Abstract
There is a paucity of data on research funding levels for male reproductive health (MRH). We investigated the research funding for MRH and infertility by examining publicly accessible web-databases from the UK and USA government funding agencies. Information on the funding was collected from the UKRI-GTR, the NIHR’s Open Data Summary, and the USA’s NIH RePORT web-databases. Funded projects between January 2016 and December 2019 were recorded and funding support was divided into three research categories: (i) male-based; (ii) female-based; and (iii) not-specified. Between January 2016 and December 2019, UK agencies awarded a total of £11,767,190 to 18 projects for male-based research and £29,850,945 to 40 projects for female-based research. There was no statistically significant difference in the median funding grant awarded within the male-based and female-based categories (p = 0.56, W = 392). The USA NIH funded 76 projects totalling $59,257,746 for male-based research and 99 projects totalling $83,272,898 for female-based research Again, there was no statistically significant difference in the median funding grant awarded between the two research categories (p = 0.83, W = 3834). This is the first study examining funding granted by main government research agencies from the UK and USA for MRH. This results should stimulate further discussion of the challenges of tackling male infertility and reproductive health disorders and formulating appropriate investment strategies.
Introduction
Several recent studies have highlighted considerable research gaps in the understanding of male infertility encompassing critical areas such as basic science research, clinical diagnostics, non-Medically Assisted Reproduction (MAR) treatment options, and the impact of damage to the male genome on the health of the next generation (Barratt et al., Citation2017, Citation2018, Citation2021; De Jonge & Barratt, Citation2019; Schlegel et al., Citation2021a, Citation2021b). One general conclusion that can be drawn from these analyses is that significant funding is required to address the research questions (Barratt et al., Citation2017, Citation2018). For any discipline, including reproductive medicine, an important aspect of assessing and formulating future funding requirements is to ascertain the current funding levels. This knowledge can then be used as a starting point to facilitate strategic investments for the discipline.
Surprisingly, there is a paucity of data on funding levels for male infertility and male reproductive health research (Barratt et al., Citation2018, Citation2021). To date, only one study has specifically documented funding for male reproductive health research. Liao et al. (Citation2020) assessed funding by the National Natural Science Foundation of China (NNSFC) for male infertility and reproductive health research between 1998 and 2018. The authors split this 20-year period into 3 funding phases beginning from 1998. By the third phase (2010–2018), a substantial increase of funding was awarded for male reproductive health (MRH) basic research by the NNSFC. However, there was minimal detail on the exact funding values. Barratt et al. (Citation2021) and colleagues provided a snapshot of funding for Male Reproductive Health in several countries that suggested overall funding levels were low, but no other details were provided.
In this study, we investigated government funded support of male reproductive health research. We examined research funded between January 2016 and December 2019 from the UK and USA agencies. To provide context, we included funding for female-based reproductive health research and examined the proportion of research funding for reproductive health research and compared that to the total research funding.
Materials and methods
Experimental design
Publicly accessible UK Research and Innovation (UKRI), National Institute for Health Research (NIHR), and National Institutes of Health (NIH) funding agency databases covering awards from January 2016 to December 2019 were examined (see Supplementary Table 1). Following the inclusion and exclusion criteria outlined within Supplementary Tables 2 and 3, funding data were collected on research proposals investigating infertility and reproductive health. For simplicity, these are referred to collectively as ‘infertility research’. As the primary focus of this research is on infertility, the data were divided into three main categories: (i) male-based, (ii) female-based, and (iii) not-specified (Supplementary Table 2). The first two groups covered projects whose primary aim, based on the information presented in the research abstracts, timeline summaries and/or impact statements, was male- or female-focussed. “Not-specified” includes research projects that have either not specified a primary focus towards either male or female or have explicitly stated a focus on both. The process was conducted and reviewed by E.G. with C.L.R.B. Total funding for all three groups, funding over time, and comparison with overall funding for a particular agency was examined.
Briefly, E.G. retrieved the primary data and produced the first set of data for discussion with C.L.R.B. Both went through the complete list and discussed each study/project and decided whether: (a) it should be included or not, and (b) what category does it fell under (male-, female-, or not-specified). The abstracts, which were almost always available and provided by each research study, were all examined and scrutinised by both E.G. and C.L.R.B together. If there was clear disagreement between E.G. and C.L.R.B, which were very rare, the project would not be included.
UK data collection
Starting in April 2018, the UK research councils, Innovate UK, and Research England were combined reporting under one organisation, the UKRI (UKRI, Citation2019). The councils, such as the Medical Research Council (MRC), Biotechnology and Biological Sciences Research Council (BBSRC), Engineering and Physical Sciences Research Council (EPSRC), and Natural Environment Research Council (NERC), independently fund research projects according to their respective visions and missions; however, from 2018/19, their annual funding expenditures were reported under the UKRI’s annual reports and budgets. The UKRI’s Gateway to Research (UKRI-GTR) web-database allows users to analyse information provided on taxpayer-funded research. Relevant search terms such as “male infertility” or “female reproductive health” (see Supplementary Table 2) were applied with appropriate database filters (Supplementary Table 1). The project award relevance was determined by assessing the objectives in project abstracts, timeline summaries, and planned impacts. Supplementary Tables 1–3 provide the search filters and the reference criteria for inclusion/exclusion utilised for analysis. The UKRI-GTR provides the total funding amount granted to the projects within a designated period.
The Open Data Summary View dataset from the NIHR was used as it provided details on funded projects, grants, summary abstracts, and project dates. Like the UKRI data, the NIHR excel datasheet had specific search terms and filters applied to exclude irrelevant projects (Supplementary Tables 1–3).
The UKRI councils and NIHR report their annual expenditure and budgets for 1st April to 31st March. Thus, the selected projects will fall under the funding period of when their research activities begin (e.g. if a research project is started between May 20th, 2017 and March 20th, 2019, the project will be categorised under the funding period 2017/18). The projects assessed would begin their investigations between January 2016 and December 2019, therefore 5 consecutive funding periods were examined (2015/16, 2016/17, 2017/18, 2018/19, and 2019/20).
USA data collection
The NIH has a research portfolio online operating tools site (RePORT) providing access to their research activities, such as previously funded research, actively funded research projects, and information on NIH’s annual expenditures (NIH Report, Citation2021). The RePORT-Query database has similar features as the UKRI-GTR and NIHR such as providing information on project abstracts, research impact, start- and end-dates, funding grants, and type of research. The same inclusion-exclusion criteria were applied as for the UK data collection, (see Supplementary Tables 1–3).
In contrast to the UK funding agencies, the NIH’s fiscal year (FY) funding follows a calendar period from October 1st to September 30th (i.e. FY2016 comprises funding activity from October 1st, 2015, to September 30th, 2016). Projects running over one calendar period are reported several times under consecutive fiscal years and the funds are divided according to the annual period of the project’s activity.
During data collection, 74 projects were found as active with incomplete funding sums as the NIH divides the grants according to the budgeting period of every FY. The NIH are in the process of granting funds for the FY2021, so projects ending in FY2020 or FY2021 have provided a complete funding sum. For the active projects ending after 2021, incomplete funding data are shown. It is assumed the funding will increase in value by the time the research project ends in the future. To remain consistent with the UK data, projects granted funding are totalled as one figure and recorded under the FY the project first began research, whether they are active or completed. Thus, the USA funding is referred to as “Current Total Funding.” For the USA, the initial data collection period ran between October 2020 and December 2020 but then restarted for a brief period in January 2021 to complete the remaining funding values for several of the active research projects.
Data analysis
The data were divided into the three groups and organised into the funding period or FY during which the project was first awarded. R-Studio (Version 1.3.1093) was utilised for the data analysis. Box-and-whisker plots are presented with rounded p values. Kruskal-Wallis and Wilcoxon Rank Sum tests were generated to assess any statistical significance. The data were independently collected and do not assume a normal distribution, so rank-based, non-parametric tests such as the Kruskal-Wallis and Wilcoxon Rank-Sum were used. The Kruskal-Wallis test was used between more than 2 groups, with the p values and Chi-Squared (χ2) values provided. The Wilcoxon test was used between two groups with the p value and the Wilcoxon test statistic, W, included. P values <0.05 were considered statistically significant.
Results
Total and median funding: UK data
Total funding for infertility from the UK funding agencies and the summary statistics of the UK data are presented in . details the proportion of funding by the MRC and NIHR from 2015/16 to 2018/19. Between 2016 and 2019, 76 studies were awarded funding by 4 UKRI councils and the NIHR investigating infertility and reproductive health. The MRC, BBSRC, and NIHR were the top 3 awarding agencies, having funded 29, 23, and 15 projects, respectively. The UK agencies have awarded 18 projects for male-based, 40 for female-based, and 18 projects for the non-specified group (). For NIHR funding, there were only 2 awards for the male group compared to 11 for female group. presents a distribution of funding for the three groups. There was more spread for the female group, however there was no statistically significant difference between the mean values of the 3 groups (p = 0.69, Kruskal-Wallis, χ2 = 0.72). There was no significant difference between male-based versus female-based funding (p = 0.56, W = 392).
Figure 1. Box-and-whisker plot with a 95% confidence interval (CI) of awards for UK infertility and reproductive health research under the three research categories: (i) male-based; (ii) female-based; and (iii) not-specified. A total of 18 projects were funded for male-based research, 40 projects for female-based, and 18 for not-specified by the UKRI and NIHR.
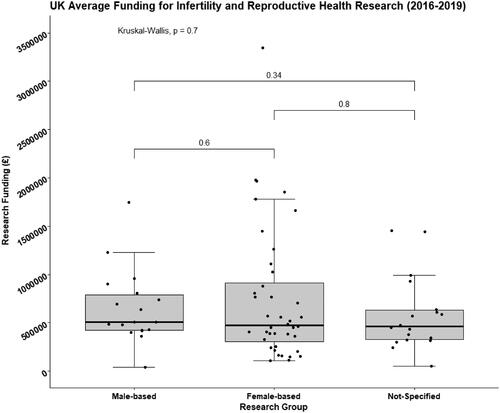
Table 1. Total funding awarded by the UKRI and NIHR agencies for infertility research groups along with annual allocated funding.
Table 2. Summary of the UK awarded research by the UKRI and NIHR.
Table 3. The UK Proportion of Funding for Infertility Research.
Total and median funding: USA data
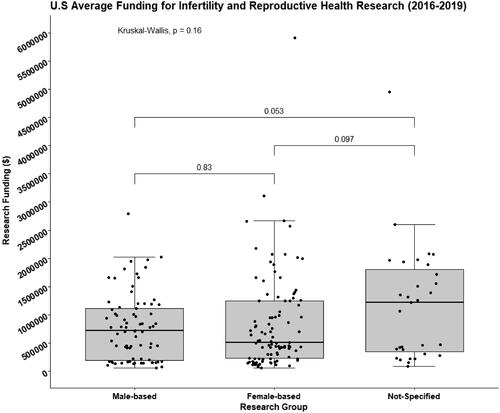
The USA total funding for infertility and summary statistics are presented in . The funding amounts presented in includes research grants, program grants, and fellowships and contains the respective annual spending of each NIH institute. The NIH have awarded 76 projects for male-based, 99 for female-based, and 31 projects for the non-specified group. The National Institute of Child Health and Human Development (NICHD), Environmental Health Sciences (NIEHS), and General Medical Sciences (NIGMS) have awarded the most for infertility research out of 14 institutes, funding 138, 27, and 26 projects, respectively.
Table 4. Current total funding for infertility research awarded by the NIH's funding institutes and the respective fiscal years.
Table 5. Summary statistics of the USA awarded research by the NIH.
The spread of funding is not largely different between the male-based and female-based groups (), but more projects appeared to localise at the lower end of the scale for the female-based group. However, there was no statistical difference between the mean values of the 3 groups (p = 0.16, Kruskal Wallis χ2 = 4.1). There were no significant differences between male- and female-based research (p = 0.83, W = 3834).
Figure 2. Box-and-whisker plot has a 95% CI of the funding collected for USA infertility and reproductive health research under the three research focus categories: (i) male-based; (ii) female-based; and (iii) not-specified. A total of 76 projects were funded for male-based, 99 projects for female-based, and 31 for not-specified group by the NIH agencies.
Funding over the years
Funding over 4 consecutive years is presented in Supplementary Tables 4 and 5 for the UK and USA, respectively. The total funding, mean funding amount over the respective funding periods, and the distribution of data are presented in Supplementary Figures 1 and 2. There were no statistically significant difference in the funding over time within each of the 3 groups (p > 0.05, Kruskal-Wallis), for both the UK and USA.
Proportion of funding for infertility and reproductive health research in the UK and USA
The proportion of funding allocated to male and female infertility research is presented in for UK and for USA. The MRC funds research for reproduction and infertility and the NIHR has a dedicated research specialty for Reproductive Health and Childbirth (NIHR, 2021). When examining funding allocated directly for infertility research by the MRC, the proportion of total funding peaks at 1.58% in 2016/17 (). For the NIHR, the largest proportion of funding allocated to infertility research was in 2019/20 with 2.31% of the year’s total awards. When examining total funding by the NIHR between 2015/16 and 2019/20, the proportion of funding for male-based infertility research was 0.07% and 0.79% for female-based research.
In the USA, of the 27 NIH institutes and research centres, the NICHD is the primary funder for furthering research on human development, improvement for reproductive health, and enhancing the lives of children and young adults (NIH, 2020). This also encompasses research for infertility and contraception development. The NICHD’s annual funding for research between fiscal years 2011 and 2020 was between $873 million and $1.1 billion (NIH, Citation2021). In the FY2016, NICHD funded $1,021,132,045 for research grants and fellowships, but only 1.63% or $16,684,751 was for infertility research (as defined by the eligibility criteria in this study; ). The funding proportion for the male-based research group was 0.48%, which was similar to the female-based funding proportion, 0.51%. The proportion of total funding provided by the NICHD between 2016 and 2019 that was allocated to infertility research was estimated at 2.56%, with male-based receiving 0.83% and female-based receiving 1.32%.
Discussion
This study provides details of UK and USA government funding for male infertility and male reproductive health covering the period 2016–2019. The information will be instructive for different stakeholders (e.g. workers in the discipline, grant organisations, commercial companies, and policy makers). This will enable the development of evidence-based informed decisions for future funding strategies. This is critical as male infertility poses a global health risk for many millions of men, yet research funding is clearly not concomitant with the prevalence or impact of the disease.
We analysed public-accessible databases for UKRI, NIHR (UK) and USA (NIH) covering the period of awards from January 2016 to December 2019. The primary objective was to determine funding for male reproductive health and infertility research. To provide context, we assessed 3 groups based on the primary focus of the research in reproductive biology/medicine: (i) male-based, (ii) female-based, and (iii) not-specified (Supplementary Table 2). Information from the aims, research abstracts, timeline summaries, and/or impact statements, was used to determine if a study was included and, if so, to which group it was assigned. This is necessarily a subjective process, therefore we provide our search and entry/exclusion criteria (Supplementary Tables 1–3), as well as a supplementary table of the research projects’ titles from the UK and USA (Supplementary Tables 4 to 7). Whilst incorporation of different terms may produce different answers, the results are robust. For example, the application of data extraction is consistent between countries as the inclusion/exclusion criteria were the same. We were focussed on infertility and associated links to infertility and reproductive disorders. No analysis was made to assess if there is bias in funding research for female reproduction versus male reproduction. Moreover, we do not examine submission numbers, triage, rejection rates, etc. and thus prioritisation of research cannot be assessed.
Although the number of awards for female-based research is generally higher than for the male group (ratio of ∼2:1 in UK, and 1.3:1 in USA), the average amount awarded per project was not significantly different in either country (see ; ), indicating that funding per project was not different between male and female reproductive health.
An important question to answer is, what is the proportion of funding for reproduction/male reproductive health compared to general research funding? There are several approaches to address this question. For both the UK and USA data, one method is to examine the total funding for research by the main funding agency and compare this to the data for male- and female-based research. Reproductive health research is primarily supported by the MRC and NIHR in the UK, and by the NICHD in the USA. In the funding periods 2015/16 to 2017/18, the total infertility research funding by MRC ranged from 0.87% to 1.58% of the total budget (). Infertility research funding from NIHR ranged from 0.08% to 2.31% (2015/16 to 2019/20, ). For the USA, the maximum infertility research funding by the NICHD was 3.39% of its total budget ().
Another approach is to assess the proportion of funding compared between research disciplines, or research categories, in the UK and USA, respectively. Within the UK data, we specifically examined research disciplines funded by the NIHR. From the 1st April 2011 to December 2020, the NIHR awarded over £216 million for Reproductive Health and Childbirth research, their 7th largest funding category. Mental Health, Cancer, and Cardiovascular Diseases were within the top 5 most funded categories (Supplementary Table 8). NIHR awarded £21 million in 2017/18 for Reproductive Health and Childbirth research (NIHR, 2021, yet surprisingly there was minimal support towards male-based research as between 2016 and 2019 only two projects were funded (, Supplementary Table 6). The small number of projects in male reproductive health funded by the NIHR was unexpected as NIHR is the largest UK funder for health care and clinical research (NIHR, 2021). NIHR supported 302 studies for reproductive health with 94 of them being newly funded projects for 2019/20. However, using our criteria for study inclusion we only identified 4 projects focussing on infertility over the whole period (, Supplementary Table 4). While we do not know the reason for the low funding rate, a plausible explanation is that, as NIHR fund a significant number of clinical trials, there may not have been sufficient high-quality candidates for either diagnostic and/or treatment trials to be developed in male reproductive health (Barratt et al., Citation2021).
To compare different research categories for the USA data, we did not use our collected data to provide estimated funding. Instead, we used the NIH’s Research Portfolio Online Reporting Tools estimates of funding for various Research Condition and Disease Categories (RCDC) (https://report.nih.gov/funding/categorical-spending#/) and the NIH’s annual research grants (https://report.nih.gov/funding/nih-budget-and-spending-data-past-fiscal-years/budget-and-spending). For the NIH, the values presented for the 299 RCDCs are not mutually exclusive because a project can fall under several categories. We examined research categories like those at the NIHR. For NIH these included: Contraception/Reproduction, Infertility, Obesity, and Mental Health (Supplementary Table 9). By estimating the proportion of funding for these categories from the NIH’s Total Research Funding, we can see those categories such as Obesity and Mental Health were highly funded in comparison to Contraception/Reproduction and Infertility.
NICHD has funded under 1% of their annual research grants for male-based research for 3 out of 4 consecutive fiscal years (). NICHD is the primary funder for reproduction, infertility, and contraceptive development, therefore, it was unexpected to observe such low funding proportions. A possible factor for why our calculated funding proportion values by the NICHD are low may be due to our strict eligibility criteria during data collection. However, we applied our eligibility and exclusion criteria equally across all funding agencies, for the UK and USA.
Table 6. The current total NICHD proportion of funding for infertility research.
Two pertinent points arise from our study. Firstly, compared to the prevalence of the disease where 1:7 heterosexual couples are infertile (Boivin et al., Citation2007; National Institute for Health & Clinical Excellence, Citation2013), the proportion of research funding for male reproductive health is small (less than 1%, see and ) compared to other diseases in the UK and USA (Supplementary Table 9). This is surprising especially because MAR is a multi-billion-dollar global industry. Secondly, although the number of awards for female-based research is generally higher than for the male group (ratio of ∼2:1 in the UK and 1.3:1 in the USA), the average funding awarded per project is not significantly different in either UK or USA (see ; ). Whilst there are many challenges in comparing research funding between disciplines, the present findings directly imply a significant gap between impact of disease prevalence and research funding to investigate the disease, e.g. diagnosis and treatment. This apparent gap requires further detailed analysis and should include a comprehensive assessments of the health economic impact of male reproductive health.
There are several limitations to our study. Firstly, these findings cannot be generalised to reflect funding trends towards infertility and reproductive health worldwide. The data were collected from governmental agencies of two countries and over a narrow funding period. Further, the funding priorities of UK and USA governmental agencies may not be a ‘good fit model’ for the funding priorities of government research agencies in other countries. Secondly, only government funding was investigated. We did not examine funding from non-governmental organisations (NGO’s) (e.g. Wellcome Trust, industry, Bill and Melinda Gates Foundation), and other major philanthropic organisations. As the UKRI, NIHR, and NIH are governmental agencies, their prioritisation to providing fellowships, research grants, program centre grants, and others may not be the same as other charities and international organisations. Detailed analysis of funding from these other agencies would be instructive and assist in a more comprehensive analysis. Future work should include data from more countries, NGO’s and include longer funding timeframes to accurately estimate total funding supporting for male infertility and male reproductive health and for more comprehensive assessment of funding trends.
In summary, we present recent government funding for male-based infertility and reproductive health, and by extension, funding towards female-based research. The information provided in this study will be useful for a variety of stakeholders as discussed earlier. A sentinel message is that whilst male infertility poses a global health risk for many millions of men, research funding to develop better diagnostic tools and treatment regimens is not at an appropriate level. In fact, funding for reproduction research (male and female) is substantially below what would be expected given the frequency of infertility and the impact of the diagnosis on society. There is clearly much work to be done to formulate coherent, persuasive, and effective arguments for substantial strategic investment in reproduction research. We are just starting to see the emergence of societies and groups making these cases (e.g. MRHI), https://www.eshre.eu/Specialty-groups/Special-Interest-Groups/Andrology/MRHI but we are only at the beginning. The data analysis presented herein should help shape discussions and galvanise the argument for the strategic development of male reproductive health care investment.
Supplemental Material
Download MS Word (136.6 KB)Acknowledgements
The initial concept for this work was based on discussions as part of the ESHRE MRHI Working Group. We are grateful to ESHRE for providing ground-breaking funding and for their continued support. We are grateful to Dr Stephen J. Publicover of University of Birmingham for providing critical feedback on the manuscript.
Disclosure statement
CLRB is Editor for RBMO and has received lecturing fees (2019) from Merck, Pharmasure, and Ferring. His laboratory is funded by Bill and Melinda Gates Foundation, CSO, Genus. No other authors declare a conflict of interest.
Data availability statement
The data underlying this article are available in the Dryad Digital Repository at https://doi.org/10.5061/dryad.v9s4mw6wc (Gumerova et al., Citation2021).
Additional information
Funding
References
- Barratt, C., Björndahl, L., De Jonge, C. J., Lamb, D. J., Osorio Martini, F., McLachlan, R., Oates, R. D., van der Poel, S., St John, B., Sigman, M., Sokol, R., & Tournaye, H. (2017). The diagnosis of male infertility: An analysis of the evidence to support the development of global WHO guidance-challenges and future research opportunities. Human Reproduction Update, 23(6), 660–680. https://doi.org/10.1093/humupd/dmx021
- Barratt, C., De Jonge, C. J., Anderson, R. A., Eisenberg, M. L., Garrido, N., Rautakallio Hokkanen, S., Krausz, C., Kimmins, S., O'Bryan, M. K., Pacey, A. A., Tüttelmann, F., & Veltman, J. A. (2021). A global approach to addressing the policy, research and social challenges of male reproductive health. Human Reproduction Open, 2021(1), hoab009. https://doi.org/10.1093/hropen/hoab009
- Barratt, C., De Jonge, C. J., & Sharpe, R. M. (2018). 'Man Up': The importance and strategy for placing male reproductive health centre stage in the political and research agenda. Human Reproduction, 33(4), 541–545. https://doi.org/10.1093/humrep/dey020
- Boivin, J., Bunting, L., Collins, J. A., & Nygren, K. G. (2007). International estimates of infertility prevalence and treatment-seeking: Potential need and demand for infertility medical care. Human Reproduction, 22(6), 1506–1512. https://doi.org/10.1093/humrep/dem046
- De Jonge, C., & Barratt, C. (2019). The present crisis in male reproductive health: An urgent need for a political, social, and research roadmap. Andrology, 7(6), 762–768. https://doi.org/10.1111/andr.12673
- Gumerova, E., De Jonge, C., & Barratt, C. (2021). Research funding for male reproductive health and infertility in the UK and USA [2016 – 2019]., Dataset. https://doi.org/10.5061/dryad.v9s4mw6wc
- Liao, S. J., Xu, Y. Y., Sun, R. J., & Lyu, Q. Y. (2020). National natural science foundation of China leads the comprehensive development of basic research in the field of male reproductive health in China. Asian Journal of Andrology, 22(6), 547–548. https://doi.org/10.4103/aja.aja_129_19
- National Institute for Health and Clinical Excellence. (2013). Fertility: Assessment and Treatment for People with Fertility Problems. NICE Clinical Guideline, Manchester. https://www.nice.org.uk/guidance/cg156
- NIH Report. (2021). Research Portfolio Online Reporting Tools. Budget and Spending. 2021. Available from: https://report.nih.gov/funding/nih-budget-and-spending-data-past-fiscal-years/budget-and-spending
- NIH (2021). National Institutes of Health – Institutes, Centers and Office. 2021. Available from: https://www.nih.gov/institutes-nih/list-nih-institutes-centers-offices
- NIHR. (2021). National Institute for Health Research - Reproductive Health and Childbirth. 2021; Available from: https://www.nihr.ac.uk/explore-nihr/specialties/reproductive-health.htm
- Schlegel, P. N., Sigman, M., Collura, B., De Jonge, C. J., Eisenberg, M. L., Lamb, D. J., Mulhall, J. P., Niederberger, C., Sandlow, J. I., Sokol, R. Z., Spandorfer, S. D., Tanrikut, C., Treadwell, J. R., Oristaglio, J. T., & Zini, A. (2021a). Diagnosis and treatment of infertility in men: AUA/ASRM guideline part I. Fertility and Sterility, 115(1), 54–61. https://doi.org/10.1016/j.fertnstert.2020.11.015
- Schlegel, P. N., Sigman, M., Collura, B., De Jonge, C. J., Eisenberg, M. L., Lamb, D. J., Mulhall, J. P., Niederberger, C., Sandlow, J. I., Sokol, R. Z., Spandorfer, S. D., Tanrikut, C., Treadwell, J. R., Oristaglio, J. T., & Zini, A. (2021b). Diagnosis and treatment of infertility in men: AUA/ASRM guideline part II. Fertility and Sterility, 115(1), 62–69. https://doi.org/10.1016/j.fertnstert.2020.11.016
- UKRI. (2019). UK Research and Innovation - Annual Report and Accounts 2018–2019. In Department for Business EaIS (ed), pp. 144. https://www.gov.uk/government/publications/ukri-annual-report-and-accounts-2018-to-2019
