Abstract
In-vitro fertilisation (IVF) and intra-cytoplasmatic sperm injection (ICSI) are available in Scotland through the National Health Service (NHS) according to specific criteria. There is no standardised NHS tariff for these treatments in Scotland, and variation exists amongst different centres providing NHS services. The aim of this study was to calculate the mean cost of IVF and ICSI cycles for NHS-funded treatment in Scotland. A detailed cost analysis of fresh and frozen cycles was performed, and a breakdown of the various cost components was presented. A deterministic approach was applied using NHS-funded individual cycle data from 2015–2018 and aggregate data. All costs were calculated in UK pounds sterling (£- using 2018 prices). Resource use was assigned to individual cycles based on cycle-level data or expert-informed assumptions; whenever needed, average aggregate costs were assigned to cycles. A total of 9442 NHS-funded cycles were included in the analysis. The average cost of fresh IVF and ICSI cycles was £3247 [£1526–£4215] and £3473 [£1526–£4416], respectively. Frozen cycles averaged £938 [£272–£1085]. This data can be useful to decision-makers, especially where IVF/ICSI is publicly funded, as it delivers a detailed IVF/ICSI cost breakdown. It is an opportunity for other authorities to estimate IVF/ICSI costs, as the methods applied are clear and reproducible.
Introduction
Over 1.3 million in vitro fertilisation (IVF) cycles have been performed in the United Kingdom (UK) since 1991. In 2019, approximately 69,000 IVF cycles were carried out. Globally, there is an increasing demand for assisted reproductive technologies (ART) in general, due to ageing population as well as cultural changes (HFEA, Citation2021). The availability of ART around the world varies greatly, as does access to ART-related services provided by nationalised and private healthcare systems. For instance, Greece has over 4 ART centres per 1,000,000 people, whilst there are only 0.01 per 100,000,000 in Indonesia; this value is around 1.3 in the UK and USA.
ART is covered by some nationalised healthcare systems, subject to eligibility criteria. In the USA, no government reimbursement is offered, and in the UK some cycles may be funded via the National Health System (NHS) (Chambers et al., Citation2009; Collins, Citation2002). In Scotland, these eligibility criteria are based on evidence of infertility and the clinical effectiveness of the ART method, which varies according to a patient’s age. There are four specialist referral centres that provide NHS-funded ART within Scotland, and increasing demand across these four centres was documented (Scottish Government, Citation2016). Coupled with increasing costs, the increasing demand puts pressure on their fixed public budget. IVF and intra-cytoplasmatic sperm injection (ICSI) are complex techniques, with variable costs. Costing studies of ART techniques use different estimation methods applied in different contexts, resulting in a mix of studies hardly comparable between themselves.
Cost estimation may help nationalised healthcare systems to standardise prices for IVF/ICSI and even set tariffs, whilst helping decision-makers to audit expenses based on evidence. Currently, there is a lack of costing studies published in this field. This study aimed to estimate the cost of IVF/ICSI in each of the four ART centres in Scotland to inform a standardised tariff for NHS-Scotland. The study provides information to other decision-makers around the world, especially where ART funding is reimbursed by the healthcare system.
Materials and methods
A conceptual model of the process of fresh and frozen IVF/ICSI cycles was constructed based on Standard Operational Procedures (SOPs) from each of the four fertility centres, followed by consultation with experts at each centre. The aim was to identify key processes and cost components for the cost analyses of a typical ART cycle. The conceptual model is provided in Figure S1 of the Supplementary Material.
Data
Data from 1 January 2015 to 31 July 2018 were extracted from each centre. Individual anonymised cycle-specific data was obtained; resource use data (staff time, equipment, and consumables) was extracted from each centre using aggregated macro-level data or micro-costing, depending on availability. The following cycles were excluded from the analysis: (i) self-funded cycles; (ii) non-IVF/ICSI data (e.g. intra-uterine insemination); (iii) cycles with no funding or date information. The eligibility criteria for NHS-funded cycles in Scotland are described in the Supplementary Material (Scottish Government, Citation2016).
Data analysis
The included costs were staff time, laboratory, equipment, overhead, consumables, and medication costs. Resources use data were obtained from specific cycles, centre-specific expert opinion or derived from the SOPs or conceptual model.
NHS-related costs for adverse events, ongoing pregnancy, and related events (e.g. miscarriage) were not included. Annual storage costs were not considered in the average cycle cost estimation; although storage is continued until patients are no longer eligible for NHS-funded care (e.g. they had a live birth), the subsequent charging is not consistent across Scotland (three centres charge one does not), making it harder to estimate and compare costs. All costs were calculated in UK pounds sterling (£) using 2018 prices. Details of cost calculation are provided in the following sections. All analyses were conducted using the statistical software R version 1.1.463.
Staff cost
Micro-costing was used to calculate the average costs for staff time in each step of the specific cycles. Unit costs were taken from NHS Agenda for Change - Scotland (midpoint pay bands) (NHS, Citation2019a) or centre-specific salaries. Assumptions over contracted working hours and annual leave were based on recommended guidance (Curtis & Burns, Citation2018; NHS, Citation2019b). National insurance and superannuation were included as salary on-costs at appropriate rates (HMRC, Citation2019; NHS Employers, Citation2019). For some procedures, where only aggregate data was available, a top-down approach was adopted.
Equipment cost
Annuitisation over the lifespan was used to calculate the capital costs of equipment (Drummond et al., Citation2015; Glick et al., Citation2014) with a discount rate of 3.5%. Wherever the year of purchase or lifespan was missing, 2018 and 10 years years were assumed, respectively. The equivalent annual cost was calculated per unit of equipment per use. Equipment mean calculated costs were assigned to each specific cycle based on the occurrence of procedures.
Medication cost
Top-down approach was adopted using the budget on medication for NHS-funded procedures from 1 January 2015 to 31 July 2018 for each centre. Based on the SOPs and consultation with the centres, the ratio between the average cost of medication during fresh and frozen cycles was estimated and the average cost per cycle was calculated and allocated to all cycles, for fresh and frozen cycles.
Consumables cost
Aggregate level data on consumables expenditure for NHS-funded procedures was provided by each centre, including delivery charges, gasses, stationary, laboratory consumables, and general consumables. The cost per cycle was considered to be proportional to the time staff spent in each procedure, using centre-specific data from the staff costs/time calculation.
Costs of laboratory tests
SOPs and expert advice from each centre determined which laboratory tests were recommended during cycles. The unit costs of the tests were taken from appropriate reference sources (Table S6 of Supplementary Material) and were adjusted for inflation to 2018 costs (Drummond et al., Citation2015; Thompson, Citation2009).
Overhead cost
Step-down cost accounting method was used (Drummond et al., Citation2015) for the following overhead costs: cleaning, portering, laundry and linen services, energy, rent and rates, and administration and management. Data were obtained from ISD-Scotland (ISD, Citation2018), and details on how these costs were estimated can be found in the reference provided. Costs were redistributed from the hospitals where the ART centres are located to the ART centres based on the floor area ratio between them (Conteh & Walker, Citation2004). Just as for consumables, the assumption that the total overhead costs for each cycle would be proportional to the time staff members spend in each step was adopted.
Total cost
The total cost for each cycle was calculated by the sum of the different costs for fresh IVF, fresh ICSI, and frozen cycle (or embryo transfer – ET). The cost of a full cycle was calculated considering the HFEA definition of a full cycle (HFEA, Citation2019), i.e. one fresh cycle plus the cost of a frozen cycle multiplied by the ratio between frozen and fresh cycles in the centre. Sensitivity analysis was also performed to test for the impact of varying: the proportion of frozen ET in relation to fresh cycles (from 0.35:1 to 1:1); assuming the costs of equipment maintenance are the same for all centres (average cost of maintenance for the provided data); and excluding cycles that were cancelled at early stages (further details in the Supplementary Material).
Adjusting costs for inflation to 2021
Overall average total cost and average total costs for each centre were adjusted for inflation using the NHS Cost Inflation Index (Drummond et al., Citation2015; Jones & Burns, Citation2021; Thompson, Citation2009) in order to keep the values up to date.
Results
Cycle-specific data
Anonymised data from 9,442 NHS-funded cycles (fresh and frozen) in all four centres are summarised in . The data shows little variation in the demographic characteristics of the patients across the centres. The average age is 34 years, and fewer patients were <30 or ≥40 years old, which reflects the average age of patients that seek ART in the UK − 35 years (HFEA, Citation2021) and the age eligibility criteria imposed by NHS-Scotland described in the Supplementary Material.
Table 1. NHS-funded patients’ baseline details and treatment characteristics.
Glasgow and Edinburgh have a much greater number of cycles per annum than the other centres. The distribution of cycles across the years and centres is even. Diagnosis of infertility was missing for over 90% of cycles in Glasgow, however, this variable does not directly impact the costs of a cycle. There was little variation between the proportions of ICSI and IVF across the centres, except in Glasgow, where 86% of cycles are ICSI (40% in other centres). This is because since 2016 Glasgow exclusively performs ICSI, bringing the average up to 86% across the years. On average, across all centres, 69% of the cycles were fresh, of which 45% were ICSI.
Information on the total number of fresh and frozen cycles including self-funded cycles for each centre is shown in . The number of fresh/frozen and NHS-funded/self-funded cycles is important for some of the calculation of costs.
Table 2. Number of cycles from 1 January 2015 to 31 July 2018 per centre.
Costs analysis
A breakdown of the mean costs is summarised in by cost category, cycle type, and centre. Further details of the breakdown can be found in Table S8 of the Supplementary Material. Fresh cycles cost on average £3,364 (IVF + ICSI), whilst this was £938 for frozen cycles. The variation for fresh cycles was £1526 to £4416; for frozen cycles, the variation was £272 to £1085.
Figure 1. Average costs by category, cycle type, insemination type, and centre. The table (bottom) includes total cost (average and range) and the average between centres (in blue). All costs in UK pounds sterling using 2018 prices. IVF: in-vitro fertilisation; ICSI: intra-cytoplasmatic sperm injection; Ab: Aberdeen; Dun: Dundee; Ed: Edinburgh; Gla: Glasgow.
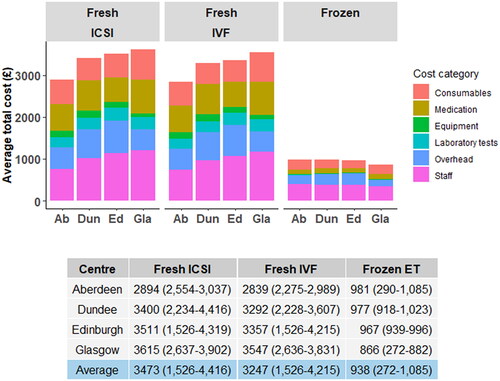
The average total cost of fresh cycles is more than three times higher than frozen cycles, which is unsurprising given that fresh cycles encompass more steps, medication, and procedures. Both IVF and ICSI fresh cycles present similar cost distributions across the centres; staff and medications being the greatest cost components. A similar distribution of costs per category is observed for frozen cycles. Details on unit costs and resource allocation can be found in Tables S1 to S7 of the Supplementary Material.
Staff costs presented some variation between centres due to variations in some procedures, whilst other procedures had similar costs across centres (e.g. sperm thawing). An example of an operational procedure with high variation between centres is “pregnancy confirmation” (coefficient of variation of 76%, with Dundee having the highest cost and Glasgow having the lowest; the difference is driven by the fact that this procedure is done mainly by a nurse in Glasgow and by a team of 2 nurses and one medical doctor in Dundee). Other sources of variation are the time estimated by each centre per procedure (for example, 15 minutes for “embryo scoring” in Aberdeen and 60 minutes in Edinburgh) and professional grades/salaries involved in each procedure (for example, grade 5/6 embryologists perform the procedure in Aberdeen, whilst in Dundee it is performed by grade 7 embryologists).
The budget for equipment and consumables is higher in Glasgow due to the increased activity levels. However, consumables and equipment costs per cycle were similar across centres. The cost of equipment is the lowest cost category in every centre, contributing less to the final total cost of cycles.
Despite their different protocols for laboratory testing, the final laboratory cost per cycle was similar between centres, being almost negligible for frozen cycles.
Medication cost for fresh cycles was estimated to be approximately 6.13 times more than for frozen cycles. Considering there is minimal variation in the costs of medication between NHS- or self-funded cycles, the total budget for medication in each centre per year was split between NHS-funded and self-funded cycles and again distributed 6.13:1 between fresh and frozen cycles. Although Glasgow’s total budget is more than double compared to the other centres, the medication costs per cycle varied only around 10% across centres.
Regarding overhead costs, Edinburgh presented the highest cost per square-metre of area. The overheads in Glasgow and Edinburgh were similar, however, Glasgow has a higher number of cycles, which proportionally decreases the overhead costs per cycle.
The cost of full cycles was based on the frozen ET data for each centre (). Proportionally, 51% (634/1,254) of NHS-funded fresh cycles are accompanied by a frozen ET in Aberdeen. The percentages of frozen ET following a fresh cycle are 38%, 62%, and 35% for Dundee, Edinburgh, and Glasgow, respectively. This means that the costs of “full cycles”, as defined by HFEA, are 1 fresh cycle plus: 0.51, 0.38, 0.62, and 0.35 frozen ET for Aberdeen, Dundee, Edinburgh, and Glasgow. This was used to estimate the average cost of a full cycle per patient per centre, which was £3,328 for Aberdeen (1 fresh cycle + 0.51 frozen ET); following the same logic, full cycles costed £3,693, £3,999, and £3,908 for Dundee, Edinburgh, and Glasgow, respectively. These values represent an estimate of the cumulative cost of a full cycle as only 35% of cycles in Glasgow, for example, had both a fresh and frozen ET. The provision of the two separate cost estimates of fresh and frozen embryo transfer allows the reader to be able to calculate the anticipated cost if this percentage of frozen cycles should vary (e.g. increase to 60%).
The sensitivity analysis scenarios described in the Supplementary Material show that increasing the number of frozen cycles after a fresh cycle increases the costs (maximum of +16% when one full frozen ET after every fresh cycle in Dundee is added); however, this is likely to increase the chances of a successful pregnancy within a full cycle and more studies are necessary. Keeping the maintenance cost of equipment the same across centres had a low impact on final full cycle costs (highest impact of +3% for Glasgow). The final scenario of excluding cancelled cycles also did not impact greatly the final costs (highest of +1% for Aberdeen).
Discussion
This study estimates the cost of IVF and ICSI NHS-funded cycles in Scotland, aiding decision-makers to understand fertility treatment composition and expenses, variations across ART centres, and the impact of the various cost categories on the final total cost. The study includes a wide variety of cost categories not included in previously published studies, comprising staff, equipment, medication, consumables, laboratory tests, and overheads. It is the first study to use this detailed methodology and includes costs of both fresh and frozen cycles. The results show that between 1 January 2015 to 31 July 2018, there were 9442 publicly funded cycles performed through NHS-Scotland. A total of 53% of the cycles were IVF and 46% ICSI; and substantially more fresh cycles were performed than frozen ETs (69% and 31%, respectively).
The cost of a fresh cycle was on average £3364 (£1526 to £4416) with frozen cycles costing on average, £938 (£272 to £1085). The minimum value within the range refers to patients that started treatment but did not get to the final stages: they did not result in egg retrieval or insemination. For frozen cycles, the lower range refers to patients that only attended the follow-up consultation and did not go through embryo transfer. The maximum value within the range refers to patients that finished the treatment, incurring all possible costs included in the study. Fresh cycles were more costly than frozen cycles due to the higher costs inherent to fresh cycles and the complexity of starting a new ART treatment with a patient. Both IVF and ICSI fresh cycles present similar average costs (£3247 and £3473, respectively).
The cost difference between IVF and ICSI is relatively low (average cost £3247 vs. £3473) using the method we adopted for cost estimation. In our study, this difference is related to differences in staff, consumables, and overhead costs. There are differences between ICSI and IVF that may result in a preference for one of them, however, this may be related to factors that are beyond the scope of this study, such as cost-saving components before the cycle starts or differences in effectiveness that may play a role on “cost-per-effective-cycle”.
Comparison to other studies
There is a lack of published studies involving ART costs, and the ones available are hard to compare due to the variation between methods and lack of transparency. The cycles included in this study were all NHS-funded and followed the inclusion criteria established by NHS-Scotland; therefore, the patient cohort is context-specific, somewhat limiting comparability with other studies in different contexts (e.g. ART not publicly funded or different eligibility criteria). No published study was found with this level of methodological detail including fresh and frozen cycles. To our knowledge, this is currently the most comprehensive published ART costing study.
According to a price benchmarking published by NHS-England (NHS, Citation2019c), an IVF cycle (including one fresh and one frozen cycle) costs between £3100 and £3500 (£3500 and £4000 for ICSI). Each subsequent frozen cycle is reported to cost around £1000. This data is useful for comparison yet lacks transparency regarding the methods and included costs; however, it is encouraging that the results reported are similar to those in our study. This study is likely to involve a similar cohort of patients, given similar eligibility criteria across NHS-England and NHS-Scotland.
Cassettari et al. (Citation2016) used activity-based costing and Monte Carlo simulation to estimate the cost of IVF to the Italian healthcare system. They found an average cost of €2300/cycle (2014 prices) however, this study did not include overhead, medication, and laboratory costs. Moreover, the definition of cycle is not defined, making the interpretation of the results and comparison to the present study difficult.
Another study (Pandey et al., Citation2014) presented ART costs according to women of different ages and BMI. The study was a retrospective analysis of Scottish data from a cohort of over 2400 patients between 1998 and 2008 (using 2011 prices). It included costs related to staff time, equipment, antenatal hospital admissions, and some diagnostic procedures. Additionally, it included the cost of treating outcomes, such as miscarriage, which we did not. The mean total cost varied with age and BMI, the average being £3700 across age/BMI categories. Although our costs were not shown by age stratification, the cost analysis by age showed no significant difference between groups; however, the success rate drops considerably at higher ages (data not shown), which drives the cost per live birth up. The decrease in ART effectiveness with age has been vastly covered in the scientific literature (Maheshwari Citation2009; McLernon et al., Citation2019; Zarinara et al., Citation2016). Several economic studies have been published where authors report the cost estimation within different analyses, however, they are very heterogeneous (Daya et al., Citation2001; Fiddelers et al., Citation2006, Citation2009; Polinder et al., Citation2008; Scotland et al., 2011; Sykes et al., Citation2001).
Strengths and limitations
This work uses a transparent and robust method to set costs to specific cycles across all four NHS-funded provider ART centres in Scotland. The large number of cycles adds robustness to the method, and detailed information on each cycle allows the estimation to reflect the centres’ activity. With the available data, it was possible to follow the path each patient took for each cycle, resulting in an accurate distribution of resources for each cycle/patient. The main limitation to the study was the lack of some cycle-specific data (e.g. consumables); whenever this was the case, aggregate data and estimations were transparently adopted.
This study also covered a wide range of direct costs implied in ART, including staff, equipment, medication, consumables, laboratory tests, and overheads. By categorising each cycle in fresh/frozen and IVF/ICSI, the study also becomes a powerful tool to help decision-makers to understand how the resources are distributed and how to apply them more efficiently across cycle categories. To our knowledge, this is the first study that adopted this approach, resulting in transparent and robust costs of category-specific ARTs. It is also important to reiterate that this study was based on a typical IVF/ICSI process and did not include specific data from special cases (e.g. HIV-positive patients). Moreover, the cost of adverse events and pregnancy outcomes (e.g. miscarriage) were not included. These costs may cause the budget to be underestimated.
Implications and conclusions
The results of this study can be used to set a tariff for ART services in Scotland and are useful as a benchmarking for other healthcare systems/providers. Our findings also have wider implications for future planning with varying levels of frozen ET in the UK, for example. The data presented in this study can be useful to policy-makers in countries with publicly funded ART, health insurance providers who provide ART services, and those countries with similar eligibility criteria for ART to those adopted by NHS-Scotland. The breakdown detail of the cost-components involved in ART and how they were allocated can be reproduced in other settings, costs may be estimated, and comparisons may be drawn across countries.
The present study is the most transparent and detailed study published to date and the results serve as a guide to decision-makers in setting a reference tariff price for ART. Future work could explore how much ARTs cost using a prospective approach, including costing diaries and following specific patients for specific periods of time alongside randomised clinical trials.
This work provides a comprehensive picture of the cost variation across the country using a robust and transparent method, enabling decision-makers to set an informed tariff price for reimbursement of ART treatment.
Supplemental Material
Download MS Word (71.2 KB)Acknowledgments
We would like to thank all the staff at the Assisted Reproduction centres in Scotland for their hard work and dedication in extracting data and making it available for analysis. Special thanks to Alison Mctavish, Dr Helen Lyall, Graham Roberts, Ellen Drew, and Lindsey White. We thank Sarah Corcoran and Anthea Taylor for managing and overseeing the project.
Disclosure statement
SMN has participated in Advisory Boards and received consultancy or speaker fees from Access Fertility, Modern Fertility, Ferring, Merck, Roche Diagnostics and The Fertility Partnership. AM has participated in Advisory Boards and has received grants or contracts from HTA/NIHR and NHS Endowment, both not related to the present work; AM has also been paid honorarium and funding to attend scientific meetings by Cook Medical, Ferring, Pharmasure, Geodon Ritcher and Merck Serono for speaking at educational meetings or for attending scientific events; AM became the Editor-in-Chief for this journal in January 2023, but she has not been part of any editorial process for this paper.
Additional information
Funding
References
- Cassettari, L., Mosca, M., Mosca, R., Rolando, F., Costa, M., & Pisaturo, V. (2016). IVF cycle cost estimation using activity based costing and Monte Carlo simulation. Health Care Management Science, 19(1), 20–30. https://doi.org/10.1007/s10729-014-9282-2
- Chambers, G. M., Sullivan, E. A., Ishihara, O., Chapman, M. G., & Adamson, G. D. (2009). The economic impact of assisted reproductive technology: a review of selected developed countries. Fertility and Sterility, 91(6), 2281–2294. https://doi.org/10.1016/j.fertnstert.2009.04.029
- Collins, J. A. (2002). An international survey of the health economics of IVF and ICSI. Human Reproduction Update, 8(3), 265–277. https://doi.org/10.1093/humupd/8.3.265
- Conteh, L., & Walker, D. (2004). Cost and unit cost calculations using step-down accounting. Health Policy and Planning, 19(2), 127–135. https://doi.org/10.1093/heapol/czh015
- Curtis, L. A., & Burns, A. (2018). Unit Costs of Health and Social Care 2018. Report number: Personal Social Services Research Unit, University of Kent. https://doi.org/10.22024/UniKent/01.02.70995
- Daya, S., Ledger, W., Auray, J. P., Duru, G., Silverberg, K., Wikland, M., Bouzayen, R., Howles, C. M., & Beresniak, A. (2001). Cost-effectiveness modelling of recombinant FSH versus urinary FSH in assisted reproduction techniques in the UK. Human Reproduction, 16(12), 2563–2569. https://doi.org/10.1093/humrep/16.12.2563
- Drummond, M. F., Sculpher, M. J., Claxton, K., Stoddart, G. L., & Torrance, G. W. (2015). Methods for the economic evaluation of health care programmes. (4th ed.). Oxford University Press.
- Fiddelers, A. A., Dirksen, C. D., Dumoulin, J. C., van Montfoort, A. P., Land, J. A., Janssen, J. M., Evers, J. L., & Severens, J. L. (2009). Cost-effectiveness of seven IVF strategies: results of a Markov decision-analytic model. Human Reproduction, 24(7), 1648–1655. https://doi.org/10.1093/humrep/dep041
- Fiddelers, A. A., van Montfoort, A. P., Dirksen, C. D., Dumoulin, J. C., Land, J. A., Dunselman, G. A., Janssen, J. M., Severens, J. L., & Evers, J. L. (2006). Single versus double embryo transfer: cost-effectiveness analysis alongside a randomized clinical trial. Human Reproduction (Oxford, England), 21(8), 2090–2097. https://doi.org/10.1093/humrep/del112
- Glick, H. A., Doshi, J. A., Sonnad, S. S., & Polsky, D. (2014). Economic Evaluation in Clinical Trials. Oxford University Press.
- HFEA. (2019). Commissioning guidance for fertility treatment. https://www.hfea.gov.uk/media/2920/commissioning-guidance-may-2019-final-version.pdf
- HFEA. (2021). Fertility treatment 2019: trends and figures. https://www.hfea.gov.uk/about-us/publications/research-and-data/fertility-treatment-2019-trends-and-figures/
- HMRC. (2019). Rates and thresholds for employers: 2019 to 2020. https://www.gov.uk/guidance/rates-and-thresholds-for-employers-2019-to-2020
- ISD. (2018). Costs book 2017/18 - detailed tables. https://www.isdscotland.org/Health-Topics/Finance/Costs/Detailed-Tables/index.asp
- Jones, K., & Burns, A. (2021). Unit costs of health and social care 2021. Personal Social Services Research Unit. https://doi.org/10.22024/UniKent/01.02.92342
- Maheshwari, A. (2009). Impact of Ovarian Ageing on fertility (Thesis). University of Aberdeen.
- McLernon, D. J., Lee, A. J., Maheshwari, A., van Eekelen, R., van Geloven, N., Putter, H., Eijkemans, M. J., van der Steeg, J. W., van der Veen, F., Steyerberg, E. W., Mol, B. W., & Bhattacharya, S. (2019). Predicting the chances of having a baby with or without treatment at different time points in couples with unexplained subfertility. Human Reproduction, 34(6), 1126–1138. https://doi.org/10.1093/humrep/dez049
- NHS. (2019a). Agenda for change in NHS Scotland. https://www.sehd.scot.nhs.uk/pcs/PCS2019(AFC)01.pdf
- NHS. (2019b). NHS pay and benefits. https://www.healthcareers.nhs.uk/working-health/working-nhs/nhs-pay-and-benefits
- NHS. (2019c). Non-mandatory prices - NHS Improvement. https://improvement.nhs.uk/documents/477/Non-mandatory_currencies_and_prices.xlsx
- NHS Employers. (2019). Pension contributions and tax arrangements. https://www.nhsemployers.org/pay-pensions-and-reward/pensions/pension-contribution-tax-relief
- Pandey, S., McLernon, D. J., Scotland, G., Mollison, J., Wordsworth, S., & Bhattacharya, S. (2014). Cost of fertility treatment and live birth outcome in women of different ages and BMI. Human Reproduction, 29(10), 2199–2211. https://doi.org/10.1093/humrep/deu184
- Polinder, S., Heijnen, E. M., Macklon, N. S., Habbema, J. D., Fauser, B. J., & Eijkemans, M. J. (2008). Cost-effectiveness of a mild compared with a standard strategy for IVF: a randomized comparison using cumulative term live birth as the primary endpoint. Human Reproduction, 23(2), 316–323. https://doi.org/10.1093/humrep/dem372
- Scotland, G. S., McLernon, D., Kurinczuk, J. J., McNamee, P., Harrild, K., Lyall, H., Rajkhowa, M., Hamilton, M., & Bhattacharya, S. (2011). Minimising twins in in vitro fertilisation: a modelling study assessing the costs, consequences and cost-utility of elective single versus double embryo transfer over a 20-year time horizon. BJOG: An International Journal of Obstetrics and Gynaecology, 118(9), 1073–1083. https://doi.org/10.1111/j.1471-0528.2011.02966.x
- Scottish Government. (2016). National infertility group report. https://www.gov.scot/publications/national-infertility-group-report/
- Sykes, D., Out, H. J., Palmer, S. J., & van Loon, J. (2001). The cost-effectiveness of IVF in the UK: a comparison of three gonadotrophin treatments. Human Reproduction, 16(12), 2557–2562. https://doi.org/10.1093/humrep/16.12.2557
- Thompson, G. (2009). Statistical literacy guide - How to adjust for inflation. https://commonslibrary.parliament.uk/research-briefings/sn04962/
- Zarinara, A., Zeraati, H., Kamali, K., Mohammad, K., Shahnazari, P., & Akhondi, M. M. (2016). Models predicting success of infertility treatment: A systematic review. Journal of Reproduction & Infertility, 17(2), 68–81.
