Abstract
Twenty-three years ago when women and their children were recruited to a longitudinal genetic epidemiological study during pregnancy, placentas were collected at birth. This paper explores the history of a regional placenta biobank and contemporary understandings of its value for the constitution of a research population. We draw on interviews with some of the mothers and those responsible for the establishment and curation of the placenta collection in order to explore the significance and meaning of the collection for them. Given its capacity to stand in for the study cohort of mothers and children, we argue that the material significance of the placenta biobank as a research tool seems far less important than the work it does in constituting a population. The stories about this collection may be understood within the wider context of developments in biobanking and the bioeconomy.
Introduction
Recent attention has focused on how contemporary bioeconomies may be characterized by practices of bioprospecting and biobanking that generate new forms of biovalue from human tissue. The ways in which bodily tissues such as skin, bone, eyes, brains, oocytes, embryos, fetal tissue and umbilical cord blood may be extracted, exchanged or become transformed in different social contexts have been analyzed by a number of social researchers (Brown and Kraft Citation2006; Waldby and Mitchell Citation2006; Kent Citation2012; Hoeyer Citation2013). Biobanks as tissue repositories for research have become common place as nations have invested in them as part of a political commitment to genetic science, epidemiological research and public health. A central feature of these banks has been the linking of genetic information to health and lifestyle data (Lenk, Sandor, and Gordijn Citation2011). Other biobanks such as blood banks or skin and bone marrow banks provide therapeutic resources for clinical applications (Greenleaf and Hansborough Citation1994; Titmuss Citation1997; Sabatino et al. Citation2012; Busby, Kent, and Farrell Citation2014). Umbilical cord blood has attracted particular attention in light of debates around public and private banks that enroll different models of personal investments for individual benefit and altruistic donation for the benefit of others (Brown and Kraft Citation2006; Fannin Citation2011). In this context, we were interested to investigate why a large number of whole placentas had been collected as part of the establishment in Bristol, UK, of a renowned regional biobank in the early 1990s, how different constituents viewed the collection and what kinds of research had made use of the tissues.
In pregnancy, the placenta is understood as having important physiological functions in sustaining fetal life (Chaddha Whittle, and Kingdom Citation2004). Visualization of the placenta, via ultrasound, provides a diagnostic tool for identifying maternal or fetal health problems and enables midwives to locate the position of the placenta that may in turn have significance for birth. In the management of birth, the safe delivery of the placenta is a primary objective and an important aspect of the “third stage” of the labor and birthing process (Jangsten, Hellström, and Berg Citation2010). In western economies, once delivered, the placenta has commonly been regarded as a clinical waste product, sometimes sold by hospital midwives to firms such as Pasteur Mérieux for use in the cosmetics industry, the income generated used for improvements to the maternity unit or social eventsFootnote1; but more often incinerated by the hospital or sometimes taken home by the mother for ingestion (perhaps via encapsulation) or burial (Helsel and Mochel Citation2002; Colls and Fannin Citation2013; Cremers and Low Citation2014). Another potential use of the placenta is its transformation into a research object through methods of collection, processing and storage (Yoshizawa Citation2013). More recently, it has also been suggested that the placenta may be a useful source of stem cells with therapeutic potential (Evangelista, Soncini, and Parolini Citation2008; Parolini et al. Citation2008; Dzierzak and Robin Citation2010; Parolini and Caruso Citation2011; Guillaume-Gentil et al. Citation2011). Santoro (Citation2011, 76) suggests that “study of the manipulation of cords and placentas provides access to the ‘moral' constitution of collectivities, the practical and discursive production of social ties, the philosophical anthropology of man [sic] as a political being” and may be seen as a site of social change.
This paper explores the history of the collection of placental tissue as a key moment in the establishment of a longitudinal, regionally based population study (Avon Longitudinal Study of Parents and Children, ALSPAC)Footnote2 of links between genetics, lifestyle and health. Placenta biobanking may be understood as historically situated within an era where human tissues appear to acquire new potentialities and new forms of biovalue associated with the scientific enterprise, the linking of information to biological samples and emerging technologies. For us, the biopolitics of placental tissue collection represents a relatively unexplored dimension of contemporary biobanking practices. As we discuss below, researchers and scientists involved with the biobank consider the placenta collection a unique archive of the connection between the mother and the child during pregnancy. The biobank seeks to preserve the placenta's capacity to link the life of the child with the mother's pregnancy and to link the “fetal environment” to the child's future health. Unlike other biobanked materials, this status of the placenta as a “connective tissue,” its capacity to link the development of the fetus with that of the mother's behavior, lifestyle and corporeal experience of pregnancy is integral to its value. The placenta is a distinctive kind of biobanked material precisely because it is more than fetal material. It embodies the connection between mother and fetus during pregnancy and its presence in the biobank signals their separation at birth. Our attention to the distinctive capacities of the placenta as a connective tissue corresponds to the efforts by feminist scholars to develop more nuanced accounts of the gendered aspects of the bioeconomy (Cooper and Waldby Citation2014).
Founding the ALSPAC study
From 1990 to 1992, pregnant women were recruited to a new study in South West England which aimed “to determine which biological, environmental, social, genetic, psychological and psychosocial factors are associated with the survival and health of the fetus, infant and child” (Anon. Citation1989, cited in Overy, Reynolds, and Tansey Citation2012, 10–11) and which subsequently became known as the “Children of the 90s” study. Women with expected delivery dates from 1 April 1991 to 31 December 1992 and from three maternity hospitals in the area were invited to take part. When they gave birth each placenta was collected by midwives, placed in plastic bags and stored in plastic buckets with formalin, either singly or in batches of up to 10. The midwives were compensated for the loss of monies they would otherwise have received from its collection for the production of blood products (see note 1), and the women's consent for examination of the placenta was sought. The placenta collection grew with the successful recruitment of 14,541 women to the “Children of the 90s” study. Given the scale of the study, space for storing the placenta collection had to be found, first in a hospital basement, then years later in newly acquired university accommodation. Curation of the collection was demanding in terms of the space required and the need to maintain the condition of the specimens.
Few large cohort studies at the time of ALSPAC's inception were involved in the collection of biological materials from their cohort populations. But as the key figure in the design and development of the study, Jean Golding, explained in 2012:
… I'd thought through the importance of pregnancy and thought through the importance of following up in detail, particularly looking at environmental factors in pregnancy, which had been very much ignored, other than smoking. As things developed it was the importance of including biological samples that came to the fore as one of the ways of measuring environments that you couldn't measure in other ways. (Overy, Reynolds, and Tansey Citation2012, 5)
Golding, a mathematician by training, conducted early work on data from the 1958 UK Birth Cohort Study and subsequently designed large-scale national birth surveys in Greece in 1983 and in Jamaica in 1986. In the ALSPAC study, biological materials were in effect seen as proxies for the “fetal environment” and would thus allow researchers to look at processes and events that could not be gleaned from survey data or medical records – the primary modes of data collection in previous birth cohort studies – such as infections and immune system response. This emphasis on the importance of pregnancy as an origin point for understanding child health, and of the fetal environment as a research site accessible through the collection of biological materials during pregnancy and at birth, was reflected in an early account of the study's “unique features”:
it will, for the first time, be possible to identify biochemical features of the fetal environment which may relate to the subsequent ability and development of the child. The potential for relating the relationships between the child's genetic endowment and the environment in causing disease will be powerful. (Golding Citation1989, 462)
This approach to the “fetal environment” informed the efforts to enroll women very early in their pregnancies in the research study. As Golding writes in a report from the study's first two months of activity:
after all, the embryo is likely to be most susceptible to the potential hazards and possible benefits of the environment during the very first months of pregnancy. The logistics, however, are a problem since ideally we need to contact women even before they see their community midwife. (Overy, Reynolds, and Tansey Citation2012, 30)
As will be discussed below, our interviews with other researchers involved in the study from its inception echo this view of pregnancy and intrauterine life as an important “origin” point for understanding a child's future health.
For Golding and the others involved in designing and managing the study, its significance was not only the combination of traditional birth cohort data collection methods and the relatively novel collection (at that time) of biological materials linked to this data, but also the open-ended nature of the study. As one scientist involved recalled, “We didn't have any specific hypotheses” (Overy, Reynolds, and Tansey Citation2012, 14). Given its broad remit, the study aimed to capture as much information as possible from a cohort in a defined area over a short period of time (babies born between April 1991 and December 1992). This distinguishes the study from other disease- or pathology-oriented biobanking projects in existence at the time of the study's inception, although its methodological presuppositions are now commonplace in an era of genome-wide association studies. The aim of ALSPAC was not to collect materials from a population with a known disease or condition but to collect as much biological material as ethically and economically feasible from a subset of a general population of pregnant women, their children, their partners and eventually their parents (Golding Citation1989). It also signifies, as we will discuss later, how the value attributed to the biobank materials was multivalent and never directly imagined as therapeutic or commercial in nature. Rather, the reasons why the placenta biobank in particular was deemed “worth” retaining is intimately linked to its role in constituting and maintaining a research population.
Funding for the study was from the outset rather uncertain and short term, dependent on generating research grant income and the goodwill of those involved and the University. “The collect everything philosophy was not one that funding bodies were used to supporting in the 1980s and 90s” and only since 2001 did the biobank receive more long-term core funding from the Wellcome Trust and Medical Research Council (Children of the Citation90s Citation2012). In our interviews and reports about the study it was the vision and tenacity attributed to its founder, who was awarded an OBE in 2012 for her work, that had kept the biobank going from those early days. Given this population-based epidemiological approach, the circumstances behind ALSPAC's development and its collection of biological materials are linked to the public health imperatives of the UK's national health care system. A timeline of the development of ALSPAC could begin in the late 1970s, when Golding was commissioned by the UK Department of Health to design a national birth cohort study for babies born in 1982, a project that was eventually not funded (see Overy, Reynolds, and Tansey Citation2012). In 1985, Golding was invited by the WHO to design a set of European birth cohort studies. These cohort studies were designed to be carried out in health systems across Europe, although ELSPAC, as the European study was called, was implemented primarily in countries with well-established public health systems that would support the resources needed to undertake the collection and management of data: Great Britain, Isle of Man, the Czech Republic, Slovakia, Russia, Ukraine and at the outset, Spain and Belgium, although both these countries eventually dropped out of the larger study (Overy, Reynolds, and Tansey Citation2012, 9; Anon, Citation1989). Although the initial planning stages of the study were supported by WHO, there was little funding to fully implement ELSPAC across all the European states that were involved, and little interest in collecting biological samples.
So while the ALSPAC study was set up as part of a wider international initiative and was based on beliefs that pregnancy and the tissues obtained at birth could reveal much about the health of the child it could be seen as a product of its time; yet, in certain respects, this was not a new idea. For as previously documented, cultural beliefs about the significance of the placental tissues for child health, and rituals for its proper management and disposal, have a long history (Santoro Citation2011) and the notion of the placenta as an important tool for understanding fetal development had become well recognized. What was innovative and especially “modern” was the idea of collecting and storing these and other biological materials on a large scale, creating a biobank, for study into the future about the population's (cohort's) health. Research biobanks emerge as a feature of contemporary genetic science and health research from this period, associated with the capitalization of the biosciences (Rajan Citation2006; Rabinow and Rose Citation2006; Rose Citation2006; Waldby and Mitchell Citation2006; Cooper Citation2008) and the reconfiguring of biopower (Raman and Tutton Citation2010; Santoro Citation2011).
Following high-profile scandals about the retention of children's organs and tissues without parental consent in the UK, new techniques and regulatory standards for research biobanks also emerged resulting from new legislation (the UK Human Tissue Act 2004) designed to (re)build trust between tissue donors, scientists and clinicians (Kent and ter Meulen Citation2011). This meant that auditable records and clear labeling of tissue specimens were necessary in order to comply with new licensing requirements, and any significant deterioration in a specimen could lead to it being removed from the collection and destroyed. In 2010, the University identified a secure storage location resembling farm buildings, away from the main campus and the collection was moved again. The location is relatively easy to access and is maintained by research staff on site and serviced by University security if required. At the time of our visit in 2013, the collection, now some twenty-two years old, was reduced in size to 8933 placentas (Fraser et al. Citation2012, see ).
Figure 1. Interior of ALSPAC placenta biobank.Reproduced by kind permission of the ALSPAC Executive.

We wanted to know how the “journey” of the placenta from women's bodies to the hospital and then to the biobank, that is, the placenta's transformation into a scientific object, might be understood. Below we discuss what meanings and values could be attributed to the placental tissue collection and what this particular collection, its history and geography can tell us about the wider socio-cultural significance of placental tissue as a research object. We consider how the value of the placenta collection was imagined at its inception and how it has been maintained over time in light of the development of new techniques and the expansion of the original study itself. We interviewed six past and present staff (health professionals and scientists) involved in setting up and curating the collection, and a small number (12) of mothers who were still active participants in the population studyFootnote3. We draw on this interview data here. We also carried out a site visit to the collection, and reviewed published accounts of ALSPAC to gain a better sense of how the placenta collection and the ALSPAC biobank more generally is presented by ALSPAC staff to the research community.Footnote4
The ALSPAC study is notable for several reasons. It is described as “uniquely placed” to permit analysis of gene/environment interactions: the collection of biological materials from mothers and children at birth and throughout infancy, childhood and adolescence combined with repeated survey and interview data collection over its 21-year history has generated significant research interest in the resource.Footnote5 It has been described by researchers as a resource whose “scale and richness is … unprecedented in epidemiological studies” (Fraser et al. Citation2012, 5). It is perhaps then no surprise that a “major epidemiological study” such as ALSPAC would have a strong local presence. Indeed, “Children of the 90s” is a highly visible part of the local health landscape in Bristol. It draws extensively on the social ties and geographic proximity between participants who through the course of the study got to know each other as members of the same antenatal groups, with children in the same primary schools and who maintained their participation in the study as it extended into their children's adolescence and now adulthood. These ties are seen to generate value, because they mean that participants may be more likely to stay involved if others in their personal networks are also participating. In this way, the biobank is part of what Emma Kowal (Citation2013) calls an “affective network” linking samples, scientists and living tissue donors. Indeed, the identification of the study with a particular place, and the resources on which the study could then draw by virtue of its geographical configuration of the study, was not accidental. When asked whether a “local” study would be too restrictive in scale (compared to the national birth cohort studies that had preceded ALSPAC), Golding responded that the longitudinal, rather than prevalence-orientated nature of the study, meant that although the study might not include all environments of child health, “it does have a lot of environments you can look at longitudinally to see what the effects are … you can go out and sample, whereas that would be much more difficult to do nationally” (Overy, Reynolds, and Tansey Citation2012, 12). Golding continues:
That's one argument for having it local, but the major advantage, I think, is that locally you can get your local media and all the local health professionals to become part of the study, to be interested in it and want to know what the latest results are. Nearly everybody who's lived in Bristol or the surrounding area knows somebody who's in the study. It's very unusual for me to meet somebody who doesn't tell me about their cousin or their nephew or a friend who is part of the study. I think that sort of drawing together of the community couldn't happen with a national study. They don't know one another, whereas here you have whole classes at school where nearly everybody in the class is part of the study, and those who aren't feel very jealous of those who are, which keeps the whole thing rolling along. (13)
To ensure the ongoing participation of those enrolled in the study, these affective networks need to be continually maintained. The maintenance over time of a collection of biological materials is part of this continual work to constitute, call upon and maintain the study population as a whole.
Research on biobanking argues that the value attached to samples and information held by a biobank is contingent on analytical techniques, the availability and accessibility of the biobank's resources, and the quality and quantity of both the materials and the information linking samples to medical histories, lifestyle and other kinds of social or behavioral data. At present, the number of human tissue samples collected in biobanks is growing as techniques for analysis and storage improve and large-scale, highly publicized biobanking projects are carried out (Gottweis and Petersen Citation2008). Biobanking on a national scale is now aimed at developing “biological resources” for the analysis of health and disease patterns in a large population. This marks a change from disease-based biobanks insofar as national or regional biobanks identify participants within a particular geographical area as the first criterion for selection (Busby Citation2006; Busby and Martin Citation2006; Mitchell and Waldby Citation2010). Although the establishment of large-scale national and multinational biobanks have garnered significant attention, research on a smaller scale and notably on regional biobanks such as ALSPAC that predate these more recent collections have been far less well-studied by social researchers. What our research on the ALSPAC placenta biobank suggests is that the value attached to a biobank is constituted in part by its political geography. This geography is not simply a measure of the scale of the collection or the proximity of participants to each other, a factor that makes accessing the population and collecting samples, for example, much easier. More importantly, as Golding recounts, this geography refers to the ability to marshal the resources needed to ensure the population's ongoing research value: to call upon the social and professional communities of health care professionals, media, schools, parents and children and in so doing construct a new “community of promise” (Martin, Brown, and Kraft Citation2008a, Citation2008b; Santoro Citation2011). The promissory value of the bank is tied to the building of expectations that ALSPAC would in the future, and does in the present, lead to improvements in child health.
As such, our research makes an important contribution to the literature on the material and spatial aspects of the bioeconomy (see Greenhough Citation2011; Davies Citation2013; Nash Citation2013), and to Hoeyer's (Citation2008) exhortation to examine the social and cultural imaginaries of biobanking. For although our research confirms what other social research on biobanking has detailed – that biobanking is often a speculative practice, and that the nature of a study population's consent contributes to the biobank's current legibility and legitimacy – what we learn from this research is that the value of a biobank may also depend on its capacity to draw on unpaid and emotional labor, to generate emotional investment and to spatially re-embody a dispersed study population.
The placenta as a biographical object
Our interviews with mothers involved in ALSPAC began by asking women to recount what they remembered about their antenatal care in the National Health Service and what they remembered about joining the study. Of the twelve women we interviewed, half were first-time mothers when they enrolled in the study; the rest had between one and three children when they were recruited. Some of the women interviewed had since donated other materials to the study and some were blood donors, or carried an organ donor card. None of them knew where the placenta collection was held now or what had happened to it and some were curious to find out.
When asked to recall what they remembered about how the placenta became part of the collection, most women shared stories of their study child's birth; narrating how the placenta moved from the birthing room to the study collection also meant recalling the pregnancy and birth of the study child and often their other pregnancies. The placenta was described as visually revealing a mother's habits during pregnancy or indications of the development of the child. One woman described in detail her experiences of giving birth to a set of twins and attributed differences between the identical twins to the differences in the placentas observed at birth.Footnote6
They were born three weeks early and they were induced and they were induced because twin one wasn't thriving as well as they wanted him to, and in actual fact at three weeks early they were six pound ten and a half and seven pound two, so they were like enormous. They were bigger than singletons at that age. So it's not as though they were actually small babies or anything, but when they were born, his placental tissue was … they described it as becoming grainy and it wasn't good. So it was beginning to break down. So I guess I had some kind of interest in placental tissue at that point because of what had happened to him and he was absolutely fine when he came out with an Apgar score of nine.Footnote7 I'm sure he was fed before his brother was even born, but you know, it was interesting that in later life, the second twin, who had a very good placental tissue who was the bigger of the two and the second born, he is, although they're identical, undoubtedly slightly smarter than his brother. Now there's all kinds of factors that can affect that I know, but it's interesting and the smaller twin remained smaller up until they were about- And it was only like six ounces or whatever it was, 6.10, 7.2, he remained smaller until probably ten-ish, something like that. Not much. Just a little bit. … They're amazing kids. They're absolutely fantastic. They're fit. They're healthy. They're very, very clever, both of them, but [the second twin's] just slightly cleverer and I often wonder whether that had any tie-back to the differences in their placentas and the fact that [the first twin's] was breaking down and [the second twin's] was strong. (MO14)
Women's memories of discussing the placenta at birth with midwives tended to link the health of the placenta with the mother's behavior and the length of the pregnancy, with a “grainy” placenta being associated with the poor health of the baby or, in other accounts, the mother's habit of smoking. In one interview, a woman described the placenta as “scraggy” on account of a longer than average gestation. These stories of the placenta as “diagnostic” were also reflected in some of the interviews with researchers. As one of the staff involved in setting up the collection explained:
When a placenta comes to a pathologist, they're normally sent from abnormal pregnancies. Stillbirths, small babies, abnormal babies, and all that sort of thing, to see if we can throw any light on the cause for the benefit of the parents and the health and medical staff and also as part of providing a perinatal pathology service, the whole object is to see if we can stop it happening again and give that mother a normal healthy pregnancy next time. So for example for babies [who are] very small, you would send a placenta to see if there were any signs that the blood supply to the placenta from the uterus from the mother was sufficient. Pre-eclampsia, eclampsia, and you can see changes in the placenta that equate with that. (RES02)
This member of staff went on to describe other pathological changes which can be observed in placenta and which may have significance for healthy pregnancy and the health of the fetus or newborn. The significance of such changes for longer term health was less well understood, but they highlighted how the placenta was viewed as an “archive” of potential information about the future health of the child.
Many of the women we interviewed described how the placenta was not something they thought about much, and that in any case they themselves did not want it, even though they often remarked how other women might want to eat the placenta or bury it. For this group, who by now had a longstanding relationship with the epidemiological study, donating the placenta was an easy thing to do, since they saw it as a way of contributing to medical research and helping others. In a particularly vivid account of a rapid home birth followed by a delayed third stage, one woman described the extraordinary lengths that she went to in order to ensure that the placenta reached the ALSPAC researchers:
The ambulance men then tried to deliver the placenta and I was having none of it. It was not going to move. It was the coldest morning of March and we had to wait an hour and a half for the emergency midwife to come out because she couldn't defrost her car. She couldn't get into her car. And in that hour-and-a-half, the ambulance men tried several times to get me to deliver the placenta and I was having none of it. It just did not want to move. They were getting concerned because the midwife hadn't turned up. The hospital phoned because we'd phoned them to say we were on our way in, but we never arrived. So they phoned back to say where were we and then we said like, you know, “She's been born at home, we're waiting for the ambulance men to bring us into [the hospital] but the emergency midwife.” So it was like chaos just waiting. I told the ambulance men that I wanted the placenta to go towards the study and obviously they were aware of that. So they wrapped it all in a bag, you know, and put it in a kidney dish, and that eventually ended up coming to the hospital with us and we passed it over to those that wanted it there. We gave it to the team and they took it to wherever it had to go.
So you remember that the study did ask for the placenta when you signed up or at some point during your antenatal care?
Yes. Yes. I actually remembered that and said, “Whatever you do, that's not going anywhere, I'm taking that with me. It's got to go to the hospital.” [Laughs] But once the midwife actually arrived, within five-ten minutes of her doing what she did, you know, I'd got no problem. It was away and that was it. It was all packed up and ready to transport with me.
And on arrival at the hospital:
I was going to say it was a case of, you know, this is the placenta that I've promised will go to the “Children of the 90s” study and they just said, ‘Oh yes. Thank you very much. We'll make sure it gets to where it needs to go. Yeah. I went one way and that went the other [laughter]. Yes. We parted company. (MO19)
In these stories, the placenta “had a job” to do, and for many of the mothers we interviewed, birth meant the placenta ceased to “do” anything for the mother and child. They therefore had little emotional connection to it after the birth or concern about what may have happened to it. Indeed, midwives had suggested to us that often fathers take more of an interest in the placenta when it is delivered than a motherFootnote8. In one interview where the father was present he recalled memories of the birth and seeing the placenta, saying:
Like I said, I've never really given it any thought until now really. It was just something that was there to feed the baby, but when you really think about it in some depth, … […] … when I seen one and it was quite inspiring to look at. I can't say it was attractive, but it was like, “Cor”, you know, it was a fair old size. It was a lot bigger than I imagined it was going to be and it was a thought of, ‘What is that exactly? … […] … . It's left me a bit of a sense of wonder hasn't it? (MO12)
Although women understood the placenta as a biographical object that could act as a source of information about the mother and child, in their accounts, the notion of “ownership” and the identity of the placenta were ambiguous. The placenta was eloquently described as something shared between mother and child, as possibly belonging to both, though some women saw it as “more me” (MO12) than the child's, others as “more the child's than mine” (MO14). Yet one woman responded that she did not think that the placenta belonged to either her or her baby: “it felt like it had served its purpose. So I didn't feel like it sort of belonged to either of us really” (MO21). One health professional recalled how these ambiguities relating to ownership of the placenta influenced the approach to consent for retaining it.
We asked specifically for their permission to retain the placenta for examination. It wasn't to donate it because it's an interesting use of words. So that's what we did while not doing an exhaustive scholarly study of who owns the placenta. So attitudes towards that have changed as well. Of course a lot of women now I think do believe that it does belong to them, but it could be argued … That was the basis and as far as I know, that was the first time. So that was where getting permission for use of the placenta, I think we were ahead of the game at that point. (RES01)
Respondents involved with the study since its inception described how the ethical and policy context had changed since the 1990s. In subsequent years placenta that had been retained which could not be linked to a signed consent form were discarded:
So we had samples that didn't have consent, but we decided that we couldn't use those. So we disposed of the ones that didn't have consent and it's not that there were any issues with the way it was done because it was done in the way that was acceptable twenty-two years ago. We just decided to tighten it up and never use anything from somebody without consent and it was a way of getting the storage size down a bit. It was probably about a quarter of what we originally had. (RES05)
For some of our respondents, this was an especially sensitive issue due to the specific location of the collection (in Bristol) and changes in regulation of the use of human tissue following the 2004 Human Tissue Act.Footnote9 Yet we were struck by the relative ease with which the women we interviewed regarded the fate of the placenta collection. For several of the mothers we interviewed, the perception that the placenta had “done its job” during the pregnancy qualified it as a potential research resource. They understood that if it had not been retained the placenta would have been incinerated or “put in the bin.” Rendered as waste or rubbish, the placenta becomes available for other uses (Waldby and Mitchell Citation2006; Svendsen Citation2007). It was suggested that “most mothers, that once they'd had the baby they weren't really interested in the placenta. It would be surprising I think if anyone had any sort of strong feelings about giving their placenta” (MO17). Indeed most mothers confirmed that they were more interested in their newborn baby and were very happy for the placenta to be collected if it could be “of use.” There was a widely held view that research on the placenta could “help others” or even have direct benefits in treating disease within the family.
The fate of the collection: mothers’ hopes and aspirations
The women we interviewed had maintained a relationship with ALSPAC over a 21-year period, and believed that the potential of the placenta collection could bring benefits for the child and, through research, help others in the wider community:
I thought it would be if somebody, say your child, had cancer and they needed a bone marrow or some tissue obviously that you get from a close relative, theirs would be already there on standby if they needed any help in that way. And also I did think it would possibly be used for some sort of experiments and sort of research into diseases for either cancer or nervous system and things like that and stem cells. (MO12)
Several mothers believed that the placenta could yield stem cells which in turn could be useful for research and development of therapies. Another said:
So I'm sure they would harvest the bits they want for the reasons they would want and I'm guessing that stem cell research would be part of it, although I couldn't be sure that they can harvest stem cells from the placental side, but I'm guessing they would. (MO14)
Neither of these mothers imagined that the whole placenta would have been stored; rather they believed “bits” would have been kept. For as this same mother suggested:
I would assume just, you know, if I thought about such a thing, that obviously they're not just going to keep whole placentas. They're going to have done whatever it is they do with them. Freeze them and take sections of them on a slide somewhere with dates, identification number on it in a stack of other ones in a deep-freeze somewhere or whatever it is they do with them. They dry them out first or whatever and that's what I would and why they would want to do that is beyond me [laughs], but just in case they need to go back and check something in the future …
But you mentioned that you couldn't imagine that they would keep the whole placenta. Why do you think that would be?
Because that's quite a lot of space [laughs]. There's a lot of them and I can't imagine- I don't know how many children were in the study initially but it ran into thousands didn't it and that's quite a big room filled with frozen placentas isn't it? It's a big fridge somewhere. I can't imagine why they'd want all of it, and if they do, fine. But I imagine that they would just take samples of them. (MO14)
Here the method of storage was assumed to be cryopreservation but another mother imagined “pickled placentas” as having “limited shelf life” and thought that inevitably the placentas deteriorated and could become unusable and therefore discarded:
So you start off with a large sample and I suppose it just gets reduced over the years and then you end up with not so many as it is with most studies I suppose with children dropping out and things. (MO17)
Other mothers also thought the samples were frozen, though another said:
How do you think they would have stored the placenta? Do you remember being told?
I think I was told it was formaldehyde. Buckets of formaldehyde aren't they somewhere in Bristol? Corridors of them. [Laughs] I'm assuming there must be so many of them. [ … .] I think it's quite sweet. It's quite nice. It's part of the most wonderful thing that ever happened to me is stored somewhere in Bristol in a bucket. Feels quite special. (MO15)
Several of the mothers described the reluctance of their children to continue as active participants in the “Children of the 90s” study. In their view, the retained placenta was of little concern to these young adults even where it might be regarded as part of them or contained their child's DNA. The prospect of intergenerational comparisons, where second-generation placental tissue might be compared to findings from the older tissues, was seen by mothers and scientists as enhancing the collection's value and creating new possibilities for research.
Although very few women were able to recall learning of the fate of the placenta collection, how it is maintained and what research studies have been done with it, all expressed hope and some conviction of the placenta collection's usefulness for scientific research. Interestingly some of the women we interviewed hoped it might be a useful alternative to animal tissues:
So guess in this way it's not going to harm anybody and if some good can come of it, I don't see any problem with it, especially if it's used to cure disease. I mean I suppose if it were used- I think I would- I don't know about cosmetics and stuff, but I don't suppose I could argue about that either because it's not like a live…it's only live when it's inside you I guess. It doesn't live on does it like some kind of horror movie [laughs]? So I suppose if that's used for cosmetics rather than animals, that's a good thing as well, but if it's used to research for disease instead of on animals and humans, that's a good thing. So I don't see a problem with it. I think it's probably a positive thing actually. (MO11)
This woman felt there were fewer ethical issues associated with the use of human placenta in research than “live animals.” Amongst the mothers we interviewed, the idea that the placenta collection might reduce the need for animal experiments was a recurrent theme. In their view, the tissue once separated from the body was not “live” and making use of it was seen as “a positive thing.”
Women's aspirations that cells derived from the placenta could be used to develop drugs or cell therapies drew on contemporary understandings of techniques for culturing cells in the laboratory (Landecker Citation2007). The method of preserving these placentas in formalin means that they have no direct therapeutic value but since the 1990s efforts to develop innovative tissue and cell therapies within “regenerative medicine” have led to new forms of “bioprospecting.” Mining of biological materials obtained from embryos, aborted fetuses, blood, ova, bone and placenta for stem cell production in order to develop therapeutic applications has led to new investments and efforts to commercialize cell therapies (Parry and Gere Citation2006; Kent Citation2008, Citation2012; Fannin Citation2013). Women's hopes that the placenta collection could be used as a substitute for experimental animal models reflect broader social anxieties about animal research. The re-location of the placenta collection to what resembled farm buildings, close to where animal research is conducted, recalls the close connection between the development of techniques to culture animal life in order to benefit human health (Brown et al. Citation2006; Franklin Citation2007a, Citation2007b). “Down on the farm,” the placenta collection was secure and well maintained, but its value as a research resource, despite women's hopes, seemed unfulfilled.
Speculating, accumulating and curating the collection
The placenta collection was established at a time in the 1990s when genomics research was considered of increasing importance for understanding health and disease. Those responsible for setting up the collection speculated that the placentas could hold valuable information that might be accessed in the future. The promise of new knowledge and new ways of investigating the links between genes and environment heralded by the internationally supported Human Genome Project represented new research opportunities and new investments in biobanking (Hirtzlin et al. Citation2003; Brand and Probst-Hensch Citation2007; Knoppers, Zawati, and Kirby Citation2012). Moreover, the placenta was the material embodiment of “in-utero” life as described by this interviewee:
The kind of idea that the baby when born was a clean slate and things and that was only when its life started in a sense, I knew was false, that there were things happening which were going to shape its future and those were happening in-utero, and that one could argue that there were many things which were in the placenta which actually hadn't marked or embedded the placenta, which might be of extraordinary value in understanding the whole context of ALSPAC and understanding the whole business between genes and genetics, and nature and nurture, genetics and environment … [ … .] … there was a potentially much more valuable use for it and that was holding on to it. And of course in a sense that hypothesis was a very large and all-encompassing hypothesis about the placenta, we didn't have any, apart from infection, but we didn't have any specific ideas of what we might do with it, but it was the kind of ethos of ALSPAC that gosh, we're going to take bloods and at some point a question will arise and we'll only be able to answer it if we go back to the blood. That was the same with the placenta, that if we store them of course, they were going to be in formaldehyde. So the potential, if it was DNA for example, that could affect the DNA, could fracture the DNA, but we felt there was a huge potential for benefit that might not become apparent for quite a long time. And so that's why we actually stored them. I'm not sure that many researchers kind of share this belief because they haven't been used. They lay dormant for a long time … but I think people are now beginning to realise the potential. Even now I don't know what work has been done on them, but that was the ethos. That was the ethos. (RES01)
The hypothesis that a placenta contained information about the future life of the child underpinned and justified the initial collection of placentas. A kind of “promissory capital” (Brown, Kraft, and Martin Citation2006; Martin, Brown, and Kraft Citation2008a, Citation2008b) became invested in the collection, a motivation that underpins much of the data and tissue collection in longitudinal studies more generally. Accumulation of biological materials obtained from the ALSPAC study population was a strong ethos as mothers, their children and mothers’ partners were asked to donate blood, urine, teeth, hair and nail clippings to the biobank to build a research resource that could attract further funding and research studies (Pearson Citation2012). At the same time the banking of these placental tissues and their curation relied on available, relatively low-cost techniques for processing and storage (see ). One interviewee recalled the practical difficulties of collecting the placentas, the burden on the midwifery staff and the impossibilities of freezing the materials.
Figure 2. Placentas are stored in individual buckets or in individually sealed batches of up to ten placentas in larger storage containers. Reproduced by kind permission of the ALSPAC Executive.
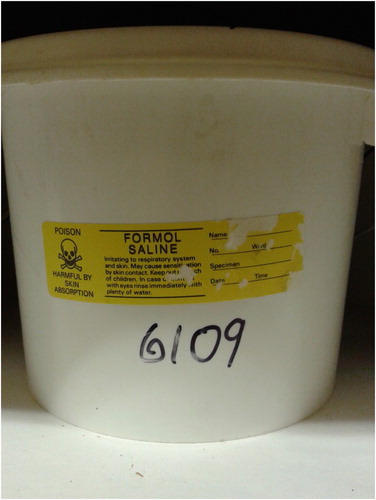
We wanted the placenta frozen but we couldn't persuade our colleagues in midwifery to do it. It was a step too far for them, but they did freeze the little bit of umbilical cord from every one, which was great of them. And the rest of the placenta we fixed in formalin and bagged individually with a number and then put those I think ten or fifteen into a great big bucket. Put more formalin on top. Put the lid on the bucket and gave it to ALSPAC. And the idea of all that is we were looking in the very long-term so that they would never dry out. There's a problem with anything in formalin. Five, ten years down the road it's dried out. (RES02)
And
We had no opportunity to freeze tissue. There were worries about HIV and hepatitis and things and midwives didn't want to handle them, cut them with anything sharp. You can understand that. There was a small hazard. Placenta comes out at 4am in the morning. Everybody's dog tired and you have to take the scalpel, there's blood everywhere … It was also an extra burden to them. They were already putting the placentas in buckets for us and doing all sorts of other stuff for ALSPAC. Freezing requires liquid nitrogen which again has a hazard. We don't leave it on the wards. It always used to come with a pathologist attached to a technician. So there were issues and it was just too difficult, although it's a pity. (RES02)
Investment in the collection was constrained by both the conditions of knowledge and practice of the time and also research grant funding. The spatial size of the collection – because it included whole organs – was a particular feature of the collection, with implications for its management and curation.
Despite these constraints considerable time and effort were required to curate the collection, to move it from one location to another when new governance arrangements came into force and organizational circumstances changed. These efforts involved the unpaid labor of maintaining the collection given the contingent funding environment that marked the early years of ALSPAC. These emotional investments were marked by the personal commitment of the biobank's originators to maintain the collection for future use. As one interviewee recalled a colleague's efforts to check on the collection during its storage in a local hospital:
I think she'd have gone round trying to do whatever she could really. That was what was deemed to be the given. She wasn't paid to do it. She was looking after that out of the goodness of her heart because she'd invested so much of herself in collecting them in the first place. That's the thing. (RES04)
A recurring narrative in the interviews with collectors was that the potential of the collection had not yet been realized. There had been few transactions between the wider research community and the collection. After a small-scale doctoral study in the early 2000s (Hargitai Citation2004), only two recent studies had subsequently made use of the collection (Barker et al. Citation2013; Salafia Citation2013, Girardi et al. Citation2014). All focused on the morphology of the placenta in an attempt to link its surface area or structural development to health conditions in the child.
This limited use of the tissues was accounted for in a number of ways. Paradoxically, the large size of the collection, combined with the form of storage and the limits of funding the time-consuming work of analyzing the whole tissue, was a constraint:
We're trying to understand what the potential research use of them now is because you've had so few studies.
I think the reason why there are so few studies is the sheer volume of them, you know, the sheer number. There have been smaller studies, but it's just the practicality of- I mean the technician that worked here photographing and measuring the placentas was, you know, initially it was, “Oh she'll do as many as possible but we'd like her to do the lot,” but basically after a year she said, “I can't do this anymore.” [Laughs] She was a really competent, really good technician, but after a year she said, “I've had enough,” because it was literally going down, and this is when they were in the same building, going downstairs, bringing up twenty for the day. Photographing them. Measuring them. She has got full protective clothing on.
And how many did she actually?
She managed- I can't remember the exact number, but probably only just over a thousand.
So actually the fact that there's so many is almost off-putting you seem to be saying? I would have thought that would be seen as enhancing their potential value.
I think it does enhance the potential value but the practicalities of it, of getting funding to- When you actually think about okay this would be wonderful, but then you think, “Who are we actually going to get to do that practical work?” I think that's more of an issue sometimes. (RES05)
It was suggested that the method of preservation, in formalin, severely limited the kinds of research questions that might be addressed using these placental tissue samples to studies that focused on morphology, rather than genetics. As this interviewee put it: I think potentially it could be of great value, but not as valuable as it might have been if we'd preserved it differently (RES01). One of our interviewees responded that this was a “failure” and a “disappointment” given the effort expended to collect and maintain the placenta. Research questions had not yet been identified which could exploit the collection, a view that drove the initial collection of research materials for the study.
There was an anticipation that new techniques and new methods of study were yet to emerge which could best use the collection. In addition, the ongoing nature of the study and the effort to recruit a second generation – the Children of the “Children of the 90s”, known as the COCO90s cohort – could redefine the value of the placenta collection because researchers would then have access to three generations of pregnancy, birth and health data.
Yeah. I think it will be enhanced working with [second generation placentas]. There are limitations of the tissue because it's all in formalin and a lot of the techniques that we would like to use, we can't because it's been in formalin, but there are lots of things with DNA that we could possibly do.
Even now?
I think possibly but we'd need to do some pilots, but looking possibly at epigenetic markers at different points of the placenta.
And what are some of the things that you couldn't do because it's in formalin that you maybe could with some of the [next generation] placentas?
Well for example there's no way we could get RNA out of them. There's no biochemical assays or anything that we could do because they're in formalin. (RES05)
The “anachronistic” method of preservation of the placenta and the excitement generated by other methods and techniques, in particular gene studies, may have informed perceptions that the value of the placenta biobank remains latent, not yet fulfilled, in which techniques to analyze the collection have yet to be developed. In Radin's (Citation2013) research on the development of cryopreservation techniques in the International Biological Program (a precursor to the controversial Human Genome Diversity Project), the ability to freeze a sample in time aligned with the identification of the Program's study populations as untapped archives of human evolution. Formalin fixing, a much older technique, similarly arrests a tissue in time but also makes it much less available for more “modern” forms of analysis. The pragmatic concern for using a low-cost and low-risk method of preservation meant that the value of the preserved placenta was “fixed” to enable “classical” morphological study, rather than modern molecular analysis (see Nyhart Citation1995). The value of the placenta as a scientific object was deferred to an undetermined point in the future, a future when advanced morphological or genetic techniques might access the collection's previously untapped value.
The placenta collection, large scale and well maintained, yet relatively underutilized, is only a part of the vast quantity of biological and informational material collected as part of the broader ALSPAC study. Crucially, the placenta was envisioned as a key “mediator” of the link between mother and child:
I think if you think about the ALSPAC placentas, the key thing that we've got is not just the placenta collection. It's everything else that we've got. So it could be that there's something specific about the placenta structure that relates to a child's outcome, but then we can then go back and say, “Well okay. Is there anything that these mothers did or any genotypes these mothers have that meant their placenta looked like this that led to that child's outcome?” It could be that there's some intervention that you could use during pregnancy to prevent the placenta becoming like that and then the child having that outcome. So it's like an intermediate.
So those are research questions really. Is it perinatal pathology that we were told is that kind of study of that? They're questions for that kind of research group.
Yeah. But I think the beauty of ALSPAC is we can then take what people find in the placenta and look in both directions. So what is it about the mother that led to this in the placenta and then what is the outcome of the child twenty years later related to that? (RES05)
There is little evidence that the collection has been exploited for scientific research studies on placental tissue, yet it continued to be regarded as an important resource by current and past staff. We suggest that its value, at present, seems to lie less in the actual use of the tissue than in its performative significance as one of or indeed the key moment in the history of the “Children of the 90s” study when women were first recruited to the study during pregnancy or birth. It is imbued with the symbolic value of a population study cohort assembled in one place and at one time. The collection, we suggest, thus represents the cohort at birth and bears physical witness to the link between the generations of mothers and children. It is a permanent record in this collection of the temporary state of pregnancy and therefore of the “fetal environment,” identified as a crucial moment in the child's development, with lasting consequences for the health of the child. The placental collection thus represents the population cohort in its most complete state, at the inception of the life of the study child. As a connective tissue, the placenta collection “fixed” in formalin links the community of mothers and babies that create the study's research population. The efforts to retain the collection, to maintain it as a resource for future research and to claim a speculative future value for it, suggest that its value partly rests on its capacity to stand in for the entire cohort.
Conclusion
Despite ALSPAC's overall importance to the (local and wider) scientific community, the researchers involved with the study considered the placenta collection as “underutilized.” We began our research out of interest in why materials that have been little used since collection (two research projects in the last 20 years) continue to be seen as worthy of ongoing investment. Funds are being invested to maintain and conserve the collection and to comply with licensing regulations regarding human tissue biobanks, as well as more “immaterial” investments that position a little-used collection as potentially valuable in the future. Our research demonstrates that the placenta collection's value resides in its perception as what we call a “connective tissue”: a material archive of pregnancy; an untapped potential resource in relation to current and future collections of biological materials and a performative instantiation of the original study population of mothers and babies.
The placenta is described by the women who joined the study as mothers in biographical terms as an entity that invites stories of pregnancy and birth, and is viewed as a source of information about the mother and child, the mother's habits during pregnancy, and the child's future health. Having “done its job,” its value for the mothers we interviewed lay elsewhere. Both researchers and women we interviewed identified the placenta as a potential resource for future research. The development of new techniques and new research questions that will link the collection to existing and future collections of biological materials is seen as a means to enhance the value of the placental tissue held in the biobank. In this way, the placenta collection has a “promissory” potential to reveal information about the relationship between fetal development and future health and social outcomes.
We suggest that the placenta collection in this particular study is also valued because it is a potent symbol of the entire study population. Securing the sustained participation of a study population over a long period of time in large-scale longitudinal research requires a considerable amount of effort to maintain contact, interest, and compliance. Despite the relatively few projects that have made use of the ALSPAC placentas, the collection has been maintained by the strength of the personal relationships and affective networks that have sustained the study as a whole. Indeed, social research on other regional biobanking projects suggests that identification with an imagined community of participants and with obligation or loyalty to such place-based projects is a key element in the recruitment and retention of participants to long-term research studies (Hoeyer Citation2003; Haimes and Whong-Barr Citation2004). A key aspect of the investment in maintaining the placenta collection over a long period of time is thus its symbolic value: it represents the “origins” of the study population and recreates the cohort of mothers and their children (born over an 18-month period and now dispersed around the world) in time and space.
As Warwick Anderson argues in his work on the history of research into the causes of kuru, a fatal brain disease, “it becomes clear that the value attributed to scientific objects – indeed, even the constitution of scientific objects – cannot be readily extricated from the making of relationships and self-formation” (Citation2012, 13). To this we would add that the constitution of the placenta as a scientific object in this collection is inextricable from the social and affective networks that sustain ALSPAC as a place-based “regional” study. The regional nature of the longitudinal study for which the placentas were collected highlights how the performative aspects of biobanking, that is, the ability of the biobank to serve as a stand in for the population cohort, in effect, to produce the cohort as a cohort, is an important part of the biovalue story of tissue collections. Measures of this biological value in the placenta biobank cannot be defined solely by accounts of their economic worth as “commodities” or even “assets” but rather as a kind of reserve upon which future estimations of value may be made (Fannin Citation2013; for a critique of the notion of “biovalue” see Birch and Tyfield Citation2013). To discount what we are calling the performative value of the collection and its capacity to re-embody the study population of mothers and babies through the “connective tissue” of the placenta would reduce value solely to its economic function and neglect how non-commercial population-based studies like ALSPAC, funded in part by a mix of public and private charitable sources, are engaged in the more profoundly biopolitical work of constituting a research population. Our research also suggests that critical accounts of the construction of the promissory communities of biobanking should be attentive to how geography shapes a biobank's value: the regional scope of the study enables researchers to more easily call upon participants as a “community” to solicit their ongoing participation, while the sheer physical size of the collection has helped determine its method of preservation, its location and its accessibility to researchers. The bodily geography of pregnancy is also significant insofar as the placenta is viewed as the connection between the life of the mother and the development of the fetus. All of these examples point to the importance of taking the spaces of biobanking into account.
ALSPAC is heralded as one of the pioneering studies of its type (Overy, Reynolds, and Tansey Citation2012) and careers have been built on its achievements. It was established at a time and in a place where human tissue research became the focus of national (and international) attention. From our analysis, we demonstrate that placental tissue retained in this collection for over 22 years marks out a number of developments in biobanking over that period. The collection of biological materials from a population cohort was novel in the early 1990s but is now commonplace and increasingly viewed as central to the development of personalized approaches to healthcare provision. The placenta collection itself is unique in its scale – storing thousands of whole placentas in formaldehyde. Subsequent collectors of placental tissue have cryopreserved tissue samples and/or histology sections. Preservation of whole placentas in formalin reflected a compromise between the preferred method for storing biological materials in the study (freezing) and the contingencies of cost and available space given the study's early financial uncertainties. Yet as one researcher noted, the possibility of identifying epigenetic markers in the stored placentas would enhance their research value and reflects the broader “epigenetic turn” in recent genetic and genomic research, a field in which “vast expectations coexist with significant uncertainty” (Meloni and Testac Citation2014, 1).Footnote10 Our respondents who were health professionals and scientists claimed its promissory value was its potential to answer as yet unidentified research questions, using unidentified methods.
It hasn't been used to its full potential. It really hasn't…
Do you think that in the future there's still a value for it? This is about what hasn't been done to promote it or publicise it…but do you think there's a kind of potential for it still?
Yes. I think it's like a fine wine in that it gets better and better, because more and more information is collected about these young people, young adults. (RES02)
Reiterating the view that linkages between biological materials and bio-information are central to the generation of new forms of biovalue (Parry Citation2004; Gere and Parry Citation2006; Mazanderani, Locock, and Powell Citation2013), they speculated that the value of the placentas could be enhanced by collecting the next generation placentas in Children of “Children of the 90s” (COCO90s), underscoring our contention that it is the placenta's distinctive status as a connective tissue (here between generations) that is valued.
Mother's accounts drew attention to the biographical heritage of the material, their personal birth stories and what the placenta might be able say about them and their children. What neither group acknowledged, but which was an emergent theme within these accounts, was the performative work the collection does to embody the study population of both mothers and their children. Curating the collection, in cold storage, “down on the farm,” may have meant that the collection was kept in the dark, away from the daily business of ALSPAC's headquarters but there was no question it would be destroyed. Rather, the collection was an investment in a future that had yet to be defined and a potent reminder of the many women and children who continue to be regarded as a valuable study population. The views of those children, some of whom have become the generation of mothers and fathers now being asked to donate new placenta for the biobank, will be interesting to explore as the next chapter in this story.
Acknowledgements
We are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses. This publication is the work of the authors who will serve as guarantors for the contents of this paper.
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
Maria Fannin http://orcid.org/0000-0002-8922-2499
Additional information
Funding
Notes
1. According to newspaper reports, between 1976 and 1993 Pasteur Mérieux UK collected 360 tons of frozen placental tissue each year from 282 British hospitals and sent them to France for use in manufacturing immunoglobulin, veinglobuline and albumin. For a discussion of Institut Mérieux and its role in sourcing placenta for the production of blood products, see Hagen (Citation1993).
2. Avon Longitudinal Study of Parents and Children (ALSPAC), see http://www.bristol.ac.uk/alspac/. For access to the searchable data dictionary that includes details of available study data, see http://www.bris.ac.uk/alspac/researchers/data-access/data-dictionary/.
3. Two hundred invitation letters were sent to ALSPAC mothers and 12 agreed to be interviewed.
4. The study was approved by the ALSPAC Law and Ethics Committee at the University of Bristol. We had also hoped to analyze the historical documents of this committee but these were in the process of being archived. See http://www.bristol.ac.uk/alspac/.
5. In 2011–2012, ALSPAC received on average 14 proposals per month to access study data.
6. Some identical twins share a placenta.
7. Apgar scoring is an assessment of a newborn's breathing, heart rate, skin color, muscle tone and reflexes and is carried out 1 minute and again at 5 minutes after birth. A score between 7 and 9 is considered normal.
8. In a workshop held on ‘Ethics in Midwifery’ at the University of the West of England in May 2013.
9. The Bristol Royal Infirmary and Liverpool's Alder Hey hospital were among a number of UK hospitals whose retention of children's and adult's tissues postmortem without relatives’ consent became the center of a public controversy, leading to the creation of a new legal framework for the collection, storage and use of human tissue in the Human Tissue Act 2004.
10. See for example Baby Biobank https://www.ucl.ac.uk/tapb/sample-and-data-collections-at-ucl/biobanks-ucl/baby-biobank (Accessed November 2013).
References
- Anderson, W. 2012. “Objectivity and Its Discontents.” Social Studies of Science 43 (4): 557–576. doi: 10.1177/0306312712455732
- Anon. 1989. “Study on Factors Influencing Child Health.” Lancet 334 (8661): 518.
- Barker, D., C. Osmond, S. Grant, K. L. Thornburg, C. Cooper, S. Ring, and G. Davey Smith. 2013. “Maternal Cotyledons at Birth Predict Blood Pressure in Childhood.” Placenta 34 (8): 672–675. doi: 10.1016/j.placenta.2013.04.019
- Birch, K., and D. Tyfield. 2013. “Theorizing the Bioeconomy: Biovalue, Biocapital, Bioeconomics or … What?” Science, Technology & Human Values 38 (3): 299–327. doi: 10.1177/0162243912442398
- Brand, A. M., and N. M. Probst-Hensch. 2007. “Biobanking for Epidemiological Research and Public Health.” Pathobiology 74 (4): 227–238. doi: 10.1159/000104450
- Brown, N., A. Faulkner, J. Kent, and M. Michael. 2006. “Regulating Hybrids: ‘Making a Mess’ and ‘Cleaning Up’ in Tissue Engineering and Transpecies Transplantation.” Social Theory & Health 4 (1): 1–24. doi: 10.1057/palgrave.sth.8700062
- Brown, N., and A. Kraft. 2006. “Blood Ties: Banking the Stem Cell Promise.” Technology Analysis & Strategic Management 18 (3/4): 313–327. doi: 10.1080/09537320600777044
- Brown, N., A. Kraft, and P. Martin. 2006. “The Promissory Pasts of Blood Stem Cells.” BioSocieties 1 (3): 329–348. doi: 10.1017/S1745855206003061
- Busby, H. 2006. “Biobanks, Bioethics and Concepts of Donated Blood in the UK.” Sociology of Health & Illness 28 (6): 850–865. doi: 10.1111/j.1467-9566.2006.00546.x
- Busby, H., J. Kent, and A. M. Farrell. 2014. “Revaluing Donor and Recipient Bodies in the Globalised Blood Economy: Transitions in Public Policy on Blood Safety in the United Kingdom.” Health 18 (1): 79–94.
- Busby, H., and P. Martin. 2006. “Biobanks, National Identity and Imagined Genetic Communities: The Case of UK Biobank.” Science as Culture 15 (3): 237–251. doi: 10.1080/09505430600890693
- Chaddha, V., W. M. Whittle, and J. C. Kingdom. 2004. “Improving the Diagnosis and Managements of Fetal Growth Restriction: The Rationale for a Placenta Clinic.” Fetal and Maternal Medicine Review 15 (3): 205–230. doi: 10.1017/S0965539504001299
- Children of the 90s. 2012. Twenty One Years: Our Journey, Celebrating Children of the 90s 1991–2012. Bristol: University of Bristol.
- Colls, R., and M. Fannin. 2013. “Placental Surfaces and the Geographies of Bodily Interiors.” Environment and Planning A 45 (5): 1087–1104. doi: 10.1068/a44698
- Cooper, M. 2008. Life as Surplus: Biotechnology and Capitalism in the Neoliberal Era. Seattle: University of Washington Press.
- Cooper, M., and C. Waldby. 2014. Clinical Labour: Tissue Donors and Research Subjects in the Global Bioeconomy. Durham, NC: Duke University Press.
- Cremers, G. E., and K. G. Low. 2014. “Attitudes Toward Placentophagy: A Brief Report.” Health Care for Women International 35 (2): 113–119. doi: 10.1080/07399332.2013.798325
- Davies, G. 2013. “Writing Biology with Mutant Mice: The Monstrous Potential of Post Genomic Life.” Geoforum 48: 268–278. doi: 10.1016/j.geoforum.2011.03.004
- Dzierzak, E., and C. Robin. 2010. “Placenta as a Source of Hematopoietic Stem Cells.” Trends in Molecular Medicine 16 (8): 361–367. doi: 10.1016/j.molmed.2010.05.005
- Evangelista, M., M. Soncini, and O. Parolini. 2008. “Placenta-Derived Stem Cells: New Hope for Cell Therapy?” Cytotechnology 58 (1): 33–42. doi: 10.1007/s10616-008-9162-z
- Fannin, M. 2011. “Personal Stem Cell Banking and the Problem with Property.” Social and Cultural Geography 12 (4): 339–356. doi: 10.1080/14649365.2011.574795
- Fannin, M. 2013. “The Hoarding Economy of Endometrial Stem Cell Banking.” Body & Society 19 (4): 32–60. doi: 10.1177/1357034X13479147
- Franklin, S. 2007a. “‘Crook’ Pipettes: Embryonic Emigrations from Agriculture to Reproductive Biomedicine.” Studies in History and Philosophy of Biological and Biomedical Sciences 38 (2): 358–373. doi: 10.1016/j.shpsc.2007.03.004
- Franklin, S. 2007b. Dolly Mixtures: The Remaking of Genealogy. Durham, NC: Duke University Press.
- Fraser, A., C. Macdonald-Wallis, K. Tilling, A. Body, J. Golding, G. Davey Smith, G. Henderson, et al. 2012. “Cohort profile: The Avon Longitudinal Study of Parents and Children: ALSPAC Mothers Cohort.” International Journal of Epidemiology 42 (1): 97–110. doi: 10.1093/ije/dys066
- Gere, C., and B. Parry. 2006. “The Flesh Made Word: Banking the Body in the Age of Information.” BioSocieties 1 (1): 41–54. doi: 10.1017/S1745855205050076
- Girardi, T., C. M. Salafia, C. Platt, D. P. Misra, R. Shah, and G. Merz. 2014. “Angiogenesis Drives Neurogenesis: Fetal-Placental Vascular Network Structure in a Population Based Cohort of ASD and Matched Controls.” Paper delivered at international meeting for autism research, Atlanta, Georgia, May 15.
- Golding, J. 1989. “European Longitudinal Study of Pregnancy and Childhood (ELSPAC).” Paediatric and Perinatal Epidemiology 3 (4): 460–469. doi: 10.1111/j.1365-3016.1989.tb00533.x
- Gottweis, H., and A. Petersen. eds. 2008. Biobanks: Governance in Comparative Perspective. Abingdon: Routledge.
- Greenhough, B. 2011. “Citizenship, Care and Companionship: Approaching Geographies of Health and Bioscience.” Progress in Human Geography 35 (2): 153–171. doi: 10.1177/0309132510376258
- Greenleaf, G., and J. F. Hansbrough. 1994. “Current Trends in the Use of Allograft Skin for Patients with Burns and Reflections on the Future of Skin Banking in the United States.” Journal of Burn Care and Rehabilitation 15 (5): 428–431. doi: 10.1097/00004630-199409000-00009
- Guillaume-Gentil, O., O. V. Semenov, A. H. Zisch, R. Zimmermann, J. Vörös, M. Ehrbar. 2011. “pH-Controlled Recovery of Placenta-Derived Mesenchymal Stem Cell Sheets.” Biomaterials 32 (19): 4376–4384. doi: 10.1016/j.biomaterials.2011.02.058
- Hagen, P. 1993. Blood Transfusion in Europe: A “White Paper”. Strasbourg: Council of Europe Press.
- Haimes, E., and M. Whong-Barr. 2004. “Levels and Styles of Participation in Genetic Databases: A Case Study of the North Cumbria Community Genetics Project.” In Genetic Databases: Socio-ethical Issues in the Collection and Use of DNA, edited by R. Tutton and O. Corrigan, 57–77. London: Routledge.
- Hargitai, B. 2004. “Koraszülöttek, újszülöttek tüdo és agykárosodásának etiológiájára valamint pathogenezisére irányuló vizsgálatok [Etiology and Pathogenesis of Chronic Lung Disease and Hypoxic-Ischaemic Brain Damage in Term and Preterm Neonates].” PhD thesis, Semmelweis University, Budapest. Summary accessible here http://phd.semmelweis.hu/mwp/phd_live/vedes/export/hargitaibeate.e.pdf.
- Helsel, D. G., and M. Mochel. 2002. “Afterbirths in the Afterlife: Cultural Meaning of Placental Disposal in a Hmong American Community.” Journal of Transcultural Nursing 13 (4): 282–286. doi: 10.1177/104365902236702
- Hirtzlin, I., C. Dubreuil, N. Préaubert, J. N. Duchier, B. Jansen, J. Simon, P. Lobato de Faria, et al. 2003. “An Empirical Survey of Biobanking of Human Genetic Material and Data in Six EU Countries.” European Journal of Human Genetics 11 (6): 475–488. doi: 10.1038/sj.ejhg.5201007
- Hoeyer, K. 2003. “‘Science is Really Needed – That's All I Know’: Informed Consent and the Non-Verbal Practices of Collecting Blood for Genetic research in Northern Sweden.” New Genetics and Society 22 (3): 229–244. doi: 10.1080/1463677032000147199
- Hoeyer, K. 2008. “The Ethics of Research Biobanking: A Critical Review of the Literature.” Biotechnology and Genetic Engineering Reviews 25 (1): 429–452. doi: 10.5661/bger-25-429
- Hoeyer, K. 2013. Exchanging Human Bodily Material: Rethinking Bodies and Markets. New York: Springer.
- Jangsten, E., A. L. Hellström, and M. Berg. 2010. “Management of the Third Stage of Labour – Focus Group Discussions with Swedish Midwives.” Midwifery 26 (6): 609–614. doi: 10.1016/j.midw.2008.12.004
- Kent, J. 2008. “The Fetal Tissue Economy: From the Abortion Clinic to the Stem Cell Laboratory.” Social Science and Medicine 67 (11): 1747–1756. doi: 10.1016/j.socscimed.2008.09.027
- Kent, J. 2012. Regenerating Bodies: Tissue and Cell Therapies in the Twenty-First Century. Abingdon: Routlege.
- Kent, J., and R. ter Meulen. 2011. “Public Trust and Public Bodies: The Regulation of the Use of Human Tissue for Research in the UK.” In Biobanks and Tissue Research, edited by C. Lenk, J. Sandor, and B. Gordijn, 17–35. New York: Springer.
- Knoppers, B. M., M. H. Zawati, and E. S. Kirby. 2012. “Sampling Populations of Humans Across the World: ELSI Issues.” Annual Review of Genomics and Human Genetics 13: 395–413. doi: 10.1146/annurev-genom-090711-163834
- Kowal, E. 2013. “Orphan DNA: Indigenous Samples, Ethical Biovalue and Postcolonial Science.” Social Studies of Science 43 (4): 577–597. doi: 10.1177/0306312712471739
- Landecker, H. 2007. Culturing Life: How Cells Became Technologies. Cambridge, MA: Harvard University Press.
- Lenk, C., J. Sandor, and B. Gordijn. 2011. Biobanks and Tissue Research. New York: Springer.
- Martin, P., N. Brown, and A. Kraft. 2008a. “From Bedside to Bench? Communities of Promise:Translational Research and the Making of Blood Stem Cells.” Science as Culture 17 (1): 29–41. doi: 10.1080/09505430701872921
- Martin, P., N. Brown, and A. Turner. 2008b. “Capitalizing Hope: The Commercial Development of Umbilical Cord Blood Stem Cell Banking.” New Genetics and Society 27 (2): 127–143. doi: 10.1080/14636770802077074
- Mazanderani, F., L. Locock and J. Powell. 2013. “Biographical Value: Towards a Conceptualisation of the Commodification of Illness Narratives in Contemporary Healthcare.” Sociology of Health & Illness 35 (6): 891–905. doi: 10.1111/1467-9566.12001
- Meloni, M., and G. Testac. 2014. “Scrutinizing the Epigenetics Revolution.” BioSocieties 9 (2): 431–456. doi:10.1057/biosoc.2014.22.
- Mitchell, R., and C. Waldby. 2010. “National Biobanks: Clinical Labor, Risk Production and the Creation of Biovalue.” Science, Technology & Human Values 35 (3): 330–355. doi: 10.1177/0162243909340267
- Nash, C. 2013. “Genome Geographies: Mapping National Ancestry and Diversity in Human Population Genetics.” Transactions of the Institute of British Geographers 38 (2): 193–206. doi: 10.1111/j.1475-5661.2012.00512.x
- Nyhart, L. 1995. Biology Takes Form: Animal Morphology and the German Universities, 1800–1900. Chicago, IL: University of Chicago Press.
- Overy, C., L. A. Reynolds, and E. M. Tansey, eds. 2012. History of the Avon Longitudinal Study of Parents and Children (ALSPAC), c. 1980–2000. Wellcome Witnesses to Twentieth Century Medicine, Vol. 44. London: Queen Mary, University of London.
- Parolini, O., F. Alviano, G. P. Bagnara, G. Bilic, H. J. Bühring, M. Evangelista, S. Hennerbichler, et al. 2008. “Concise Review: Isolation and Characterization of Cells from Human Term Placenta: Outcome of the First International Workshop on Placenta Derived Stem Cells.” Stem Cells 26 (2): 300–311. doi: 10.1634/stemcells.2007-0594
- Parolini, O., and M. Caruso. 2011. “Review: Preclinical Studies on Placenta-Derived Cells and Amniotic Membrane: An Update.” Placenta 32 (4): S186–S195. doi: 10.1016/j.placenta.2010.12.016
- Parry, B. 2004. Trading the Genome: Investigating the Commodification of Bio-Information. New York: Columbia University Press.
- Parry, B., and C. Gere. 2006. “Contested Bodies: Property Models and the Commodification of Human Biological Artefacts.” Science as Culture 15 (2): 139–158. doi: 10.1080/09505430600708036
- Pearson, H. 2012. “Children of the 90s: Coming of Age.” Nature 484 (7393): 155–158. doi: 10.1038/484155a
- Rabinow, P., and N. Rose. 2006. “Biopower Today.” BioSocieties 1 (2): 195–217. doi: 10.1017/S1745855206040014
- Radin, J. 2013. “Latent Life: Concepts and Practices of Human Tissue Preservation in the International Biological Program.” Social Studies of Science 43 (4): 484–508. doi: 10.1177/0306312713476131
- Rajan, K. S. 2006. Biocapital: The Constitution of Postgenomic Life. Durham, NC: Duke University Press.
- Raman, S., and R. Tutton. 2010. “Life, Science, and Biopower.” Science, Technology and Human Values 35 (5): 711–734. doi: 10.1177/0162243909345838
- Rose, N. 2006. The Politics of Life Itself: Biomedicine, Power, and Subjectivity in the Twenty-First Century. Princeton, NJ: Princeton University Press.
- Sabatino, M., J. Ren, V. David-Ocampo, L. England, M. McGann, M. Tran, S. A. Kuznetsov, et al., 2012. “The Establishment of a Bank of Stored Clinical Bone Marrow Stromal Cell Products.” Journal of Translational Medicine 10 (23). doi:10.1186/1479-5876-10-23.
- Salafia, C. M. 2013. “Prenatal Origins of Autism as Reflected in Placental Structure and Function – Experience with the ALSPAC and EARLI Cohort.” Paper delivered at New York State Institute for basic research in developmental disabilities, Staten Island, New York, February 20.
- Santoro, P. 2011. “Liminal Biopolitics: Towards a Political Anthropology of the Umbilical Cord and the Placenta.” Body & Society 17 (1): 73–93. doi: 10.1177/1357034X10394668
- Svendsen, M. N. 2007. “Between Reproductive and Regenerative Medicine: Practising Embryo Donation and Civil Responsibility in Denmark.” Body & Society 13 (4): 21–45. doi: 10.1177/1357034X07087098
- Titmuss, R. 1997. The Gift Relationship: From Human Blood to Social Policy. New York: The New Press.
- Waldby, C., and R. Mitchell. 2006. Tissue Economies: Blood, Organs, and Cell Lines in Late Capitalism. Durham, NC: Duke University Press.
- Yoshizawa, R. S. 2013. “Review: Public Perspectives on the Utilization of Human Placentas in Scientific Research and Medicine.” Placenta 34 (1): 9–13. doi: 10.1016/j.placenta.2012.10.014
