ABSTRACT
Objective
To describe the tobacco use profile among COVID-19-infected adult smokers, to assess the nicotine addiction level, and its impact on the disease progression and outcome in Qatar during the early pandemic.
Design
A cross-sectional study was conducted between May 2020 and May 2021.
Setting
Electronic medical records from Qatar’s National Health Information System under the Communicable Disease Center.
Participants
All confirmed COVID-19-infected adults who could communicate in English and Arabic were randomly selected and invited to participate in a telephone survey.
Result
Among 576 subjects, 118 (20.48%) had a smoking history, with 76.3% being current tobacco smokers and 23.7% former smokers. Current smokers were predominantly male (93.3%), single (51.1%), and highly educated (80%).
Cigarette smoking was prevalent among 66.4% of current smokers, with 49.3% smoking ten or fewer cigarettes daily and 71% having low nicotine dependence. In addition, many cigarette users smoked more than one tobacco product during the pandemic. Among COVID-19-infected smokers, 75.6% were symptomatic, and highly nicotine-addicted individuals experienced more hospitalizations, including ICU admissions, with all deaths occurring in this group.
Conclusion
This research concludes that deaths and poor health outcomes were more frequent among COVID-19-infected smokers. Prioritizing smokers for vaccination and promoting cessation is critical.
Introduction
Tobacco smoking is a significant public health problem claiming more than eight million lives annually of which seven million deaths are due to direct smoking while approximately one million are due to exposure to secondhand smoking. Most tobacco users and fatalities are usually in low-and middle-income countries. Since 1990, the prevalence of smoking has declined steadily around the world (WHO, F. Sheets, Citation2023). However, between 2019 and 2020, due to the growth of the global population, the total number of smokers increased to 1.1 billion, establishing the global population tobacco use as 22.3%. This percentage represented 36.7% of all men and 7.8% of women worldwide (Commar et al. Citation2021; WHO, Citation2023).
Smoking is one of the significant preventable risk factors associated with many diseases, including Coronavirus disease 2019 (COVID-19), which is a form of severe acute respiratory syndrome caused by a novel strain of coronavirus (SARS-CoV-2) that initially appeared in Wuhan, China, in December 2019 among a group of patients with pneumonia (CDC-COVID-19, Citation2022). Subsequently, the World Health Organization (WHO) officially declared COVID-19 a Public Health Emergency of International Concern in March 2020 (WHO Director, Citation2020; Coronavirus disease (COVID-19), Citation2023). Studies confirm smoking significantly impairs immunity in smokers, heightening concerns about infection susceptibility, especially during the COVID-19 pandemic. The increased risk is linked to the recurrent hand-to-mouth movement in smoking and the well-established correlation between tobacco smoking and compromised immunity (Beamer et al., Citation2015).
ACE-nicotine mechanism
The ACE2 receptor provides a human cell-binding site for the S protein for SARS-CoV-2, which is found to have a higher affinity for binding with ACE2 in human cells and leads to an increase in the capability of the virus to spread faster from person to person (Hamming et al., Citation2004; Li et al., Citation2003). However, doubt exists regarding the association between COVID-19 infection and the nicotine receptors mechanism. Some studies claim the protective effect of nicotine on contracting the disease, while others present the opposite opinion (Lippi & Henry, Citation2020). It was suggested that ACE2 is upregulated in the airway epithelium of smokers, which was recently observed higher ACE2 gene expression in samples from smokers compared to never-smokers (Cai et al., Citation2020). While Zhao et al. observed that ACE2 is expressed explicitly in type-2 pneumocytes, genes regulating viral reproduction and transmission are highly expressed (Zhao et al., Citation2020). These findings indicate that smokers may be more susceptible to infection by SARS-CoV-2. Nevertheless, Wang et al. also noted an ACE2 connection between smoking and COVID-19 (Wang et al., Citation2020). Furthermore, viral attachment to cell surface ACE2 receptors protects them from immune surveillance mechanisms. However, it leaves them attached to the host longer, thus making them vulnerable hosts for future infections and spread (Sohal et al., Citation2017).
All tobacco users have similar tobacco-related risks, including those associated with traditional cigarettes, waterpipes, and electronic devices. However, none of these products are safer than others, especially among smokers with co-morbidities, such as respiratory and cardiovascular diseases and diabetes, who are at higher risk of infection caused by COVID-19 (Auer et al., Citation2017; McAlinden et al., Citation2019; Rojewski et al., Citation2016; Sohal et al., Citation2019).
Smoking in Qatar and Gulf countries
In Qatar, according to the last GATS survey conducted in 2012, the prevalence of current tobacco smokers was 12.1% (Qatar GATS, Citation2013). However, when comparing Qatar with other neighboring countries, it was found that Qatar had a higher smoking prevalence than the Sultanate of Oman, as Oman was reported to have (7.1%) of current tobacco smokers during 2013 (Oman STEPS, Citation2017), but less than what was observed in Kuwait at 20.5% and Saudi Arabia at 21.4% (Algabbani et al., Citation2018; Kuwait - STEPS 2014, Citationn.d.).
Moreover, in two national studies conducted by Al-Mulla et al., in Qatar during 2003 and 2019 concerning tobacco smoking, the latter study showed a significant drop (15%) in the prevalence of tobacco smoking in Qatar when compared with that published in 2003 as reflected by a 36.5% to 21.5% decrease (Al-Mulla, Citation2003; AlMulla et al. Citation2021). This successful reduction in smoking prevalence could be due to Qatar’s commitment to reduce smoking by 5% by 2022 (Qatar National Health Strategy, Citation2018–2022). Qatar is working hard to achieve this commitment. They adopted the World Health Organization (WHO) Framework Convention on Tobacco Control (FCTC). They implemented Qatar’s anti-tobacco law in 2002 in addition to implementing the MPOWER interventions to reduce the demand for tobacco. In addition to a massive expansion of tobacco-dependence treatment services throughout the country, including all hospitals, primary health care facilities, and specialized cessation centers, all are providing free treatment and support (Tobacco Control-Qatar Public Health Strategy, Citation2017–2022; WHO FCTC, Citation2014).
During the COVID-19 pandemic, many smokers feared contracting infection, which impacted them differently. Some of them increased their smoking rate due to stress and anxiety. In contrast, others found the pandemic an excellent time for quitting, especially with the restrictions and demanding access to tobacco products. On the other hand, there was an increase in-smoking health awareness and promotion during the pandemic. The Ministry of Public Health (MOPH) developed a unique guidance brochure for smokers to advise them on protecting themselves and stopping smoking (Qatar-MOPH, Citation2020).
Nevertheless, smoking cessation services continue to provide support and counseling via the telephone, which is more accessible and preferable among smokers even after removing the restrictions and lockdown (AlMulla & Kouyoumjian, Citation2021). These measures will likely change the smoking pattern of Qatar’s population during the pandemic. However, no study has investigated the level of nicotine dependence among adult smokers in Qatar during the pandemic. Therefore, this cross-sectional study examined the level of nicotine addiction, the everyday tobacco products used among smokers infected with COVID-19 during the pandemic, and how this practice impacted disease progression and outcome.
This study’s results will help establish a baseline for further research on a national level, promote the availability of evidence for policymakers, and guide the implementation of effective smoking-related interventions.
Methods
Study design and setting
This cross-sectional study was conducted in Qatar and is part of a more extensive study published recently (Adli et al., Citation2023). A list of positive COVID-19 patients was obtained from the Health Information System (HIS) department, Qatar’s primary record system at Hamad Medical Corporation (HMC-Qatar, Citation2020).
Study population
The study targeted all current adult smokers aged 18 years and above, both genders and from all nationalities, who could communicate in Arabic or English and were diagnosed with COVID-19 infection by either polymerase chain reaction (PCR) or SARS-CoV-2 rapid antigen test (RDT) during 2020 and 2021.
Current tobacco smoking was defined based on the Centers for Disease Control (CDC) criteria as smoking 100 cigarettes in their lifetime and currently smoking. In contrast, those who smoked at least 100 cigarettes and are now not smoking are classified as former smokers (CDC-NHIS-Tobacco, Citation2017).
Sampling
The required sample size consisted of 576 respondents based on the sample size calculation formula for cross-sectional study (Dean & Sullivan, Citation2013), at a 95% confidence level, with prevalence of 25%, and population of 215,742 COVID-19 infected patients in early pandemic, and design effect of 2.
Ethical consideration
This study is part of a large study (Adli et al., Citation2023), which was conducted in accordance with the Declaration of Helsinki and was approved by an Institutional Review Board of the Medical Research Centre at Hamad Medical Corporation (MRC-HMC); under protocol number MRC-01-21-524. Verbal consent was obtained from all participants by telephone before the interview.
Materials
Study questionnaire
The questionnaire was developed in English after an extensive literature review and consultation with field experts. It was then translated into Arabic by an accredited translation body. We consulted infectious disease and smoking cessation specialists upon selecting the final items to be included in the questionnaire. The face validity of the questionnaire was ensured to avoid ambiguity. The questionnaire consisted of three sections. The first section explored participants’ sociodemographic characteristics (age, gender, nationality, marital status, educational level, employment, and household income). The second section included questions about smoking status and types of tobacco products used by adult smokers. The third section assessed the clinical characteristics of COVID-19 infection, including the number of COVID-19 illnesses, symptomatic or asymptomatic, disease progression, and outcome (CDC-COVID-19 Symptoms, Citation2022; NIH-COVID-19 Treatment Guidelines, Citation2023). In addition, we used the Fagerström Nicotine Dependence (FTND) checklist to assess nicotine addiction. The Fagerström Test for Nicotine Dependence (FTND) scale serves as a validated and reliable instrument for assessing cigarette consumption, compulsion for use, and dependence in individuals who smoke. The tool comprises six questions, with a total score ranging from zero to ten. A higher total FTND score indicates more intense nicotine dependence (Heatherton et al., Citation1991; Pomerleau et al., Citation1989).
Outcome measures
The primary outcome variable was the Nicotine dependence level among COVID-19-infected smokers. It was a quantitative variable that had been classified according to the total score into five categories: (1) 0–2: very low dependence; (2) 3–4: low dependence; (3)5: moderate dependence; (4) 6–7: high dependence; and (5) 8–10: very high nicotine dependence level.
The smoking status is a nominal variable categorized into current and former smokers. Types of tobacco products also were a nominal variable. The participants were asked about each tobacco product they might use, and the answer was recorded as (Yes or No). In addition, COVID-19-related variables consisted of six questions, and all were nominal variables categorized into a specific order, such as (once vs. more than once) for numbers of COVID-19 infection, (Symptomatic or Asymptomatic) for symptoms of COVID-19 infection, level of care, which was categorized into (home isolation, quarantine, or hospital admission). In addition, (Yes or No) variable was used for intensive care unit (ICU) admission and mechanical ventilation (MV) requirement, and (alive or dead) option was used for the COVID-19 outcome.
Other variables, such as sociodemographic aspects, included both quantitative and qualitative variables like age, gender, etc
Study procedure
A list of 576 COVID-19 positive cases was obtained from the electronic medical records (HIS) at Hamad Medical Corporation (HMC) after the IRB approval. A simple random sampling technique was used to approach our participants using a random number generator. Out of 576 invitees, 118 participants had a history of tobacco smoking and were eligible for our study.
Participation was voluntary, and people who agreed to participate gave verbal consent before starting the interview. In addition, our trained interviewer assured the confidentiality of the collected information.
Analysis
We utilized the IBM SPSS version 26 to conduct statistical analysis. First, we presented the quantitative data in mean and standard deviation while we obtained the frequency and percentage of the qualitative variables.
Results
Description of the study sample
During the pandemic, 576 adults aged 18 years and above were approached by telephone interview to participate in our study. One hundred eighteen had a history of smoking. Among 118 smokers, 90 were current tobacco smokers, and 28 were former smokers.
illustrates the main sociodemographic characteristic of current tobacco smokers. Most current tobacco users were males (n = 84, 93.3%), non-Qatari (n = 57, 63.3%), and were between the age of 24 and 39 years. More than half of current smokers (57.8%) had low monthly income (n = 52).
Table 1. Socio-demographic characteristics of current adult smokers diagnosed with COVID-19 infection in Qatar during 2020–2021 (n = 90).
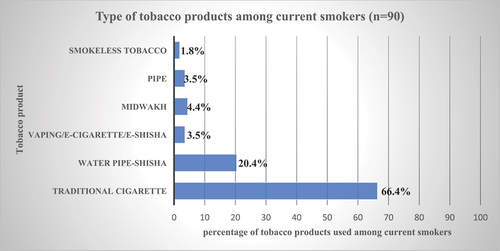
Among current tobacco users, the majority (66.4%, n = 75) of participants were traditional cigarette users, 20.4% (n = 23) were regular shisha users, and 4.4% (n = 5) were midwakh user, as shown in . (Midwakh is a pipe used to inhale tobacco leaves with a variety of barks, herbs, spices, dried flowers, or dried fruit, together called Dokha, which contains high levels of nicotine) (Vupputuri et al., Citation2016).
Figure 1. Type of tobacco products commonly used by current smokers in Qatar during 2020–2021 (n = 90).
Regarding the smoking history of the current tobacco users, the duration of smoking ranged between one year and 35 years, with a mean (± SD) of 9.6 (±7.4) years of smoking tobacco.
Among current cigarette smokers (n = 75, 66.4%), the mean (± SD) number of cigarettes smoked daily was 13.63 (±13.08), with a minimum of one cigarette/day and a maximum of 60 cigarettes/day.
Regarding the consumption of cigarettes, 49.3% (n = 37) of the participants reported smoking 10 or fewer cigarettes per day in response to the first question of the FTND-1. In addition, more than half (56%) of current cigarette users reported smoking their first cigarette 60 minutes after waking up.
Moreover, when the participants were asked about the most challenging cigarette to quit (FTND-3), whether the morning/waking up a cigarette or any other time, 45.3% (n = 34) of them claimed difficulty stopping the morning cigarette. In contrast 54.7% (n = 41) referred to trouble stopping at any other time.
Also, 62.7% of the respondents (n = 47) denied smoking more frequently during the first hours of the day than the rest of the day (FTND-4), and more than half (56.0%, n = 42) of cigarette users reported pausing when they were very ill (FTND-5). In addition, 72% of participants (n = 54) denied having difficulty refraining from smoking in areas where it is prohibited (FTND-6), as seen in . The mean (± SD) FTND score, which ranged between 0 and 10, was 3.43 (±2.99) among our participants.
Table 2. Smoking characteristics of current adult cigarette smokers infected with COVID-19 in Qatar during 2020–2021 (n = 75).
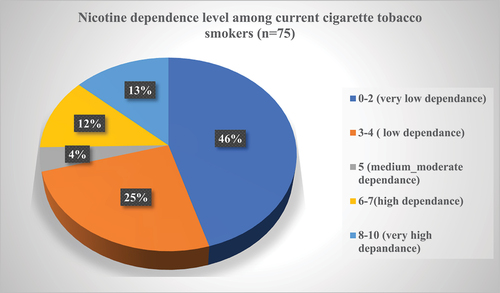
By categorizing the nicotine dependence level into five categories based on the FTND scores, about 71% of the participants (n = 53) had low and very low nicotine dependence. However, 25.3% (n = 19) of the smokers were highly dependent on nicotine, as seen in .
Figure 2. Distribution of cigarette smokers by Fagerstrom Nicotine Dependence Scale (FNDS) categories (n = 75).
Nevertheless, current cigarette tobacco smokers used dual tobacco products or more than one tobacco product during the pandemic, like Shisha (14.7%) and Midwakh (5.3%), as elaborated in .
Table 3. Dual tobacco products used among cigarette smoker adults (n = 75).
Among the current tobacco smokers, the majority (40%, n = 36) underwent quarantine, while a contrasting (23.3%, n = 21) necessitated hospitalization for comprehensive assessment and management. The hospitalized smokers exhibited a mean (± SD) age of 36.67 (±13.74) years, with the duration of hospital admission ranging from 2 to 66 days with a mean (± SD) of 12.67 (±14.14) days. Notably, the survival rate among current tobacco smokers exceeded 97%, as delineated in .
Table 4. Hospital course, progression, and outcome among adult current tobacco smokers infected with COVID-19 infection in Qatar during 2020–2021 (n = 90).
Nevertheless, current cigarette smokers were divided into two groups according to their nicotine dependence levels to determine the impact of nicotine addiction levels on the course of COVID-19 infections. We found that smokers with high nicotine addiction levels (n = 11) required longer hospital admission with a mean (± SD) of 16.82 (±18.15) days compared to the smokers with low nicotine addiction levels (n = 10); which had a mean (± SD) of 8.10 (±5.84) hospital admission days.
In addition, shows that 85.7% of cigarette smokers with high addiction levels were admitted to the ICU compared to 14.3% of smokers with low nicotine addiction levels. Furthermore, both deaths (100%) recorded among current cigarette smokers were from the highly nicotine-dependent group.
Table 5. Severity and outcome of COVID-19 infection among current cigarette smokers with low and high nicotine addiction levels in Qatar during 2020–2021 (n = 75).
Statistics were not applicable due to zero values in the column, so the Odds Ratio and the p-value didn’t calculate.
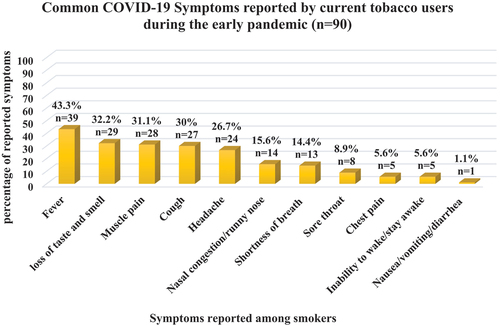
Most current tobacco smokers infected with COVID-19 during the early pandemic reported fever (43.3%). Also, symptoms such as muscle pain, cough, and/or loss of taste/smell were commonly observed among the participants. However, chest pain and nausea, vomiting, and diarrhea were less frequently reported, as illustrated in .
Discussion
Socio-demographical characteristics
In this cross-sectional study, current tobacco smokers among COVID-19-infected adults were single males with high educational levels, in contrast to a survey conducted among 6,659 Chinese participants that found current smokers were reported more among married males with low educational levels (Yang & Ma, Citation2021).
Regarding the type of tobacco products, the number of cigarettes, morning smoking, and addiction level
Traditional cigarettes are the most familiar tobacco products in Eastern Mediterranean Region (EMR) countries, followed by waterpipe/shisha (Maziak et al., Citation2014). Among our study participants, 66.4% of current tobacco users used traditional cigarettes, while 20.4% were on regular shisha, 4.4% and 3.5% were E-Cigarette/E-shisha smokers and midwakh users. These results are inconsistent with a recent national study conducted in 2019 among 1,550 current tobacco users. It was reported that 42.8% of the participants were cigarette smokers, 20.9% used waterpipes, 3.2% were midwakh users, and 2.0% used electronic cigarettes. Moreover, 28.1% of current smokers used more than one type of tobacco product in 2019 (AlMulla et al. Citation2021).
In addition, an increasing tendency for dual, poly-tobacco, and non-traditional tobacco product use among smokers was reported during 2021 in Tzu-hsuan chen et al study (Tzu-Hsuan Chen et al., Citation2021); this tendency was found in our study, as 29.3% of current smokers used dual or more than one type of tobacco product during the COVID-19 pandemic. This finding might be attributed to a high prevalence of anxiety and stress during the pandemic that impacted their smoking behavior.
On average, 66.4% of our study participants smoked about 13.6 cigarettes daily, and 56% reported smoking their first cigarette 60 minutes after waking up. These results seem slightly higher than that reported in Yang’s study, which showed that Chinese smokers smoked around 11.02 cigarettes per day (Yang & Ma, Citation2021). In contrast to our study, Saudi Arabian smokers consumed about 16.8 cigarettes daily (Jarallah et al., Citation1999). A study from the United Kingdom (UK) during the COVID-19 pandemic reported that current smokers smoke a mean of 17.5 cigarettes per day, and 54.5% of them start smoking within 5 minutes after waking up. Moreover, in a UK study, 23.2% of the participants were highly addicted to nicotine, while about 50.5% were moderately addicted (Peckham et al., Citation2021). Compared to our study findings, 71% of current smokers had low levels of nicotine addiction. This difference reflects the ongoing health promotion activities and free tobacco cessation services during the pandemic in Qatar. The low degree of addiction might be explained by changes in smoking behavior in relation to the number of cigarettes per day. Postponing the first-morning cigarette due to their concern about the impact of smoking on COVID-19 infection.
Additionally, a study conducted in China compared smokers’ behavior before and during the pandemic. They found that smokers tend to reduce the number of cigarettes smoked daily, an average reduction of 0.38 per smoker per day. These changes increased smokers’ satisfaction with their health (Yang & Ma, Citation2021).
The impact of smoking on COVID-19 infection and associated outcomes
The current study revealed that COVID-19 symptoms, such as shortness of breath, were less frequently reported (14.4%) among current smokers; however, fever (43.3%), loss of taste and smell (32.2%), muscle pain (31.1%), and cough (30%), were commonly reported among them.
In addition, a large proportion of current smokers underwent quarantine (40%) and home isolation (36.7%). These findings contradicted Hopkinson’s study, in which most current smokers presented with the classic triad of COVID-19 symptoms (fever, cough, and shortness of breath), and most symptomatic patients came to the hospital for further support (Hopkinson et al., Citation2021).
In Qatar, during the early pandemic, quarantine in healthcare facilities was required for asymptomatic patients and mild to moderate cases according to the guidelines (Boston University Chobanian & Avedisian School of Medicine: Infectious Disease, Citation2020).
Also, in our study, 23.3% of current tobacco smokers were hospitalized. Among the hospitalized smokers, 33.3% of patients required admission to the ICU, 71.4% required mechanical ventilation, and 2.2% died. Consistent with our findings, a large study conducted by Guan’s involved 1,085 patients; 137 were current smokers. Among the current smokers, 21.1% (n = 29) had severe COVID-19 disease, and 58.6% (n = 17) had unpleasant consequences, such as ICU admission, requiring invasive mechanical ventilation, or death. However, the study didn’t show statistically significant differences between smokers and nonsmokers (Guan et al., Citation2020).
In addition, a large cohort study was conducted in the United States to identify the effect of smoking history on COVID-19 disease severity among 6,717 hospitalized patients. The authors concluded that adult smokers had a 15% greater chance of requiring mechanical ventilation and a 41% greater chance of death regardless of their sociodemographic characteristics and medical history (Poudel et al., Citation2022). Comparing these results with a study conducted by Huang among 41 patients, none of the current smokers required an ICU admission (Huang et al., Citation2020). This difference might be attributed to the effect of smoking on the regulation of nicotine response, which causes an increase in the severity of respiratory infection (Wang et al., Citation2020). Nonetheless, two independent studies conducted at the University Hospital in Padova and the Hospital in Wuhan, China, reported no significant association between smoking and COVID-19 infection among hospitalized cases. Both studies highlighted a low prevalence of smoking among individuals diagnosed with COVID-19 (Zhang et al., Citation2020).
Strengths and limitations
This study is the first in the Middle East and Qatar that investigate the type of tobacco products used among COVID-19-infected adult smokers during the early stages of the pandemic. It also examines the level of nicotine addiction and its impact on disease progression.
We adapted the international definition of COVID-19 to avoid misclassification bias. In addition, we utilized a simple random sampling technique to allow the generalization of the results. In addition, all study participants were counseled and referred to the tobacco cessation clinic at either the Primary Health Care Center (PHCC) or the tobacco prevention center at HMC, which were active through telephone consultations during the pandemic.
Limitations
Comparing the degree of nicotine addiction before and after the pandemic was unfeasible due to the absence of pre-COVID-19 nicotine dependence data. The Fagerström Test for Nicotine Dependence (FTND) could not be universally applied to diverse tobacco products like shisha and midwakh. Additionally, self-reported information obtained through telephone interviews may lead to potential overestimating or underestimating results. Nevertheless, the researcher addressed this limitation by cross-verifying the information through medical records, enhancing the validation of smoking history and hospital-related data.
Conclusion
Further analytic studies are recommended to investigate the association of nicotine addiction level and COVID-19 disease progression.
Recommendation
Smokers should be prioritized for vaccination, and continuous encouragement to quit should be applied.
Emphasis on the importance of tobacco cessation counseling.
Author contributions
Nada Adli: Conceptualization, methodology, investigation, formal analysis, data curation, project administration, writing- original draft, and writing – review & editing.
Iheb Bougmiza and Nagah Selim: Methodology, supervision, and writing – review & editing.
Consent
Verbal consent was obtained from all participants by telephone before the interview.
Acknowledgments
We Appreciate the Communicable Disease Center and Medical Research Center at Hamad Medical Corporation, Doha-Qatar, for their support. In addition, we thank Qatar National Library (QNL) for providing open-access funding for this article.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- Adli, N., Naja, S., Aabdien, M., Selim, N., Chehab, M., Mohamed, A., Abdu, Y., Faris Shalayel, M. H., Shahbal, S., Abukhattab, M., Al Maslamani, M., & Bougmiza, I. (2023). Smoking-related complications among COVID-19 cases: A population-based survey in Qatar. Journal of Substance Use, 1–11. https://doi.org/10.1080/14659891.2023.2202771
- Algabbani, A. M., Almubark, R., Althumiri, N., Alqahtani, A., & BinDhim, N. (2018). The prevalence of cigarette smoking in Saudi Arabia in 2018. Food and Drug Regulatory Science Journal, 1(1), 1. https://doi.org/10.32868/RSJ.V1I1.22
- Al-Mulla. (2003, September 1). Cigarette smoking habits among Qatari population. Public Health Medicine. https://www.researchgate.net/publication/286737319_Cigarette_Smoking_Habits_among_Qatari_Population
- AlMulla, A., & Kouyoumjian, S. P. (2021). Telephone counseling and quitline service: An opportunity for tobacco use cessation during the COVID-19 pandemic. Qatar Medical Journal, 2021(2), 25. https://doi.org/10.5339/qmj.2021.25
- AlMulla, A., Mamtani, R., Cheema, S., Maisonneuve, P., BaSuhai, J. A., Mahmoud, G., Kouyoumjian, S., & Yang, X. Y. (2021). Epidemiology of tobacco use in Qatar: Prevalence and its associated factors. Public Library of Science One, 16(4), e0250065. https://doi.org/10.1371/JOURNAL.PONE.0250065
- Auer, R., Concha-Lozano, N., Jacot-Sadowski, I., Cornuz, J., & Berthet, A. (2017). Heat-not-burn tobacco cigarettes: Smoke by any other name. JAMA Internal Medicine, 177(7), 1050–1052. https://doi.org/10.1001/JAMAINTERNMED.2017.1419
- Beamer, P. I., Plotkin, K. R., Gerba, C. P., Sifuentes, L. Y., Koenig, D. W., & Reynolds, K. A. (2015). Modeling of human viruses on hands and risk of infection in an office workplace using micro-activity data. Journal of Occupational and Environmental Hygiene, 12(4), 266–275. https://doi.org/10.1080/15459624.2014.974808
- Boston University Chobanian & Avedisian School of Medicine: Infectious Disease. (2020, December 2). Clinical algorithms for admission and discharge | Infectious diseases. https://www.bumc.bu.edu/id/covid-19-response/clinical-algorithms-for-admission-and-discharge/
- Cai, G., Bossé, Y., Xiao, F., Kheradmand, F., & Amos, C. I. (2020). Tobacco smoking increases the lung gene expression of ACE2, the receptor of SARS-CoV-2. American Journal of Respiratory and Critical Care Medicine, 201(12), 1557–1559. https://doi.org/10.1164/rccm.202003-0693LE
- CDC-COVID-19. (2022, December 13). About COVID-19 epidemiology | CDC. https://www.cdc.gov/coronavirus/2019-ncov/science/about-epidemiology/index.html
- CDC-(COVID-19) Symptoms. (2022, October 26). Symptoms of COVID-19 | CDC. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html
- CDC-NHIS-Tobacco. (2017, August 29). NHIS - Adult tobacco use - Glossary. https://www.cdc.gov/nchs/nhis/tobacco/tobacco_glossary.htm
- Commar, A. (WHO Jenewa), Prasad, V., and d’Espaignet, E. T. (2021). WHO global report on trends in prevalence of tobacco use 2000–2025 (4th ed.). World Health Organization.
- Coronavirus disease (COVID-19). (2023). WHO-Coronavirus disease (COVID-19). World Health Organization. https://www.who.int/news-room/fact-sheets/detail/coronavirus-disease-(covid-19)
- Dean, A. G., Sullivan, K. M., Soe, M. M. (2013, April 6). OpenEpi: Open Source Epidemiologic Statistics for Public Health, Version. https://www.openepi.com/Menu/OE_Menu.htm
- Guan, W., Ni, Z., Hu, Y., Liang, W., Ou, C., He, J., Liu, L., Shan, H., Lei, C., Hui, D. S. C., Du, B., Li, L., Zeng, G., Yuen, K.-Y., Chen, R., Tang, C., Wang, T., Chen, P., Xiang, J., … Zhong, N. (2020). Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine, 382(18), 1708–1720. https://doi.org/10.1056/NEJMoa2002032
- Hamming, I., Timens, W., Bulthuis, M. L. C., Lely, A. T., Navis, G. J., & van Goor, H. (2004). Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. The Journal of Pathology, 203(2), 631–637. https://doi.org/10.1002/PATH.1570
- Heatherton, T. F., Kozlowski, L. T., Frecker, R. C., & Fagerstrom, K. ‐. (1991). The fagerström test for nicotine dependence: A revision of the fagerstrom tolerance questionnaire. British Journal of Addiction, 86(9), 1119–1127. https://doi.org/10.1111/J.1360-0443.1991.TB01879.X
- HMC-Qatar. (2020, January 1). Health information management. https://www.hamad.qa/en/hospitals-and-services/hamad-general-hospital/pages/health-information-management.aspx
- Hopkinson, N. S., Rossi, N., El-Sayed-Moustafa, J., Laverty, A. A., Quint, J. K., Freidin, M., Visconti, A., Murray, B., Modat, M., Ourselin, S., Small, K., Davies, R., Wolf, J., Spector, T. D., Steves, C. J., & Falchi, M. (2021). Current smoking and COVID-19 risk: Results from a population symptom app in over 2.4 million people. Thorax, 76(7), 714–722. https://doi.org/10.1136/THORAXJNL-2020-216422
- Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., Hu, Y., Zhang, L., Fan, G., Xu, J., Gu, X., Cheng, Z., Yu, T., Xia, J., Wei, Y., Wu, W., Xie, X., Yin, W., Li, H., Liu, M., … Cao, B. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (London, England), 395(10223), 497–506. https://doi.org/10.1016/S0140-6736(20)30183-5
- Jarallah, J. S., Al-Rubeaan, K. A., Al-Nuaim, A. R. A., Al-Ruhaily, A. A., & Kalantan, K. A. (1999). Prevalence and determinants of smoking in three regions of Saudi Arabia. Tobacco Control, 8(1), 53–56. https://doi.org/10.1136/TC.8.1.53
- Kuwait - STEPS 2014. (n.d.). Retrieved August 20, 2022, from https://extranet.who.int/ncdsmicrodata/index.php/catalog/472
- Li, W., Moore, M. J., Vasllieva, N., Sui, J., Wong, S. K., Berne, M. A., Somasundaran, M., Sullivan, J. L., Luzuriaga, K., Greeneugh, T. C., Choe, H., & Farzan, M. (2003). Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature, 426(6965), 450–454. https://doi.org/10.1038/nature02145
- Lippi, G., & Henry, B. M. (2020). Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19). European Journal of Internal Medicine, 75, 107–108. https://doi.org/10.1016/j.ejim.2020.03.014
- Maziak, W., Nakkash, R., Bahelah, R., Husseini, A., Fanous, N., & Eissenberg, T. (2014). Tobacco in the Arab world: Old and new epidemics amidst policy paralysis. Health Policy and Planning, 29(6), 784–794. https://doi.org/10.1093/HEAPOL/CZT055
- McAlinden, K. D., Sohal, S. S., & Sharma, P. (2019). There can be smoke without fire: Warranted caution in promoting electronic cigarettes and heat not burn devices as a safer alternative to cigarette smoking. ERJ Open Research, 5(3), 00114–2019. https://doi.org/10.1183/23120541.00114-2019
- NIH-COVID-19 Treatment Guidelines. (2023, March 6). Clinical spectrum | COVID-19 treatment guidelines. https://www.covid19treatmentguidelines.nih.gov/overview/clinical-spectrum/
- Oman STEPS. (2017, January 1). 2017 STEPS fact sheet Oman (Databook tobacco). WHO. https://www.who.int/publications/m/item/2017-steps-fact-sheet-oman-databook-tobacco
- Peckham, E., Allgar, V., Crosland, S., Heron, P., Johnston, G., Newbronner, E., Ratschen, E., Spanakis, P., Wadman, R., Walker, L., & Gilbody, S. (2021). Investigating smoking and nicotine dependence among people with severe mental illness during the COVID-19 pandemic: Analysis of linked data from a UK closing the Gap cohort. British Journal of Psychiatry Open, 7(3), e86. https://doi.org/10.1192/BJO.2021.45
- Pomerleau, C. S., Majchrzak, M. J., & Pomerleau, O. F. (1989). Nicotine dependence and the fagerström tolerance questionnaire: A brief review. Journal of Substance Abuse, 1(4), 471–477. https://doi.org/10.1016/S0899-3289(20)30011-0
- Poudel, R., Daniels, L. B., DeFilippis, A. P., Hamburg, N. M., Khan, Y., Keith, R. J., Kumar, R. S., Strokes, A. C., Robertson, R. M., Bhatnagar, A., & Santulli, G. (2022). Smoking is associated with increased risk of cardiovascular events, disease severity, and mortality among patients hospitalized for SARS-CoV-2 infections. Public Library of Science One, 17(7), e0270763. https://doi.org/10.1371/JOURNAL.PONE.0270763
- Qatar GATS. (2013, January 1). Global Adult Tobacco Survey (GATS) 2013 Qatar. https://cdn.who.int/media/docs/default-source/ncds/ncd-surveillance/data-reporting/qatar/gats/qatcountryreport.pdf?sfvrsn=baf6e4ac_2&download=true
- Qatar-MOPH. (2020, March 1). Ministry of public health - Educational & awareness materials about coronavirus disease 2019 (COVID-19). MOPH. https://www.moph.gov.qa/english/Pages/covid19edu.aspx
- Qatar National Health Strategy. (2018–2022). Ministry of Public Health 2018. Retrieved from https://www.moph.gov.qa/english/strategies/National-Health-Strategy-2018-2022/Pages/default.aspx
- Rojewski, A. M., Baldassarri, S., Cooperman, N. A., Gritz, E. R., Leone, F. T., Piper, M. E., Toll, B. A., & Warren, G. W. (2016). Exploring issues of comorbid conditions in people who smoke. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco, 18(8), 1684–1696. https://doi.org/10.1093/NTR/NTW016
- Sohal, S. S., Eapen, M. S., Naidu, V. G. M., & Sharma, P. (2019). IQOS exposure impairs human airway cell homeostasis: Direct comparison with traditional cigarette and e-cigarette. ERJ Open Research, 5(1), 00159–2018. https://doi.org/10.1183/23120541.00159-2018
- Sohal, S. S., Hansbro, P. M., Shukla, S. D., Eapen, M. S., & Walters, E. H. (2017). Potential mechanisms of microbial pathogens in idiopathic interstitial lung disease. Chest, 152(4), 899–900. https://doi.org/10.1016/J.CHEST.2017.05.024
- Tobacco Control-Qatar Public Health Strategy. (2017–2022). Ministry of Public Health 2017. Retrieved from https://www.moph.gov.qa/english/strategies/Supporting-Strategies-and-Frameworks/QatarPublicHealthStrategy/Pages/default.aspx
- Tzu-Hsuan Chen, D., Girvalaki, C., Mechili, E. A., Millett, C., & Filippidis, F. T. (2021). Global patterns and prevalence of dual and poly-tobacco use: A systematic review. Nicotine & Tobacco Research, 23(11), 1816–1820. https://doi.org/10.1093/NTR/NTAB084
- Vupputuri, S., Hajat, C., Al-Houqani, M., Osman, O., Sreedharan, J., Ali, R., Crookes, A. E., Zhou, S., Sherman, S. E., & Weitzman, M. (2016). Midwakh/Dokha tobacco use in the Middle East: Much to learn. Tobacco Control, 25(2), 236–241. https://doi.org/10.1136/TOBACCOCONTROL-2013-051530
- Wang, J., Luo, Q., Chen, R., Chen, T., & Li, J. (2020). Susceptibility analysis of COVID-19 in smokers based on ACE2. Preprints, 2020030078. https://doi.org/10.20944/PREPRINTS202003.0078.V1
- WHO Director. (2020, March 11). WHO director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020
- WHO FCTC. (2014, May 5). Parties to the WHO FCTC (ratifications and accessions) - Global alliance for tobacco control. https://fctc.org/parties-ratifications-and-accessions-latest/
- WHO F. Sheets. (2023, July 31). Tobacco. https://www.who.int/news-room/fact-sheets/detail/tobacco
- Yang, H., & Ma, J. (2021). How the COVID-19 pandemic impacts tobacco addiction: Changes in smoking behavior and associations with well-being. Addictive Behaviors, 119, 106917. https://doi.org/10.1016/J.ADDBEH.2021.106917
- Zhang, J. J., Dong, X., Cao, Y. Y., Yuan, Y. D., Yang, Y. B., Yan, Y. Q., Akdis, C. A., & Gao, Y. D. (2020). Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy, 75(7), 1730–1741. https://doi.org/10.1111/ALL.14238
- Zhao, Y., Zhao, Z., Wang, Y., Zhou, Y., Ma, Y., & Zuo, W. (2020). Single-cell RNA expression profiling of ace2, the receptor of SARS-CoV-2. American Journal of Respiratory and Critical Care Medicine, 202(5), 756–759. https://doi.org/10.1164/RCCM.202001-0179LE