Abstract
Objectives. To examine whether possibilities to improve care among patients with diabetes are reflected in the numbers of cardiovascular complications at national and regional level in Finland. Methods. The study population included all patients with diabetes in Finland since 1964. The incidences of first acute coronary syndrome, ischemic stroke and lower limb amputation were examined for the period from 2010 to 2017. The age- and sex-standardised incidence rates were calculated for the first events. Adjusted Poisson regression mixed models were used to calculate average annual trends and assess regional variation of incidences during the periods 2010 to 2013 and 2014 to 2017 in the university hospital districts (UHDs) and hospital districts (HDs). Results. The nationwide incidence of first acute coronary syndrome decreased among patients with diabetes by 2.7% (95% confidence interval 2.3%; 3.0%), ischemic stroke by 2.0% (1.5%; 2.4%) and major lower limb amputation by 4.6% (3.1%; 5.9%) annually. The sexes differed only in the decrease in acute coronary events. The annual decrease among males was 2.1% (1.6%; 2.6%) and among females was 3.4% (2.8%; 4.0%) (p = .001). Marked variation was observed among UHDs and HDs in the incidences of cardiovascular events and lower limb amputations in patients with diabetes. The variation in annual trends of diabetic complications was most pronounced in acute coronary syndrome among UHDs with an estimated variance of 0.0006 (p = .034). Conclusions. The decrease in the incidence of first cardiovascular events among patients with diabetes continued from 2010 to 2017 in Finland. However, the declining national incidence rates hide regional differences which should be a target for improvement.
1. Introduction
Diabetic complications bring an increasing burden to health care due to the growing number of patients with diabetes mellitus [Citation1]. At the same time when the number of patients with diabetes is growing in high-income countries, the proportion of patients having diabetic complications is diminishing [Citation1]. The positive development has been explained by better treatment of diabetes and other risk factors [Citation2,Citation3] but the interpretation is complicated by changes in the definition of the denominator population [Citation4].
Despite the decreasing trends in cardiovascular complications among patients with diabetes, the excess in cardiovascular events and total mortality due to diabetes has not decreased in the total population [Citation5]. One explaining factor is that type 2 diabetes starts at younger age [Citation6,Citation7], and the younger the disease starts, the higher the risk for total mortality, cardiovascular mortality and even non-cardiovascular mortality [Citation8]. The same detrimental effects have been seen among patients with type 1 diabetes [Citation9]. Other known factors affecting the incidence of diabetic complications include ethnicity, sex and quality of risk factor treatment [Citation10]. The domicile also affects the treatment results. Standards of care were better met in urban areas and less deprived areas [Citation11].
Our earlier population-based study for the years from 2000 to 2011 showed an annual decrease of 4.1% (95% confidence interval 3.2%; 5.0%) of the first acute coronary syndrome (ACS) and 3.7% (3.0%; 4.3%) of the first ischemic stroke (IS) among patients with diabetes in Finland [Citation12]. Significant differences were observed among the university hospital districts (UHDs) [Citation13] and hospital districts (HDs) [Citation12] in the incidence of ACS and IS. For instance, the incidence of ACS differed by 1.51-fold (1.29; 1.76) between the UHDs with the highest and the lowest age-standardised incidence rates [Citation13]. For IS, the corresponding difference was 1.36-fold (1.18; 1.56).
Currently, a remarkable change is going on in the treatment of diabetes. During the last decade, the hazardous effect of nephropathy on the cardiovascular prognosis of patients with diabetes has been pointed out as a reason for the need for extra improvement in care [Citation14, Citation15], and new antihyperglycaemic medicines have widened the treatment options in type 2 diabetes. Sodium/glucose co-transporter 2 inhibitors and glucagon-like peptide-1 receptor agonists are effective in the prevention of mortality, cardiovascular disease and nephropathy [Citation16, Citation17].
The possibilities of improvement in treatment make it especially interesting to follow up the changes in the incidence of cardiovascular complications in diabetes. In this study, we aimed to update the nationwide and regional trends in cardiovascular morbidity of patients with diabetes including the incidences of first ACS, IS and lower limb amputations (LLAs) for the years 2010 to 2017. We hypothesised that there would be regional differences in the development of UHDs and HDs.
2. Methods
2.1. Study population and definition of cardiovascular complications
We used the FinDM database which aims to include all patients identified as having diabetes in Finland since 1964. Patients with diabetes included in the database were identified by combining the information from the national registers of hospital discharges and ambulatory care visits, causes of death register and reimbursement registers of antihyperglycaemic medications. The three first registers also included patients without antihyperglycaemic medicines. Therefore, virtually all persons who are treated for diabetes in Finland are included in the register. In addition, it should be noted that the national guidelines in Finland have recommended for years to start metformin medication immediately when type 2 diabetes is diagnosed [Citation18]. A precise description of the FinDM database has been published elsewhere [Citation19]. All patients with diabetes during the years 2010 to 2017 were included in the study population. The regional distribution of the diabetes population was based on the municipal residence of each person on the last day of each preceding year. All municipalities belong to one of the 21 HDs and each HD to one of the five UHDs: Helsinki, Turku, Tampere, Kuopio and Oulu.
The incidence of first ACS, IS and LLA for each person were defined from the hospital discharge register and causes of death register based on the International Classification of Diseases codes. For identification of incident ACS, we used in non-fatal cases ICD-10 codes I20.0, I21, I46, and in fatal cases ICD-10 codes I21-I25 and I46. For incident IS ICD-10 codes I63 (except I63.6) and I64 (due to the fact that most strokes are ischaemic) were used, plus code G45 for transient ischaemic attack. All LLAs through and proximal to the ankle were considered major (the surgical codes of Nordic Medico-Statistical Committee, NOMESCO, NFQ10, NFQ20, NGQ10, NGQ20, NHQ10 and NHQ20), and those distal to the ankle were considered minor (NOMESCO codes NHQ30 and NHQ40). We excluded LLAs due to trauma (ICD-10 codes S70-S99) except those recorded with ICD-10 codes S90–91 (superficial lesions of the foot). For all first events, we looked back at our hospital discharge register data for 10 years to exclude cases having had a prior hospitalization with the same event.
2.2. Statistical methods
Patients with diabetes were classified into five age groups: 54 years or younger, 55–64 years, 65–74 years, 75–84 years and 85 years or older. The annual modified Charlson Comorbidity Index was counted for each patient at risk to account for 11 comorbid conditions from diagnoses of hospitalisations in two preceding years and classified into five groups according to the predicted one-year prognosis of the patients based on the comorbidities [Citation20]. In addition, preceding parallel complications (ACS, IS and LLA) were defined to adjust for vascular complications. Person years calculated for patients with diabetes from 2010 to 2017 were used as the population at risk.
The age- and sex-standardised incidence rates among patients with diabetes were calculated for the first ACS, IS and minor and major LLAs. The direct method of standardization was used with the total population with diabetes in 2017 as the standard population.
To examine the secular development in the regional incidence of cardiovascular complications, the data were split into two periods, 2010 to 2013 and 2014 to 2017. That allowed us to compute the estimates using separate multilevel Poisson regression models for UHDs and HDs. In these models, we adjusted for sex, age group, type of diabetes, Charlson Comorbidity Index and parallel complications. To assess the extent of regional variation, we used Markov chain Monte Carlo estimation techniques to calculate p values for variance components.
Poisson regression mixed models adjusted for sex and age group were used to calculate average annual trends in the incidence of the first cardiovascular complications in population at risk. Trends were estimated as average annual change at national, UHD and HD levels. In the latter settings, multilevel models were used with UHD and HD modelled as random factors. While comparing the trends in HDs the data were pooled in two-year periods to balance the variation in small HDs.
Further, we used respective logistic regression mixed models to explore potential changes in the proportion of major LLAs of the first LLAs as a marker of a shift to less invasive operations. UHD and HD level estimates were derived from the multilevel models by converting random level best linear unbiased predictions (BLUPs) to risk ratios (RRs) and, in the case of logistic regression models, odds ratios (ORs). Area level estimates were compared to model-based national average estimates.
Finally, we examined the use of medicines that reduce cardiovascular risks in patients with diabetes. Our intention was to analyse whether the region-wise prevalence of medicine use reflect differences in the incidence of complications among UHDs. We were able to use the UHD-level data for the year 2017 of antihyperglycaemic medicines (ATC group A10 and separately groups A10A, A10BB, A10BJ, A10BK), medicines for high cholesterol (ATC groups C10AA and separately C10AX09 and C10BA) and elevated blood pressure (ATC groups C02, C03A, C03B, C07, C08 and C09) using the data from FinDM database. We cross-tabulated the number of different medications used by ATC group in each UHD and analysed separately some of them as described above. Cochran–Mantel–Haenszel statistics were used to test the differences. All statistical analyses were conducted using the R statistical software, version 4.0.5 [Citation21].
3. Results
During the study period from 2010 to 2017, the annual numbers of the first ACS varied from 5527 to 6535, the first IS from 3930 to 4809, the first major LLA from 411 to 485 and the first minor LLA from 492 to 728 among patients with diabetes in Finland (patients at risk 366,490 in 2010 and 468,168 in 2017) (). Study population characteristics are presented for the periods 2010 to 2013 and 2014 to 2017 in . The table shows the basic figures of study populations which are used in the analyses comparing the two periods.
Table 1. Age and sex standardized incidence rates with 95% confidence intervals (CI) of the first acute coronary syndrome (ACS), ischaemic stroke (IS), major lower limb amputation (LLA) and minor LLA per 100,000 person-years among patients with diabetes in Finland from 2010 to 2017.
Table 2. Characteristics of the study population during the periods 2010 to 2013 and 2014 to 2017.
Marked variation was observed in the incidences of diabetic cardiovascular events and LLAs among UHDs and HDs ( and ). The age- and sex-adjusted incidence of ACS was lower in the southern UHDs (Helsinki, Turku and Tampere) and higher in the eastern and northern UHDs (Kuopio and Oulu) during the whole study period compared to the average (). The incidence of IS was lower in Tampere UHD during the whole study period and higher in Kuopio UHD during the first half of the study period and in Oulu UHD during the second half of the study period (). The incidence of major LLA was lower in Helsinki UHD during the whole study period and during the first half of the study period in Tampere UHD. The incidence of major LLA was higher in Kuopio UHD during the whole study period (). The UHDs did not differ in the incidence of minor LLA during the first half of the study period but during the second half Kuopio UHD had higher incidence (). The UHDs did not differ in the proportion of major LLAs of all first LLAs during the study period.
Figure 1. Risk ratios (RR) and odds ratios (OR) with 95% confidence interval (95%CI) derived from best linear unbiased predictions (BLUPs) for the differences in university hospital districts (UHDs) in the incidence of first acute coronary syndrome (ACS), ischaemic stroke (IS), major lower limb amputation (LLA), minor LLA and percentage of major LLA in the first amputation among patients with diabetes in Finland during the years 2010 to 2013 and 2014 to 2017 compared to the model average. Models adjusted for age, sex, type of diabetes, Charlson Comorbidity Index and parallel cardiovascular complications.
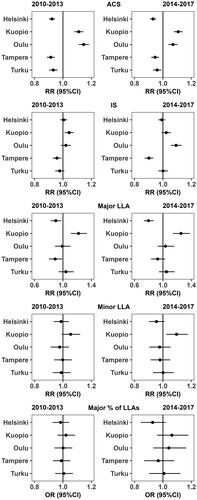
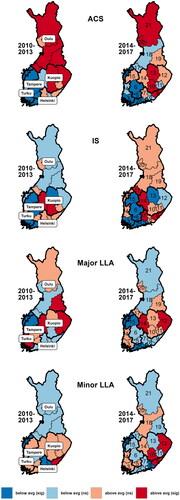
Figure 2. Risk ratios (RR) derived from the best linear unbiased predictions (BLUPs) for the differences in hospital districts (HDs) in the incidence of first acute coronary syndrome (ACS), ischaemic stroke (IS), major lower limb amputation (LLA) and minor LLA among patients with diabetes in Finland during the years 2010 to 2013 and 2014 to 2017 compared to the model average. Models adjusted for age, sex, type of diabetes, Charlson Comorbidity Index and parallel cardiovascular complications. The university hospitals districts are marked in the map of the first period and HDs in the map of the second period with following numbers (3) Varsinais-Suomi, (4) Satakunta, (5) Kanta-Häme, (6) Pirkanmaa, (7) Päijät-Häme, 8) Kymenlaakso, (9) Etelä-Karjala, (10) Etelä-Savo, (11) Itä-Savo, (12) Pohjois-Karjala, (13) Pohjois-Savo, (14) Keski-Suomi, (15) Etelä-Pohjanmaa, (16) Vaasa, 17) Keski-Pohjanmaa, (18) Pohjois-Pohjanmaa, (19) Kainuu, (20) Länsi-Pohja, (21) Lappi, (25) Helsinki/Uusimaa.
The nationwide age-standardized annual incidence of all other cardiovascular complications except the minor LLAs were decreasing during the study period. The incidence of the first ACS decreased annually by 2.7% (2.3%; 3.0%), the first IS by 2.0% (1.5%; 2.4%) and the first major LLA by 4.6% (3.1%; 5.9%) (). The proportion of major LLAs of the first amputations decreased by 8.3% (6.3%; 10.2%) annually. The decrease was significantly faster in ACS among women than among men with diabetes ().
Table 3. Age-standardized annual trends with 95% confidence intervals (95%CI) in the incidence of first acute coronary syndrome (ACS), ischaemic stroke (IS), major lower limb amputation (LLA), minor LLA and proportion of major LLAs of all first LLAs (MLLA %) by sex among patients with diabetes in Finland during the year 2010 to 2017.
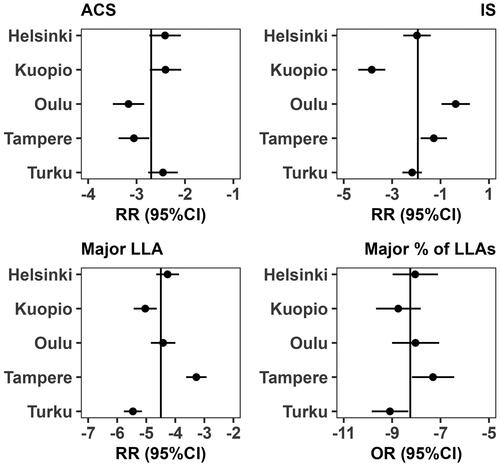
When studying the trends among the UHDs, the annual decrease of first cardiovascular events was faster than the average in Oulu and Tampere UHDs for ACS, in Kuopio UHD for IS, in Kuopio and Turku UHDs for major LLA, and in Turku UHD for the proportion of major LLAs in the first amputation (.) The variation in annual trends of cardiovascular events was most pronounced in ACS with an estimated variance of 0.0006 (p = .034).
Figure 3. Average annual trend as risk ratio (RR) or odds ratio (OR) with 95% confidence intervals (95%CI) in the incidence of the first acute coronary syndrome (ACS), ischaemic stroke (IS), major lower limb amputation (LLA) and proportion of major LLAs of all first LLAs among patients with diabetes in Finland during the years 2010 to 2017 in the five university hospital districts compared to the model average.
Regarding HDs, in the adjusted incidence of ACS the country was divided into two; higher incidence in north and east and lower incidence in south and west during the first half of the study period. During the second half of the study period, the differences narrowed to some extent (). In IS, two HDs in central Finland had significantly higher incidences than the average in the country during the first half of the study period. During the second half of the study period, the differences between HDs were growing (). Concerning major LLAs, the number of HDs that had a higher incidence of major LLAs than the average diminished from six HDs during the first half to two HDs during the second half of the study period (). The differences in the incidence of minor LLA increased between the HDs. There were no or only small differences in the trends of the cardiovascular events and LLAs among HDs and so they are not separately reported.
The UHD-level analyses showed significant differences in the proportion of patients with diabetes in reducing the risk of cardiovascular complications with medicines: any of the antihyperglycaemic, cholesterol-lowering or antihypertensive medicines, the number of used medicines in each group and separately the sodium/glucose co-transporter 2 inhibitors and glucagon-like peptide-1 receptor agonists, sulphonylureas, insulins, statins and ezetimibe (all p < .001 in cross-tabulations). Patients with diabetes in Kuopio UHD had the most intensive medicine care to lower all studied cardiovascular risks (). Medicines for hypertension and to lower cholesterol were used least frequently in the Helsinki UHD. Newer medicines recommended for cardiovascular prevention, ezetimibe and sodium/glucose co-transporter 2 inhibitors, were used least frequently in Turku UHD ().
Table 4. University hospital district (UHD) based comparison of the use of medicines for elevated blood pressure (BP), medicines for elevated cholesterol (CH) and antihyperglycaemic medicines (DM); the numbers and proportions of patients with diabetes using the medicines in 2017.
4. Discussion
Our study showed that the favourable trend of decreasing incidence of the first cardiovascular events that we have demonstrated earlier for the years 2000 to 2011 [Citation12,Citation13], has continued among patients with diabetes in Finland. The age-standardised annual incidence of cardiovascular complications and proportion of major LLAs in the first LLA was decreasing during the years 2010 to 2017.
This study showed a 2.7% annual reduction of the first ACS and 2.0% of the first IS for the years 2010 to 2017. The annual reductions were 4.1% and 3.7%, respectively, during the years 2000 to 2011 [Citation13]. Thus, the speed of the improvement seems to be slowing down. This can have several reasons. One of them is the good results which we saw also in this study; improvement becomes harder when the rates are lower. Another explanation could be the changes in the treatment of patients with diabetes or how their treatment is organised. The third explanation can be the changes in the risk population. We may assume that the promising results of the new medications, sodium/glucose co-transporter 2 inhibitors, and glucagon-like peptide-1 receptor agonists would bring further decrease in cardiovascular complications in the near future [Citation16,Citation17] which calls for regular follow-ups of incidence figures.
Our nationwide results agree to a great extent with the numbers reported from Hong Kong [Citation22,Citation23]. The Hong Kong results and the results from Finland show annual improvements that are better than in many other countries [Citation1,Citation4]. Age and sex-standardised total mortality and cardiovascular complications of patients with diabetes are decreasing in high-income countries even when the analyses are performed using the total population as the denominator [Citation4]. Secular trends can be misinterpreted due to changes in diagnostic criteria for type 2 diabetes, screening for diabetes and definitions of complications [Citation4]. Even immigration plays a role while studying the trends as was shown in a study from Sweden [Citation24].
The improvements we have seen in the incidence of ACS and IS in patients with diabetes are also reflected in the decreasing incidence of LLAs. Many countries report decreasing numbers of major LLAs while minor LLAs remain stable [Citation25].
There are few studies examining regional variations of diabetic complications within a country. Anyhow, the research has shown that differences can be seen even in different populations within a country [Citation4]. We believe that regional developments should be studied more to help healthcare providers to improve their performance. There are several reasons behind the regional variation, some of them outside the scope of health care. Ethnicity and social status have been shown to influence the results of diabetes treatment [Citation26]. A Finnish study showed that area-level socio-economic status affected the results of diabetes treatment [Citation27]. A recent study from the United States showed differences in life expectancy of the general population among racial–ethnic groups and among counties [Citation28]. The incidence of ACS and IS has shown great geographic variation in the general population [Citation29,Citation30]. The same also applies to regional differences in cardiovascular risk factor profiles within a country [Citation31].
Our regional analyses of the UHDs showed marked differences but even more between HDs. This emphasizes the need to analyse outcome data in administrative units to show where the needs for improvement are the biggest. In our study, the incidence of a cardiovascular complication could be among the highest and lowest in two HDs that are next to each other. For example, within Helsinki UHD there was one HD with significantly better results and one with significantly worse results than the average in the country in the incidence of ACSs during the second half of the study period. We found the same kind of situation with the incidence of ISs in HDs both in Helsinki and Kuopio UHDs.
Differences in the incidence and trend figures between UHDs can be explained by differing genetic backgrounds in the populations but they can also be explained by differences in medical education, use of national guidelines and how treatment goals are implemented. Differences between HDs next to each other are more difficult to be explained by genetic factors. There can be distances to educational events and thus the activity to treat risk factors be an even better explanation.
The high rates of cardiovascular complications in the first half of the study period were only weakly reflected in the speed of decrease in the incidence of cardiovascular complications. The finding calls for strong regional implementation strategies for the effective treatment of risk factors.
It is also important to point out that the incidence of different cardiovascular complications in diabetes could show contrary results in an HD; ACS rate high and IS rate low. This is interesting because the risk factors are much the same. The competitive role of different cardiovascular complications can be reflected in the results. One can assume that if the treatment of one risk factor, say hypertension, differs a lot between HDs that this is reflected in the outcomes as was shown by Adamsson Eryd et al. [Citation32]. The authors found a much stronger effect of elevated blood pressure on the incidence of the first stroke than on the first myocardial infarction among patients with type 2 diabetes.
Our study showed that the differences in the incidence of diabetic cardiovascular complications are only weakly explained by the UHD-level use of medications to prevent these complications. The interpretation of results is difficult because we have known for decades that the risk factor level of patients with type 2 diabetes and people without diabetes is worse in Eastern than Western Finland [Citation33]. The activity to treat risk factors with medicines was better in Eastern UHD of Kuopio than in the rest of the country but still, for example, some 53% of patients with diabetes were without cholesterol-lowering medication in 2017.
We believe that our study results are of special interest to all active in the quality improvement of diabetes care. Especially important was the finding that in a country with good national average improvement, there are regions with markedly slower development. This calls for regional analyses to enable politicians, leaders and healthcare professionals to react. It is important to notice that the four-year pooling in the incidence analyses revealed marked differences between HDs which is important in comparisons of improvement [Citation33], while the two-year pooling in trend analyses was not able to demonstrate differences. Either one needs a longer time or a larger population for stable comparisons.
A strength of our study is that virtually all patients with diabetes living in Finland are included. Another strength is that we have been able to follow up on domicile-based each patient’s cardiovascular complications for a long time and were able to report the development in cardiovascular events by UHD and HD. Even though estimated regional variances remained relatively small, multilevel modelling allowed us to assess regional variation at two administrative levels and adjust for several confounding factors. The Limitations of our study are the lack of background information to explain the regional differences. It would have helped if we had been able to adjust for regional demographic differences, and social status together with clinical variables such as body mass index, blood pressure and kidney function for each patient. We were, however, able to conduct UHD-level analyses about the regional activity to use medicines for lowering the risk of cardiovascular complications among patients with diabetes.
It has been emphasised that the prevalence figures for cardiovascular complications among patients with diabetes should be known to improve decision-making in the allocation of resources [Citation34]. We agree with the statement but find it equally important to have up-to-date incidence figures and be as close to service producers as possible to enable them to improve their performance in the prevention of cardiovascular complications. Further studies are needed to assess individual and regional level factors behind the regional differences in cardiovascular complications among patients with diabetes.
Ethical approval
The ethical approval for the study was received from the Research Ethics Committee of THL, an excerpt of proceedings 5/2018 (§791).
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
Due to data protection legislation in Finland, individual-level data on the study subjects cannot be released.
Additional information
Funding
References
- Harding JL, Pavkov ME, Magliano DJ, et al. Global trends in diabetes complications: a review of current evidence. Diabetologia. 2019;62(1):3–16. doi:10.1007/s00125-018-4711-2.
- Ford ES. Trends in the risk for coronary heart disease among adults with diagnosed diabetes in the U.S.: findings from the National Health and Nutrition Examination Survey, 1999–2008. Diabetes Care. 2011;34(6):1337–1343. doi:10.2337/dc10-2251.
- Wong ND, Zhao Y, Patel R, et al. Cardiovascular risk factor targets and cardiovascular disease event risk in diabetes: a pooling project of the atherosclerosis risk in communities study, multi-ethnic study of atherosclerosis, and Jackson heart study. Diabetes Care. 2016;39(5):668–676. doi:10.2337/dc15-2439.
- Ali MK, Pearson-Stuttard J, Selvin E, et al. Interpreting global trends in type 2 diabetes complications and mortality. Diabetologia. 2022;65(1):3–13. doi:10.1007/s00125-021-05585-2.
- Heintjes EM, Houben E, Beekman-Hendriks WL, et al. Trends in mortality, cardiovascular complications, and risk factors in type 2 diabetes. Neth J Med. 2019;77(9):317–329.
- Wilmot EG, Davies MJ, Yates T, et al. Type 2 diabetes in younger adults: the emerging UK epidemic. Postgrad Med J. 2010;86(1022):711–718. doi:10.1136/pgmj.2010.100917.
- Saeedi P, Petersohn I, Salpea P, IDF Diabetes Atlas Committee., et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843., doi:10.1016/j.diabres.2019.107843.
- Sattar N, Rawshani A, Franzén S, et al. Age at diagnosis of type 2 diabetes mellitus and associations with cardiovascular and mortality risks. Circulation. 2019;139(19):2228–2237. doi:10.1161/CIRCULATIONAHA.118.037885.
- Rawshani A, Sattar N, Franzén S, et al. Excess mortality and cardiovascular disease in young adults with type 1 diabetes in relation to age at onset: a nationwide, register-based cohort study. Lancet. 2018;392(10146):477–486. doi:10.1016/S0140-6736(18)31506-X.
- Grimaldi A, Heurtier A. Epidémiologie des complications cardio-vasculaires du diabète [epidemiology of cardio-vascular complications of diabetes] (in French). Diabetes Metab. 1999;25(Suppl 3):12–20.
- Kurani SS, Lampman MA, Funni SA, et al. Association between area-level socioeconomic deprivation and diabetes care quality in US primary care practices. JAMA Netw Open. 2021;4(12):e2138438. doi:10.1001/jamanetworkopen.2021.38438.
- Winell K, Arffman M, Salomaa V. Significant regional differences in the incidence of acute coronary syndromes and strokes among diabetic patients in Finland (in Finnish). Duodecim. 2020;136(5):561–568.
- Winell K, Arffman M, Pietilä A, et al. Regional differences in the incidence of diabetic cardiovascular events reflect the quality of care. Scand Cardiovasc J. 2018;52(5):232–237. doi:10.1080/14017431.2018.1497198.
- Fox CS, Matsushita K, Woodward M, Chronic Kidney Disease Prognosis Consortium., et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis [published correction appears in lancet 2013;381:374]. Lancet. 2012;380(9854):1662–1673., doi:10.1016/S0140-6736(12)61350-6.
- Tuttle KR, Bakris GL, Bilous RW, et al. Diabetic kidney disease: a report from an ADA Consensus Conference. Diabetes Care. 2014;37(10):2864–2883. doi:10.2337/dc14-1296.
- Zinman B, Wanner C, Lachin JM, EMPA-REG OUTCOME Investigators., et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–2128., doi:10.1056/NEJMoa1504720.
- Kristensen SL, Rørth R, Jhund PS, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet Diabetes Endocrinol. 2019;7(10):776–785. doi:10.1016/S2213-8587(19)30249-9.
- Type 2 diabetes. Current Care Guidelines. 2020). In Finnish. (cited 2023 June 12). Available from: https://www.kaypahoito.fi/hoi50056#K1.
- Arffman M, Ilanne-Parikka P, Keskimäki I, et al. FinDM database on diabetes in Finland. Discussion paper: 2020_019. (cited 2022 Jun 7) Available from http://urn.fi/URN:ISBN:978-952-343-492-9. .
- Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi:10.1097/01.mlr.0000182534.19832.83.
- R Development Core Team R. A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2018. Available from http://www.R-project.org (cited 2022 June 7).
- Wu H, Lau ESH, Yang A, et al. Trends in diabetes-related complications in Hong Kong, 2001–2016: a retrospective cohort study. Cardiovasc Diabetol. 2020;19(1):60. doi:10.1186/s12933-020-01039-y.
- Wu H, Yang A, Lau ESH, et al. Secular trends in rates of hospitalisation for lower extremity amputation and 1 year mortality in people with diabetes in Hong Kong, 2001–2016: a retrospective cohort study. Diabetologia. 2020;63(12):2689–2698. doi:10.1007/s00125-020-05278-2.
- Bennet L, Nilsson C, Mansour-Aly D, et al. Adult-onset diabetes in Middle Eastern immigrants to Sweden: novel subgroups and diabetic complications – the all new diabetes in Scania cohort diabetic complications and ethnicity. Diabetes Metab Res Rev. 2021;37(6):e3419. doi:10.1002/dmrr.3419.
- Carinci F, Uccioli L, Massi Benedetti M, et al. An in-depth assessment of diabetes-related lower extremity amputation rates 2000–2013 delivered by twenty-one countries for the data collection 2015 of the Organization for Economic Cooperation and Development (OECD). Acta Diabetol. 2020;57(3):347–357. https:/ doi:10.1007/s00592-019-01423-5.
- Lee W, Lloyd JT, Giuriceo K, et al. Systematic review and meta-analysis of patient race/ethnicity, socioeconomics, and quality for adult type 2 diabetes. Health Serv Res. 2020;55(5):741–772. doi:10.1111/1475-6773.13326.
- Sikiö M, Tykkyläinen M, Tirkkonen H, et al. Type 2 diabetes care in North Karelia Finland: do area-level socio-economic factors affect processes and outcomes? Diabetes Res Clin Pract. 2014;106(3):496–503. doi:10.1016/j.diabres.2014.09.023.
- GBD US Health Disparities Collaborators. Life expectancy by county, race, and ethnicity in the USA, 2000–19: a systematic analysis of health disparities. Lancet. 2022;400(10345):25–38. doi:10.1016/S0140-6736(22)00876-5.
- Havulinna AS, Pääkkönen R, Karvonen M, et al. Geographic patterns of incidence of ischemic stroke and acute myocardial infarction in Finland during 1991–2003. Ann Epidemiol. 2008;18(3):206–213. doi:10.1016/j.annepidem.2007.10.008.
- Bihrmann K, Gislason G, Larsen ML, et al. Joint mapping of cardiovascular diseases: comparing the geographic patterns in incident acute myocardial infarction, stroke and atrial fibrillation, a Danish register-based cohort study 2014-15. Int J Health Geogr. 2021;20(1):41. doi:10.1186/s12942-021-00294-w.
- Vähämurto L, Pahkala K, Magnussen CG, et al. Coronary heart disease risk factor levels in Eastern and Western Finland from 1980 to 2011 in the cardiovascular risk in Young Finns study. Atherosclerosis. 2019;280:92–98. doi:10.1016/j.atherosclerosis.2018.11.007.
- Adamsson Eryd S, Gudbjörnsdottir S, Manhem K, et al. Blood pressure and complications in individuals with type 2 diabetes and no previous cardiovascular disease: national population based cohort study. BMJ. 2016;354:i4070. PMID: 27492939; PMCID: PMC4975020. doi:10.1136/bmj.i4070.
- Laakso M, Rönnemaa T, Pyörälä K, et al. Atherosclerotic vascular disease and its risk factors in non-insulin-dependent diabetic and nondiabetic subjects in Finland. Diabetes Care. 1988;11(6):449–463. PMID: 3402300. doi:10.2337/diacare.11.6.449.
- Einarson TR, Acs A, Ludwig C, et al. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17(1):83. doi:10.1186/s12933-018-0728-6.
