Abstract
Objectives: To investigate whether normal body mass index (BMI) shortly after percutaneous coronary intervention (PCI) for myocardial infarction is associated with increased risk of long-term major cardiovascular events (MACE), and to explore potential clinical determinants of long-term weight loss (WL) after PCI. Methods: Single-center cohort study with 5-year follow-up of patients treated with PCI for myocardial infarction between 2016 and 2018. Categorical WL was defined as > 0 kg body weight reduction from baseline to end of follow-up. Results: Of 236 patients (24% women), mean age was 64.9 ± 10.2 years and mean BMI within 4 days after PCI was 27.1 ± 4.3 kg/m2. Seventy-five patients (32%) had at least one MACE, equally distributed between those with normal weight (31%), overweight (32%), and obesity (31%). Patients with overweight or obesity had a lower crude mortality rate than their normal weight counterparts (7.4% vs 16.4%, p = 0.049), but the relative hazard of death did not differ from those with normal weight, HR 0.50, 95% CI 0.22-1.15. Patients with either a long-term WL (n = 112) or no WL (n = 95) had a comparable incidence of non-fatal MACE (27% vs 22%, p = 0.518). The proportion of patients reporting unintentional weight loss was significantly higher in the normal weight group (82%) compared with those with overweight (41%) or obesity (28%), p < 0.001. Conclusion: Our results did not confirm any association between normal BMI after PCI and long-term MACE. However, patients with normal BMI at baseline had a higher incidence of unintentional WL than those with elevated BMI. Trial registration: Current research information system in Norway (CRISTIN): ID 542528
Introduction
Obesity is a well-established independent risk factor for cardiovascular disease. However, an intriguing phenomenon known as the "obesity paradox" has been observed, showing that individuals with elevated body mass index (BMI) have improved survival after acute myocardial infarction (AMI) and percutaneous coronary intervention (PCI) as compared with those with normal BMI [Citation1–3]. Despite extensive research through large registry studies and meta-analyses, the underlying mechanisms of this paradox are not clearly understood [Citation2–5]. One common denominator has been that patients with increased BMI have been younger compared with normal weight patients. Further, existing studies have been limited to one single measure of BMI at baseline without fully determining how changes in weight after the cardiovascular event associate with clinical outcome. In a meta-analysis of weight changes in patients with coronary artery disease, Pack et al. [Citation6] reported observational (unintentional) weight loss (WL) to be associated with adverse cardiovascular events, while presumed intentional WL was associated with improved outcomes. Although the heterogeneity of studies was high, the design was quite similar, with a weight change time interval ranging from 1.5 to 60 months (mean 12.6), and a mean follow-up for 3.2 years for a composite outcome of mortality and major cardiovascular events (MACE). However, adjustments for potential confounders such as age, sex, smoking, and new onset malignancy were incompletely reported.
The objectives of the present long-term follow-up study of PCI treated patients with incident AMI were twofold: First, to investigate whether patients with normal BMI (<25 kg/m2) had higher incidence of major cardiovascular events (MACE) compared with patients with elevated BMI (≥25 kg/m2) considering potential confounders. Second, to assess whether clinical baseline characteristics (including BMI), incident non-fatal MACE, or new-onset comorbidities were associated with long-term weight loss (WL); intentional or unintentional.
Material and methods
Study design
This is an ancillary study derived from a recent prospective observational study focusing on the prognostic impact of changes in global longitudinal strain 3 months following PCI-treated AMI [Citation7]. We used a retrospective cohort design to compare the long-term clinical outcomes in patients with overweight, obesity and normal weight at baseline. Additionally, a prospective cohort design was employed by interviewing patients about their current body weight at end-of-follow-up to investigate the associations between baseline predictors, lifestyle measures, non-fatal MACE, new-onset comorbidities, and long-term WL.
Setting
The study was conducted at Vestfold Hospital Trust, a secondary care general hospital in Norway. Eligible patients with AMI underwent PCI at Oslo University Hospital (tertiary care hospital). Following PCI, patients returned within 1-2 days for subsequent management at Vestfold Hospital Trust, including measurements of weight. Stabilized patients were included consecutively within 4 days following PCI from April 8, 2016 to December 20, 2018. After the index AMI and following all recurrent coronary event after discharge, patients were offered participation in a multidisciplinary cardiac rehabilitation program [Citation8]. Medical treatment was given according to present guidelines. Patients were followed from the time of index AMI until the date of last telephone interview (25th October 2022) or death, and all available hospital records were carefully screened for relevant data. The mean follow-up of MACE and new-onset comorbidities was 56 months (range 5-71). The interviews were conducted prospectively by a clinically experienced cardiologist (JEO) between 25th March and 25th October 2022 with a mean follow-up of 60 (range 46-71) months. During the interviews, all patients were asked whether they had intended to lose weight, either by reducing calorie intake or increasing physical activity, and whether they had attended any expert led weight loss course.
The study was approved by the Regional Ethics Committee of Health Region South-East, Norway (2015/2359). This ancillary study focusing on the impact of obesity and WL was approved by the same authorities on March 10, 2021 without requirement of a new written consent.
Participants
Eligibility criteria
Patients with a diagnosis of AMI type 1 [Citation9] and PCI performed according to prevailing guidelines [Citation10] at the time when the study was planned (2015) were eligible for participation [Citation7]. No limitations for age or LV systolic function were applied, but patients had to be stabilized for a representative echocardiographic examination before discharge.
Exclusion criteria
Exclusion criteria were hemodynamically unstable patients, ongoing atrial fibrillation / flutter, irregular heart rhythm, or anticipated inability to attend a second echocardiographic examination after 3 months, and life expectancy <2 years [Citation7].
Variables
Baseline BMI categories
Weight was measured to the nearest 1.0 kg during the pre-planned echocardiographic examination when patients were up and going, with inner clothes and without shoes. Height was self-reported. Normal weight was defined as BMI <25.0 kg/m2, overweight as BMI 25.0–29.9 kg/m2, and obesity as BMI ≥30.0 kg/m2. Elevated BMI was defined as BMI ≥25 kg/m2.
Echocardiographic measures
The echocardiography methods have been described in detail [Citation7]. In the present ancillary study we included baseline measurements of global longitudinal strain, left ventricular ejection fraction and left ventricular volume indexes as potential baseline predictors of outcomes.
Comorbidities, lifestyle measures and medication
All patient records were reviewed at baseline and during the entire follow-up study for the occurrence of comorbid diagnoses, including hypertension, cancer, type 2 diabetes (HbA1c ≥6.5% and/or treatment with antidiabetic drug), chronic inflammatory disease, chronic pulmonary disorders, and major abdominal surgery performed after index AMI.
Level of physical activity at follow-up was classified as low (30 min/week), medium (30–90 min/week) and high (>90 min/week). Present cardiovascular medication was assessed with emphasis on the use of betablockers (with dose equivalent with metoprolol), statins, angiotensin-converting enzyme inhibitors, diuretics, antidiabetic drugs and WL drugs.
Clinical outcomes
MACE was defined as either all-cause death or a non-fatal cardiovascular event. All non-fatal cardiovascular events were recorded, both from patients who subsequently died and from those who were alive at follow-up. MACE were assessed by two independent investigators who were blinded to baseline BMI and weight changes (VR, and JEO). Disagreements were solved by consensus.
Death was categorized as cardiovascular or non-cardiovascular by one investigator not involved in the results related to conduction of the study (JS, acknowledgment). In cases of doubt it was categorized as cardiovascular.
Non-fatal cardiovascular events were defined as first hospitalization for either reinfarction [Citation9], heart failure, angina pectoris requiring a new coronary angiogram confirming progression of coronary artery stenosis, stroke or a transitory ischemic attack.
Categorical WL was defined as any body weight reduction (> 0 kg) from baseline to follow-up. Self-reported body weight with inner clothes and without shoes, was applied for evaluation of weight. Intentional WL was defined as either self-reported explicit intention to lose weight and/or participation in a WL program. To assess any associations between degree of unintentional WL and MACE or comorbidities, those with unintentional WL were subdivided into three groups according to low (0–4.9%), moderate (5–9.9%) and large (≥10%) WL, or below versus at or above median WL.
Statistical analyses
Numerical data are presented as mean ± SD, and categorical data as number and percentages. In patients with more than one hospitalization for a non-fatal MACE, only the first event was included in the statistical analysis. The groups with normal weight, overweight or obesity at baseline were compared using analysis of variance or chi square tests as appropriate. The groups with either BMI < 25 kg/m2 or BMI ≥ 25 kg/m2 at baseline were compared using independent t-tests, chi square tests and Cox regression analysis, including hazard ratio (HR) with 95% confidence interval (CI). Logistic regression analysis was applied to calculate odds ratio (OR) with 95% CI where indicated. The WL (yes/no) groups, and the intentional versus unintentional WL groups were compared using independent samples t-tests or chi-square tests as appropriate. P-values < 0.05 were considered statistically significant. IBM SPSS version 29.0.0 was used for statistical analysis.
Results
Participants
A total of 289 patients were screened for inclusion, 53 were excluded, leaving 236 to be included in the analysis of baseline characteristics and clinical outcomes across BMI categories (Supplemental File 1). The main causes of exclusion were cardiac instability (n = 25), short life expectancy (n = 14) and ongoing atrial fibrillation (n = 9).
Further, during the prospective follow-up, 23 (10%) patients died, five patients did not participate in the telephone interviews, and one patient was excluded from the WL study due to a leg amputation. Consequently, 207 patients completed the telephone interview (Supplemental File 1).
Baseline characteristics
The baseline study cohort comprised 236 patients (24% women), all of Caucasian ethnicity, with a mean age of 64.9 ± 10.2 years, and a mean BMI 27.1 ± 4.3 kg/m2. 26% of the patients were categorized as normal weight, 47% as overweight and 27% as having obesity (). Patients with normal weight were on average 2 to 5 years older than patients with overweight and obesity respectively. Normal weight patients had a lower prevalence of type 2 diabetes and hypertension. The prevalence of cancer, chronic inflammatory disease, chronic obstructive pulmonary disease and current smoking was comparable between groups. The severity of AMI as expressed by Troponin T serum levels, time to PCI, angiographic findings, PCI procedures and echocardiographic assessment of left ventricular systolic function. Mean LVEF was 50 (8%), 60% of patients had a value ≥50% and 11 % had LVEF < 40%. Cardioprotective medication at discharge was comparable across BMI categories.
Table 1. Baseline characteristics of patients with normal weight, overweight and obesity.
MACE and mortality
Seventy-five of 236 patients (32%) had at least one MACE, defined as first event being death (n = 12) or non-fatal (n = 63). MACE were equally distributed between those with normal weight (31%), overweight (32%), and obesity (31%) at baseline (). Twenty-three patients died, including 11 who died from cardiovascular disease. The overall mortality rates between patients with normal weight, overweight or obesity did not differ significantly, but tended to be higher in the normal weight group (). Further, the proportions of patients with at least one non-fatal MACE or any new-onset comorbidity did not differ substantially across BMI-categories ().
Table 2. Major cardiovascular events (MACE) and new-onset comorbidities during follow-up among patients with normal weight, overweight and obesity.
Patients with overweight or obesity (BMI >25kg/m2) had a lower crude death rate during the 5-year follow-up (7.4% vs 16.4%, p = 0.049), but the relative hazard of death did not differ from those with normal weight, HR 0.50, 95% CI 0.22-1.15 (). Further, eight patients (4.6%) in the overweight/obesity-group developed new-onset cancer as compared with six patients (10.2%) in the normal weight-group, p = 0.201.
Table 3. Risk for major cardiovascular events (MACE) and new-onset co-morbidities during follow-up among patients with elevated body mass index (BMI) versus those with normal BMI at baseline.
Long-term WL
A total of 112 (54%) patients had a long-term WL (mean WL 7.6%) after PCI, while 95 (46%) patients had a stable weight or weight gain (mean weight gain 4.3%). Median body weight change was − 5.0 kg (95%CI −6.0 to −4.5) and 3.0 kg (95% CI 2.5 to 4.0), respectively. The two groups did not differ substantially regarding baseline BMI, age, gender distribution, medical history, smoking status, severity of AMI and echocardiographic findings (). Any intentional WL period was reported by 54% of WL patients versus 31% of those with no-WL (p = 0.001), while only a minority (<6%) in both groups had attended a structured WL program. The majority (>70%) of patients in both groups had participated in a cardiac rehabilitation program, and the self-reported physical activity levels were high in both groups (). The incidence of non-fatal MACE, current smoking and the proportions of patients with new-onset comorbidities or using cardioprotective medication, did not differ between groups (). A substantial WL (mean 13 ± 15 kg) was observed in a small group of patients (n = 7) who had undergone major abdominal surgery. None of the patients had used WL drugs.
Table 4. Demograpic and clinical characteristics of 207 patients at baseline and 5-year follow-up according to presence or absence of weight loss.
Intentional versus unintentional WL
A total of 61 (54%) of 112 patients with categorical WL reported an explicit intention to lose weight. The intentional WL group was approximately 6 years younger and 12 kg heavier than the unintentional WL group (). However, total body WL (%), comorbidities, smoking habits, physical activity, and the incidence of non-fatal MACE did not differ significantly between groups (). A sensitivity analysis excluding patients treated with an SGLT2-inhibitor and /or a GLP-analogue showed similar results (supplemental file 2). Notably, as shown in , the proportion of patients (n = 51) reporting unintentional WL was significantly higher in the normal weight group (82%) as compared with those with overweight (41%) or obesity (28%), p < 0.001. Accordingly, the odds of unintentional WL was approximately 8-fold higher in the normal weight group as compared with the combined overweight/obesity group, (OR 7.8, 95% CI 2.4-24.9). Further, five out of seven patients with chronic obstructive pulmonary disease at baseline had at least 5% unintentional WL. By contrast, the amount of unintentional WL was not associated with physical activity level, smoking habits, comorbidities or nonfatal MACE (, Supplemental files 3 and 4).
Figure 1. (A) Proportions (%) of patients with intentional or unintentional weight loss 5 years after PCI across baseline BMI categories. (B) Mean total body weight loss (%) in patients with intentional or unintentional weight loss 5 years after PCI across baseline BMI categories.
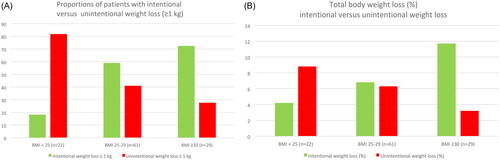
Table 5. Comparison of groups with either intentional or unintentional weight loss (n = 112).
In addition, the mean intentional total body WL (%) differed significantly between baseline BMI categories; normal weight 4.2%, overweight 6.8% and obesity 11.7%, respectively (p = 0.009) ().
Discussion
Obesity is an independent risk factor for coronary artery disease, and WL is recommended to reduce cardiovascular risk and improve long-term outcomes. Accordingly, it is difficult to understand that some lines of evidence indicate that patients with obesity treated with PCI have lower long-term mortality and reduced incidence of cardiovascular outcomes than their normal weight counterparts, and that WL after PCI may be associated with worse outcomes. We explored these apparent paradoxes in a 5-year follow-up study of patients with myocardial infarction who underwent PCI.
First, our results did not support the common notion that a normal BMI at time of PCI increases the risk of long-term MACE. Rather the contrary, approximately one out of three patients within all three BMI categories had at least one MACE during the 5-year follow-up. However, patients with overweight or obesity had a lower crude death rate than their normal weight counterparts even though the risk of death did not differ significantly. However, the relatively small number of patient deaths in the present study suggests that a survival benefit of overweight or obesity cannot be excluded.
Second, our study did not confirm any association between WL and long-term non-fatal MACE. Further, patients with or without long-term WL did not differ significantly regarding age, BMI, medical history, medical treatment, smoking habits, physical activity level, or comorbidities.
Third, the odds of unintentional WL were approximately 8-fold higher in the normal weight group. This finding may be of particular importance, since unintentional WL has been associated with increased all-cause mortality [Citation6]. However, since we do not have information about WL in the patients who died in the current study, we can only speculate that unintentional WL might have affected the mortality in the normal weight group.
Large meta-analyses and registries have supported the existence of an obesity paradox in coronary artery disease patients [Citation2–5, Citation11]. This is of importance since a relatively low body weight may be a manifestation of ill health, including heart failure and malignancy. However, in line with our results, recent large-scale studies [Citation12–14] did not verify the presence of an obesity paradox in patients treated with PCI. Al-Shaar et al. [Citation12] examined the relationship between BMI before and after AMI and did not find any survival benefit of adiposity in relation to risk of mortality in the Nurses Health study and Health Professionals Follow-up study. In a prospective German Drug-eluting stent registry [Citation13] similar rates of all-cause death and MACE were observed in a 1-year follow-up comparison between patients with normal weight, overweight and obesity. Also in the International RESOLUTE program, comprising five stent trials worldwide [Citation14], BMI at baseline was not found to have any impact on MACE 2 years after drug-eluting stent implantation. As evident from the aforementioned studies, the existence of an obesity paradox may still be regarded as controversial.
Influence on long term WL
The meta-analysis of Pack et al. [Citation6] showed that unintentional WL was associated with increased risk of adverse cardiovascular events. A large Swedish registry study [Citation15] included 1-year survivors aged < 75 years after MI (78.4% treated with PCI) and followed them up for 8.5 years, demonstrating that reduced BMI after 1 year was associated with higher long-term mortality, potentially being an indicator of deteriorated health. Further, Al-Shaar et al. [Citation12] found that a reduction of more than 4 BMI units was associated with increased mortality, and speculated that WL from before to after MI without lifestyle improvement may reflect reverse causation (WL due to underlying illness) and disease severity. Yui et al. [Citation16] enrolled patients 1 year after PCI and divided them into three grups by changes in BMI tertiles and followed them up for 4 years. The incidence of MACE was significantly higher in the reduced BMI group than the maintained and elevated groups. However, the results of the latter study are not comparable with ours as only 1-year survivors after PCI for any type of coronary artery disease were included, and, in addition, comorbidities at baseline and during follow-up were not reported [Citation16].
To our knowledge, the present study is the first to evaluate the association between clinical determinants (independent variables) with long term WL (dependent variable).
The apparently higher mortality rate in patients with normal BMI might have several explanations. The study population represents AMI survivors treated with PCI and discharged in a stable condition, with the majority having a preserved systolic left ventricular function. Therefore a number of early cardiac deaths has not been included, as reflected from less than 50% of deaths being classified as cardiovascular, as also reported by others [Citation17, Citation18]. This must be considered as a possible confounder in long-term assessment of the obesity paradox in PCI-treated post-AMI patients when using total mortality as an end-point. In addition, patients with normal weight were older than their heavier counterparts. On the other hand, the higher crude mortality in patients with normal BMI was counteracted by a higher incidence of non-fatal MACE among patients with overweight and obesity, resulting in nearly identical frequency of first MACE (1 out of 3 patients) across BMI-categories.
Further, the study population assessed for long term WL constituted survivors in stable condition after 5 years. Nevertheless, approximately one out of four had suffered at least one non-fatal MACE and 14% had developed comorbidities, potentially influencing weight changes. As opposed to our expectation, WL was not influenced by baseline BMI or the occurrence of subsequent MACE, with a potential “dietary effect” of a new hospitalization. Further, our expectations that WL would be associated with comorbidities at baseline or during follow-up were not fulfilled. Neither did our results reveal any differences in physical activity levels, smoking habits, or use of medical secondary prophylactic drugs.
Similarly, when comparing patients who reported intentional versus unintentional WL, we did not find any differences in physical activity level, smoking habits, co-morbidities or number of non-fatal MACE.
Limitations
The major limitations of this study are a relatively small sample size, low number of events, and the single- center design. We cannot rule out that some findings may be by chance. In addition, the population studied may represent a low-risk group, since it was restricted to clinical stable patients treated with early PCI after type 1 AMI, and the majority of patients had a LVEF ≥50%. Furthermore, follow-up weights were self-reported and may be inaccurate. However, a validation study has shown high correlations between self-reported and measured weight [Citation19].
Conclusions
The results of this clinical long-term follow-up study after PCI did not support any paradoxical association between normal weight at time of PCI and long-term MACE. Although normal weight patients had a higher crude mortality rate than their heavier counterparts, this difference could be partly explained by their older age. For long-term WL among survivors, patients with normal BMI had a significantly higher incidence of unintentional WL than those with elevated BMI, which may be of prognostic importance.
Author contributions
All authors contributed to the study conception and design. Medical preparation, data collection and data analysis were performed by JEO, VR, JM, TE and JH: The first manuscript was written by JEO and JH and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Supplemental Material
Download MS Word (139.1 KB)Acknowledgement
Dr. Joshua Ravindran has carefully analyzed the causes of death and subdivided them into cardiovascular or non-cardiovascular without knowledge of baseline BMI data.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from the corresponding author, [JEO], upon reasonable request.
Additional information
Funding
References
- Ellis SG, Elliot J, Horrigan M, et al. Low-normal or excessive body mass index: newly identified and powerful risk factors for death and other complications with percutaneous coronary intervention. Am J Cardiol. 1996;78(6):642–646. doi: 10.1016/s0002-9149(96)00386-4.
- Holroyd EW, Sirker A, Kwok CS, et al. The relationship of body mass index to percutaneous coronary intervention outcomes: does the obesity paradox exist in contemporary percutaneous coronary intervention cohorts? Insights from the British cardiovascular intervention society registry. JACC Cardiovasc Interv. 2017;10(13):1283–1292. doi: 10.1016/j.jcin.2017.03.013.
- Wang ZJ, Zhou YJ, Galper BZ, et al. Association of body mass index with mortality and cardiovascular events for patients with coronary artery disease; a systematic review and meta-analysis. Heart. 2015;101(20):1631–1638. doi: 10.1136/heartjrnl-2014-307119.
- Wolny R, Maehara A, Liu Y, et al. The obesity paradox revisited: body mass index and long-term outcomes after PCI from a large pooled patient-level database. EuroIntervention. 2020;15(13):1199–1208. doi: 10.4244/EIJ-D-19-00467.
- Alhuneafat L, Jabri A, Abu Omar Y, et al. Relationship between body mass index and outcomes in acute myocardial infarction. J Clin Med Res. 2022;14(11):458–465. doi: 10.14740/jocmr4818.
- Pack QR, Rodriguez-Escudero JP, Thomas RJ, et al. The prognostic importance of weight loss in coronary artery disease: a systematic review and meta-analysis. Mayo Clin Proc. 2014;89(10):1368–1377. doi: 10.1016/j.mayocp.2014.04.033.
- Otterstad JE, Norum IB, Ruddox V, et al. Prognostic impact of non-improvement of global longitudinal strain in patients with revascularized acute myocardial infarction. Int J Cardiovasc Imaging. 2021;37(12):3477–3487. doi: 10.1007/s10554-021-02349-2.
- Peersen K, Munkhaugen J, Gullestad L, et al. The role of cardiac rehabilitation in secondary prevention after coronary events. Eur J Prev Cardiol. 2017;24(13):1360–1368. doi: 10.1177/2047487317719355.
- Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J. 2012;33(20):2551–2567. doi: 10.1093/eurheartj/ehs184.
- Windecker S, Koth P, Alonso F, et al. 2014 ESC/EACTS guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35(37):2541–2619.
- Liu S-H, Lin Y-Z, Han S, et al. The obesity paradox in ST-segment elevation myocardial infarction patients: a meta-analysis. Ann Noninvasive Electrocardiol. 2023;28(2):e13022. doi: 10.1111/anec.13022.
- Al-Shaar L, Li Y, Rimm EB, et al. Body mass index and mortality among adults with incident myocardial infarction. Am J Epidemiol. 2021;190(10):2019–2028. https://academic.oup.com/aje/article/190/10/2019/6255430 doi: 10.1093/aje/kwab126.
- Akin I, Tölg R, Hochadel M, et al. No evidence of “obesity paradox” after treatment with drug-eluting stents in a routine clinical practice: results from the prospective multicenter German DES.DE (German Drug-Eluting Stent) Registry. JACC Cardiovasc Interv. 2012;5(2):162–169. doi: 10.1016/j.jcin.2011.09.021.
- Diletti R, Garcia-Garcia HM, Bourantas C, et al. Impact of body mass index on long-term clinical outcomes after second-generation drug-eluting stent implantation: insights from the international global RESOLUTE program. Catheter Cardiovasc Interv. 2015;85(6):952–958. doi: 10.1002/ccd.25828.
- Berglund L, Risérus U, Hambraeus K. Repeated measures of body mass index and waist circumference in the assessment of mortality risk in patients with myocardial infarction. Ups J Med Sci. 2019;124(1):78–82. doi: 10.1080/03009734.2018.1494644.
- Yui H, Ebisawa S, Miura T, et al. Impact of changes in body mass index after percutaneous coronary intervention on long-term outcomes in patients with coronary artery disease. Heart Vessels. 2020;35(12):1657–1663. doi: 10.1007/s00380-020-01648-3.
- Yamashita Y, Shiomi H, Morimoto H, et al. Cardiac and non-cardiac causes of long-term mortality in ST-segment-elevation acute myocardial infarction patients who underwent primary percutaneous coronary intervention. Circ Cardiovas Qual Outcomes. 2017;10(1):e002790.
- Brener SJ, Tarantini G, Leon MB, et al. Cardiovascular and noncardiovascular death after percutaneous coronary intervention: insights from 32 882 patients enrolled in 21 randomized trials. Circ Cardiovasc Interv. 2018;11(7):e006488. doi: 10.1661/CIRCINTERVENTIONS.118.0064881.
- Rimm EB, Stampfer MJ, Colditz GA, et al. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1(6):466–473. doi: 10.1097/00001648-199011000-00009.
