Abstract
Objectives: To compare the clinical outcome of cardiac resynchronization therapy (CRT) in patients receiving a bipolar left ventricular (LV) lead with a side helix for active fixation to the outcome in patients receiving a quadripolar passive fixation LV lead.
Design: Sixty-two patients (mean age 72 ± 11 years) were blindly and randomly assigned to the active fixation bipolar lead group (n = 31) or to the quadripolar lead group (n= 31). The LV leads were targeted to the basal LV segment in a vein concordant to the LV segment with the latest mechanical contraction chosen on the basis of preoperative radial strain (RS) echocardiography.
Results: At the 6-month follow-up (FU), the reduction in LV end-systolic volume and LV reverse remodelling responder rate, defined as LV end-systolic volume reduction >15%, was 77% in the active fixation group and 83% in the quadripolar group, which was not significantly different. At the 12-month FU, the LV ejection fraction (LVEF) did not differ between the groups. There were no significant differences between the two groups in changes in New York Heart Association (NYHA) functional class or Minnesota Living with Heart Failure Questionnaire score. The occurrence of phrenic nerve stimulation (PNS) was 19% in the active fixation group versus 10% in the quadripolar group (p=.30), and all cases were resolved by reprogramming the device. All patients were alive at the 12-month FU. There was no device infection.
Conclusions: There were no significant differences between the active fixation group of patients and the quadripolar group of patients concerning improvement in echocardiographic parameters or clinical symptoms.
ClinicalTrials.gov number, NCT04632472
Introduction
Cardiac resynchronization therapy (CRT) improves heart failure symptoms and reduces hospitalization and total mortality in selected patients [Citation1]. Resynchronization reverses the adverse process of ventricular remodelling when combined with medical therapy in selected patients with heart failure [Citation2]. The clinical response to CRT is difficult to predict, and the position of the left ventricular (LV) lead significantly influences the outcome [Citation3]. The achievement of an advantageous position of the LV lead depends on the lead characteristics. A favourable LV lead should have excellent trackability along coronary veins in addition to a low rate of lead dislocations and a low pacing capture threshold (PCT). Quadripolar LV leads allow multiple pacing configurations and demonstrate evidence of better outcomes; they have been proven superior to passive bipolar LV leads due to a lower rate of phrenic nerve stimulation (PNS) and fewer lead dislocations [Citation4–7]. Adding a helix for active fixation of a bipolar lead enhances lead stability [Citation8]. Whether active fixation bipolar leads may surpass quadripolar leads is not yet known. The aim of our study was to analyse differences between active fixation bipolar leads and passive quadripolar leads concerning the degree of reverse remodelling and heart failure symptoms. We also investigated factors that may influence the clinical outcome of the cohort.
Methods
Patients and study protocol
This prospective single-centre randomized and blinded trial included patients scheduled for CRT device implantation. From February 2016 until November 2017, 62 consecutive patients were suitable for enrolment in the study. They all had indications for CRT according to the 2016 European Society of Cardiology heart failure guidelines. The regional committee for medical and health research ethics approved the study (Reference 2015/1507), and written informed consent was obtained from all patients. ClinicalTrials.gov number, NCT04632472. Patients were assigned to receive either an active fixation bipolar lead or a quadripolar passive LV lead. Prior to randomization, the patients were stratified into two cohorts based on whether they received a CRT device with a defibrillator (CRT-D) or without defibrillator (CRT-P). Inclusion criteria were symptomatic heart failure in New York Heart Association (NYHA) functional class II or III or ambulatory class IV. Further, left bundle branch block (LBBB) with a QRS duration ≥120 ms or non-LBBB with a QRS duration ≥150 ms as well as an LV ejection fraction (LVEF) ≤35% measured by echocardiography were mandatory. The mean age of the study population was 72 ± 11 years, and 27% were females. The mean LVEF was 25.7 ± 6%, and the mean QRS duration was 163 ± 19 ms. The NYHA functional classes of the patients were class II (n = 22), class III (n = 37), and class IV (n = 3). Ninety-five percent of patients had LBBB. Aetiology was considered to be ischaemic if they had a history of myocardial infarction or prior coronary artery revascularization. There were no significant differences in the baseline clinical characteristics between the two groups of patients (). A CRT-D device was implanted in 67% of the patients. All patients were treated for heart failure with the currently available optimal medical treatment ().
Table 1. Baseline characteristics.
Echocardiographic imaging
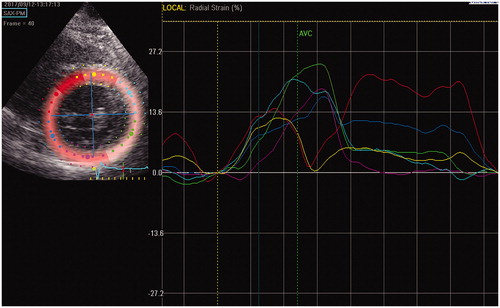
As published previously from our centre, transthoracic echocardiography including 2D speckle-tracking radial strain (ST-RS) measurement was performed prior to the implantation procedures (Citation9, Citation10]. The echocardiographic measurements were repeated at follow-up (FU) after 6 and 12 months of CRT. The GE Vivid E9 echomachine was used for all measurements, and all images were processed offline by using EchoPac 202 (GE Medical System, Vingmed Ultrasound, Horten, Norway). LV volumes and the biplane Simpson LVEF were calculated from apical four- and two-chamber images, and LV end-diastolic dimension was measured. Intraventricular dyssynchrony was assessed by using ST-RS echocardiography from 2D images in the mid-LV parasternal short-axis view with a frame rate ≥70 Hz. Time-strain curves were generated for the different LV segments (). We excluded LV segments with strain <10% to avoid LV lead placement in areas with transmural scars. The times from Q-wave onset to the peak RS in the anterior, lateral, and posterior LV segments were calculated as a mean of five consecutive cardiac cycles. The latest contracting segment of the anterior, lateral, and posterior LV segments was determined from these analyses. If the peak RS for the onset of contraction for two LV segments was separated by ≤10 ms, the segment between them was judged as the latest segment. Consequently, a 5-segment model was established, and the target segment for the LV lead could be identified as the anterior, anterolateral, lateral, posterolateral, or posterior segment. The segments neighbouring the target segment were classified as adjacent segments, and the other segments were classified as remote segments.
Figure 1. Echocardiographic imaging in parasternal short-axis view. The left ventricle (LV) is divided into 6 equal colour coded segments. The right hand picture demonstrates radial strain time curves. The septal LV segment (yellow dots and line) has early mechanical activation. The lateral LV segment (green) and the posterior LV segment (purple) demonstrates late and almost simultaneous timed mechanical activation which is significantly delayed compared to that of the anterior segment (blue). Since the mechanical activation of the lateral and the posterior LV segment are separated by less than 10 ms, the posterolateral segment between them is selected as target LV segment for placement of the LV lead (10). AVC=aortic valve closure.
Technique for implantation
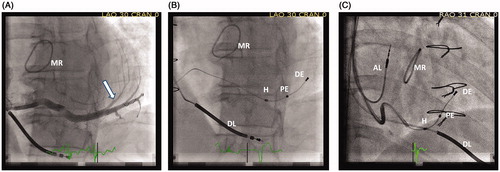
Two experienced implanters performed all implantations. The right ventricular leads were placed in the apex of the right ventricle, and the right atrial leads were placed in the appendage of the right atrium. After the cannulation of the coronary sinus, an occlusive venogram was obtained in the 30–40° left anterior oblique (LAO) view and the 30° right anterior oblique (RAO) view (). In the LAO view, the LV was divided into five equal segments, corresponding to the 5-segment division acquired in the preoperative RS echocardiographic measurement, and a vein located in the target segment was selected. In the absence of a suitable vein in that segment, a vein in an adjacent segment was used, and in rare cases, the lead had to be placed in a remote segment [Citation9]. A long-axis position for the stimulating electrode as close as possible to the coronary sinus entry was preferred. The leads were delivered over the wire through standard coronary sinus cannulation catheters. In 72% of the patients, a subselection catheter was used. For the active fixation lead, a J-shaped stylet was used to apply a lateral force on the helix towards the vein wall, and the lead was fixated to the vein wall by clockwise rotation. The lead stability was tested by pushing and pulling the lead. The time intervals for LV-Q, RVsense-to LVsense, and RVpace-LVsense were recorded before removing the catheters. The leads were connected to a CRT-D generator (Medtronic, Minneapolis, MN) or a CRT-P generator (Abbot, Lake Bluff, IL). The final locations of the lead were recorded in anteroposterior (AP), LAO, and RAO views. Later, with information about the target location blinded, the stored fluoroscopic recordings were processed offline. Thus, the exact position for all LV electrodes was reassessed concerning their short-axis segment location and distances from CS. Final LV lead positions in the target LV segment or in an adjacent LV segment were categorized as concordant lead placements. Subsequently, a lead position was categorized as a disconcordant placement when the position was ≥2 LV segments from the target LV segment.
Figure 2. A) Fluoroscopic left anterior oblique view (LAO) demonstrates selective venogram of a posterolateral vein. The arrow indicates the target location for the left ventricular (LV) lead.B) LAO view of the final lead placement of an active fixation bipolar LV lead. The helix(H) is fixated proximal in the target vein. The proximal electrode (PE) is located in the basal third of the LV long- axis and is selected as the stimulating cathodal electrode. The distal electrode (DE) is in the mid third of the LV long-axis. The high voltage right ventricular defibrillator lead (DL) is located in the apex of the right ventricle.C) Demonstrate the final LV lead placement in right anterior oblique view (RAO). MR=mitral valve ring; AL=pacing lead located in the right atrial appendage.
Lead characteristics
The active fixation lead was a bipolar steroid eluting lead (Attain Stability model 20066/4796, Medtronic Inc., Minneapolis, MN). The lead body was 3.9 French (Fr) proximal and 3.4 Fr distal with a 21 mm electrode separation. An uncovered side helix located proximal to the ring electrode enabled the fixation of the lead to the vein wall when the lead was rotated clockwise. If a change in lead position was required, the lead could easily be unscrewed from the vein wall by counterclockwise rotation and then repositioned. The quadripolar leads had a proximal diameter of 5.3 Fr and a distal diameter 3.9 Fr, with distances between the electrodes of 21 mm (LV1-LV2), 1.3 mm (LV2-LV3), and 21 mm (LV3-LV4), and were steroid eluting leads (Attain Performa, Medtronic Inc., Minneapolis, MN). The operators were free to choose from three different shapes: a dual bend lead, an S-curved lead, and a straight lead with small tines.
Programming the device
The devices were all programmed to DDD pacing mode at a lower rate of 50 pulses/min. The selected pacing configurations for the active fixation bipolar leads were true bipolar and integrated bipolar LV-tip to RV-coil/RV-ring or LV-ring to RV-coil/RV-ring. For the quadripolar leads, the preferred configurations were bipolar L3-L2, integrated bipolar LV1 to RV-coil/RV-ring, LV3 to RV-coil/RV-ring, or LV4 to RV-coil/RV-ring. The selection of the optimal pacing configuration in the individual patient was based on the PCT, occurrence of PNS, and avoidance of stimulation from an apical LV lead position. A limited number of pacing configurations for the quadripolar leads was necessary for a more precise assessment of the long-axis position of the stimulating electrode. Adjustments of optimal (AV) delay and interventricular timing for the patients with a CRT-D generator were based on an automatic device algorithm (Adaptive CRT, Medtronic, Minnesota Inc, MN). For patients with both normal AV delay and right bundle conduction, the device algorithm selected single LV pacing synchronized to the intrinsic RV conduction. In the patients with CRT-P, all devices were programmed to a sensed AV delay of 120 ms with no programmed LV offset.
Assessment of clinical response
The patients were studied during clinical FU at 2, 6, and 12 months after implantation. NYHA functional class, medication, blood pressure, and the occurrence of PNS were recorded as well as data from device interrogation and PCT, including the percentage of ventricular pacing, and atrial fibrillation burden. Additionally, at the 6- and 12-month FU, echocardiographic measurements were performed, as well as quality of life assessment according to the Minnesota Living with Heart Failure Questionnaire (MLHFQ). The patients who demonstrated a reduction in end-systolic volume of ≥15% were classified as echocardiographic responders to CRT.
Statistical analysis
The data were analysed according to the intention-to-treat principle. Statistical analyses were performed by IBM SPSS Statistics for Windows version 24.0 (IBM Corp., Armonk, NY). To evaluate the normality of continuous variables, we used histograms and Q-Q plots. Continuous variables are expressed as the mean ± standard deviation. Categorical variables are presented as frequencies and percentages. Groups were compared by using paired-sample t-tests and independent-sample t-tests for continuous variables. Pearson’s chi-squared test was used for ordinal categorical variables, and the Fisher’s exact test was used for nominal categorical variables. A p value of ≤.05 was considered statistically significant. For sample size calculation, we estimated a 30% absolute difference in response rate. Powered at 80% and with a 1-sided alpha value of 0.05, assuming no loss at FU, 56 patients were required for the analyses.
Results
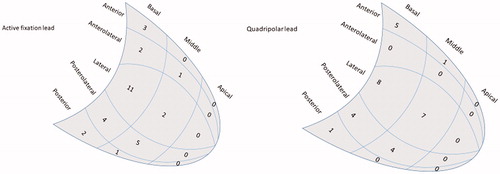
In one patient randomized to the quadripolar group, we were not able to achieve a stable position either with the quadripolar lead or when changing to the active fixation lead, and an alternative thicker lead had to be used. The rest of the patients were implanted according to the randomization, with no crossovers. The LV leads were positioned in the target segment or in an adjacent segment in 52 out of 61 patients (85%), with no differences with respect to lead type (). There was no device infection, and all patients were alive at the 12-month FU. There were 3 LV lead dislodgements, all occurred in the active fixation group and required repositioning of the lead. For the quadripolar leads, the proximal electrode was used as stimulating cathode (LV4-RVring/can) in 37% of the patients; the bipolar LV2-LV3 configuration was used in 37% of the patients and the distal electrode (LV1-RVring/can) was used in 27% of the patients. For the active fixation lead, the proximal electrode was used for unipolar stimulation in 48% of the patients, bipolar configuration was used in 32% of the patients, and the distal electrode was used for unipolar stimulation in 23% of the patients. The PCT for the final selected electrode configuration was higher at implantation for the active fixation lead (1.09 V ± 0.48 vs. 0.77 V ± 0.25; p=.002), but not significantly different at 6- and 12-months FU.
Figure 3. Location and number of selected stimulating electrodes in different left ventricular segments in the active fixation lead group and in the quadripolar lead group.
At the 6-month FU, the reduction in LV end-systolic volume was significant (mean reduction 35 ml, p<.001), but the difference between the patients with active fixation leads and patients with quadripolar leads was not significant ( ). A reduction in the end-systolic volume ≥15% at the 6-month FU was found in 77% and 84% of the patients with active fixation leads and quadripolar leads, respectively (p = 0.51; ). From baseline to the 6-month FU, the LVEF improved significantly in both patient groups and significantly more in the quadripolar lead patient group. However, at the 12-month FU, the LVEF did not differ between the two groups (). In addition, no significant differences were observed between the patient groups for changes in end-diastolic LV volume or end-diastolic LV diameter from baseline to the 6-month FU (). Both groups of patients experienced a significant improvement in NYHA functional status from baseline to FU, but with no significant differences between groups. Quality of life assessment according to the MLHFQ demonstrated significant improvement at FU in both groups of patients, but with no significant differences between the two patient groups ().
Figure 4. The time-related changes of left ventricular end-systolic volumes demonstrates substantial reduction, statistically significantly most pronounced for patients with quadripolar leads at the 6-month follow-up, but almost identical at the 12-month follow-up.
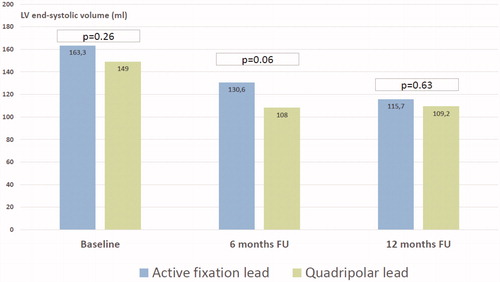
Table 2. Echocardiographic outcomes.
Table 3. Clinical response.
Six patients (19%) in the patient group with active fixation leads experienced PNS during the study period, compared with only three patients (10%) in the quadripolar group (p=.47). All cases of PNS were resolved by reprogramming the devices.
The impact of lead position, lead concordance, and electrical delays on reverse remodelling
Univariate and multivariate linear regression analyses were performed to estimate the eventual effect on reverse remodelling, defined as a ≥ 15% change in end-systolic volume at the 6-month FU. Concordant LV lead position, the final LV segment, QRS duration, Q-LV delay, RV to LV interlead sensed delay, and RV-paced to LV-sensed delay were assessed, but none of the parameters significantly predicted statistically significant LV reverse remodelling.
Discussion
The active fixation bipolar lead (Medtronic Attain Stability) has proven to have high lead implant success and a low rate of lead dislodgement in previous studies [Citation8,Citation11,Citation12]. In this randomized single-centre trial, the use of active fixation bipolar leads was not associated with improved clinical outcome or echocardiographic response compared to regular passive fixation quadripolar leads. The clinical response, assessed by improvement in NYHA classification and in MLHFQ score, was also not significantly different. This is the first randomized clinical trial comparing active fixation LV leads with quadripolar LV leads. However, a retrospective study reported that active fixation bipolar leads were similar in terms of clinical response when compared to quadripolar leads [Citation12]. Since 2010, quadripolar LV leads have been available and have progressively replaced the use of bipolar leads. In addition to more advanced LV lead delivery systems, the use of quadripolar LV leads has improved the implant success rate [Citation13]. In addition, the rate of reinterventions for LV lead dislodgement and PNS has been reduced due to the switch from bipolar to quadripolar leads [Citation13]. A significant impact of the type of LV lead on the clinical outcome of CRT was not obvious. However, several trials have found a reduction in mortality when comparing quadripolar LV leads with bipolar LV leads [Citation4,Citation5,Citation14]. All these trials have been retrospective analyses, and LV lead placement has been empirical and not guided by measurements of mechanical or electrical LV activation delays. Further, the final LV lead positions have not been systematically evaluated in these analyses. Nevertheless, there is now much clinical evidence supporting the routine use of quadripolar LV leads rather than bipolar LV leads. If the structural features of the LV lead have an impact on the clinical and echocardiographic response, this presumably is affected by improving the ability to attain a more advantageous position of the stimulating electrode. We hypothesized that the thinner lead body of the active fixation lead would improve the possibility of reaching smaller coronary veins for optimal LV pacing and that the active fixation mechanism would reduce the chance of the dislodgement of the lead even in large veins. However, the study did not show any significant differences regarding the degree of achieving target placement. These findings may explain the lack of significant differences in clinical and echocardiographic response to CRT provided by the two types of LV leads. Unexpectedly three dislodgements of the active fixation LV leads were observed as compared to none dislodgements of the quadripolar LV leads. Although the trial was not powered to show differences in the rate of lead dislodgement, the finding casts doubt on whether the active fixation bipolar LV leads or the used implantation technique are as stable as modern quadripolar leads. During FU, PNS was more often seen in the patients with active fixation leads versus those with quadripolar leads, but in all cases, reprogramming solved this problem. The sample size in the current trial was considered too limited to disclose any significant differences in the categorical rate of PNS (p=.47). However, the rate of PNS correlated strongly with the long-axis position of the LV lead. Compared to LV pacing from a basal segment, the apical LV pacing site was associated with a higher risk of PNS, as previously reported in another study [Citation15]. In large coronary veins, the active fixation mechanism enables stable lead placement even in a more basal location of the LV lead tip compared to standard passive fixation bipolar LV leads. Thus, this active fixation LV lead can be more comparable to the features of the quadripolar leads, even with fewer options for programmable electrode configurations. This study confirms that active fixation bipolar LV leads are not inferior to quadripolar passive leads in terms of clinical and echocardiographic response. These results are similar to those reported in a larger observational study [Citation16]. When patients were included in the current trial, a quadripolar lead with active fixation was not available. Recently, a quadripolar LV lead (Medtronic lead 4798), which has an identical helix as Attain Stability, has been approved. Recently published data from a large multicentre study of this new active fixation quadripolar LV lead report a very low LV lead dislodgement rate of 0.7%, which is lower than that of comparable passive fixation quadripolar leads [Citation17]. Implanters of CRT devices will regularly encounter challenging coronary vein anatomy with a relatively high risk of LV lead dislodgement. Perhaps this new quadripolar LV lead with a proven active helix fixation mechanism, which provides the advantages of both a high number of programmable pacing vectors and an improvement in lead stability even in large coronary veins, can further contribute to the optimization of the clinical response to CRT [Citation8,Citation14]. A bipolar active fixation lead is a good alternative for patients the with a thin and short target coronary vein because in such cases trackability and stability have to be preferred over multi-electrode availability.
Limitation
This single-centre study had a relatively small sample size and may be underpowered to identify real differences in echocardiographic response and clinical response between the two types of leads that were compared. Perhaps even a longer observation period than 12 months could have augmented the clinical benefit of the active fixation LV lead. The quadripolar leads were all of a single manufacturer (Medtronic Inc., Dublin, Ireland) and the results could have been different with other types of quadripolar leads.
Conclusion
When comparing active fixation bipolar LV leads and passive fixation quadripolar leads, this randomized study showed no significant differences concerning the improvement in clinical symptoms or echocardiographic parameters in response to CRT. The improvement in clinical outcomes of CRT was significant, with an almost similar high number of LV reverse remodelling responders for both the active fixation and the quadripolar LV leads.
Disclosure statement
S. Faerestrand has been a consultant for Medtronic. The other authors declare no conflicts of interests.
Additional information
Funding
References
- McAlister FA, Ezekowitz J, Hooton N, et al. Cardiac resynchronization therapy for patients with left ventricular systolic dysfunction: a systematic review. JAMA. 2007;297(22):2502–2514.
- St John Sutton MG, Plappert T, Abraham WT, et al. Effect of cardiac resynchronization therapy on left ventricular size and function in chronic heart failure. Circulation. 2003;107(15):1985–1990.
- Ypenburg C, van Bommel RJ, Delgado V, et al. Optimal left ventricular lead position predicts reverse remodeling and survival after cardiac resynchronization therapy. J Am Coll Cardiol. 2008;52(17):1402–1409.
- Behar JM, Bostock J, Zhu Li AP, et al. Cardiac resynchronization therapy delivered via a multipolar left ventricular lead is associated with reduced mortality and elimination of phrenic nerve stimulation: long-term follow-up from a multicenter registry. J Cardiovasc Electrophysiol. 2015;26(5):540–546.
- Leyva F, Zegard A, Qiu T, et al. Cardiac resynchronization therapy using quadripolar versus non-quadripolar left ventricular leads programmed to biventricular pacing with single-site left ventricular pacing: impact on survival and heart failure hospitalization. J Am Heart Assoc. 2017;6(10):e007026.
- Erath JW, Vamos M, Domokos D, et al. Effects of implantation of quadripolar left ventricular leads on CRT response. J Interv Card Electrophysiol. 2019;55(1):73–81.
- Bencardino G, Di Monaco A, Russo E, et al. Outcome of patients treated by cardiac resynchronization therapy using a quadripolar left ventricular lead. Circ J. 2016;80(3):613–618.
- Keilegavlen H, Hovstad T, Faerestrand S. Active fixation of a thin transvenous left-ventricular lead by a side helix facilitates targeted and stable placement in cardiac resynchronization therapy. Europace. 2016;18(8):1235–1240.
- Kristiansen HM, Vollan G, Hovstad T, et al. The impact of left ventricular lead position on left ventricular reverse remodelling and improvement in mechanical dyssynchrony in cardiac resynchronization therapy. Eur Heart J Cardiovasc Imaging. 2012;13(12):991–1000.
- Kristiansen HM, Vollan G, Hovstad T, et al. A randomized study of haemodynamic effects and left ventricular dyssynchrony in right ventricular apical vs. high posterior septal pacing in cardiac resynchronization therapy. Eur J Heart Fail. 2012;14(5):506–516.
- Yee R, Gadler F, Hussin A, et al. Novel active fixation mechanism permits precise placement of a left ventricular lead: early results from a multicenter clinical study. Heart Rhythm. 2014;11(7):1150–1155.
- Ziacchi M, Giannola G, Lunati M, et al. Bipolar active fixation left ventricular lead or quadripolar passive fixation lead? An Italian multicenter experience. J Cardiovasc Med (Hagerstown). 2019;20(4):192–200.
- Boriani G, Connors S, Kalarus Z, et al. Cardiac resynchronization therapy with a quadripolar electrode lead decreases complications at 6 months: results of the MORE-CRT randomized trial . JACC Clin Electrophysiol. 2016;2(2):212–220.
- Turakhia MP, Cao M, Fischer A, et al. Reduced mortality associated with quadripolar compared to bipolar left ventricular leads in cardiac resynchronization therapy. JACC Clinical Electrophysiol. 2016;2(4):426–433.
- Biffi M, Exner DV, Crossley GH, et al. Occurrence of phrenic nerve stimulation in cardiac resynchronization therapy patients: the role of left ventricular lead type and placement site. Europace. 2013;15(1):77–82.
- Ziacchi M, Diemberger I, Corzani A, et al. Cardiac resynchronization therapy: a comparison among left ventricular bipolar. Sci Rep. 2018;8(1):13262.
- Jackson KP, Faerestrand S, Philippon F, et al. Performance of a novel active fixation quadripolar left ventricular lead for cardiac resynchronization therapy: attain stability quad clinical study results. J Cardiovasc Electrophysiol. 2020;31(5):1147–1154.
