatic arterial lesion, causing further covert brain infarcts and vascular cognitive impairment [Citation1].
Most of these adverse events occur in the initial 48–72 h after symptom onset and have delayed recovery of neurological functions [Citation2–4].
In acute stroke patients, both neurologic deterioration and recurrent strokes are common events with severe outcomes [Citation5,Citation6]. Given that platelet activation has been shown to play a pivotal role in both arterial thrombogenesis and the pathophysiology of TIA/IS, antiplatelet therapy is accepted as the standard therapy to prevent IS [Citation7].
The role of antiplatelet therapy for secondary stroke prevention has been well reported. Aspirin is the mainstay of antithrombotic therapy in the secondary prevention of non-cardioembolic stroke, including transient ischemic attack (TIA) and IS (IS). According to the previously established trials, due its efficacy, aspirin is generally thought to be the standard antiplatelet therapy among patients with non-cardioembolic stroke [Citation8]. Dual antiplatelet therapy is increasingly being used in ischemic heart disease, but strong evidence for its efficacy in preventing stroke is presently limited. An updated systemic review showed that dual antiplatelet therapy could safely and effectively reduce stroke recurrence and combined vascular events in TIA/IS patients, compared with mono-therapy [Citation9].
Clopidogrel is an ADP-receptor antagonist that has clinical benefit compared with aspirin on both ex vivo platelet aggregation and thrombosis in animal models [Citation10]. Combination treatment of clopidogrel and aspirin taken soon after a minor IS or TIA was shown to reduce the early risk of new stroke without increasing bleeding risk [Citation11,Citation12].
The addition of clopidogrel to aspirin has been shown to decrease the risk of stroke among patients with atrial fibrillation [Citation13] and acute coronary syndromes [Citation14], with several cases described in the recent literature. It is possible that the dual antiplatelet therapy may contribute to increased bleeding [Citation15]. Of note, the risk of bleeding increased as the duration of dual antiplatelet therapy became prolonged [Citation16]. Therefore, the optimal duration of dual antiplatelet therapy for minor stroke or TIA is presently controversial.
To evaluate the optimal duration of dual antiplatelet therapy, we sought to delineate the risks and benefits of clopidogrel with aspirin versus aspirin mono-therapy in TIA/IS patients using data from RCTs.
Materials and methods
Ethical review
Ethics approval was waived because this study did not involve any human participants or animals.
Search strategy
We searched the electronic databases including PubMed, Embase, and Cochrane database from their inception to December 2018 to identify all the eligible studies. The literature search process was performed by two reviewers independently. The following key words were used: ‘aspirin’, ‘clopidogrel’, ‘ischemic stroke’, and ‘transient ischemic attack’. Furthermore, relevant Medical Subject Heading (MeSH) terms were utilized. Literature was also searched using reference lists and materials.
Eligibility criteria
Studies were included in the meta-analysis if they met the following criteria: [Citation1] articles that enrolled patients with IS or TIA; [Citation2] design: randomized controlled trials (RCTs) comparing dual-antiplatelet therapy to aspirin mono-therapy for secondary stroke prevention; [Citation3] studies with data of clinical interest, and RRs (Risk Ratios) with corresponding 95% confidence intervals (CIs) were provided; [Citation4] all publications were available only in English. If duplicated or overlapped data were found in multiple reports, the one with the most complete and latest data was included.
Quality assessment
We used the New- castle–Ottawa Quality assessment scale recommended by The Cochrane Handbook for Systematic Reviews of Interventions. The process was performed by two investigators independently; differences were settled through discussion.
Data extraction
Two investigators independently extracted the following information from each study. Disagreement was resolved through discussion to reach a consensus. From each of the eligible studies, the following information was collected: the trial name; publication year; mean age of the patients; variables related to the interventions; number of male patients; outcome of interest for each group.
Data synthesis and analysis
RRs and their 95%CIs were combined to evaluate the safety and efficacy of dual antiplatelet therapy to aspirin mono-therapy, and the associated outcomes including recurrent stroke, recurrent IS, TIA, bleeding episodes, moderate-severe major bleeding, and mild bleeding.
To assess the heterogeneity of study trial and determine the model for analysis (random-effects model or fixed-effects model), I2 tests and Chi-squared were conducted. [Citation17]. Studies with an I2 ≥ 50% was considered to indicate moderate and high heterogeneity, I2 < 50% was considered to have low heterogeneity, respectively [Citation18]. For studies of low heterogeneity, the fixed-effects model was used. Meanwhile, the pooled RRs were calculated using the randomized-effects model. Results with a p < .05 were considered statistically significant. Statistical analyses were conducted using Review Manager version 5.3 software (Revman; The Cochrane Collaboration Oxford, UK). Findings of our meta-analysis were shown in forest plots.
Results
Overview of literature search and study characteristics
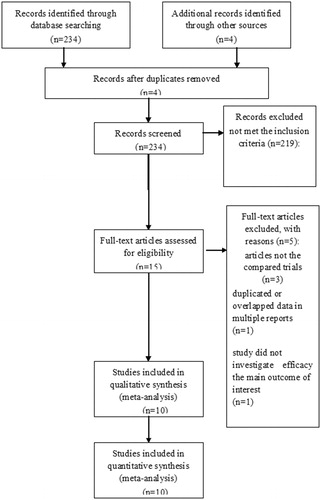
A total of 324 articles were included by the index words. During preliminary screening of the abstracts and titles, 16 publications were evaluated in more detail, but 5 did not meet the inclusion criteria. At last, a total of 11 studies were included. shows the detailed search process.
All included studies in this study were of moderate quality at least. describes the primary characteristics of the eligible studies in more detail.
Table 1. The Primary characteristics of the eligible studies.
Clinical and methodological heterogeneity
Pooled analysis of recurrent stroke between dual-antiplatelet therapy and aspirin Mono-therapy
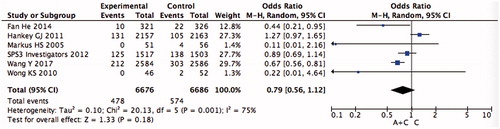
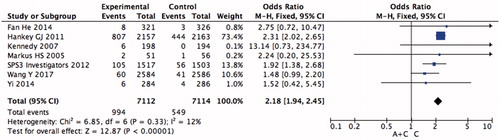
For recurrent stroke, no significant differences between dual-antiplatelet therapy and aspirin mono-therapy were observed (RR = 0.81, 95% CI = 0.63–1.03, p = .09) ().
Pooled analysis of recurrent IS between dual-antiplatelet therapy and aspirin Mono-therapy
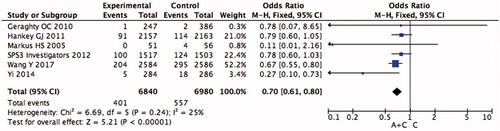
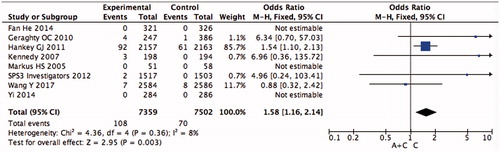
The fixed-effects model was used to pool the recurrent IS data since the heterogeneity across the four studies was not significant. The pooled data showed that the addition of clopidogrel to aspirin significantly reduced the recurrent rate of IS (OR = 0.70, 95%CI = 0.63–0.79, p < .001) than aspirin monotherapy ().
Pooled analysis of TIA between dual-antiplatelet therapy and aspirin Mono-therapy
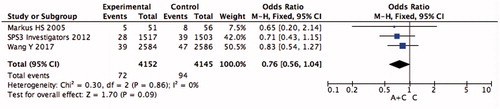
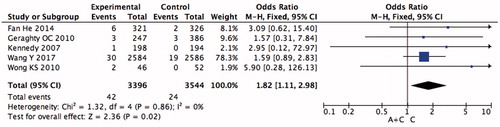
The pooled TIA data did not show advantage of dual-antiplatelet therapy (OR = 0.76, 95%CI = 0.56–1.04, p = .09). In other words, the addition of clopidogrel to aspirin did not reduce the rate of TIA ().
Pooled analysis of bleeding episodes between dual-antiplatelet therapy and aspirin Mono-therapy
Bleeding episode data was available for seven RCTs. The results showed that dual-antiplatelet therapy was associated with increased bleeding episodes versus aspirin mono-therapy (RR = 1.81, 95%CI = 1.65–1.99, p < .001) ().
Pooled analysis of moderate-severe major bleeding between dual-antiplatelet therapy and aspirin Mono-therapy
For TIA/IS, significant differences between dual-antiplatelet therapy and aspirin mono-therapy were observed in moderate-severe major bleeding (RR = 1.64, 95% CI = 1.24–2.16, p < .001) ().
Pooled analysis of mild bleeding between dual-antiplatelet therapy and aspirin Mono-therapy
The pooled data on mild bleeding of five studies showed that dual-antiplatelet therapy had a mild bleeding disadvantage (RR = 2.25, 95%CI = 1.54–3.31, p < .001) compared with aspirin mono-therapy (). This result indicated that the addition of clopidogrel to aspirin significantly increased the risk of mild bleeding of TIA/IS patients.
Pooled analysis of intracranial hemorrhage between dual-antiplatelet therapy and aspirin Mono-therapy
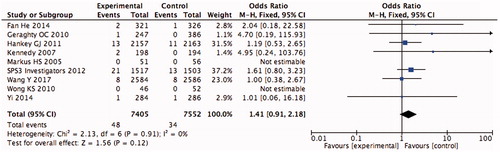
In the analysis of intracranial hemorrhage, nine studies were included, and the data are shown in . Dual-antiplatelet therapy did not demonstrate any benefit in intracranial hemorrhage in TIA/IS patients (RR = 1.44, 95% CI = 0.95‐2.19, p = .09).
Discussion
Stroke is a serious condition with consequent high morbidity and mortality, making early prevention of relevant events a top priority. Of note, patients with an IS or a TIA are at a higher stroke recurrence rate [Citation27]. Treatment with antiplatelet regimens is the current standard therapy for these patients. Many researchers have focused on its role in the secondary prevention of TIA/IS [Citation28–30], but difficulties exist concerning the selection of best treatment from multiple treatment options.
Aspirin and clopidogrel synergistically inhibit platelet aggregation [Citation31], and such combination of aspirin and clopidogrel dual therapy has decreased the risk of recurrent ischemic events in patients with acute coronary syndrome [Citation10,Citation14]. The results of CARESS found that the addition of clopidogrel to aspirin reduced large-vessel atherosclerotic stroke [Citation19]. The FASTER [Citation23] trial demonstrated significant reduction of early recurrent stroke, which was associated with the combination of aspirin and clopidogrel compared with aspirin alone. However, the recent POINT trial suggested that no additional benefit was found from dual antiplatelet therapy with aspirin and clopidogrel versus clopidogrel alone in preventing recurrent ischemic events [Citation27].
In our study, we found that the addition of clopidogrel to aspirin was superior in significantly decreasing the risk of ischemic recurrent stroke. There were several potential explanations for the reduction of stroke in the clopidogrel-aspirin group. According to Yi’s study [Citation24], they found that arachidonic acid (AA)-induced or adenosine diphosphate (ADP)-induced platelet aggregation and platelet-leukocyte aggregates on initial admission were higher in patients who later suffer neurologic deterioration or recurrent stroke than in patients who did not experienced these problems. The mentioned studies have implications that platelet aggregation and platelet-leukocyte aggregates may be associated with the pathogenesis of neurologic deterioration or recurrent stroke after acute large-artery atherosclerosis stroke. Furthermore, the number, rather than type, of antiplatelet drugs appears tobe more susceptible to reduce stroke recurrence. Different anti-platelet combinations have synergistic effects based on different antiplatelet mechanisms. Therefore, combined antiplatelet therapy may reduce the incidence of recurrent IS or neurologic deterioration. On the other hand, in the acute stage of TIA/IS, dual antiplatelet therapy reduces the presence of microembolic signals in patients with predominantly intracranial symptomatic stenosis, compared with monotherapy alone [Citation32].
Antiplatelet treatment is a double-edged sword: high platelet inhibition is effective in decreasing the risk of recurrent ischemic events, but the risk of bleeding remains uncertain [Citation33].The risk of bleeding was the primary safety concern when combination treatment of clopidogrel and aspirin were administered in clinical practice. It is always important to balance the conflicting effect of decreasing stroke recurrence and increasing major bleeding events risk. In the SPS3 trial [Citation1], treatment with aspirin alone significantly increased the risk of bleeding. However, in the EXPRESS study [Citation25], the use of aspirin plus clopidogrel in high-risk patients decreased early recurrent stroke by 80% without increasing bleeding-related adverse events. Our observation showed favorable treatment effect of potent dual antiplatelet therapy immediately after TIA and ischemic stroke with increasing the risk of bleeding.
Concerns exist because older age, history of antiplatelet agent use and presentation of stroke as qualifying event (vs. TIA) [Citation34] and duration of antiplatelet treatment could be other strong indicators of increased risk of bleeding for dual antiplatelet therapy. The outcomes of the Management of Atherothrombosis with Clopidogrel in high-risk Patients (MATCH) trial showed that bleeding complications of clopidogrel-aspirin were constant over time and a time window (approximately 3 months) existed at which risk outweighed benefit in high-risk patients with IS or TIA [Citation28]. The use of a loading dose has also been reported to lead to more rapid inhibition of platelet aggregation with an antithrombotic effect apparent within 90 min and which became maximal within 6 h [Citation35], and higher doses of aspirin could be less efficacious than lower doses to prevent vascular events [Citation36].
Limitations
In the present systematic analysis of RCTs, there were several limitations that should not be ignored. First, the combined influence of multiple factors existed, such as the limitation of the study-level meta-analysis due to lack of patient-level data. Clinical heterogeneity among studies should be taken into consideration in the interpretation of our findings, even though all the included studies were RCTs. Second, subgroup analysis of important indicators of increased risk in the two cohorts was restricted because patients with high-risk might be more susceptible to complications, which limited relevant subgroup data from literature. Therefore, analyses from important indicators of increased risk data on subtype, such as the use of a loading dose and different stroke subtypes, were not done in the present analysis.
Conclusion
Moderate evidence has been gathered in the present study that aspirin plus clopidogrel is superior to monotherapy in reducing IS recurrence, but increasing the bleeding rate. Considering the heterogeneity of stroke and loading dose due to differences from trials, to examine the effect of therapies on different stroke subtypes and loading dose is strongly needed. More high-quality studies with further data on the balance of those risks and larger RCTs are required to confirm the effectiveness and safety of antiplatelet therapy in an effort to treat patients with recent TIA or IS.
Ethics approval
Ethics approval was waived because this study does not involve any human participants or animals.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Benavente OR, Hart RG, McClure LA, et al. Effects of clopidogrel added to aspirin in patients with recent lacunar stroke. N Engl J Med. 2012;367:817–825.
- Johnston SC, Gress DR, Browner WS, et al. Short-term prognosis after emergency department diagnosis of TIA. JAMA 2000;284:2901–2906.
- Lovett JK, Dennis MS, Sandercock PA, et al. Very early risk of stroke after a first transient ischemic attack. Stroke 2003;34:e138–40.
- Coull AJ, Lovett JK, Rothwell PM, et al. Population based study of early risk of stroke after transient ischaemic attack or minor stroke: implications for public education and organisation of services. Bmj. 2004;328:326
- Alawneh JA, Moustafa RR, Baron JC. Hemodynamic factors and perfusion abnormalities in early neurological deterioration. Stroke 2009;40:e443–50.
- Nolte CH, Albach FN, Heuschmann PU, et al. Silent new DWI lesions within the first week after stroke. Cerebrovasc Dis. 2012;33:248–254.
- Lavallee PC, Labreuche J, Faille D, et al. Circulating markers of endothelial dysfunction and platelet activation in patients with severe symptomatic cerebral small vessel disease. Cerebrovasc Dis. 2013;36:131–138.
- Furie KL, Kasner SE, Adams RJ, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2011;42:227–276.
- Geeganage CM, Diener HC, Algra A, et al. Dual or mono antiplatelet therapy for patients with acute ischemic stroke or transient ischemic attack: systematic review and meta-analysis of randomized controlled trials. Stroke 2012;43:1058–1066.
- Herbert JM, Dol F, Bernat A, et al. The antiaggregating and antithrombotic activity of clopidogrel is potentiated by aspirin in several experimental models in the rabbit. Thromb Haemost. 1988;80:512–518.
- Wang Y, Wang Y, Zhao X, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med. 2013;369:11–19.
- Wang Y, Pan Y, Zhao X, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack (CHANCE) trial: one-year outcomes. Circulation 2015;132:40–46.
- Connolly SJ, Pogue J, Hart RG, et al. Effect of clopidogrel added to aspirin in patients with atrial fibrillation. N Engl J Med. 2009;360:2066–2078.
- Yusuf S, Zhao F, Mehta SR, et al. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 2001;345:494–502.
- Usman MH, Notaro LA, Nagarakanti R, et al. Combination antiplatelet therapy for secondary stroke prevention: enhanced efficacy or double trouble?. Am J Cardiol. 2009;103:1107–1112.
- Ge F, Lin H, Liu Y, et al. Dual antiplatelet therapy after stroke or transient ischaemic attack - how long to treat? The duration of aspirin plus clopidogrel in stroke or transient ischaemic attack: a systematic review and meta-analysis. Eur J Neurol. 2016;23:1051–1057.
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Statist Med. 2002;21:1539–1558.
- Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. Bmj. 2003;327:557–560.
- Markus HS, Droste DW, Kaps M, et al. Dual antiplatelet therapy with clopidogrel and aspirin in symptomatic carotid stenosis evaluated using doppler embolic signal detection: the Clopidogrel and Aspirin for Reduction of Emboli in Symptomatic Carotid Stenosis (CARESS) trial. Circulation 2005;111:2233–2240.
- Pan Y, Jing J, Chen W, et al. Risks and benefits of clopidogrel-aspirin in minor stroke or TIA: time course analysis of CHANCE. Neurology 2017;88:1906–1911.
- Wong KS, Chen C, Fu J, et al. Clopidogrel plus aspirin versus aspirin alone for reducing embolisation in patients with acute symptomatic cerebral or carotid artery stenosis (CLAIR study): a randomised, open-label, blinded-endpoint trial. Lancet Neurol. 2010;9:489–497.
- He F, Xia C, Zhang JH, et al. Clopidogrel plus aspirin versus aspirin alone for preventing early neurological deterioration in patients with acute ischemic stroke. J ClinNeurosci. 2015;22:83–86.
- Kennedy J, Hill MD, Ryckborst KJ, et al. Fast assessment of stroke and transient ischaemic attack to prevent early recurrence (FASTER): a randomised controlled pilot trial. Lancet Neurol.2007;6:961–969.
- Yi X, Lin J, Wang C, et al. A comparative study of dual versus monoantiplatelet therapy in patients with acute large-artery atherosclerosis stroke. J Stroke Cerebrovasc Dis.2014;23:1975–1981.
- Geraghty OC, Kennedy J, Chandratheva A, et al. Preliminary evidence of a high risk of bleeding on aspirin plus clopidogrel in aspirin-naïve patients in the acute phase after TIA or minor ischaemic stroke . Cerebrovasc Dis. 2010;29:460–467.
- Hankey GJ, Johnston SC, Easton JD, et al. Effect of clopidogrel plus ASA vs. ASA early after TIA and ischaemic stroke: a substudy of the CHARISMA trial. Int J Stroke. 2011;6:3–9.
- Johnston SC, Easton JD, Farrant M, et al. Clinical research collaboration, neurological emergencies treatment trials network, and the POINT investigators. Clopidogrel and Aspirin in acute ischemic stroke and high-risk TIA. N Engl J Med. 2018;379:215–225.
- Dhamoon MS, Sciacca RR, Rundek T, et al. Recurrent stroke and cardiac risks after first ischemic stroke: the Northern Manhattan Study. Neurology 2006;66:641–646.
- Diener HC, Bogousslavsky J, Brass LM, et al. Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial. Lancet. 2004;364:331–337.
- Sacco RL, Diener HC, Yusuf S, et al. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med. 2008;359:1238–1251.
- Shindoh J, D Tzeng C-W, Vauthey J-N. Portal vein embolization for hepatocellular carcinoma. Liver Cancer. 2012;1:159–167.
- Steinhubl SR, Berger PB, Mann JT. III,. Early and sustained dual oral anti- platelet therapy following percutaneous coronary intervention: a randomized controlled trial. JAMA 2002;288:2411–2420.
- Esagunde RU, Wong KS, Lee MP, et al. Efficacy of dual antiplatelet therapy in cerebrovascular disease as demonstrated by a decline in microembolic signals. A report of eight cases. Cerebrovasc Dis. 2006;21:242–246.
- Ferreiro JL, Sibbing D, Angiolillo DJ. Platelet function testing and risk of bleeding complications. Thromb Haemost. 2010;103:1128–1135.
- Wang D, Gui L, Dong Y, et al. Dual antiplatelet therapy may increase the risk of non-intracranial haemorrhage in patients with minor strokes: a subgroup analysis of the CHANCE trial. Stroke Vasc Neurol. 2016;1:29–36.
- Cadroy Y, Bossavy JP, Thalamas C, et al. Early potent antithrombotic effect with combined aspirin and a loading dose of clopidogrel on experimental arterial thrombogenesis in humans. Circulation 2000;101:2823–2828.