Abstract
As the average age of first-time parents continues to rise, there has been a concerted effort by educators, policy makers and several reproductive health groups to improve fertility awareness. This study explored fertility knowledge of lay men and women and healthcare professionals (HCPs) using the same test instrument, providing a new and unique perspective compared with previous studies. Results were obtained from 1082 survey respondents: 347 HCPs, 319 men and 413 women, 105 of whom were trying to conceive (TTC). A total of 35 interviewees were purposively sampled to include 9 HCPs, 13 men and 13 women from the reproductive age range and of varying ethnic and educational backgrounds. Interview data were transcribed and analysed using the framework method. The proportion of HCPs correctly answering the survey knowledge questions was 47.1 (95% CI = 41.7%, 52.5%) compared to 44.4% for women (95% CI = 38.9%, 50.1%); 49.9% (95% CI = 39.0, 59.9%) for women TTC; and 32.5% (95% CI = 27.1%, 37.9%) for men. HCPs were ranked as the most trusted source for seeking fertility information. Overall HCPs did not demonstrate better fertility knowledge than lay participants, with inconsistencies regarding where responsibility lies for providing the right information to patients. HCPs need to improve their knowledge about fertility to help improve patient’s fertility awareness.
Introduction
Childbearing at advanced maternal and paternal age has shown a marked increase in many high-income countries over the last two decades. In the UK, fertility rates for women aged under 30 years were at the lowest level since records began (The UK Office For National Statistics, Citation2021a). This UK ONS data also show that fertility rates have decreased in all age groups except for women aged 40–44 years, in which they have more than quadrupled in the past two decades. A similar trend is observed in many high-income countries, with evidence so far showing that the COVID-19 pandemic could be an exacerbating factor (Aassve et al., Citation2021; Berrington et al., Citation2022). These trends show that individuals are progressively delaying having children. In response, there has been a concerted effort from educators, healthcare professionals (HCPs), charities, reproductive health groups and government policymakers, to improve fertility education.
Since earning potential generally tends to increase with age, delaying parenthood is a rational economic strategy, and one of the frequent reasons cited for delaying childbearing (Leung et al., Citation2016). Economic reasons such as studying, employment and career progression are not the only motivators for a delay in family building but are collectively cited as the most important reasons (Brand & Davis, Citation2011; Mills et al., Citation2011). Changing social norms about ideal age for parenthood (McQuillan et al., Citation2011), education, availability of contraception and assisted reproductive technologies are also contributing factors. Studies (Hodes-Wertz et al., Citation2013; Koert et al., Citation2021; Mac Dougall et al., Citation2013; Schytt et al., Citation2014) have shown that delayed childbearing is not necessarily a conscious choice; rather a complex interrelationship of factors including financial and emotional stability, relationship status, health and fertility status determine when or whether women start to have children. Nevertheless, in many cases, the likelihood of conception is reduced by a lack of awareness and knowledge regarding risk of infertility with advancing maternal age and delayed childbearing (Birch Petersen et al., Citation2015; Grace et al., Citation2019; Harper et al., Citation2017).
Overall, the demographic shift towards delayed family building is of increasing public health and clinical concern due to elevated risks of poor maternal and foetal outcomes (Cooke et al., Citation2012). Although most women will be able to conceive naturally if they do so by the age of 35 for those who have difficulty conceiving, poor outcomes increase rapidly (RCOG, Citation2011). Improving fertility knowledge remains an important part of public health initiatives for preventing involuntary childlessness and helping individual achieve their desired family-building intentions (García et al., Citation2016; Grace et al., Citation2022a; Virtala et al., Citation2011; Yu et al., Citation2016). Understanding reproductive cycles and fertility are essential for both pregnancy prevention and pregnancy planning. Education should enable men and women to understand how their individual fertility may decline with age, based on a combination of genetic (Stoop et al., Citation2014) and lifestyle factors (Smith, Citation2015). Rapid advances in assisted reproductive technologies highlight the emphasis placed on potential solutions rather than the root causes, which include poor knowledge about fertility.
Most studies designed to assess the level of knowledge of fertility and reproductive health have been conducted in student population groups or those visiting fertility clinics, as shown by a recent systematic review (Perez Capotosto, Citation2021). Although such settings provide good sources of closed population groups, findings are not representative of the wider lay population. This study aimed to assess fertility knowledge among different population groups; men, women and HCPs using the same test instrument, therefore, enabling direct comparisons between groups. The use of mixed qualitative and quantitative research methods provides a deeper insight into the issue; and the inclusion of men and HCPs fills an important gap in literature as there is a paucity of studies on this topic for both groups.
Materials and methods
Quantitative – survey
To assess the knowledge of the three population groups, including those actively trying to conceive (TTC), the survey test instrument was designed by authors to cover fertility and reproductive health topics including male and female reproductive biology, basic definitions, age-related fertility decline and conception. The survey questionnaire was adapted from previous studies (Lampic et al., Citation2006; Zinaman et al., Citation2019), using the UK Office for National Statistics format for demographic characteristics to compare with the general UK population. To test the survey instrument’s validity and reliability, three pilot studies were conducted, with revisions after each pilot study prior to administering the final version (Supplementary Tables) was online via the SurveyMonkey® survey software and questionnaire platform. The survey included lay men and women of reproductive age, and HCPs. Men and women were recruited nationwide via online newspapers and social media adverts with a target sample size of 300 for each of the three core groups. Not all HCPs groups contacted responded to our request for participation. HCP participants were recruited from professional bodies: Royal College of General Practitioners, Royal College of Physicians, Royal College of Nursing, Primary Care Women’s Health Forum and doctors.org.uk. Participants who signed up for the study were provided with a link containing the study information and preliminary screening questionnaire to confirm eligibility based on the inclusion and exclusion criteria. Those who met the initial screening requirements were then provided with access to the survey via a unique link and Study ID Number which was connected to the email address provided during the first stage, receiving a £10 electronic shopping voucher. Percentages and 95% confidence intervals of questions answered correctly by each group were calculated using Minitab® Statistical package. A Chi-Squared test was used to determine whether the group of a participant was related to how they responded to a question and whether there was a statistically significant difference between groups. HCPs who identified as men, women or women TTC were grouped in the HCP category during analysis. As there were multiple choice questions, the overall chance of any of the analysis being significant was adjusted by adjusting using the Bonferroni correction; dividing the significance level by the number of tests (0.05/9 = 0.0056). Therefore, for each individual test, we used a significance level of 0.0056; where p values less than 0.0056 were considered significant.
Qualitative – interviews
Survey participants who had agreed to a follow-up interview were recruited for the interviews. Criteria-based purposive sampling was used to cover the socio-demographic diversity of the population groups, including age, ethnicity and education. Research (Bowers et al., Citation2011; Guest et al., Citation2020; Saunders et al., Citation2018) indicates that a sample of 15–20 participants is sufficient for theme saturation for this kind of study. A total of 35 interviews (13 men, 13 women and 9 HCPs) were conducted remotely by one trained interviewer. Semi-structured interviews lasted 1 h on average, questions from the topic guide developed by authors covered: sources for seeking information on fertility, fertility knowledge, myths and misconceptions, issues and barriers associated with improving fertility awareness. Interviewees received a £20 electronic shopping voucher. All interviews were digitally recorded, transcribed verbatim and coded electronically using the NVIVO Pro version 11, QSR International. Analysis was conducted using thematic framework methodology (Gale et al., Citation2013), providing a structure into which the data can be systematically interrogated and analysed by case and by code. The coded framework matrix was exported from the NVIVO software into a Microsoft Excel file which was used for further examination, categorization and analysis. In summary, the data analysis process consisted of the coding of individual quotations verbatim, summarizing quotations, grouping into higher order categories (themes) and analysis within theme.
Favourable ethical approval was obtained from UCL Research Ethics committee (Reference 8421/001). All participants in this study participated voluntarily and gave informed consent.
Results
Survey
Participant demographics
The sociodemographic characteristics of study participants are summarized in .
Table 1. Sociodemographic characteristics of study participants.
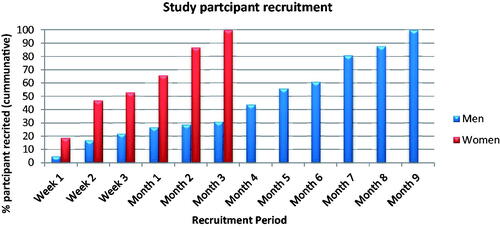
During study execution, the duration had to be extended twice due to the difficulty encountered recruiting men. Although male readership was higher, national newspaper adverts which delivered the required study sample size of women in less than a 3-month period did not yield a similar number of men in 6 months. Additional adverts in sporting sections of online newspaper adverts, targeting gyms, sporting centres and a construction centre were placed to attract more men. Recruitment of male participants took 9 months in total versus two and a half for women. Most HCPs were recruited within 2 months; however, this may be due to direct targeting of HCPs through professional bodies. highlights the duration for recruitment of study participants. The slower rate of engagement by men is very notable.
As shown in , when asked to rank the most trusted source of information, HCPs received the highest-ranked source of information. Women TTC ranked the internet more highly than other groups.
Table 2. Ranking of the most trusted sources for seeking information.
In terms of knowledge of the fertility topics raised in the survey, on average, HCPs in this study, did not demonstrate better knowledge than lay groups, apart from men. The proportion of each group correctly answering the fertility knowledge questions is summarized in .
Table 3. Percentage of lay population groups and healthcare professionals correctly answering fertility knowledge questions.
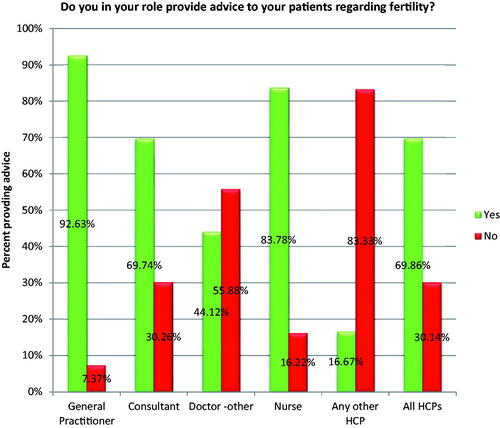
The majority of HCPs who participated in the survey provide patients with fertility advice, the proportion of each group is shown in .
As shown in , when asked, HCPs (79.9%) felt that it was the responsibility of HCPs to ensure that men and women obtain accurate and reliable fertility information.
Table 4. Responsibility for accurate and reliable fertility information (HCPs).
Qualitative themes
In this section, we discuss the key themes from the interviews.
Trust in healthcare professionals and responsibility for providing information
Similar to the survey findings, during interviews, participants reiterated that HCPs were the most trusted on fertility issues:
I trust the healthcare professional most. And I think it’s the same for my husband. We were talking about moving off of contraception and moving in to wanting to have a baby which is why he felt we should go to the doctors at that point. You just can’t trust the internet with these things., FP2 – Female, Age 32
Some HCPs expressed concerns regarding information provided by other professionals and a lack of trust in the information provided. There were inconsistencies among HCPs regarding where responsibility lies for providing the right information on fertility awareness:
GPs are the ones who see women the most but I guess Family Planning Clinics, discussing this kind of thing at pill checks, and people who are having coils put in. That would probably be the most appropriate time when, as part of general reproductive health, fertility issues should probably be discussed… when they come into contact with their GP, where for blood pressure check, to have more oral contraceptive or, you know, dealing with family planning. HCP1 – Doctor, Female, Age 33
There were suggestions that the responsibility ought to lie with clinicians delivering the service whilst others suggested primary care practitioners. Others suggested a more collaborative environment:
The primary care practitioners would probably need some guidance and support from us [consultants] but I think they do have a very big role which probably they don’t utilise enough. HCP7 – Consultant, Male, Age 57
Many suggestions were made regarding improving education, sharing responsibilities, and addressing the problem at the preventive stage:
Rather than spending lots of money afterwards, fixing the problem. HCP9 – Consultant, Female, Age 55
Knowledge gaps
There were several knowledge gaps amongst HCPs interviewed, some were aware of their own poor knowledge, but many were not:
A lot of myths are out there both among professionals as well as lay people. Even though I was working as a professional I wouldn’t have said I was particularly an expert and necessarily knew more than the lay people … plus practices change all the time so you know contraceptive advice, maybe a new type of pill comes in and so knowledge and research is moving on all the time. I think there is a lot of ignorance. HCP3 – General Practitioner, Female, Age 45
Concerns regarding access to HCPs and some reluctance to seek advice
Patients’ concerns regarding HCPs were mainly about accessibility, with many reporting waiting times as a key barrier. Some stated that trying to find an appointment can be stressful when working, and/or that they did not feel the subject (their fertility) was important enough to make an appointment with a HCP. Others, especially men in our study, reported reluctance to speak to their doctor on the topic due to embarrassment or simply a general reluctance around seeing a doctor:
I'm still the kind of person where I won’t go to the doctor unless I'm dying. MP11 – Male, Age 36
Training for HCPs
General practitioners concurred that they had poor education and training in this area, recommending additional information on fertility and reproductive health should be included as part of general HCP training:
Currently I undergo clinical training, and I feel that there is a lack of information regarding fertility etc. within my field. We do touch upon it, on our course, but I think that with the current climate it’s such a significant part of people’s lives. I don’t think there’s enough emphasis on training clinical staff when it comes to fertility, obviously dealing with their patients and their choices regarding it. HCP8 – General Practitioner, Female, Age 36
Discussion
Overall, the study participants showed poor fertility knowledge with men, on average, scoring lower than women and HCPs in the survey, but women TTC scored higher than all other groups. These results are consistent with findings of other fertility awareness studies (Hammarberg et al., Citation2017; Lampic et al., Citation2006; Rovei et al., Citation2010), where men have shown poorer knowledge of fertility and reproductive health than women. Women TTC correctly answered knowledge questions on the definition of ovulation menstrual cycle and menstrual cycle length. However, questions on conceiving were poorly answered. Studies (Boivin et al., Citation2011; Greil et al., Citation2011; Peterson, Citation2017; Schardt, Citation2005) have shown that infertility can be a significant source of emotional and psychological distress in individuals, therefore it is very important to improve knowledge and awareness in this population group and provide relevant support. Knowledge of male and female age-related fertility decline was poor across all study population groups with statistically significant differences between groups. Less than 26% of each of the population groups correctly identified a response in line with current literature on fertility decline. Interestingly, the most frequently selected option for male fertility decline was ‘it never declines’. This is contrary to literature evidence on age-related fertility decline in men (Eisenberg & Meldrum, Citation2017; Harris et al., Citation2011; Phillips et al., Citation2019; Urhoj et al., Citation2017).
Although HCPs were cited as the most trusted and used sources by all population groups, they did not demonstrate higher knowledge than lay population groups in this study and their role did appear to affect knowledge. Poor fertility knowledge among HCPs has been demonstrated by other studies (García et al., Citation2017; Kadmon et al., Citation2014). Additionally, being in a role that requires advising patients did not appear to improve knowledge. The majority, 92.6% of GPs, 83.7% of nurses and 69.7% of consultants in this study advise patients in this area. When asked to select where responsibility lies for providing accurate information on fertility awareness, most HCPs (79.9%) selected ‘HCPs’ (that is other HCPs). Evidence from the follow-up interviews showed that there were inconsistencies regarding where responsibility lies for providing the right information and support. Suggestions ranged from primary to secondary care to government policies, further highlighting a lack of clarity on where responsibility lies. Our findings are consistent with a previous study on HCPs’ knowledge, attitudes, and views of providing fertility and preconception care, where there was poor knowledge and no clear consensus on who takes the responsibility for providing preconception care and advice (Ojukwu et al., Citation2016).
In addition to websites based on robust scientific evidence and centres specializing in sexual education, there remains an important need for additional training for HCPs on reproductive health as they are key sources of information. HCPs in our study emphasized the importance of preventive measures, such as improving fertility awareness, instead of spending funds on trying to address the impact of preventable infertility. They also cited concerns around tailoring information to the right patient and prioritizing issues related to fertility because UK GP appointments are in very high demand. Some expressed concerns regarding tailoring information to suit varied patient types; methods of introducing the topic to patients; limited time to discuss issues with patients; and variations due to practices and services. Other concerns covered the timing of the discussions and how to broach the topic with a patient, if not initiated. For issues like these, we recommend a lifecourse approach such as The Reproductive Life Plan (RLP) strategy as a useful tool to implement across the UK. The RLP has been advocated by many reproductive healthcare organizations and interest groups (American College of Obstetricians and Gynecologists’ Committee on Health Care for Underserved Women, Citation2016; Malnory & Johnson, Citation2011; Stern et al., Citation2013; Tydén et al., Citation2016) in order to help individuals achieve their desired fertility intentions (Grace et al., Citation2022b).
While we emphasize the importance of good fertility knowledge to help individuals achieve their desired fertility intentions, it is crucial to highlight the impact of wider determinants in family building decision making. A study on women who became pregnant after the age of 40 (Mac Dougall et al., Citation2013) showed that nearly half of those who had undergone in vitro fertilization admitted that, even if they had the appropriate knowledge prior to their years of peak fertility, their circumstances at the time would not have permitted a pregnancy. Another study (Cooke et al., Citation2012) suggested limited choice regarding when to start a family. Similarly, other studies (Bodin et al., Citation2021; Hviid Malling et al., Citation2022), reveal that although individuals may have reached a juncture in their lives when they felt they should start a family, factors such as financial stability, relationship and health affect decision making. Highlighting the importance of health policies taking wider determinants, as a key part of fertility awareness campaigns.
In terms of study strengths and limitations, to our knowledge, this is the first fertility awareness study to include men, women, women TTC and HCPs, therefore, enabling direct comparisons between groups. Most of the studies exploring psychosocial aspects of infertility have focussed on those seeking fertility treatment, leaving a research gap in the general population. The inclusion of men and HCPs in this study fills an important gap in literature as there is a paucity of studies for both groups, providing an opportunity for inclusive innovative practices. The study included a spread of socioeconomic demographic and HCP groups. Different categories of HCPs were also represented. Another key strength of this study is the mixed methods approach for assessing fertility knowledge. Most fertility awareness studies in the literature are quantitative and survey based. Using mixed methods, we obtained deeper insights and better understanding regarding the fertility knowledge. Compared to the general UK population (The UK Office for National Statistics, Citation2021b), black and minority ethnic groups whose views are underrepresented in fertility awareness studies, were overrepresented in this study.
One of the main limitations of the study is that, as with all surveys, participants and interviewees were self-selected, which has implications for generalizability. Additionally, the online recruitment method and the potential bias towards more educated respondents, was evident from the demographic data, where over two thirds of the study population had achieved a degree or post graduate qualification. Nevertheless, this did not appear to result in overall good fertility knowledge. Since the recruitment of lay men took longer than the other groups, additional effort was made to recruit men from specific sources, this may have an impact on when comparing and women’ knowledge. While in principle, the findings may be applicable in similar contexts, the generalizability of the UK population would need to be considered.
In conclusion, HCPs, especially primary care providers play a key role in improving fertility awareness and are often cited as the most trusted source of obtaining fertility formation but do not necessarily have better knowledge than the general population. Although school education is potentially an important, widespread source of health information, it does not adequately cover fertility education. There remains an important need for additional training for HCPs on fertility and reproductive health to facilitate promotion of fertility awareness. In terms of wider implications, improvements through a more holistic life course approach to reproductive health, including family building, should be a key component of public health programmes. This requires collaborative initiatives supported by several stakeholders including, policy makers; HCPs, educators and other special interest groups in order to help individuals achieve their desired family-building outcomes.
Supplemental Material
Download MS Word (58.9 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Aassve, A., Cavalli, N., Mencarini, L., Plach, S., & Sanders, S. (2021). Early assessment of the relationship between the COVID-19 pandemic and births in highincome countries. Proceedings of the National Academy of Sciences, 118(36), e2105709118. https://doi.org/10.1073/pnas.2105709118
- American College of Obstetricians and Gynecologists’ Committee on Health Care for Underserved Women. (2016). Committee opinion No. 654: Reproductive life planning to reduce unintended pregnancy. Obstetrics and Gynecology, 127(2), e66–e69. https://doi.org/10.1097/AOG.0000000000001314
- Berrington, A., Ellison, J., Kuang, B., Vasireddy, S., & Kulu, H. (2022). Scenario-based fertility projections incorporating impacts of COVID-19. Population, Space and Place, 28(2), e2546. https://doi.org/10.1002/psp.2546
- Birch Petersen, K., Hvidman, H. W., Sylvest, R., Pinborg, A., Larsen, E. C., Macklon, K. T., Andersen, A. N., & Schmidt, L. (2015). Family intentions and personal considerations on postponing childbearing in childless cohabiting and single women aged 35-43 seeking fertility assessment and counselling. Human Reproduction (Oxford, England), 30(11), 2563–2574. https://doi.org/10.1093/humrep/dev237
- Bodin, M., Holmström, C., Plantin, L., Schmidt, L., Ziebe, S., & Elmerstig, E. (2021). Preconditions to parenthood: Changes over time and generations. Reproductive Biomedicine & Society Online, 13, 14–23. https://doi.org/10.1016/j.rbms.2021.03.003
- Boivin, J., Griffiths, E., & Venetis, C. A. (2011). Emotional distress in infertile women and failure of assisted reproductive technologies: Meta-analysis of prospective psychosocial studies. BMJ, 342, d223. https://doi.org/10.1136/bmj.d223
- Bowers, D., House, A., & Owens, D. (2011). Chapter 8. Selecting samples for qualitative research. Getting Started in Health Research, 56–60. https://doi.org/10.1002/9781444341300.CH8
- Brand, J. E., & Davis, D. (2011). The impact of college education on fertility: Evidence for heterogeneous effects. Demography, 48(3), 863–887. https://doi.org/10.1007/s13524-011-0034-3
- Cooke, A., Mills, T. A., & Lavender, T. (2012). Advanced maternal age: Delayed childbearing is rarely a conscious choice a qualitative study of women’s views and experiences. International Journal of Nursing Studies, 49(1), 30–39. https://doi.org/10.1016/j.ijnurstu.2011.07.013
- Eisenberg, M. L., & Meldrum, D. (2017). Effects of age on fertility and sexual function. Fertility and Sterility, 107(2), 301–304. https://doi.org/10.1016/j.fertnstert.2016.12.018
- Gale, N. K., Heath, G., Cameron, E., Rashid, S., & Redwood, S. (2013). Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Medical Research Methodology, 13, 117. https://doi.org/10.1186/1471-2288-13-117
- García, D., Vassena, R., Prat, A., & Vernaeve, V. (2016). Increasing fertility knowledge and awareness by tailored education: A randomized controlled trial. Reproductive Biomedicine Online, 32(1), 113–120. https://doi.org/10.1016/j.rbmo.2015.10.008
- García, D., Vassena, R., Prat, A., & Vernaeve, V. (2017). Poor knowledge of age-related fertility decline and assisted reproduction among healthcare professionals. Reproductive Biomedicine Online, 34(1), 32–37. https://doi.org/10.1016/j.rbmo.2016.09.013
- Grace, B., Shawe, J., Johnson, S., & Stephenson, J. (2019). You did not turn up… I did not realise I was invited…: Understanding male attitudes towards engagement in fertility and reproductive health discussions. Human Reproduction Open, 2019(3), hoz014. https://doi.org/10.1093/hropen/hoz014
- Grace, B., Shawe, J., Barrett, G., Usman, N. O., & Stephenson, J. (2022a). What does family building mean? A qualitative exploration and a new definition: A UK-based study. Reproductive Health, 19(1), 1–9. https://doi.org/10.1186/s12978-022-01511-w
- Grace, B., Shawe, J., Johnson, S., Usman, N. O., & Stephenson, J. (2022b). The ABC of reproductive intentions: A mixed-methods study exploring the spectrum of attitudes towards family building. Human Reproduction (Oxford, England), 37(5), 988–996. https://doi.org/10.1093/humrep/deac036
- Greil, A. L., Shreffler, K. M., Schmidt, L., & McQuillan, J. (2011). Variation in distress among women with infertility: Evidence from a population-based sample. Human Reproduction (Oxford, England), 26(8), 2101–2112. https://doi.org/10.1093/humrep/der148
- Guest, G., Namey, E., & Chen, M. (2020). A simple method to assess and report thematic saturation in qualitative research. PLoS One, 15(5), e0232076. https://doi.org/10.1371/journal.pone.0232076
- Hammarberg, K., Collins, V., Holden, C., Young, K., & McLachlan, R. (2017). Men’s knowledge, attitudes and behaviours relating to fertility. Human Reproduction Update, 23(4), 458–480. https://doi.org/10.1093/humupd/dmx005
- Harper, J., Boivin, J., O’Neill, H. C., Brian, K., Dhingra, J., Dugdale, G., Edwards, G., Emmerson, L., Grace, B., Hadley, A., Hamzic, L., Heathcote, J., Hepburn, J., Hoggart, L., Kisby, F., Mann, S., Norcross, S., Regan, L., Seenan, S., … Balen, A. (2017). The need to improve fertility awareness. Reproductive Biomedicine & Society Online, 4, 18–20. https://doi.org/10.1016/j.rbms.2017.03.0022
- Harris, I. D., Fronczak, C., Roth, L., & Meacham, R. B. (2011). Fertility and the aging male. Reviews in Urology, 13(4), e184–e190.
- Hodes-Wertz, B., Druckenmiller, S., Smith, M., & Noyes, N. (2013). What do reproductive-age women who undergo oocyte cryopreservation think about the process as a means to preserve fertility? Fertility and Sterility, 100(5), 1343–1349.e2. https://doi.org/10.1016/j.fertnstert.2013.07.201
- Hviid Malling, G. M., Pitsillos, T., Tydén, T., Hammarberg, K., Ziebe, S., Friberg, B., & Schmidt, L. (2022). Doing it in the right order’: Childless men’s intentions regarding family formation. Human Fertility, 25(1), 188–196. https://doi.org/10.1080/14647273.2020.1778803
- Kadmon, I., Goldin, Y., Bdolah, Y., Farhat, M., & Liebergall-Wischnitzer, M. (2014). Knowledge, attitudes and practices of physicians and nurses regarding the link between IVF treatments and breast cancer. European Journal of Oncology Nursing: The Official Journal of European Oncology Nursing Society, 18(2), 201–205. https://doi.org/10.1016/j.ejon.2013.10.009
- Koert, E., Sylvest, R., Vittrup, I., Hvidman, H. W., Petersen, K. B., Boivin, J., Nyboe Andersen, A., & Schmidt, L. (2021). The importance of the ‘family clock’: Women’s lived experience of fertility decision-making 6 years after attending the Fertility Assessment and Counselling Clinic. Human Fertility, 1–13. https://doi.org/10.1080/14647273.2021.1950851
- Lampic, C., Svanberg, a S., Karlström, P., & Tydén, T. (2006). Fertility awareness, intentions concerning childbearing, and attitudes towards parenthood among female and male academics. Human Reproduction (Oxford, England), 21(2), 558–564. https://doi.org/10.1093/humrep/dei367
- Leung, M. Y. M., Groes, F., & Santaeulalia-Llopis, R. (2016). The relationship between age at first birth and mother’s lifetime earnings: Evidence from Danish data. PLoS One, 11(1), e0146989. https://doi.org/10.1371/journal.pone.0146989
- Mac Dougall, K., Beyene, Y., & Nachtigall, R. D. (2013). Age shock: Misperceptions of the impact of age on fertility before and after IVF in women who conceived after age 40. Human Reproduction (Oxford, England), 28(2), 350–356. https://doi.org/10.1093/humrep/des409
- Malnory, M. E., & Johnson, T. S. (2011). The reproductive life plan as a strategy to decrease poor birth outcomes. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 40(1), 109–121. https://doi.org/10.1111/j.1552-6909.2010.01203.x
- McQuillan, J., Greil, A. L., & Shreffler, K. M. (2011). Pregnancy intentions among women who do not try: Focusing on women who are okay either way. Maternal and Child Health Journal, 15(2), 178–187. https://doi.org/10.1007/s10995-010-0604-9
- Mills, M., Rindfuss, R. R., McDonald, P., & Te Velde, E, ESHRE Reproduction and Society Task Force (2011). Why do people postpone parenthood? Reasons and social policy incentives. Human Reproduction Update, 17(6), 848–860. https://doi.org/10.1093/humupd/dmr026
- Ojukwu, O., Patel, D., Stephenson, J., Howden, B., & Shawe, J. (2016). General practitioners’ knowledge, attitudes and views of providing preconception care: A qualitative investigation. Upsala Journal of Medical Sciences, 121(4), 256–263. https://doi.org/10.1080/03009734.2016.1215853
- Perez Capotosto, M. (2021). An integrative review of fertility knowledge and fertility-awareness practices among women trying to conceive. Nursing for Women’s Health, 25(3), 198–206. https://doi.org/10.1016/J.NWH.2021.04.001
- Peterson, B. (2017). A validated measure for fertility awareness: An essential step toward informed reproductive decision-making. Fertility and Sterility, 108(4), 606–607. https://doi.org/10.1016/j.fertnstert.2017.08.027
- Phillips, N., Taylor, L., & Bachmann, G. (2019). Maternal, infant and childhood risks associated with advanced paternal age: The need for comprehensive counseling for men. Maturitas, 125, 81–84. https://doi.org/10.1016/j.maturitas.2019.03.020
- RCOG. (2011). Reproductive ageing. Scientific Impact Paper, 24, 1–6. https://www.rcog.org.uk/guidance/browse-all-guidance/scientific-impact-papers/reproductive-ageing-scientific-impact-paper-no-24
- Rovei, V., Gennarelli, G., Lantieri, T., Casano, S., Revelli, A., & Massobrio, M. (2010). Family planning, fertility awareness and knowledge about Italian legislation on assisted reproduction among Italian academic students. Reproductive Biomedicine Online, 20(7), 873–879. https://doi.org/10.1016/j.rbmo.2010.03.024
- Saunders, B., Sim, J., Kingstone, T., Baker, S., Waterfield, J., Bartlam, B., Burroughs, H., & Jinks, C. (2018). Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality & Quantity, 52(4), 1893–1907. https://doi.org/10.1007/s11135-017-0574-8
- Schardt, D. (2005). Delayed childbearing: Underestimated psychological implications. International Journal of Childbirth Education, 20(3), 34–37.
- Schytt, E., Nilsen, a B. V., & Bernhardt, E. (2014). Still childless at the age of 28 to 40 years: A cross-sectional study of Swedish women’s and men’s reproductive intentions. Sexual & Reproductive Healthcare: Official Journal of the Swedish Association of Midwives, 5(1), 23–29. https://doi.org/10.1016/j.srhc.2013.11.001
- Smith, K. R. (2015). Paternal age bioethics. Journal of Medical Ethics, 41(9), 775–779. https://doi.org/10.1136/medethics-2014-102405
- Stern, J., Larsson, M., Kristiansson, P., & Tydén, T. (2013). Introducing reproductive life plan-based information in contraceptive counselling: An RCT. Human Reproduction (Oxford, England), 28(9), 2450–2461. https://doi.org/10.1093/humrep/det279
- Stoop, D., Cobo, A., & Silber, S. (2014). Fertility preservation for age-related fertility decline. Lancet (London, England), 384(9950), 1311–1319. https://doi.org/10.1016/S0140-6736(14)61261-7
- The UK Office For National Statistics. (2021a). Births in England and Wales: 2020. Births in England and Wales: 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/bulletins/birthsummarytablesenglandandwales/2019
- The UK Office for National Statistics. (2021b). Overview of the UK population - office for National Statistics. Overview of the UK Population. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/articles/overviewoftheukpopulation/january2021
- Tydén, T., Verbiest, S., Van Achterberg, T., Larsson, M., & Stern, J. (2016). Using the reproductive life plan in contraceptive counselling. Upsala Journal of Medical Sciences, 121(4), 299–303. https://doi.org/10.1080/03009734.2016.1210267
- Urhoj, S. K., Andersen, P. K., Mortensen, L. H., Davey Smith, G., & Nybo Andersen, A.-M. (2017). Advanced paternal age and stillbirth rate: A nationwide register-based cohort study of 944,031 pregnancies in Denmark. European Journal of Epidemiology, 32(3), 227–234. https://doi.org/10.1007/s10654-017-0237-z
- Virtala, A., Vilska, S., Huttunen, T., & Kunttu, K. (2011). Childbearing, the desire to have children, and awareness about the impact of age on female fertility among Finnish university students. The European Journal of Contraception & Reproductive Health Care: The Official Journal of the European Society of Contraception, 16(2), 108–115. https://doi.org/10.3109/13625187.2011.5532955
- Yu, L., Peterson, B., Inhorn, M. C., Boehm, J. K., & Patrizio, P. (2016). Knowledge, attitudes, and intentions toward fertility awareness and oocyte cryopreservation among obstetrics and gynecology resident physicians. Human Reproduction (Oxford, England), 31(2), 403–411. https://doi.org/10.1093/humrep/dev308
- Zinaman, M. J., Johnson, S., Foster, L., Zanzi, G., & Mollard, C. (2019). Fertility knowledge of women in the United States [6M]. Obstetrics & Gynecology, 133(1), 141S–141S. https://doi.org/10.1097/01.AOG/01.AOG.0000559279.68081.a5