ABSTRACT
Evidence is growing to support mind-body practices (e.g. yoga) as a therapeutic intervention for many health conditions. In the UK, yoga is promoted as a social prescription asset by the National Health Service (NHS), yet the factors influencing its implementation are poorly understood. This study explored the attitudes, knowledge and understanding of mind-body practices as a social prescribing asset amongst health science populations within higher education. Twenty-six health science staff and students completed an online questionnaire. Data analysis used a mixed-methods approach, employing thematic analysis for qualitative data and calculating the net promoter score (NPS) to assess participants’ inclination to recommend mind-body practices as a social prescribing asset. Nineteen participants (73%) were aware of the term ‘social prescription’ and understood it to be a non-clinical, community-based alternative to medication. Whilst participants were aware of the physical benefits of mind-body practices, particularly yoga, they lacked awareness of the social, emotional, and spiritual benefits. Although 42% of participants would recommend mind-body practices as a social prescribing asset (NPS of 15), the opposite was true for yoga (NPS of −15), potentially due to poor knowledge or personal engagement with yoga. This study underlines the importance of increasing understanding and promoting yoga as an adjuvant mind-body practice to achieve social, emotional, and spiritual benefits. Implementing educational strategies to increase knowledge of mind-body practices and yoga, with a focus on social prescribing practice, may help to improve future referral pathways in practice in line with the NHS long term plan.
Introduction
Mind-body practices include activities intending to use the mind to impact physical functioning and improve health (e.g. Yoga, Tai Chi, Qigong, mindfulness, and deep breathing) (Kim et al. Citation2013; Simkin and Black Citation2014). Having increased in popularity in the last 20 years, yoga is a complex therapeutical intervention consisting of physical movements, postures, breathing techniques, meditation, visualisation, and philosophical foundations (Chetry, Telles, and Balkrishna Citation2021; Field Citation2011; McCall et al. Citation2013). Between 2011 and 2020 alone, almost four thousand scientific yoga-based publications were added to PubMed, with research from the United States, United Kingdom and India dominating publications (Chetry, Telles, and Balkrishna Citation2021) and participants spanning 29 different countries (Jeter et al. Citation2015). Yoga is commonly used in the UK to support self-care and manage health conditions (Cartwright et al. Citation2020) and has been shown to moderate stress, increase physical activity levels, and enhance wellbeing (Büssing et al. Citation2012; Pascoe and Bauer Citation2015). Additionally, yoga practice is an effective and safe therapeutic intervention for people with high blood pressure, cardiovascular disease, type 2 diabetes, aches and pains, depression, and anxiety (Field Citation2011; McCall et al. Citation2013).
Yoga practice in the UK significantly increased in popularity between 1997–2008, with Hatha (28%), Iyengar (26%), and Vinyasa (15%) being some of the most popular yoga forms practised (Ding and Stamatakis Citation2014; Hasselle-Newcombe Citation2005; Nalbant, Lewis, and Chattopadhyay Citation2022). Despite the absence of more current data, in 2004 and it was estimated that the number of yoga practitioners in the UK surpassed 2.5 million (Mace and McCulloch Citation2020; Newcombe Citation2019), with it often being provided and practised by white well-educated women (Cartwright et al. Citation2020; Cramer et al. Citation2016; Ding and Stamatakis Citation2014; Nalbant, Lewis, and Chattopadhyay Citation2022; Park, Braun, and Siegel Citation2015). In contrast with global western countries, in India primarily men with high-school education practice yoga, highlighting contrasting cultural and motivational differences (Telles et al. Citation2017). The practice of yoga in western societies, has focussed on fitness practice rather than one that cultivates transcendental states of spirituality (Brems et al. Citation2016; Hasselle-Newcombe Citation2005; Ivtzan and Jegatheeswaran Citation2015). In the UK, the largest proportion of time is allocated to yogic poses or asana (59%) whilst not including many of the more holistic aspects of yoga that are practised in South Asian countries, such as breathing practices or pranayama (18%), relaxation practices and meditation or dhyana (12%) (Nalbant, Lewis, and Chattopadhyay Citation2022). However, it has been shown that practitioners with spiritual intentions tend to report significantly higher psychological wellbeing (Ivtzan and Jegatheeswaran Citation2015), suggesting the need for western countries to emphasise the Indian-rooted holistic vision of yoga and other mind-body practices (Freeman et al. Citation2017).
Social prescribing enables general practitioners (GPs) and other health and community based staff or link workers to refer or connect people to non-clinical services and support assets in the community (Muhl et al. Citation2023). Social prescribing link workers, afford the opportunity for individuals to co=produce a personalised care and support plan that matters to them in order to empower them to take control of their wellbeing (NHS England Citation2024). It offers a formal route for referring patients to non-clinical holistic support services (Bickerdike et al. Citation2017). Due to its mental and physical health benefits, the UK National Healthcare Services (NHS) promotes yoga as a safe and feasible asset that individuals may be referred to as part of social prescribing (Cheshire, Richards, and Cartwright Citation2022; Mason, Schnackenberg, and Monro Citation2017). However, the effectiveness of such programmes in the NHS is uncertain because of the lack of high-quality evidence to support them (Bickerdike et al. Citation2017).
Yoga is a highly acceptable and appropriate intervention that brings several biopsychosocial benefits through social prescription with physical and mental health benefits, social connectedness, patient activation and positive lifestyle changes evidenced (Cartwright et al. Citation2019; Cheshire, Richards, and Cartwright Citation2022). Whilst evidence supports yoga as an asset for social prescribing, there are still barriers that could lead practitioners to avoid implementation (Cheshire, Richards, and Cartwright Citation2022). Health professionals who are unaware/less aware of the benefits of yoga, have been shown to be less likely to refer individuals to such services (Brems Citation2020; Sulenes et al. Citation2015). Students in healthcare programs in the UK have previously perceived yoga as primarily a fitness practice, leaving aside the holistic perspective embedded in the foundations of yoga philosophy (Brems et al. Citation2016). The most common barriers to yoga practice among health professional students have been reported as time, cost, lack of information about accessibility, and stereotypes related to typical yoga practitioners (Brems et al. Citation2015). Further research is needed to explore attitudes towards mind-body practices for social prescribing to begin to develop effective wider adoption. This study explored the attitudes, knowledge and understanding of mind-body practices as an asset for social prescribing amongst health science students and staff.
Methods
Participant recruitment
Purposive sampling methods were used to recruit staff and students from a UK university who were enrolled or teaching in health science programmes where social prescribing is practised within the profession and embedded within the curriculum (e.g. dietetics, speech & language therapy, occupational therapy, and physiotherapy). All participants were aged 18 years or over and gave written informed consent to participate. Data collection conformed to the declaration of Helsinki (World Medical Association Citation2018) and data protection principles. Ethical approval was granted through the University Health Ethics Committee (HEALTH 0377).
Data collection procedure
An exploratory mixed-methods anonymised questionnaire-based study was designed using Microsoft Forms. Some questions were rooted/branched and therefore a response was not required by everyone for every question.
Data and statistical analysis
Qualitative data, from open-ended questions were analysed using manual coding for thematic analysis and an inductive approach was adopted, allowing the data to generate themes (Braun and Clarke Citation2006; Saunders et al. Citation2018).
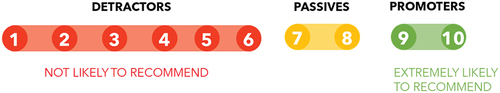
Two questions examined the likelihood of participants recommending any type of mind-body practice to a patient as an asset for social prescribing. The net promoter score (NPS) is a metric commonly used in marketing and business, but also used in healthcare services to represent practitioners’ and patients’ experiences (Ganguly and Moustafa Citation2019; Stirling et al. Citation2018). As represented in , it assumes a subdivision of respondents into ‘promoters’ (ratings of 9–10), ‘passives’ (ratings of 7–8), and ‘detractors’ (ratings of 1–6). NPS is based on a scale of −100 to 100%, where positive values indicate willingness to recommend the intervention, while negative values indicate the opposite (Stirling et al. Citation2018). The NPS was calculated from the results of this question using the following formula:
NPS = (% of promoters) - (% of detractors)
One-way chi-squared tests were used to determine whether significantly more respondents selected a question category more often. Two-way Pearson chi-square tests of independence were used to undertake bivariate cross-tabulation comparisons, specifically to test differences in responses to each question between demographic/individual characteristic variables (gender, level of education, patient-facing role, university status). Statistical significance was set at p ≤ 0.05.
Results
Participants
Twenty-six participants completed the questionnaires ().
Table 1. Participant demographics and characteristics (n = 26).
Social prescription
Participants were asked to describe their understanding of social prescription. After the thematic analysis, three core themes were identified: lack of awareness, non-clinical community alternatives, and health benefits.
Lack of awareness
Seven participants seemed unaware or unsure of the concept of ‘social prescription’. Three participants reported a poor understanding regarding the concept.
I don’t really know what it is … (P2)
Not a term I think I have heard … (P3)
Not sure. (P4)
Non-clinical community alternative
Healthcare professionals were mentioned as those in charge of making referrals and linking the health system with community services. Most participants identified the social prescribing activities as community or local-based services.
Linking medical care to well-being services in the community. (P7)
The use of community and non-clinical services to support people’s health and wellbeing, as prescribed by a GP. (P1)
These activities were proposed as an alternative to medication in a non-clinical setting, matching people’s interests with local activities.
Suggesting certain services which will suit different individuals. Keeping them well and out of hospital services. (P12)
… Prescribing activities rather than medication. (P3)
Health benefits
Social prescription was mostly linked to achieving health benefits, promoting wellness and supporting management of health conditions.
An attempt to match people’s interests with activities in their local area in order to positively impact their health & wellbeing. (P11)
… these things would build their social skills, self-esteem, improve mental wellbeing and can improve physical health too. (P18)
Mind-body practices
Participants were asked to describe their understanding of mind-body practices. Three core themes were identified: mind-body relationship, mind-body health benefits, and lack of awareness.
Mind-body relationship
Sixteen participants recognised the reciprocal interaction and connection between the mind and body, meaning that mind-body practices involve both components to pursue a balance between both.
I think it means practices in which you are consciously using both the mind and the body and in which these become in sync. (P2)
Taking a holistic approach to working with others/oneself by undertaking practices that have an impact on both the body & the mind - they are interlinked & the health of one is dependent on the health of the other. (P11)
Accordingly, mind-body practices were acknowledged as holistic approaches with some participants also highlighting how such practices raised awareness of the body.
Mind-body health benefits
Health benefits were attributed to mind-body practice by most participants. Some participants specified benefits for physical, psychological and/or emotional health, while others mentioned concepts such as overall health and wellbeing. Few participants mentioned a connection between mind-body practices and disease or pain relief:
Mindfulness and relaxation is very important when someone has a long-term condition or disability or undergoing treatment for a serious illness. (P18)
Holistic methods of healthcare, not looking at one symptom but looking at the whole body to look at the cause and cure of ill health. (P23)
Relaxation was the most common health benefit specifically recounted (n = 6).
Lack of awareness
A greater proportion of the participants were unaware or unsure of the concept of ‘social prescription’ compared to ‘mind-body practices’. While most of the participants were familiar with the term ‘mind-body practices’, two participants stated that they were not sure or were unaware of the term, while another three named some examples of practices that were familiar to them:
I don’t know much about it. Only examples I can think of are yoga and mindfulness. (P17)
I’ve not heard the term before. (P3)
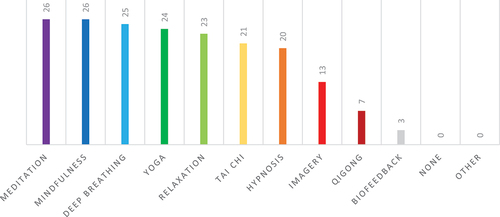
Almost half of the participants provided an example of a mind-body practice in the open question, where yoga and mindfulness were the most mentioned by all participants recognised meditation and mindfulness as mind-body practices, with yoga known by 24 participants (92%) ().
Additional benefits of mind-body practices
The benefits of mind-body practices to wellbeing reported by the participants included benefits to mental health (n = 13), physical health (n = 4) and a combination of both (n = 10).
Wellbeing can’t just be physical or mental. It must be both. (P6)
Increased wellbeing both physically and mentally. Healthy life choices, reduced tiredness, increase self of self-esteem etc. (P14)
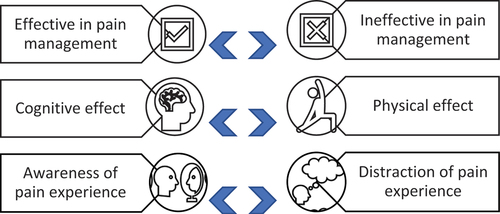
Participants were asked to give their opinion about the benefits of mind-body practices for pain management. Of the 26 participants, five didn’t answer due to uncertainty. The remaining answers showed opposing opinions on this topic ().
Most participants stated that mind-body practices can help reduce pain (n = 15).
Reduce pain you may feel. (P4)
Natural pain relief (P11)
In contrast, three participants mentioned that mind-body practices could not be the optimal option for pain management in every case:
I don’t think many people could benefit from mind-body management. (P25)
Care should be taken to monitor effectiveness for the person and shouldn’t be denied other routes, e.g., medical, if mind-body techniques are not managing the pain well. (P19)
Whilst most people attributed the benefits of pain management to a cognitive effect, four participants attributed it to physical impacts such as increased flexibility and muscle strength.
According to eight participants, awareness, acknowledgment, and acceptance of the pain experience could improve your resilience and help you ease the pain, incrementing the connection between mind and body:
… I think that if you accept what is happening sometimes this can ease pain. (P2)
Possibly people can work through reducing the amount pain perception affects them, changing perception of pain, or simply learning how to accept and work with pain. (P19)
This could be contrasted to the idea that mind-body practices help as a distraction, taking your mind away from the pain, supported by four participants:
Distraction helps pain management (P20)
I would presume it can take your mind of the pain and dependant on exercise could improve it if that is a prescribed way (P21)
Attitudes to yoga
When participants were asked to report their thoughts about yoga, most (n = 16) were aware of the benefits to health and quality of life. Six participants directed the answer straight to their own positive experience with yoga. Interestingly, seven people identified some common barriers towards yoga practice, including accessibility issues due to cost, personal capabilities, or difficulty as a beginner. Participant 25 highlighted the potential stigma around yoga and its participants:
it is very beneficial for many people of a variety of ages and health/fitness levels, but many people have a pre-conceived idea of what yoga is and who does yoga, and typically they are wrong, and this will probably stop them from participating in yoga. (p25)
Are there benefits of yoga?
Multiple benefits of yoga practice were reported by the participants, including physical (n = 25), psychological (n = 25), social (n = 4), emotional (n = 2) and spiritual (n = 2) factors. Among physical outcomes, musculoskeletal, cardiorespiratory, and metabolic benefits were highlighted. Most common responses included flexibility, muscle strength, motor function, balance, and posture improvements as the main musculoskeletal benefits. For psychological benefits, relaxation effects, body awareness and mindfulness, and reduction of stress and anxiety were the most common answers.
Perceived yoga benefits through social prescription
In contrast to the previous question, social benefits were the most common benefit of yoga through social prescription reported by the participants (n = 10). Two participants specified the advantage of being able to learn a new activity while being immersed in a community setting:
Education for those who do not already know anything about it. Access to a local group. (P20)
As above, exercise that can be calm so can be used for most people, community, learning something new. (P21)
Interestingly, five participants highlighted the benefit for the healthcare system, where yoga through social prescription has the potential to reduce the overuse of clinical resources when appropriately referred:
Health and well-being benefits could reduce need for health specific referrals. (P9)
Potentially a highly beneficial non-clinical option under the right circumstances. (P15)
Yoga practice as personal experience
Participants were asked about their yoga experience. Eleven of them (42%) had never practised yoga. Eight participants (31%) had practised yoga in the past but were no longer practising it, while seven (27%) were actively practising it at the time of completing the questionnaire. Of the 15 participants that had yoga experience, 20% practised it daily, 67% weekly and 13% monthly.
Hatha yoga (n = 5) and Vinyasa yoga (n = 2) were most practised amongst participants. Two participants mentioned that they practised or preferred a variety of different yoga types, three participants mentioned other types of yoga (group sessions, Bikram yoga, Ujjayi breath yoga), while the remaining three participants did not know or did not have a specific preference.
The main reason for practising yoga was to achieve simultaneous physical and psychological benefits (n = 5). Four participants reported practising yoga as a stress and anxiety reliever. Two of them sought physical benefits through yoga, such as injury risk and pain reduction. Other motives included pregnancy, costs, a requirement for a previous course and trying something different.
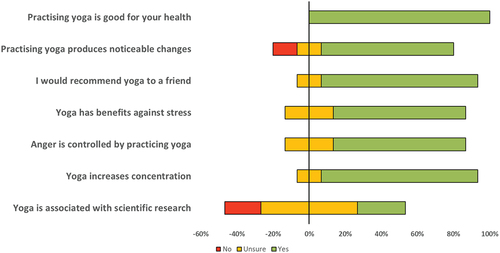
The final seven questions were aimed at understanding the attitudes and understanding towards yoga of participants with yoga experience (). All participants (100%, n = 15) agreed that yoga was good for health. The majority (73%, n = 11) found noticeable changes following yoga practice. Finally, half of the participants (53%, n = 8) were unsure about the scientific background existing around yoga.
After statistical analysis, positive responses were selected significantly more frequently for three of the questions: noticeable changes produced by yoga, recommend yoga to a friend, and yoga increased concentration (p = 0.005). A complete agreement was found regarding yoga practice as beneficial for health (100% Yes). No significant differences in positive/negative responses were found for the benefits of yoga against stress, anger control, or the association between yoga and scientific research (p < 0.05). Furthermore, there were no differences in responses to each question between demographic/individual characteristic variables, including the level of education, patient-facing role, or university status (p > 0.05).
Practice recommendations
Most participants gave promoting answers (42%) when asked to rate the likelihood that they would recommend any mind-body practice to a patient as an asset for social prescribing, whilst 27% provided detracting answers. An NPS of 15 indicated that participants were promoters of mind-body practices as an asset for social prescribing. In contrast, participants responded more negatively when asked whether they would recommend yoga specifically, with more detractors (42%) than promoters (27%) and an NPS of −15. However, no statistical significance was seen between the recommendation of mind-body practices and yoga recommendation questions (p = 0.607).
Discussion
This study aimed to explore the attitudes, knowledge and understanding of mind-body practices as an asset for social prescribing amongst health science students and staff.
Social prescribing in higher education
Santoni et al. (Citation2019) had previously found a lack of awareness regarding social prescribing amongst UK medical students (93%, n = 848). Interestingly, after teaching sessions aimed to explain social prescribing, raise awareness through peer-to-peer teaching, and evaluate current knowledge and awareness of social prescribing, 98% of participants (n = 895) considered the session’s content as useful and relevant to their future careers (Santoni et al. Citation2019). The results of the present study suggested that 19 participants (73%) were aware of the term ‘social prescription’, and understood it to be a non-clinical, community-based alternative to medication. However, to increase implementation, the importance of incorporating social prescribing education for health science staff/students is still evident, given the disparity between the present study and previous research (Santoni et al. Citation2019).
Mind-body practice in higher education
All participants recognised examples of ‘mind-body practices’, and those familiar with the term described it as ‘holistic approaches with benefits for both physical and mental health’. Participants gave mixed opinions on the mechanism of pain management through mind-body practices. Previous evidence has indicated that mind-body practice can be useful in treating pain-related medical conditions (Astin Citation2004; Cherkin et al. Citation2014; Garland et al. Citation2020). Multicomponent mind-body practices (e.g. stress management, coping skills training, cognitive restructuring, and relaxation therapy) may have the potential to improve outcomes as an adjuvant therapy for multiple conditions (e.g. chronic low back pain, rheumatoid arthritis, osteoarthritis, and cancer) (Astin Citation2004; Astin et al. Citation2002; Powers Citation1999; van Tulder et al. Citation2000). Additional benefits may include strategies for management of stress and chronic pain conditions, greater psychophysiological regulation, enhancing a sense of control and self-efficacy (Astin Citation2004; Bandura et al. Citation1987). Using social prescribing education as a springboard, it is imperative to continue to develop models for integrating these adjuvant mind-body practices into our health care and education systems (Dossett, Fricchione, and Benson Citation2020).
Yoga as a mind-body practice
Participants in this study were aware of the evidenced benefits of practising yoga, particularly the physical and psychological benefits (Büssing et al. Citation2012). In agreement with previous research, which identified improvements in social connectedness, social benefits were identified in the present study as the most common (38%) benefit of yoga social prescription (Cheshire, Richards, and Cartwright Citation2022). Results underline the importance of understanding and promoting yoga to health science students as an adjuvant mind-body practice to achieve social, emotional, and spiritual benefits (Ivtzan and Jegatheeswaran Citation2015). Whilst the health benefits have not been fully realised amongst staff/students, further promotion of community-based initiatives may help promote use to alleviate the burden on the NHS in the NHS long-term plan (NHS Citation2019).
Of the participants who had yoga experience, the main reason for practising yoga was to simultaneously achieve physical and psychological benefits, with stress and anxiety relief being a common motive. In contrast to the present study, motivators to yoga practice among health professions staff/students reported in literature also included health promotion, emotional well-being, athleticism, and pain relief, alongside seeking a sense of community (Brems et al. Citation2015). Hatha and Vinyasa yoga were identified as the most common forms of yoga practised by participants on a weekly basis, in agreement with previous UK based studies (Cartwright et al. Citation2020; Nalbant, Lewis, and Chattopadhyay Citation2022). Whilst Hatha yoga focuses on yoga as a mind-body practice, Vinyasa has a more physical focus; therefore, it remains imperative that the comprehensive benefits of yoga as a mind-body practice are further educated.
A perceived lack of scientific research or evidence-based guidelines has been previously considered a key barrier to social prescribing recommendations (Southby and Gamsu Citation2018). Despite having a positive attitude towards yoga, over half of the participants (53%) were unsure about the scientific background of yoga. Lack of familiarity with yoga research has been previously reported in half of the healthcare professionals included in a study aiming to investigate their perceptions of yoga for health and their openness to recommending yoga to patients (Smit and Cartwright Citation2023). To address the perceived lack of scientific research in yoga and evidence-based guidelines in social prescribing recommendations, tailored educational tools for staff and students may better support evidence-based implementation by future health care practitioners (NHS Citation2019).
Knowledge for patient benefit and clinical practice
In contrast to a recent study that concluded that healthcare practitioners in the UK were open and motivated to recommend yoga to patients (Smit and Cartwright Citation2023), the present study showed most participants were promoters of mind-body practices but not of yoga as an asset for social prescribing. The experience of practitioners and higher levels of personal engagement or experience with yoga may explain the greater likelihood of recommending yoga in this previous study compared to the present study (Smit and Cartwright Citation2023; Sulenes et al. Citation2015). However, as the present study focused on staff and students, further benefit may be gained in future clinical practice if social prescribing and mind-body practice education are to be better embedded into educational programmes.
Whilst this study highlighted the key gaps in higher education around social prescribing to mind-body practices and yoga, it is not without limitations. Notably, the purposive sampling from a single higher education institution in the UK cannot be considered as fully representative. Future exploratory studies may consider utilising a cross-university design, affording sub-grouped analysis according to participant characteristics, which may help to further inform the potential use of social prescribing education as a means of improving future uptake of community-based interventions. Due to the nature of health science courses, it is possible that the representation within this study is skewed towards those who identify as female. However, limited evidence from one NHS trust in the UK suggests that this may be reflective of practice, with 70% of staff within allied health professions being female, with occupational therapy, dietetics and speech and language therapy being upwards of 90% female (Eddison and Leslie Citation2022).
Conclusions
Although there is awareness of the benefits of mind-body practices and yoga, gaps in knowledge amongst staff and students within higher education health science programmes still exist. Greater recommendation of mind-body practices such as yoga as an adjuvant therapy is key to effective self-management of long-term conditions. Educating future practitioners may increase social prescription through NHS referral pathways and increase community healthcare initiatives, in line with the NHS long-term plan (NHS Citation2019).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Astin, J. A. 2004. “Mind–Body Therapies for the Management of Pain.” The Clinical Journal of Pain 20 (1): 27–32. https://doi.org/10.1097/00002508-200401000-00006.
- Astin, J. A., W. Beckner, K. Soeken, M. C. Hochberg, and B. Berman. 2002. “Psychological Interventions for Rheumatoid Arthritis: A Meta‐Analysis of Randomized Controlled Trials.” Arthritis Care & Research 47 (3): 291–302. https://doi.org/10.1002/art.10416.
- Bandura, A., A. O’Leary, C. B. Taylor, J. Gauthier, and D. Gossard. 1987. “Perceived Self-Efficacy and Pain Control: Opioid and Nonopioid Mechanisms.” Journal of Personality and Social Psychology 53 (3): 563–571. https://doi.org/10.1037/0022-3514.53.3.563.
- Bickerdike, L., A. Booth, P. M. Wilson, K. Farley, and K. Wright. 2017. “Social Prescribing: Less Rhetoric and More Reality. A Systematic Review of the Evidence.” British Medical Journal Open 7 (4): e013384. https://doi.org/10.1136/bmjopen-2016-013384.
- Braun, V., and V. Clarke. 2006. “Using Thematic Analysis in Psychology.” Qualitative Research in Psychology 3 (2): 77–101. https://doi.org/10.1191/1478088706qp063oa.
- Brems, C. 2020. “Yoga as a Mind-Body Practice.” In Nutrition, Fitness, and Mindfulness: An Evidence-Based Guide for Clinicians, edited by J. Uribarri and J. A. Vassalotti, 137–155. Springer International Publishing. https://doi.org/10.1007/978-3-030-30892-6_10.
- Brems, C., D. Colgan, H. Freeman, J. Freitas, L. Justice, M. Shean, and K. Sulenes. 2016. “Elements of Yogic Practice: Perceptions of Students in Healthcare Programs.” International Journal of Yoga 9 (2): 121. https://doi.org/10.4103/0973-6131.183710.
- Brems, C., L. Justice, K. Sulenes, L. Girasa, J. Ray, M. Davis, J. Freitas, M. Shean, and D. Colgan. 2015. “Improving Access to Yoga: Barriers to and Motivators for Practice Among Health Professions Students.” Advances in Mind-Body Medicine 29 (3): 6–13.
- Büssing, A., A. Michalsen, S. B. S. Khalsa, S. Telles, and K. J. Sherman. 2012. “Effects of Yoga on Mental and Physical Health: A Short Summary of Reviews.” Evidence-Based Complementary and Alternative Medicine 2012:1–7. https://doi.org/10.1155/2012/165410.
- Cartwright, T., H. Mason, A. Porter, and K. Pilkington. 2020. “Yoga Practice in the UK: A Cross-Sectional Survey of Motivation, Health Benefits and Behaviours.” British Medical Journal Open 10 (1): e031848. https://doi.org/10.1136/bmjopen-2019-031848.
- Cartwright, T., R. Richards, A. Edwards, A. Cheshire, T. Cartwright, R. Richards, A. Edwards, and A. Cheshire. 2019. “Yoga4Health on Social Prescription: A Mixed Methods Evaluation.” University of Westminster.
- Cherkin, D. C., K. J. Sherman, B. H. Balderson, J. A. Turner, A. J. Cook, B. Stoelb, P. M. Herman, R. A. Deyo, and R. J. Hawkes. 2014. “Comparison of Complementary and Alternative Medicine with Conventional Mind–Body Therapies for Chronic Back Pain: Protocol for the Mind–Body Approaches to Pain (MAP) Randomized Controlled Trial.” Trials 15 (1): 211. https://doi.org/10.1186/1745-6215-15-211.
- Cheshire, A., R. Richards, and T. Cartwright. 2022. “‘Joining a Group Was inspiring’: A Qualitative Study of Service users’ Experiences of Yoga on Social Prescription.” BMC Complementary Medicine and Therapies 22 (1). https://doi.org/10.1186/s12906-022-03514-3.
- Chetry, D., S. Telles, and A. Balkrishna. 2021. “A PubMed-Based Exploration of the Course of Yoga Research from 1948 to 2020.” International Journal of Yoga Therapy 31 (1). https://doi.org/10.17761/2021-D-21-00017.
- Cramer, H., L. Ward, A. Steel, R. Lauche, G. Dobos, and Y. Zhang. 2016. “Prevalence, Patterns, and Predictors of Yoga Use.” American Journal of Preventive Medicine 50 (2): 230–235. https://doi.org/10.1016/j.amepre.2015.07.037.
- Ding, D., and E. Stamatakis. 2014. “Yoga Practice in England 1997-2008: Prevalence, Temporal Trends, and Correlates of Participation.” BMC Research Notes 7 (1): 172. https://doi.org/10.1186/1756-0500-7-172.
- Dossett, M. L., G. L. Fricchione, and H. Benson. 2020. “A New Era for Mind–Body Medicine.” New England Journal of Medicine 382 (15): 1390–1391. https://doi.org/10.1056/NEJMp1917461.
- Eddison, N., and R. Leslie. 2022. The Challenge of Diversity in Allied Health Professionals. https://ihm.org.uk/2022/06/08/the-challenge-of-diversity-in-the-allied-health-professions-by-dr-nicky-eddison-and-dr-ros-leslie/.
- Field, T. 2011. “Yoga Clinical Research Review.” Complementary Therapies in Clinical Practice 17 (1): 1–8. https://doi.org/10.1016/j.ctcp.2010.09.007.
- Freeman, H., N. Vladagina, E. Razmjou, and C. Brems. 2017. “Yoga in Print Media: Missing the Heart of the Practice.” International Journal of Yoga 10 (3): 160. https://doi.org/10.4103/ijoy.IJOY_1_17.
- Ganguly, P., and A. A. Moustafa. 2019. “A Survey Proposal Towards Holistic Management of Schizophrenia.” International Journal of Psychological and Behavioral Sciences 13 (4): 164–168.
- Garland, E. L., C. E. Brintz, A. W. Hanley, E. J. Roseen, R. M. Atchley, S. A. Gaylord, K. R. Faurot, J. Yaffe, M. Fiander, and F. J. Keefe. 2020. “Mind-Body Therapies for Opioid-Treated Pain.” JAMA Internal Medicine 180 (1): 91. https://doi.org/10.1001/jamainternmed.2019.4917.
- Hasselle-Newcombe, S. 2005. “Spirituality and “Mystical Religion” in Contemporary Society: A Case Study of British Practitioners of the Iyengar Method of Yoga.” Journal of Contemporary Religion 20 (3): 305–322. https://doi.org/10.1080/13537900500249806.
- Ivtzan, I., and S. Jegatheeswaran. 2015. “The Yoga Boom in Western Society: Practitioners’ Spiritual Vs. Physical Intentions and Their Impact on Psychological Wellbeing.” Journal of Yoga & Physical Therapy 5 (3). https://doi.org/10.4172/2157-7595.1000204.
- Jeter, P. E., J. Slutsky, N. Singh, and S. B. S. Khalsa. 2015. “Yoga As a Therapeutic Intervention: A Bibliometric Analysis of Published Research Studies from 1967 to 2013.” The Journal of Alternative and Complementary Medicine 21 (10): 586–592. https://doi.org/10.1089/acm.2015.0057.
- Kim, S. H., S. M. Schneider, L. Kravitz, C. Mermier, and M. R. Burge. 2013. “Mind-Body Practices for Posttraumatic Stress Disorder.” Journal of Investigative Medicine 61 (5): 827–834. https://doi.org/10.2310/JIM.0b013e3182906862.
- Mace, J. L., and S. P. McCulloch. 2020. “Yoga, Ahimsa and Consuming Animals: UK Yoga teachers’ Beliefs About Farmed Animals and Attitudes to Plant-Based Diets.” Animals 10 (3): 480. https://doi.org/10.3390/ani10030480.
- Mason, H., N. Schnackenberg, and R. Monro. 2017. “Yoga and Healthcare in the United Kingdom.” International Journal of Yoga Therapy 27 (1): 121–126. https://doi.org/10.17761/1531-2054-27.1.121.
- McCall, M. C., A. Ward, N. W. Roberts, and C. Heneghan. 2013. “Overview of Systematic Reviews: Yoga As a Therapeutic Intervention for Adults with Acute and Chronic Health Conditions.” Evidence-Based Complementary and Alternative Medicine 2013:1–18. https://doi.org/10.1155/2013/945895.
- Muhl, C., K. Mulligan, I. Bayoumi, R. Ashcroft, and C. Godfrey. 2023. “Establishing Internationally Accepted Conceptual and Operational Definitions of Social Prescribing Through Expert Consensus: A Delphi Study.” British Medical Journal Open 13 (7): e070184. https://doi.org/10.1136/bmjopen-2022-070184.
- Nalbant, G., S. Lewis, and K. Chattopadhyay. 2022. “Characteristics of Yoga Providers and Their Sessions and Attendees in the UK: A Cross-Sectional Survey.” International Journal of Environmental Research and Public Health 19 (4): 2212. https://doi.org/10.3390/ijerph19042212.
- Newcombe, S. 2019. Yoga in Britain: Stretching Spirituality and Educating Yogis. Sheffield, UK: Equinox.
- NHS. 2019. “The NHS Long Term Plan”. www.longtermplan.nhs.uk.
- NHS England. 2024. “NHS. Social Prescribing”. https://www.england.nhs.uk/personalisedcare/social-prescribing/.
- Park, C. L., T. Braun, and T. Siegel. 2015. “Who Practices Yoga? A Systematic Review of Demographic, Health-Related, and Psychosocial Factors Associated with Yoga Practice.” Journal of Behavioral Medicine 38 (3): 460–471. https://doi.org/10.1007/s10865-015-9618-5.
- Pascoe, M. C., and I. E. Bauer. 2015. “A Systematic Review of Randomised Control Trials on the Effects of Yoga on Stress Measures and Mood.” Journal of Psychiatric Research 68:270–282. https://doi.org/10.1016/j.jpsychires.2015.07.013.
- Powers, S. 1999. “Empirically Supported Treatments in Pediatric Psychology: Procedure- Related Pain.” Journal of Pediatric Psychology 24 (2): 131–145. https://doi.org/10.1093/jpepsy/24.2.131.
- Santoni, C., B. Chiva Giurca, T. M. Li, H. Mulligan, J. Chilaka, L. Lazzereschi, M. Akhbari, et al. 2019. “Evaluating Student Perceptions and Awareness of Social Prescribing.” Education for Primary Care 30 (6): 361–367. https://doi.org/10.1080/14739879.2019.1669223.
- Saunders, B., J. Sim, T. Kingstone, S. Baker, J. Waterfield, B. Bartlam, H. Burroughs, and C. Jinks. 2018. “Saturation in Qualitative Research: Exploring Its Conceptualization and Operationalization.” Quality & Quantity 52 (4): 1893–1907. https://doi.org/10.1007/s11135-017-0574-8.
- Simkin, D. R., and N. B. Black. 2014. “Meditation and Mindfulness in Clinical Practice.” Child and Adolescent Psychiatric Clinics of North America 23 (3): 487–534. https://doi.org/10.1016/j.chc.2014.03.002.
- Smit, C., and T. Cartwright. 2023. “Recommending Yoga for Health: A Survey of Perceptions Among Healthcare Practitioners in the UK.” Complementary Therapies in Clinical Practice 52:52. https://doi.org/10.1016/j.ctcp.2023.101765.
- Southby, K., and M. Gamsu. 2018. “Factors Affecting General Practice Collaboration with Voluntary and Community Sector Organisations.” Health & Social Care in the Community 26 (3): e360–e369. https://doi.org/10.1111/hsc.12538.
- Stirling, P., P. J. Jenkins, N. D. Clement, A. D. Duckworth, and J. E. McEachan. 2018. “The Net Promoter Scores with Friends and Family Test After Four Hand Surgery Procedures.” Journal of Hand Surgery (European Volume) 44 (3): 290–295. https://doi.org/10.1177/1753193418819686.
- Sulenes, K., J. Freitas, L. Justice, D. D. Colgan, M. Shean, and C. Brems. 2015. “Underuse of Yoga as a Referral Resource by Health Professions Students.” The Journal of Alternative and Complementary Medicine 21 (1): 53–59. https://doi.org/10.1089/acm.2014.0217.
- Telles, S., S. K. Sharma, N. Singh, and A. Balkrishna. 2017. “Characteristics of Yoga Practitioners, Motivators, and Yoga Techniques of Choice: A Cross-Sectional Study.” Frontiers in Public Health 5:5. https://doi.org/10.3389/fpubh.2017.00184.
- van Tulder, M. W., R. Ostelo, J. W. S. Vlaeyen, S. J. Linton, S. J. Morley÷, and W. J. J. Assendelft. 2000. “Behavioral Treatment for Chronic Low Back Pain.” Spine 25 (20): 2688–2699. https://doi.org/10.1097/00007632-200010150-00024.
- World Medical Association. 2018. “WMA Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects.” https://doi.org/10.1001/jama.2013.281053.