Abstract
This paper reports on the feasibility and preliminary effects of a decision aid (DA) about female fertility preservation (FP). We conducted a pilot multicentre randomized controlled trial of women with breast cancer aged 18–40 who were randomized to brochures or the DA. Over 18 months, 62 women were eligible, of which 42 were invited by their healthcare provider (74%) to participate in the study. A total of 36 women signed up for participation and 26 (72%) were randomized to brochures (n = 13) or the DA (n = 13). In both groups, many women (87%) read the brochures and eight women used all available brochures. In the intervention group, 7/13 women logged in to the DA. Women who received brochures had slightly less decisional conflict, whereas knowledge improved in both groups. Our results indicate that both brochures about FP and a detailed DA have beneficial effects with regard to knowledge, but the DA seemed to introduce slightly more decisional conflict (DC) than the brochures. Although we encountered challenges with recruitment, our design and measurements seem feasible and the effects of the information materials seem promising, hence justifying conducting a larger study.
Introduction
Infertility or concerns about (in)fertility due to cancer treatment have a negative influence on quality of life (Partridge et al., Citation2004; Wenzel, DeAlba, et al., Citation2005). Therefore, interest in possibilities for fertility preservation (FP) has increased. At this moment, options to try to preserve fertility prior to oncology treatment are the cryopreservation of in vitro fertilized embryos, oocytes, and ovarian tissue, and suppression of the ovaries. The success rates of these options range from 5 to 25% (Garvelink, ter Kuile, Hilders, Stiggelbout, & Louwé, Citation2013). Despite an increasing number of studies and guidelines demonstrating the need for discussion of FP issues with cancer patients, information provision about treatment-induced infertility and FP techniques and referral for FP are still not sufficient and often provided too late (Dunn & Steginga, Citation2000; Jenninga, Hilders, Louwe, & Peters, Citation2008; Nakayama et al., Citation2009; Quinn et al., Citation2007; Rosen, Rodriguez-Wallberg, & Rosenzweig, Citation2009; Thewes et al., Citation2005; Tschudin & Bitzer, Citation2009).
Adequate information fulfils psychosocial needs (Peate, Meiser, Hickey, & Friedlander, Citation2009), increases coping with cancer (Ream & Richardson, Citation1996) and enables informed decision making (DM) (Mersereau et al., Citation2013). An informed decision is a decision based on relevant, best available evidence and reflects a patient’s values (Michie, Dormandy, & Marteau, Citation2002). Informed DM is especially important in deciding on treatments with possible long term consequences for quality of life such as FP options.
To support informed DM, and improve information provision about FP, a web-based Decision Aid (DA) was developed in Dutch (Garvelink, Ter Kuile, Fischer, et al., Citation2013). With the availability of this DA, every patient who is eligible for counselling about FP can obtain optimal information about FP at any time and in any location.
We sought to pilot test the feasibility and effects of the detailed DA compared to brochures about FP on decisional conflict (DC), knowledge, regret, and reproductive concerns. To this end, we conducted a multicentre randomized controlled trial with young women with breast cancer in oncology and gynaecology departments of medical centres in the Netherlands.
Materials and methods
Study design
A pilot multicentre randomized controlled trial, with randomization between informational brochures or a DA about FP, stratified by medical centre. We used a block randomization scheme with variable blocks sizes, developed by the department of medical statistics of the Leiden University Medical Centre (LUMC). The study was approved by the Medical Ethics Committee of LUMC (Dutch trial register NL32155.058.11).
Intervention and control
The DA is a web-based tool consisting of five chapters (26 separate web pages) with textual information, and a values clarification exercise to weigh pros and cons of the FP options (nine separate web pages; www.borstkankerenkinderwens.nl). The DA was developed using a systematic, user-centred process with involvement of patients and clinicians (Garvelink, Ter Kuile, Fischer, et al., Citation2013). The paper-based brochures (control) and web-based DA (intervention) contained the same information about FP options and about cancer treatments and their impact on fertility, but the DA additionally contained background information about normal fertility, an explicit values clarification exercise, and a question prompt sheet (Garvelink, Ter Kuile, Fischer, et al., Citation2013). The DA contained all information in one source, whereas the brochures contained information on one FP-option per brochure. There were in total four different brochures: a general brochure about breast cancer treatment and FP, and a separate brochure for each of the FP-options (cryopreservation of ovarian tissue, embryos and oocytes). Both the brochures and the DA fulfilled the six minimal qualifying criteria for DAs (Elwyn et al., Citation2009; Joseph-Williams et al., Citation2014).
Participants, recruitment strategy and setting
Eligible participants were female breast cancer patients between 18 and 40 years old, who were likely to receive chemotherapy, and who were eligible for FP. Women had to speak Dutch and have access to the Internet. Participants were invited to take part in the study either by their surgeon, oncologist or breast cancer nurse soon after diagnosis but before they were referred for counselling about FP; or by their specialised gynaecologist or fertility specialist, after (referral for) a first counselling consultation about FP (but before their decision to undergo FP or not had been made).
Eligible women received an envelope containing an invitation letter, a study brochure, and a general brochure about breast cancer and fertility. Women either enrolled themselves in the study, or let their breast cancer nurse/clinician do it. After signing up, they received the baseline questionnaire by e-mail. All women gave informed consent. Randomization took place after completion of the baseline questionnaire, with a link to the web-based DA or to a digital version of the brochures. All brochures were also publicly available, since we did not want to withhold relevant information from patients who did not participate in this study. Most participating medical centres handed out the brochures to all eligible patients, including those in the DA group. Respondents received 10 euros for completing three questionnaires.
Oncology departments of 26 medical centres had agreed to participate in the study, of which 13 actually recruited women. In addition, in three medical centres specialized gynaecologists or fertility specialists recruited women. Data were collected between June 2011 and December 2012.
Measurements
(i) Feasibility outcomes
Feasibility of the recruitment was measured by the proportion of participants eligible, invited and recruited after 16 months and the proportion of completed questionnaires after 18 months. For this we invited healthcare professionals in participating centres to complete a short questionnaire about their recruitment in the first 16 months.
(ii) Use of information
Individual website statistics were used to measure time spent on each page and on the total DA, and number and types of pages viewed during the visit. In addition, women were asked to indicate for each brochure whether they had read it and if so how thoroughly they had read it.
(iii) Effectiveness of the DA and other measures
Secondary outcomes were assessed using an online self-report questionnaire at baseline (T0), six weeks after T0, when a decision was expected to be made (T1), and six months after T0, when we expected women to be able to look back at the decision (T2).
Socio-demographic and medical characteristics were measured at baseline, with possibility to change them in follow-up questionnaires.
FP preference was measured with a single question at T0/T1/T2; the actual decision was measured at T1/T2.
Decisional conflict was measured at T1/T2 with the Decisional Conflict Scale (DCS; including its subscales DM uncertainty, informed DM, values clarity, DM support, effective DM), validated for a Dutch population (Koedoot et al., Citation2001; O’Connor, Citation1995). The 16 items are measured on a 5-point Likert scale ranging from 0 (totally disagree) to 4 (totally agree). Total scores range from 0-100. A higher score indicates more DC. Cronbach’s α (T1) was 0.82 for the total DCS (T1; subscales ranged from α = 0.42–0.69).
Knowledge about FP was measured at T0/T1/T2 with 10 statements, with answering categories “true”, “false”, or “do not know” (e.g. “Cryopreservation of embryos is possible until the age of 40 [true]”). Total scores range from 0 to 10.
Reproductive concerns were measured at T0/T1/T2 with a Dutch version of the Reproductive Concerns Scale (RCS) (Garvelink, Ter Kuile, Louwe, Hilders, & Stiggelbout, Citation2015; Wenzel, Berkowitz, Robinson, Bernstein, & Goldstein, Citation1992; Wenzel, Dogan-Ates, et al., Citation2005). The Dutch version of the scale consists of 11 of the 14 original items, measured on a 5-point scale ranging from 0 (not at all) to 4 (very much). Total scores range from 0 to 44. Cronbach’s α (T0) was 0.83.
Decisional regret related to FP was measured at T1/T2 with a 5-item decision regret scale (Brehaut et al., Citation2003). Items were measured on a 5-point Likert scale ranging from 0 (totally disagree) to 4 (totally agree). Total scores range from 0 to 20. Cronbach’s α of the decisional regret scale (T1) was 0.61. At baseline we measured anticipated regret, with two items asking after the extent to which women expected to have regret if they did not pursue FP now, when they would appear to be infertile after cancer treatment and if they did pursue FP now, when they would appear to still be fertile after cancer (van Dijk, van Roosmalen, Otten, & Stalmeier, Citation2008).
Analyses
Data were analysed descriptively. Due to the small number of participants we used nonparametric tests for all statistical analyses. Data analyses were done with SPSS 20.0 for Windows (IBM Corp., Armonk, NY). To perform analyses on as many participants as possible, missing data on outcome measures at T1 and T2 were handled using Multiple Imputation (Barnes, Lindborg, & Seaman, Citation2006; Graham, Citation2009). We used data on randomization group and all continuous secondary outcomes as predictors in the imputation model. Data were imputed five times, and combined using Rubin’s (Citation1987) rules for multiple imputation.
Results
Participants
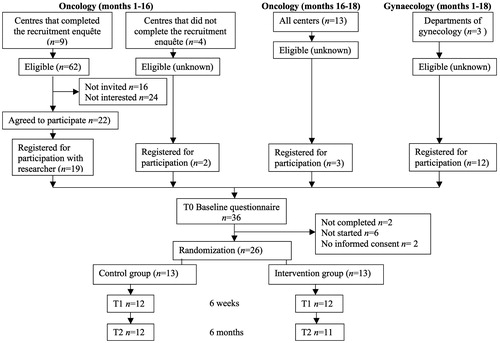
Thirty-six women were enrolled into the study, of which six did not start the baseline questionnaire, two did not give informed consent and two did not complete the baseline questionnaire and could therefore not be randomized. Thus, 26 women (72%) completed the baseline questionnaire and were randomized to brochures (n = 13) or the DA (n = 13) (). In both groups 12 women (92%) completed the T1 questionnaire, and the T2 questionnaire was completed by 12 (92%) women in the control group (brochures) and 11 (85%) randomised to the DA (). Women who completed all questionnaires were somewhat higher educated than women who missed measurements. Otherwise, we did not find differences between them. Data on relevant outcome measures were therefore imputed for missing data at T1 (n = 5) and T2 (n = 5).
Feasibility of recruitment
Nine centres responded (64%) and reported 62 eligible women in the first 16 months of recruitment. Of these, 16 women had not been invited (because it was forgotten, or they had already had a consultation with a fertility specialist, did not visit their breast cancer nurse, had to undergo neo-adjuvant chemotherapy, had no desire for children, or they were invited for too many studies already). Twenty-four women were invited but did not want to participate (because they had no desire for children or had had previous pregnancies/children, had metastasized cancer, or were preoccupied with the cancer). Twenty-two women agreed to participate. Of these, 19 women enrolled into the study ().
Two women were invited by medical centres that did not complete the above mentioned questionnaire, so we do not know their relative proportion of the total number of eligible women in these centres. In addition, for the last two months of the study, and for those who were recruited by a gynaecologist or fertility specialist, we do not have as detailed recruitment information as for those women who were recruited by their oncology department in the first 16 months of the study. Moreover, three additional women signed up in the last two months, and 12 women were invited via their gynaecology department ().
Use of the information
Twenty women reported to have used the general brochure about FP (87%; three missing) (). Eight women used all available brochures. Women, who read the brochures, read the brochures completely. Of the 13 women who were randomized to the DA group, seven (54%) logged in to the DA, of whom six used the Values Clarification Exercise (VCE). The mean time spent on the DA was 29 minutes (range: 1–74). Women viewed on average 15 of the 26 informational pages (range 0–53; some pages were viewed more than once), and 9 of the 9 VCE-pages (range: 0–21).
Table 1. Use of information materials by the study participants.
Secondary outcomes
At baseline, there were no differences with regard to socio-demographic and medical characteristics between the two study groups (). With regard to outcome measures, women who received brochures had a significantly lower perception (p = 0.046) of their risk of losing fertility (M = 6.7) compared to women who received the DA (M = 8.2), but this was not correlated to other outcome measures. Otherwise there were no differences.
Table 2. Socio-demographic and medical characteristics of the participants.
Preferences and decision making
At baseline 16 women (62%) had a preference regarding FP, but none had decided to undertake it. At T1, 21 women (88%) had a preference, 23 women (96%) had made a decision (some had no choice due to characteristics of the situation, and hence no real preference). At T2 all women (n = 23) made a decision about FP: 10 women had chosen not to pursue FP (43%), 11 had cryopreserved embryos (48%), one had cryopreserved oocytes (4%), and one both oocytes and embryos (4%). There were no differences in choices between the two study groups. Five women (22%) mentioned not to have had a choice about FP.
Decisional conflict
Women who received the brochures scored significantly lower on the effective DM subscale of the DCS (indicating they made an informed, values based decision that is likely to be implemented) than women who received the DA in addition to brochures. Total DC was not significantly different. At T2 there was a weak trend towards more total DC, and effective DM in the DA group.
Knowledge
In terms of knowledge, significant differences were found between baseline and T1 (ΔM = 1.35 out of 10), and baseline and T2 (ΔM = 1.25, p = 0.004; −0.56), indicating a relative increase of 22%. There were no differences between intervention and control groups.
Regret and reproductive concerns
There were no statistically significant differences in anticipated regret between measurement moments, nor were there differences in regret between groups. Both groups showed a trend for a minor increase in regret between measurements made at T1 and T2 (ΔM = 4.9; p = 0.15; d= −0.29). At baseline, both groups anticipated more regret when not undergoing FP and becoming infertile, than when undergoing it and remaining fertile (indicating that it had not been necessary to pursue FP). There were no differences between groups or measurement moments with regard to reproductive concerns ().
Table 3. Decision making processes and outcomes for the study participants (n = 26).
Differences between women recruited via gynaecology versus oncology
Women who were recruited via their gynaecologist were recruited at a different moment in their trajectory between diagnosis and start of the oncology treatment, and may have received more information on FP than those recruited by their oncologist. Therefore, we conducted additional analyses to see whether this route influenced the outcomes. Of the women who were invited through their gynaecologist, DA use was higher compared to that of women recruited via their oncologist (80.0% versus 37.5%). Additionally, they had slightly higher baseline knowledge than those recruited by their oncologist (6.4 versus 5.0 out of 10), as well as at T1 (7.8 versus 6.4 out of 10) and T2 (7.4 versus 6.2 out of 10), but the increase in knowledge was similar between the two groups (1.0 versus 1.2 out of 10). Otherwise there were no differences with regard to the outcomes.
Discussion
This study informed the feasibility, and pilot tested the effects of a DA about FP for women with breast cancer in oncologic and gynaecologic practice. Although the intended outcomes were feasible to be measured with digital questionnaires, and the DA was feasible to provide to the respondents, we encountered challenges with recruitment of participants and subsequent participation rates. We have made an attempt to assess effectiveness of the DA compared to brochures about FP. Despite our small sample size, the study showed some remarkable findings. Women in our sample experienced relatively low levels of DC, with the suggestion of a slightly lower score on the effective DM subscale of the DCS at T1, and higher total levels of DC at T2, in women who received the DA, compared to women who received brochures (Cohen’s d = 0.34). The results of our study lead us to make five observations.
First, recruitment of women for a study to evaluate information provision, between diagnosis and start of the oncologic treatment, was difficult. Fewer women than anticipated were eligible for the study (a majority of newly diagnosed women had complete families or no desire for children), and the combination of the difficult timing in which women had to be invited, the increasing number of studies for breast cancer patients, and the burden of a cancer diagnosis made recruiters hesitant to invite them or discouraged women’s participation. Moreover, the fact that the brochures were already publicly available made participation no longer necessary to obtain the information about FP.
Second, in our study, several health professionals could invite women, but the actual enrolment into the study was done by the researcher. It might help recruitment to future studies to appoint local champions who are, and feel, responsible for inclusion of participants in their medical centre (Rendell, Merritt, & Geddes, Citation2007). Additionally, women were often given the materials to take home so that they could enrol themselves into the study, instead of directly being enrolled by their health professional. This could have been a threshold for their enrolment. In future research, it would be interesting to engage patients in designing the most appropriate procedure for recruitment in a period with such a difficult timing (Fleurence et al., Citation2014).
Third, the slightly more favourable outcomes with regard to DC in the brochure group compared to the DA group is in contrast to what we expected based on other DA evaluations (Stacey et al., Citation2014). Reasons for this may be related to the type and moment of the decision, or the design of the DA:
The decision about FP is a different type of decision when compared to screening- or treatment decisions. The decision about FP has to be made in a difficult (and short) time frame with competing demands from decisions related to surviving the cancer (Garvelink et al., Citation2015; Lee et al., Citation2011). Explicit confrontation through a DA may therefore increase DC;
Our data indicated that a majority of the women had strong baseline preferences and may have made their decision before seeing the DA, or did not experience a choice because the preferred FP option was determined by their possibilities in combination with the highest possible success rates (Garvelink et al., Citation2015). Seeing the DA with all FP options when a decision has already been made, or when there is no choice may have (re)initiated the DM process and consequent uncertainty, which is likely to lead to more DC; and
The design and content of our DA may have suggested a difficult decision for the women [in an implicitly normative way (Molewijk, Stiggelbout, Otten, Dupuis, & Kievit, Citation2003)]. Indeed, we only found significant differences in DC at T1, and not on the longer term. Moreover, all FP options are mentioned in the DA, which will not be optional for all women. For some women the availability of information about irrelevant options might be confusing, while others want to see as much information as possible (Molewijk et al., Citation2003; Stiggelbout et al., Citation2008). Importantly, a slight increase in DC is not disadvantageous (Knops et al., Citation2013; Nelson, Han, Fagerlin, Stefanek, & Ubel, Citation2007), especially when the level of conflict is not above the threshold for elevated DC (as was the case) (O'Connor, Citation1995). This may for example indicate that women are strongly involved in the decision (Nelson et al., Citation2007).
Fourth, both information sources led to a significant increase in knowledge between baseline and follow-up, comparable to other studies (Peate et al., Citation2012). Unlike other studies (Peate et al., Citation2012; Stacey et al., Citation2014) the knowledge scores in our study did not differ between groups. However, the information in the brochures and DA was highly overlapping, and women in both randomization groups read the brochures.
Fifth, when we compared our results with regard to knowledge and DC to previous data of a historical group of women who only received counselling consultation, both brochures and our DA had more favourable scores on DC and knowledge than in women who received counselling only (Garvelink, Ter Kuile, Louwe, Hilders, & Stiggelbout, Citation2013; Peate et al., Citation2012). Therefore, the benefit of any additional information with regard to knowledge and feeling supported in DM about FP is clear (Garvelink, Ter Kuile, Louwe, et al., Citation2013). However, besides additional written information, referral to a fertility expert for counselling about FP is still of utmost importance (Kim et al., Citation2013). Indeed, the information in the DA could be a good addition to information received by the gynaecologist, as suggested by our finding that women who were recruited through their gynaecologist (and hence had already received some information on FP) still had similar relative increases in knowledge between measurement moments, when compared to women recruited by their oncologist.
Some important limitations must be taken into consideration in interpreting these results. Our sample size is very small. Therefore, results are preliminary and based on non-parametric tests only. Recruitment was a huge problem in our study which may be a challenge for future larger trials. With the incidence for breast cancer in young women in the Netherlands being almost 1000 women a year, we expected to be able to include enough participants to find small effects in DC (Cohen’s d = 0.2; β = 0.2; α = 0.05) between randomization groups within 18 months. After 18 months we stopped randomization as planned, for reasons of funding. Additionally, the brochures that we used as comparison, could be considered simple DAs since they fulfilled all minimum criteria for DAs, so a priori changes of finding significant differences between the groups were low.
Future research should take into account the afore mentioned challenges in order to provide more definitive effects of the DA and to be able to formulate a final recommendation for their use in practice. However, in the meantime, it is of utmost importance that women are offered timely information about FP in addition to counselling and our results suggest that the DA as well as brochures improved knowledge and had no disadvantageous effects. Therefore, we recommend that both can be used to inform future patients, until proven otherwise. However, since use of the DA slightly increased decisional conflict, additional assistance in DM (during counselling consultations) should be available.
Acknowledgements
We are grateful to all women who have participated in this study, and for all breast cancer nurses, surgeons, oncologists, gynaecologists and fertility specialists who have recruited these women in the Leiden University Medical Centre, HAGA Hospital, Reinier de Graaf Hospital, University Medical Centre Groningen, Bronovo Hospital, Diaconessenhuis Leiden, Amsterdam Medical Centre, Jeroen Bosch Hospital, Groene Hart Hospital, Flevo Hospital, Gelre Hospital, Medical Centre Alkmaar, De Tjongerschans Hospital, Rijnstate Alysis, Dutch Cancer Institute – Antoni van Leeuwenhoek Hospital (NKI-AvL), Meander Medical Centre, Tergooi Hospital, Isala Clinics, Martini Hospital, Vie Curie Hospital, Albert Schweitzer Hospital, Diakonessenhuis Utrecht, St. Antonius Hospital, St Elisabeth Hospital, MCH Westeinde, and the Dutch Network for Fertility Preservation (NNF). We gratefully thank Professor Dawn Stacey for her valuable comments on our manuscript.
Disclosure statement
For this study we received financial support by DSW Health Insurance, Schiedam, the Netherlands and Pink Ribbon, Hilversum, the Netherlands. The authors declare that there is no conflict of interests. The authors alone are responsible for the content and writing of the paper.
References
- Barnes, S.A., Lindborg, S.R., & Seaman, J.W. Jr. (2006). Multiple imputation techniques in small sample clinical trials. Statistics in Medicine, 25, 233–245. doi: https://doi.org/10.1002/sim.2231.
- Brehaut, J.C., O’connor, A.M., Wood, T.J., Hack, T.F., Siminoff, L., Gordon, E., & Feldman-Stewart, D. (2003). Validation of a decision regret scale. Medical Decision Making, 23, 281–292. doi: https://doi.org/10.1177/0272989x03256005.
- Dunn, J., & Steginga, S.K. (2000). Young women's experiences of breast cancer: Defining young and identifying concerns. Psycho-Oncology, 9, 137–146. doi: https://doi.org/10.1002/(SICI)1099-1611(200003/04)9:2 < 137::AID-PON442 > 3.0.CO;2-0.
- Elwyn, G., O'connor, A.M., Bennett, C., Newcombe, R.G., Politi, M., Durand, M.A., … Edwards, A. (2009). Assessing the quality of decision support technologies using the international patient decision aid standards instrument (IPDASi). Plos One, 4, e4705. doi: https://doi.org/10.1371/journal.pone.0004705.
- Fleurence, R.L., Forsythe, L.P., Lauer, M., Rotter, J., Ioannidis, J.P.A., Beal, A., … Selby, J.V. (2014). Engaging patients and stakeholders in research proposal review: The patient-centered outcomes research institute engaging patients and stakeholders in research proposal review. Annals of Internal Medicine, 161, 122–130. doi: https://doi.org/10.7326/m13-2412.
- Garvelink, M., ter Kuile, M., Hilders, G., Stiggelbout, A., & Louwé, L. (2013). Fertiliteits preservatie voor chemotherapie [Fertility preservation for chemotherapy]. Nederlands Tijdschrift Voor Oncologie, 10, 97–104. Retrieved from www.ariez.nl/DownloadFile.lynkx?guid=8cc4b4db-4f4e-4a04.
- Garvelink, M., Ter Kuile, M., Louwe, L., Hilders, C., & Stiggelbout, A. (2013). Pilot study of a decision aid about fertility preservation for breast cancer patients. Psycho-Oncology, 22, 353. 354. doi: https://doi.org/10.1111/j.1099-1611.2013.3394.
- Garvelink, M.M., Ter Kuile, M., Fischer, M.J., Louwe, L., Hilders, C., Kroep, J.R., & Stiggelbout, A. (2013). Development of a decision aid about fertility preservation for women with breast cancer in The Netherlands. Journal of Psychosomatic Obstetrics and Gynaecology, 34, 170–178. doi: https://doi.org/10.3109/0167482x.2013.851663.
- Garvelink, M.M., Ter Kuile, M., Bakker, R.M., Geense, W.J., Jenninga, E., Louwe, L., … Stiggelbout, A. (2015). Women's experiences with information provision and deciding about fertility preservation in the Netherlands: 'satisfaction in general, but unmet needs'. Health Expectations, 18, 956–968. doi: https://doi.org/10.1111/hex.12068.
- Garvelink, M.M., Ter Kuile, M.M., Louwe, L.A., Hilders, C.G., & Stiggelbout, A.M. (2015). Validation of a Dutch version of the Reproductive Concerns Scale (RCS) in three populations of women. Health Care for Women International, 36, 1143–1159. doi: https://doi.org/10.1080/07399332.2014.993036.
- Graham, J.W. (2009). Missing data analysis: Making it work in the real world. Annual Review of Psychology, 60, 549–576. doi: https://doi.org/10.1146/annurev.psych.58.110405.085530.
- Jenninga, E., Hilders, C.G., Louwe, L.A., & Peters, A.A. (2008). Female fertility preservation: Practical and ethical considerations of an underused procedure. Cancer Journal, 14, 333–339. doi: https://doi.org/10.1097/PPO.0b013e31818860ac.
- Joseph-Williams, N., Newcombe, R., Politi, M., Durand, M., Sivell, S., Stacey, D., … Elwyn, G. (2014). Toward minimum standards for certifying patient decision aids: A modified Delphi consensus process. Medical Decision Making, 34, 699–710. doi: https://doi.org/10.1177/0272989x13501721.
- Kim, J., Deal, A.M., Balthazar, U., Kondapalli, L.A., Gracia, C., & Mersereau, J.E. (2013). Fertility preservation consultation for women with cancer: Are we helping patients make high-quality decisions?. Reproductive Biomedicine Online, 27, 96–103. doi: https://doi.org/10.1016/j.rbmo.2013.03.004.
- Knops, A.M., Goossens, A., Ubbink, D.T., Legemate, D.A., Stalpers, L.J., & Bossuyt, P.M. (2013). Interpreting patient decisional conflict scores: Behavior and emotions in decisions about treatment. Medical Decision Making, 33, 78–84. doi: https://doi.org/10.1177/0272989x12453500.
- Koedoot, N., Molenaar, S., Oosterveld, P., Bakker, P., de Graeff, A., Nooy, M., … de Haes, H. (2001). The decisional conflict scale: Further validation in two samples of Dutch oncology patients. Patient Education and Counseling, 45, 187–193. doi: https://doi.org/10.1016/s0738-3991(01)00120-3.
- Lee, R.J., Wakefield, A., Foy, S., Howell, S.J., Wardley, A.M., & Armstrong, A.C. (2011). Facilitating reproductive choices: The impact of health services on the experiences of young women with breast cancer. Psychooncology, 20, 1044–1052. doi: https://doi.org/10.1002/pon.1826.
- Mersereau, J.E., Goodman, L.R., Deal, A.M., Gorman, J.R., Whitcomb, B.W., & Su, H.I. (2013). To preserve or not to preserve: How difficult is the decision about fertility preservation?. Cancer, 119, 4044–4050. doi: https://doi.org/10.1002/cncr.28317.
- Michie, S., Dormandy, E., & Marteau, T.A. (2002). The multi-dimensional measure of informed choice: A validation study. Patient Education and Counseling, 48, 87–91. doi: https://doi.org/10.1016/S0738-3991(02)00089-7.
- Molewijk, A.C., Stiggelbout, A.M., Otten, W., Dupuis, H.M., & Kievit, J. (2003). Implicit normativity in evidence-based medicine: A plea for integrated empirical ethics research. Health Care Analysis, 11, 69–92. doi: https://doi.org/10.1023/A:1025390030467.
- Nakayama, K., Liu, P., Detry, M., Schover, L.R., Milbourne, A., Neumann, J., … Ueno, N.T. (2009). Receiving information on fertility- and menopause-related treatment effects among women who undergo hematopoietic stem cell transplantation: Changes in perceived importance over time. Biology of Blood and Marrow Transplantation, 15, 1465–1474. doi: https://doi.org/10.1016/j.bbmt.2009.07.019.
- Nelson, W.L., Han, P.K., Fagerlin, A., Stefanek, M., & Ubel, P.A. (2007). Rethinking the objectives of decision aids: A call for conceptual clarity. Medical Decision Making, 27, 609–618. doi: 0272989X07306780https://doi.org/10.1177/0272989X07306780.
- O'Connor, A.M. (1995). Validation of a decisional conflict scale. Medical Decision Making, 15, 25–30. doi: https://doi.org/10.1177/0272989X9501500105.
- Partridge, A.H., Gelber, S., Peppercorn, J., Sampson, E., Knudsen, K., Laufer, M., … Winer, E.P. (2004). Web-based survey of fertility issues in Young women with breast cancer. Journal of Clinical Oncology, 22, 4174–4183. doi: https://doi.org/10.1200/JCO.2004.01.159.
- Peate, M., Meiser, B., Cheah, B.C., Saunders, C., Butow, P., Thewes, B., … Friedlander, M. (2012). Making hard choices easier: A prospective, multicentre study to assess the efficacy of a fertility-related decision aid in young women with early-stage breast cancer. British Journal of Cancer, 106, 1053–1061. doi: https://doi.org/10.1038/bjc.2012.61.
- Peate, M., Meiser, B., Hickey, M., & Friedlander, M. (2009). The fertility-related concerns, needs and preferences of younger women with breast cancer: A systematic review. Breast Cancer Research and Treatment, 116, 215–223. doi: https://doi.org/10.1007/s10549-009-0401-6.
- Quinn, G.P., Vadaparampil, S.T., Gwede, C.K., Miree, C., King, L.M., Clayton, H.B., … Munster, P. (2007). Discussion of fertility preservation with newly diagnosed patients: Oncologists' views. Journal of Cancer Survivorship, 1, 146–155. doi: https://doi.org/10.1007/s11764-007-0019-9.
- Ream, E., & Richardson, A. (1996). The role of information in patients' adaptation to chemotherapy and radiotherapy: A review of the literature. European Journal of Cancer Care, 5, 132–138. doi: https://doi.org/10.1111/j.1365-2354.1996.tb00223.x.
- Rendell, J.M., Merritt, R.D., & Geddes, J.R. (2007). Incentives and disincentives to participation by clinicians in randomised controlled trials. The Cochrane Database of Systematic Reviews, 2007, MR000021. doi: https://doi.org/10.1002/14651858.MR000021.pub3.
- Rosen, A., Rodriguez-Wallberg, K.A., & Rosenzweig, L. (2009). Psychosocial distress in young cancer survivors. Seminars in Oncology Nursing, 25, 268–277. doi: https://doi.org/10.1016/j.soncn.2009.08.004.
- Rubin, D.B. (1987). Multiple imputation for nonresponse in surveys. New Jersey: John Wiley & Sons, Inc.
- Stacey, D., Bennett, C.L., Barry, M.J., Col, N.F., Eden, K.B., Holmes-Rovner, M., … Wu, J.H.C. (2014). Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews, 2014, CD001431. doi: https://doi.org/10.1002/14651858.CD001431.pub4.
- Stiggelbout, A.M., Molewijk, A.C., Otten, W., Van Bockel, J.H., Bruijninckx, C.M., Van der Salm, I., & Kievit, J. (2008). The impact of individualized evidence-based decision support on aneurysm patients' decision making, ideals of autonomy, and quality of life. Medical Decision Making, 28, 751–762. doi: https://doi.org/10.1177/0272989x08321680.
- Thewes, B., Meiser, B., Taylor, A., Phillips, K.A., Pendlebury, S., Capp, A., … Friedlander, M.L. (2005). Fertility- and menopause-related information needs of younger women with a diagnosis of early breast cancer. Journal of Clinical Oncology, 23, 5155–5165. doi: https://doi.org/10.1200/JCO.2005.07.773.
- Tschudin, S., & Bitzer, J. (2009). Psychological aspects of fertility preservation in men and women affected by cancer and other life-threatening diseases. Human Reproduction Update, 15, 587–597. doi: https://doi.org/10.1093/humupd/dmp015.
- van Dijk, S., van Roosmalen, M.S., Otten, W., & Stalmeier, P.F.M. (2008). Decision making regarding prophylactic mastectomy: Stability of preferences and the impact of anticipated feelings of regret. Journal of Clinical Oncology, 26, 2358–2363. doi: https://doi.org/10.1200/JCO.2006.10.5494.
- Wenzel, L., Berkowitz, R., Robinson, S., Bernstein, M., & Goldstein, D. (1992). The psychological, social, and sexual consequences of gestational trophoblastic disease. Gynecologic Oncology, 46, 74–81. doi: https://doi.org/10.1016/0090-8258(92)90200-3.
- Wenzel, L., DeAlba, I., Habbal, R., Kluhsman, B.C., Fairclough, D., Krebs, L.U., … Aziz, N. (2005). Quality of life in long-term cervical cancer survivors. Gynecologic Oncology, 97, 310–317. doi: https://doi.org/10.1016/j.ygyno.2005.01.010.
- Wenzel, L., Dogan-Ates, A., Habbal, R., Berkowitz, R., Goldstein, M., Kluhsman, B.C., … Cella, D. (2005). Defining and measuring reproductive concerns of female cancer survivors. Journal of the National Cancer Institute Monographs, 2005, 94–98. doi: https://doi.org/10.1093/jncimonographs/lgi017.