Abstract
Objectives: Osteocalcin (OC) appears to be involved in the regulation of glucose and fat metabolism. We aimed to determine the association between OC and epicardial adipose tissue (EAT) in premenopausal obese women. Design: The study included 73 premenopausal obese women and 55 non-obese women. Echocardiographic examination was performed to measure EAT. Serum OC levels were measured by chemiluminescence immunoassay. Results: OC levels were significantly lower in obese women than controls (18.26 ± 5.27 vs. 22.53 ± 6.84 ng/ml, p < .001). EAT thickness was higher in obese women than controls (5.19 ± 0.73 vs. 3.25 ± 1.35 mm, p < .001). In obese women, OC was positively correlated with EAT thickness (p = .043; r = 0.326). There was no correlation in controls. Conclusions: Premenopausal obese women had lower OC levels and thicker EAT than controls. There was a weak positive correlation between OC and EAT in premenopausal obese women. This potential cross talk between bone metabolism and EAT could play a role in the development of atherosclerosis in obesity.
Introduction
Obesity may be associated with increased cardiovascular morbidity and mortality [Citation1]. Previous studies have demonstrated an association between osteocalcin (OC), glucose metabolism, and fat mass [Citation2–4]. In patients with type 2 diabetes mellitus, OC correlated inversely with percentage trunk fat and with hemoglobin A1c [Citation4]. Kindblom et al. have shown that OC level was inversely related to plasma glucose level and fat mass in elderly nondiabetic persons [Citation3]. These results support a regulatory role of the skeleton on glucose and energy homeostasis, which appears to be mediated by OC. Epicardial adipose tissue (EAT) is described as an organ involved in the production of several inflammatory cytokines [Citation5]. There is mounting evidence suggesting a connection between vascular remodeling and bone metabolism [Citation6,Citation7]. We aimed to investigate the relationship between OC and EAT in premenopausal obese women. Parts of the results of this study have been previously reported in form of an abstract [Citation8].
Methods
73 obese premenopausal women and 55 women with normal body mass index (BMI) participated. Exclusion criteria included diagnosis of polycystic ovary syndrome, regular exercise, pregnancy, current breast feeding, any disorders of glucose or lipid metabolism, the use of medication that could affect body composition or glucose metabolism, current use of tobacco. This study was approved by the Medical Ethics Committee of the the participating university (the registry number 60116787-020/41760) and was conducted in accordance with the Helsinki Declaration. Informed consent was obtained from all participants. Obesity was defined as BMI >30 kg m−2. BMI was calculated as weight (kg) divided by height (m)Citation2. Waist circumference (WC) was measured midway between the lowest rib and the iliac crest while the participants were standing upright. Complete echocardiography was performed from the standard views using Vivid 7, GE-Vingmed, Horten, Norway according to the previous criteria [Citation9]. All results were analyzed by 1 cardiologist. EAT was identified as the echo-free space or layer anterior to the right ventricle between the outer wall of the myocardium and the visceral layer of the pericardium, and its thickness was measured perpendicularly on the free wall of the right ventricle at end-systole in 3 cardiac cycles from the parasternal long-axis and short-axis views which allow the most accurate measurement of EAT on the right ventricle [Citation10]. The average value of 3 cardiac cycles from each view was taken into account. Fasting insulin was measured by chemiluminescent immunoassay. To determine the state of insulin resistance using the cut-off value of 2.7, the insulin-resistance homeostasis model assessment (HOMA) index was calculated using the following formula: (fasting plasma glucose, mmol/L × fasting plasma insülin, mU/L)/22.5 [Citation11]. Serum OC levels were measured by chemiluminescence immunoassay. Independent samples t test or Mann Whitney U test, where appropriate was used for intergroup comparisons. Correlation between continuous variables was analysed with Spearman Correlation Coefficient. Multiple linear regression analysis was used to identify the factors associated with OC. The level of statistical significance was set at p < .05. A power analysis was performed before study initiation. We targeted a moderate effect size (d = 0.6) to estimate a sample size for the present study and we found that a total number of 98 participants (49 patients and 49 controls) would result in 90% power with 0.05 two sided alpha probability error. We included 128 participants (73 patients and 55 controls) in the present study. The power analysis performed after the study showed that our results reached 96% power with 0.05 two sided alpha probability error and the effect size was d = 0.69 for osteocalcin.
Results
Anthropometric and laboratory characteristics of 128 subjects are shown in . OC levels were lower and EAT thickness was higher in premenopausal obese women. We divided premenopausal obese women based on HOMA insulin resistance (IR) and OC levels were similar in those with and without IR. There were no significant correlations between OC and biochemical and hormonal parameters. OC was not correlated with BMI and waist circumference. OC was positively correlated with EAT in premenopausal obese women (). There was no correlation between OC and EAT in normal weight women. Elevated OC levels were not associated with increased EAT thickness (p = .065, standardized beta: 0.298). Intra-observer coefficient of variation was less than 5% for all echocardiographic measurements. Intra-observer coefficient of variation of EAT measurement was less than 10%. Intraassay coefficient of variation was less than 5% and interassay coefficient of variation was less than 10% for OC measurements.
Figure 1. Correlation between osteocalcin and epicardial adipose tissue in premenopausal obese women (p = .043; r = 0.326).
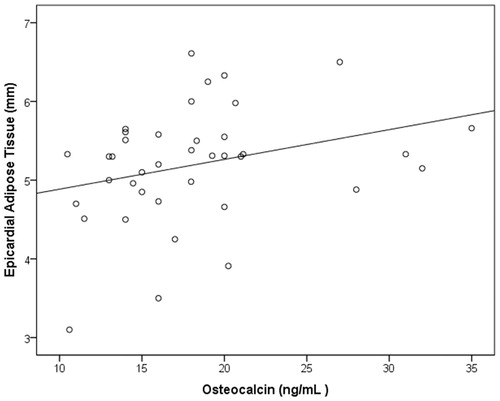
Table 1. Anthropometric and laboratory characteristics of subjects (n = 128).
Discussion
The main findings of this study are: (1) OC levels were lower; (2) EAT thickness was higher; and (3) OC was positively correlated with EAT in premenopausal obese women. The positive correlation between OC and EAT may show that skeleton, via release of OC, may play a role in relation to the metabolic phenotype. Additionally, we speculate that this correlation might link between bone metabolism and atherosclerosis and thus, potentially increased cardioavascular risk in obesity. In a recent study, EAT was associated with subclinical atherosclerosis after adjusting for age, sex, smoking, and hypertension. Adjustment for markers for dyslipidemia and hyperglycemia substantially weakened these associations suggesting that the effect of EAT on atherosclerosis could be mostly mediated by these cardiovascular risk factors [Citation12]. EAT assessment is a reliable predictor of cardiovascular risk, independent of traditional risk factors and other fat depots [Citation13]. Dysfunctional EAT may be linked to adverse cardiac events, early plaque formation, metabolic abnormality, and inflammation [Citation14]. We demonstrated lower OC levels in premenopausal obese women. A case-control study of 61 patients with coronary artery bypass grafting (CABG) with 61 age- and gender-matched controls, patients with CABG had significantly lower OC before and after adjusting for metabolic risk factors and renal function [Citation15]. In a cohort of 774 elderly Caucasian men, higher baseline OC was associated with lower 10-year all-cause mortality [Citation16]. In a study of 3542 men followed for a median of 5.2 years, mortality was lowest in men with OC in the second quintile, and higher in men with OC in the lowest and highest quintiles [Citation17]. These results suggest that OC may either be a biomarker for or a contributory factor to the risk of cardiovascular disease. Several limitations should be mentioned: this study was a single-center one; we enrolled only low-risk premenopausal obese women; we did not conduct studies of inflammatory markers or imaging studies of atherosclerosis to assess the relationship between EAT and OC; we did not evaluate the presence of vascular disease. Echocardiography provides a simple, inexpensive and readily available means of assessing EAT thickness; however, it has a high dependence on the observer’s experience, it may not reflect accurately the whole quantity of the EAT due to its two-dimensional nature. In conclusion, we demonstrate for the first time a weak correlation between OC and EAT. Elevated OC levels were associated with increased EAT thickness. This potential interaction may have an impact on the development and progression of atherosclerosis.
Disclosure statement
No potential conflict of interest was reported by the authors. The authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their interpretations. Parts of the results of this study have been previously presented as a poster at ESC 2017. Reprints will not be available upon acceptance.
Additional information
Funding
References
- Orhan AL, Uslu N, Dayi SU, et al. Effects of isolated obesity on left and right ventricular function: a tissue Doppler and strain rate imaging study. Echocardiography. 2010;27:236–243.
- Kanazawa I, Yamaguchi T, Yamamoto M, et al. Serum osteocalcin level is associated with glucose metabolism and atherosclerosis parameters in type 2 diabetes mellitus. J Clin Endocrinol Metab. 2009;94:45–49.
- Kindblom JM, Ohlsson C, Ljunggren O, et al. Plasma osteocalcin is inversely related to fat mass and plasma glucose in elderly Swedish men. J Bone Miner Res. 2009;24:785–791.
- Kanazawa I, Yamaguchi T, Yamauchi M, et al. Serum undercarboxylated osteocalcin was inversely associated with plasma glucose level and fat mass intype 2 diabetes mellitus. Osteoporos Int. 2011;22:187–194.
- Shimabukuro M. Cardiac adiposity and global cardiometabolic risk: new concept and clinical implication. Circ J. 2009;73:27–34.
- Cejka D, Weber M, Diarra D, et al. Inverse association between bone microarchitecture assessed by HR-pQCT and coronary artery calcification in patients with end-stage renal disease. Bone. 2014;64:33–38.
- Freedman BI, Register TC. Effect of race and genetics on vitamin D metabolism, bone and vascular health. Nat Rev Nephrol. 2012;8:459–466.
- Yaylali YT, Fidan-Yaylali G, Dedeoglu O, et al. The association between osteocalcin and epicardial fat tissue in obesity. Eur Heart J. 2017;38:ehx504.P4409.
- Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39.
- Iacobellis G, Assael F, Ribaudo MC, et al. Epicardial fat from echocardiography: a new method for visceral adipose tissue prediction. Obes Res. 2003;11:304–310.
- Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419.
- Ei Ei Khaing N, Shyong TE, Lee J, et al. Epicardial and visceral adipose tissue in relation to subclinical atherosclerosis in a Chinese population. PLOS One. . 2018;13:e0196328.
- Nagy E, Jermendy LA, Merkely B, et al. Clinical importance of epicardial adipose tissue. Arch Med Sci. 2017;13:864–874.
- Goeller M, Achenbach S, Marwan M, et al. Epicardial adipose tissue density and volume are related to subclinical atherosclerosis, inflammation and major adverse cardiac events in asymptomatic subjects. J Cardiovasc Comput Tomogr. 2018;12:67–73.
- Kim KM, Lim S, Moon JH, et al. Lower uncarboxylated osteocalcin and higher sclerostin levels are significantly associated with coronary artery disease. Bone. 2016;83:178–183.
- Confavreux CB, Szulc P, Casey R, et al. Higher serum osteocalcin is associated with lower abdominal aortic calcification progression and longer 10-year survival in elderly men of the MINOS cohort. J Clin Endocrinol Metab. 2013;98:1084–1092.
- Yeap BB, Chubb SA, Flicker L, et al. Associations of total osteocalcin with all cause and cardiovascular mortality in older men. The health in men study. Osteoporos Int. 2012;23:599–606.
