Abstract
We sought to find out if information about public funding for regulated donor insemination (DI) was available on UK fertility clinic websites, and if so, what information was provided for same-sex couples and single women; and if the available information was easily readable. The ‘Choose a fertility clinic’ pages of the Human Fertilisation and Embryology Authority (HFEA) website were used to identify all licensed fertility clinics in the UK, and any available text on public funding for DI treatment was extracted. The Flesch reading ease scores were calculated to determine the readability of the extracted text. Of the 52 clinics included in the synthesis, 23 mentioned public funding, and for 16 of these, it was unclear whether public funding was available. Six of the 23 clinics mentioned public funding for same-sex couples, and two mentioned public funding for single women. The Flesch reading ease scores indicated that none of the text about funding for DI treatment on any of the clinic websites met the NHS-advised level of readability for health information. Fertility clinic websites should specify whether they offer publicly funded treatment, and to whom, as well as clearly stating the eligibility criteria, using suitably readable language to communicate this.
Introduction
Internet usage has grown rapidly in the last few decades, with ever increasing numbers of people going online to seek health information (Couper et al., Citation2010). In response to this increase, healthcare providers have adapted to ensure they provide health information online, and the National Health Service (NHS) website is now central to the health information landscape of the United Kingdom (Gann & Grant, Citation2013). Online health information can serve to empower, educate, and reassure those who seek it, as well as having a significant impact on healthcare decisions and outcomes (Sbaffi & Rowley, Citation2017). Given the relative privacy afforded by the Internet, there is also evidence to suggest that online health information is commonly sought by those who suffer from stigmatised conditions such as infertility, or matters considered ‘private’, such as trying to become pregnant (Kedzior et al., Citation2019; Morahan-Martin, Citation2004). A recent report on the compliance of UK fertility clinics with consumer law, undertaken by the Competition and Marketing Authority (CMA), highlighted ‘the importance of clinics providing clear and transparent information’ to patients, especially on their websites, ‘where the vast majority of patients look when they are comparing, shortlisting and ultimately choosing a clinic’ (Competition & Markets Authority, 2022, p. 5). It is therefore vital that information on fertility treatment, including sources of funding, is easily accessible and comprehensible online, as it is often the starting point for people who are investigating their fertility options (Competition & Markets Authority, Citation2022; Tonsaker et al., Citation2014).
In 2022, the HFEA licensed 104 fertility clinics, and of these, 62 (60%) were privately owned (Human Fertilisation and Embryology Authority, Citation2022). Importantly, however, most HFEA licensed clinics, whether privately-owned, or state-owned, treat both NHS and privately funded patients, and the NHS is known to have contracts with private fertility clinics (Competition & Markets Authority, Citation2022). Nevertheless, nearly three-quarters of all self-funded IVF cycles take place in private clinics (Competition and Markets Authority, Citation2022). It is important to note that Clinical Commissioning Groups (CCGs), which are the NHS bodies responsible for the planning and commissioning of healthcare services for the local area, only exist in England, with other countries in the UK being governed in a similar way by Health Boards (Wales and Scotland), and Local Commissioning Groups (LCGs; Northern Ireland). CCGs in England have now been superseded by Integrated Care Boards (ICBs), but the criteria we refer to in this article were previously developed by CCGs and have been carried over by ICBs (Tippett, Citation2023).
In 2017, the European Policy Audit on Fertility (EPAF) reported that ongoing pressures on the NHS budget were likely to make access to funded fertility treatment even more difficult in coming years (Fertility Europe and European Society for Human Reproduction and Embryology (ESHRE), Citation2017). This has certainly been the case, and much negative attention has been given to the so-called ‘postcode lottery’ of fertility treatment by the British press, campaign groups, and National Institute for Health and Care Excellence (NICE) itself (British Pregnancy Advisory Service, Citation2020; Fertility Fairness, Citation2017; National Institute for Health and Care Excellence, Citation2014; Richardson, Citation2018; Tippett, Citation2023). While disparate funding for assisted conception (including DI) is most certainly a cause for concern, issues of funding accessibility are further exacerbated for marginalised groups, such as same-sex couples and single women, who do not ascribe to the ‘traditional’ (i.e. mixed-sex) family structures which continue to dominate regulated fertility settings (Culley et al., Citation2013; Mamo, Citation2007; Taylor et al., Citation2022; Tippett, Citation2023). However, recent HFEA figures show that same-sex female couples and single women are increasingly using regulated fertility services, and DI in particular (Human Fertilisation and Embryology Authority, Citation2022).
In June 2021, the British Pregnancy Advisory Service (BPAS) published a report which found that female same-sex couples face significant barriers when attempting to access NHS-funded fertility treatment in England and Northern Ireland. Prior to this, reporting on figures from 2017, the HFEA noted that eligibility criteria for DI ‘can mean people do not get treatment for DI under the NHS…’ which ‘particularly impacts patients in female same-sex relationships or with no partner, who do not necessarily have an infertility diagnosis, and more significantly, are unable to try to conceive naturally with their partner’ (British Pregnancy Advisory Service, Citation2021; Human Fertilisation and Embryology Authority, Citation2019). Indeed, the figures support this, with only 8% of DI treatments for single women and women in same-sex relationships being publicly funded from 2016–2020 (Human Fertilisation and Embryology Authority, Citation2022).
Given the increasing use of online health information-seeking, there is a need for clear, specific, and up-to-date information on NHS funding for all those requiring fertility treatment, and particularly for people who face the additional social stigma of infertility, childlessness and/or being part of an alternative family structure. These groups are more likely to have had negative experiences of face-to-face healthcare and consequently, may prefer to seek their health information online initially (Hinton et al., Citation2012; Jabson et al., Citation2017; Meads et al., Citation2019). We sought to replicate the initial process that patients might go through when searching for information on NHS funding for regulated DI treatment, seeking to establish whether the lack of access to NHS-funded treatment was further compounded by a lack of accessible and readable information online. To respond to this aim, the present study posed the following research questions: (i) Is information about public funding for regulated DI available on UK fertility clinic websites? If so, (ii) What information is provided for same-sex couples and single women?; and (iii) Is the available information easily readable?
Materials and methods
The HFEA is the UK’s independent regulator of fertility treatment, purporting to provide ‘free, clear and impartial information on UK fertility clinics, IVF and other types of fertility treatment, and donation’ and, as part of this, it provides a directory of all UK fertility clinics (Human Fertilisation and Embryology Authority, Citation2021). We adopted the same sampling strategy as van de Wiel et al. (Citation2020) in their study on the prevalence, promotion and pricing of IVF add-ons, using the ‘Choose a fertility clinic’ pages of the HFEA website to identify all licensed fertility clinics in the UK on 28th July 2021. Each of the ‘Clinic search’ webpages were examined alphabetically, and links provided to the clinic websites were followed. We excluded any ‘satellite clinics’ which shared the same website as the main clinic, and cryobanks which did not provide fertility treatment. Once the clinic websites were accessed, they were examined for any information provided on NHS funding for DI treatment. A record was made if there was or was not information on NHS funding for DI treatment, and if there was, that text was recorded, along with who was stated as eligible for funding (i.e. mixed-sex couples, same-sex couples, single women) and the URL to the corresponding webpage.
The Flesch Reading Ease Score (FRES) is the most commonly used and well-regarded method for providing reliable and reproducible scores on readability and is used as an objective measure of the readability of online health information (Pook et al., Citation2022). As most adults in the UK have a reading ability at or below Level 1, which is what is expected of the average 11–14-year-old, the NHS health literacy guide advises that in order to be accessible, written material should be aimed at the average 11-year-old (National Health Service, Health Education England, Citationn.d). In order to determine the readability of the text extracted from the clinic websites, we calculated the FRES using Microsoft Word’s Readability Statistics. To produce a readability score, the FRES considers the average number of words per sentence and average syllables per word and is calculated as: 206.835–1.015 × (average sentence length)–84.6 × (average syllables per word). In interpreting scores (scores can range from 0 to 100), the higher the score, the easier it is to read (e.g. a score >90 indicates that the text would easily be understood by an average 11-year-old and would be considered ‘very easy to read’). See for details of how to interpret the scores. In line with the NHS advice then, to be very easily read by most users, written health information should have a FRES of approximately ≥90.
Table 1. Flesch Reading Ease Score (FRES) categorisation.
Results
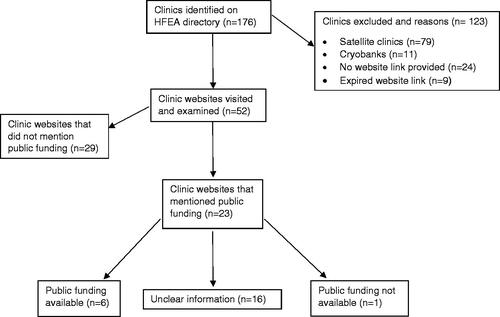
A total of 175 clinics were listed in the ‘Choose a clinic’ directory. Out of these, 79 were excluded because they were satellite clinics, and 11 were excluded because they were cryobanks. A total of 24 clinics listed in the directory had no available link to a website, and nine of the links provided had expired. This resulted in a total of 123 clinics listed in the directory being excluded. We visited the websites of the remaining 52 clinics, and of these, 23 (44%) mentioned NHS funding for fertility treatment. Please see Supplementary Appendix A for a list of the 23 clinics included in the synthesis. Of these 23 clinics, six (26.1%) stated that NHS funding was available, one (4.3%) stated that it wasn’t, and 16 (69.6%) mentioned NHS/public funding but provided unclear information about whether treatment at their clinic would be publicly funded or not. All the 23 clinics included provided treatment to both NHS and self-funded patients and the majority of these appeared to be private clinics with NHS contracts. presents the process of searching for and selecting the clinic websites. A list of the names, countries, and URLs of the 23 included clinics is available in Supplementary Appendix A. Just six out of the 23 clinics (26.1%) made specific reference to funding for female same-sex couples, and just two (8.7%) referenced funding for single women. None of the included clinics provided information on funding for male same-sex couples.
The level and detail of NHS funding information on the 23 websites ranged from a webpage containing five weblinks to relevant Clinical Commissioning Group (CCG) criteria (Fertility Exeter, England), to entire digital booklets detailing the criteria for treatment, expected timescales, treatment definitions and more (Leicester Fertility Centre, England). The most common level of information was one webpage. Six of the clinic websites encouraged would-be patients to check their local CCG criteria for treatment. One clinic website included a statement that the information provided on CCG criteria was ‘subject to change’ (The Hewitt Fertility Centre, England), and two websites provided links to more information on the local CCG criteria (Chelsea and Westminster Hospital, England; Fertility Exeter, England). Only one clinic website explained what a CCG actually was (Manchester Fertility, England). None of the clinic websites mentioned when the information provided was last updated, or when it was due to be reviewed for accuracy.
Of the six websites that mentioned funding for same-sex couples, five of these directly cited or paraphrased the NICE guidelines/Scottish Medicines Consortium (SMC) advice for fertility treatment for same-sex couples. Two websites mentioned that in same-sex couples where one of the partners has a diagnosis of infertility, there should be a discussion as to whether the other partner could try to conceive, prior to embarking on interventions involving the infertile partner (Bristol Centre for Reproductive Medicine, England; Complete Fertility Centre Southampton, England). One website stated that ‘same sex couples will not be eligible if they already have a child in the home and both have consented to legal parenthood of that child’ (Aberdeen Fertility Centre, Scotland).
The two websites that mentioned funding for single women provided just one sentence each, stating that single women ‘must have never had a biological or adopted child’ (Hewitt Fertility Centre, England), and ‘may not meet the definition of infertility and therefore may be excluded from funded treatment’ (Leicester Fertility Centre, England).
The Flesch reading ease scores for the extracted text ranged from 14.4 to 62.0, indicating that the text about NHS funding for treatment was ‘very difficult’ (n = 2), ‘difficult’ (n = 12), ‘fairly difficult’ to read (n = 7), or ‘easily understood by 13- to 15-year-olds’ (n = 2). The average score for the extracted text from the clinic webpages was 46.3, which is ‘difficult’ to read and requires the equivalent reading age of a college graduate. None of the extracted text was ‘fairly easy to read’ or better, according to the FRES.
Discussion
This study provides evidence that online health information about public funding and criteria for DI treatment is not readily available on the websites of fertility clinics in the UK. Moreover, where it is mentioned, the information is not easily readable, as measured by the FRES. There is a distinct lack of studies which have investigated the availability and readability of information on public funding for treatment, but the readability scores of the information included in this study reflect a worrying trend of online health information more generally. Previous studies undertaken in the UK found similarly low reading ease scores for online health information in reproductive medicine (Merrick et al., Citation2012) and other areas of medicine (Dobbs et al., Citation2017; Oliffe et al., Citation2019; Pook et al., Citation2022). This trend continues further afield, with studies in the USA, Canada and Australia reporting online health information from a variety of sources as ranging from ‘difficult’ to ‘very difficult’ to read (Cheng & Dunn, Citation2015; Daraz et al., Citation2018).
There are discrepancies in the information provided with regards to what and who is publicly funded across the clinic websites. These discrepancies are likely because ICBs, LCGs and Health Boards decide locally what services to fund, as well as the criteria that people must meet to be eligible for treatment. This information is regularly updated by these Groups and Boards, and it may therefore be difficult for clinics to keep track of any changes that are made (NHS Confederation, Citation2022). Consistent communication between clinics and their local ICB, LCG or Health Board is therefore integral to ensuring all information on funding and criteria for treatment is up to date.
Information on funding for same-sex couples and single women may be missing for several reasons. The lack of information on DI treatment is to be expected, given that it is less effective, and subsequently less common, than IVF (Human Fertilisation and Embryology Authority, Citation2022; Spencer et al., Citation2016). It is important to note, however, that effectiveness of any given fertility treatment depends on the individual/couple, and whether or not they have diagnosed infertility. Same-sex female couples and single women may not have diagnosed infertility but are unable to conceive without sperm. In this case, IVF may be unnecessary, and DI may be deemed the best treatment option.
Clinics can decide for themselves what services to provide based on: effectiveness, demand, and the cost of the treatments (i.e. whether it is cost effective for them to offer DI when it is not commonly used) (Spencer et al., Citation2016). The HFEA’s ‘Family formations in fertility treatment 2018’ report found that most patients opting for fertility treatment were mixed-sex couples (90%), followed by female same-sex couples (6.4%) and single women (3.2%) (Human Fertilisation and Embryology Authority, Citation2020). The report also found that single women and those in female same-sex relationships used IVF in 57% and 45% of their treatments respectively in 2018, while the remaining 43% and 55% of treatments were DI (Human Fertilisation and Embryology Authority, Citation2020). While these figures demonstrate a relatively small demand from same-sex female couples and single women for fertility treatment, there is a demand, nonetheless. The lack of information on funding for DI demonstrates that clinics are failing to recognise the needs of single women and women in same-sex couples, who may not necessarily have a diagnosis of infertility which warrants them opting for IVF but are nevertheless not able to conceive without donor sperm.
Our findings are likely to have a significant impact on potential patients looking to access publicly funded DI. In instances where patients are unable to access the information they need about funding, they may assume that that are not eligible for public funding and look for alternative routes to conception (e.g. online, unregulated sperm donation) (Harper et al., Citation2017; Taylor et al., Citation2022). As more attention is being given to the barriers faced by certain groups when attempting to access publicly funded fertility treatment (Tippett, Citation2023), it is increasingly important that this lack of access to treatment isn’t further compounded by lack of access to clear, readable information.
Prior research has identified and attempted to address the issue of poor health information. For instance, Horner et al. (Citation2000) reported the process of revising and creating appropriate patient education materials for low-income, ethnically diverse families who have children with asthma. The process undertaken to improve the materials included: initial assessment of readability and comprehensibility, as well as accuracy and currency of the information; revision of the materials; and evaluation to determine the effectiveness of the revision using the FRES (Horner et al., Citation2000).
Following the process outlined above, we recommend that the accuracy and currency of the information about criteria and funding for DI treatment is addressed. Given the number of expired links, and clinics listed in the directory with no links to a website, the HFEA’s ‘clinic search’ function might benefit from regular monitoring to ensure that links are provided, and no links are expired. Liaising closely with clinics for updates on any domain name changes would also improve accessibility. As each local ICB, Health Board and LCG has varying (and frequently changing) criteria for treatment and services on offer, it is important that clinics monitor and update this information regularly. It may be useful for clinics to include the date of when the information was last updated, and when it is due to be reviewed, as is currently done on the NHS website. It is also advisable that clinic websites clearly state whether they provide funded treatment to same-sex couples and single women, including details of their local ICB, Health Board, or LCG’s current offer regarding these groups. If clinics do not currently offer funded treatment to these groups, then they should clearly state so. Lastly, we recommend that clinics take care to ensure that funding information is presented as clearly and comprehensibly as possible on their websites, using lay language to ensure that it is below the recommended FRES of ≥90 (NHS, N.D). There are various health literacy toolkits available for those who produce health information which advise on how this can be done (NHS, N.D).
A limitation of this study may be the use of the FRES readability test, which only considers the number of words and syllables, and not the complexity of the vocabulary used. Future studies may wish to interrogate the overall functionality of the website, considering ease of navigation, imagery, font size and style, and spacing, as it is important to consider aspects other than readability which may affect the accessibly of information online. Future studies may also wish to conduct the FRES to determine the readability of the information provided to would-be patients on DI treatments themselves. It may also be useful to conduct research with users who have varying levels of health literacy to explore their experiences of using fertility clinic websites to search for information on funding. This could be achieved by conducting interviews with users after they’ve visited the websites, or during their usage using cognitive interviewing/think aloud techniques (Hattink et al., Citation2016; Wolcott & Lobczowski, Citation2021). Doing so would provide evidence of how users interact with the site, including whether they found it easy to access the desired information, as well as identifying what could be changed to improve their online experience.
Conclusions
Information on public funding for regulated DI treatment is not readily available on UK fertility websites. The lack and inaccessibility of information provided on public funding for DI treatment also made it difficult to decipher who is eligible for this funding, with only six websites mentioning funding for same-sex couples, and only two mentioning funding for single women. The readability of the available information using the FRES showed that it was significantly below the NHS’s recommended score of ≥90, with a mean of 46.3, making it ‘difficult’ to read. To address these issues, we recommend that a process of assessment and revision of the information is undertaken by clinics to ensure that information on the criteria for accessing publicly funded DI services is accessible, clear, and readable by the majority.
Author contributions
FT, RTM, AP and GJ led the conceptualisation of the paper. FT collected the data and drafted the paper. FT, RTM, GJ and AP were involved in the interpretation of the findings and writing of the paper. All authors read the final version and approved it.
Supplemental Material
Download MS Word (16.9 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- British Pregnancy Advisory Service. (2020). BPAS investigation into the IVF postcode lottery: an examination of CCG policy for the provision of fertility services. https://www.bpas.org/media/3369/bpas-fertility-ivf-postcode-lottery-report.pdf
- British Pregnancy Advisory Service. (2021). BPAS Fertility investigation: NHS-funded fertility care for female same-sex couples. https://www.bpas.org/media/3484/bpas-fertility-investigation-nhs-funded-fertility-care-for-female-same-sex-couples.pdf
- Cheng, C., & Dunn, M. (2015). Health literacy and the Internet: a study on the readability of Australian online health information. Australian and New Zealand Journal of Public Health, 39(4), 309–314. https://doi.org/10.1111/1753-6405.12341
- Competition and Markets Authority. (2022). Consumer law compliance review of fertility clinics: findings report. https://assets.publishing.service.gov.uk/media/632d65af8fa8f51d1f83391a/A._Final_findings_report.pdf
- Couper, M. P., Singer, E., Levin, C. A., Fowler, F. J., Jr, Fagerlin, A., & Zikmund-Fisher, B. J. (2010). Use of the Internet and ratings of information sources for medical decisions: results from the DECISIONS survey. Medical Decision Making : An International Journal of the Society for Medical Decision Making, 30(5 Suppl), 106S–114S. https://doi.org/10.1177/0272989X10377661
- Culley, L., Hudson, N., & Rapport, F. (2013). Assisted conception and South Asian communities in the UK: public perceptions of the use of donor gametes in infertility treatment. Human Fertility, 16(1), 48–53. https://doi.org/10.3109/14647273.2013.773091
- Daraz, L., Morrow, A. S., Ponce, O. J., Farah, W., Katabi, A., Majzoub, A., Seisa, M. O., Benkhadra, R., Alsawas, M., Larry, P., & Murad, M. H. (2018). Readability of Online Health Information: A Meta-Narrative Systematic Review. American Journal of Medical Quality : The Official Journal of the American College of Medical Quality, 33(5), 487–492. https://doi.org/10.1177/1062860617751639
- Dobbs, T., Neal, G., Hutchings, H. A., Whitaker, I. S., & Milton, J. (2017). The Readability of Online Patient Resources for Skin Cancer Treatment. Oncology and Therapy, 5(2), 149–160. https://doi.org/10.1007/s40487-017-0051-5
- Fertility Europe and European Society for Human Reproduction and Embryology (ESHRE). (2017). European Policy Audit on Fertility (EPAF). https://fertilityeurope.eu/wp-content/uploads/2018/03/EPAF_FINAL.pdf
- Fertility Fairness. (2017). Sustained disinvestment in NHS fertility services in England; the southeast hardest hit, says Fertility Fairness. https://www.fertilityfairness.co.uk/sustained-disinvestment-in-nhs-fertility-services-in-england-the-southeast-hardest-hit-says-fertility-fairness/
- Gann, B., & Grant, M. J. (2013). From NHS Choices to the integrated customer service platform. Health Information and Libraries Journal, 30(1), 1–3. https://doi.org/10.1111/hir.12020
- Harper, J., Jackson, E., Spoelstra-Witjens, L., & Reisel, D. (2017). Using an introduction website to start a family: implications for users and health practitioners. Reproductive Biomedicine & Society Online, 4, 13–17. https://doi.org/10.1016/j.rbms.2017.02.001
- Hattink, B., Droes, R. M., Sikkes, S., Oostra, E., & Lemstra, A. W. (2016). Evaluation of the Digital Alzheimer Center: Testing Usability and Usefulness of an Online Portal for Patients with Dementia and Their Carers. JMIR Research Protocols, 5(3), e144. https://doi.org/10.2196/resprot.5040
- Hinton, L., Kurinczuk, J. J., & Ziebland, S. (2012). Reassured or fobbed off? Perspectives on infertility consultations in primary care: a qualitative study. The British Journal of General Practice : The Journal of the Royal College of General Practitioners, 62(599), e438–e445. https://doi.org/10.3399/bjgp12X649133
- Horner, S. D., Surratt, D., & Juliusson, S. (2000). Improving readability of patient education materials. Journal of Community Health Nursing, 17(1), 15–23. https://doi.org/10.1207/S15327655JCHN1701_02
- Human Fertilisation and Embryology Authority. (2019). Fertility treatment 2017: trends and figures. https://www.hfea.gov.uk/media/2894/fertility-treatment-2017-trends-and-figures-may-2019.pdf
- Human Fertilisation and Embryology Authority. (2020). Family formations in fertility treatment 2018. https://www.hfea.gov.uk/about-us/publications/research-and-data/family-formations-in-fertility-treatment-2018/
- Human Fertilisation and Embryology Authority. (2021). Fertility clinic search. https://www.hfea.gov.uk/choose-a-clinic/clinic-search/
- Human Fertilisation and Embryology Authority. (2022). Trends in egg, sperm and embryo donation 2020. https://www.hfea.gov.uk/about-us/publications/research-and-data/trends-in-egg-sperm-and-embryo-donation-2020/
- Jabson, J. M., Patterson, J. G., & Kamen, C. (2017). Understanding Health Information Seeking on the Internet Among Sexual Minority People: Cross-Sectional Analysis From the Health Information National Trends Survey. JMIR Public Health and Surveillance, 3(2), e39. https://doi.org/10.2196/publichealth.7526
- Kedzior, S. G. E., Bianco-Miotto, T., Breen, J., Diener, K. R., Donnelley, M., Dunning, K. R., Penno, M. A. S., Schjenken, J. E., Sharkey, D. J., Hodyl, N. A., Fullston, T., Gardiner, M., Brown, H. M., & Rumbold, A. R. (2019). It takes a community to conceive: an analysis of the scope, nature and accuracy of online sources of health information for couples trying to conceive. Reproductive Biomedicine & Society Online, 9, 48–63. https://doi.org/10.1016/j.rbms.2019.08.004
- Mamo, L. (2007). Queering Reproduction: Achieving Pregnancy in the Age of Technoscience. Duke University Press.
- Meads, C., Hunt, R., Martin, A., & Varney, J. (2019). A systematic review of sexual minority women’s experiences of health care in the UK. International Journal of Environmental Research and Public Health, 16(17), 3032. https://doi.org/10.3390/ijerph16173032
- Merrick, H., Wright, E., Pacey, A. A., & Eiser, C. (2012). Finding out about sperm banking: what information is available online for men diagnosed with cancer? Human Fertility, 15(3), 121–128. https://doi.org/10.3109/14647273.2012.702936
- Morahan-Martin, J. M. (2004). How internet users find, evaluate, and use online health information: a cross-cultural review. Cyberpsychology & Behavior, 7(5), 497–510. https://doi.org/10.1089/cpb.2004.7.497
- NHS Confederation. (2022). Clinical Commissioning Groups: Transferring the legacy into learning. https://www.nhsconfed.org/system/files/2022-03/Clinical-commissioning-groups-transferring-the-legacy-into-learning_0.pdf
- National Health Service, Health Education England. (n.d). Health literacy ‘how to’ guide. https://library.nhs.uk/wp-content/uploads/sites/4/2020/08/Health-literacy-how-to-gu ide.pdf
- National Institute for Health and Care Excellence. (2014). NICE calls for an end to postcode lottery of IVF treatment. https://www.nice.org.uk/news/article/nice-calls-for-an-end-to-postcode-lottery-of-ivf-treatment
- Oliffe, M., Thompson, E., Johnston, J., Freeman, D., Bagga, H., & Wong, P. K. K. (2019). Assessing the readability and patient comprehension of rheumatology medicine information sheets: a cross-sectional Health Literacy Study. BMJ Open, 9(2), e024582. https://doi.org/10.1136/bmjopen-2018-024582
- Pook, C. J., Thomas, K., & Bultitude, M. F. (2022). Assessing the quality and readability of NHS urology webpages in England. Journal of Clinical Urology, 15(5), 429–433. https://doi.org/10.1177/20514158211011904
- Richardson, A. (2018). Doctors urge end to IVF postcode lottery to reduce multiple births. The Guardian. https://www.theguardian.com/society/2018/feb/02/doctors-urge-end-to-ivf-postcode-lottery-to-reduce-multiple-births
- Sbaffi, L., & Rowley, J. (2017). Trust and credibility in web-based health information: A review and agenda for future research. Journal of Medical Internet Research, 19(6), e218. https://doi.org/10.2196/jmir.7579
- Spencer, E. A., Mahtani, K. R., Goldacre, B., & Heneghan, C. (2016). Claims for fertility interventions: a systematic assessment of statements on UK fertility centre websites. BMJ Open, 6(11), e013940. https://doi.org/10.1136/bmjopen-2016-013940
- Taylor, F., Turner-Moore, T., Pacey, A., & Jones, G. L. (2022). Are UK Policies and practices for regulated donor insemination forcing women to find unregulated sperm donors online? A perspective on the available evidence. Frontiers in Global Women’s Health, 3, 644591. https://doi.org/10.3389/fgwh.2022.644591
- Tippett, A. (2023). Reproductive rights where conditions apply: an analysis of discriminatory practice in funding criteria against would-be parents seeking funded fertility treatment in England. Human Fertility, 1–11. https://doi.org/10.1080/14647273.2022.2164746
- Tonsaker, T., Bartlett, G., & Trpkov, C. (2014). Health information on the Internet: gold mine or minefield? Canadian Family Physician Medecin de Famille Canadien, 60(5), 407–408.
- van de Wiel, L., Wilkinson, J., Athanasiou, P., & Harper, J. (2020). The prevalence, promotion and pricing of three IVF add-ons on fertility clinic websites. Reproductive Biomedicine Online, 41(5), 801–806. https://doi.org/10.1016/j.rbmo.2020.07.021
- Wolcott, M. D., & Lobczowski, N. G. (2021). Using cognitive interviews and think-aloud protocols to understand thought processes. Currents in Pharmacy Teaching & Learning, 13(2), 181–188. https://doi.org/10.1016/j.cptl.2020.09.005