Abstract
Increasingly, children are considered for a unilateral CI, even if the contralateral ear falls outside current audiological guidelines, especially if they are not considered to be reaching their educational potential. The primary aim was to investigate the benefit of unilateral CI in children currently outside UK [National Institute for Health and Care Excellence Technology Appraisal Guidance. 2009. Cochlear implants for children and adults with severe to profound deafness. NICE technology appraisal guidance [TAG166]. Available January 29, 2016 from http://www.nice.org.uk/ta166] audiological guidelines in the contralateral ear. The secondary aim was to measure compliance. A retrospective case review with standard demographic data was performed. Forty-seven children were identified as having received a unilateral CI with the contralateral ear falling outside of current UK audiological criteria. These children were allocated to two groups; with hearing between 50 and 70 dB, and 70 and 90 dB at 2 and 4 kHz in the contralateral ear, respectively. Categories of auditory performance (CAP) were assessed. Pre- and post-operative CAP scores demonstrated a statistically significant improvement in auditory perception. We would suggest that assessing candidacy in individual ears and subsequent unilateral CI, has given these children a benefit they may not otherwise have acquired if they only had bilateral hearing aid.
Introduction
Traditionally, CI candidacy criteria were determined as severe to profound sensorineural hearing loss (SNHL) in both ears, with poor speech recognition in best aided conditions. When these audiological criteria are met, CI in one or both ears was recommended. The criteria for CI continue to evolve, both in response to improving technology and design, but also as our understanding of the developmental and educational consequences of hearing loss expands. Increasingly, children are considered for a unilateral CI, even if the contralateral ear falls outside current audiological guidelines, and especially if they are not considered to be reaching their educational potential.
In children with asymmetric hearing loss where one ear is considered aidable, the amount of residual hearing in the ‘better ear’ is often still poor. If these children were to receive a CI in the poorer hearing ear and a hearing aid (HA) in the better ear, this would allow for bimodal stimulation, with acoustic amplification from one ear and electric stimulation from the contralateral ear.
Here we present the outcomes of CI in children with potentially useable hearing in the contralateral ear. This study was not an attempt to evaluate CI in single sided deafness and all implanted ears met current audiological criteria.
Methods
We performed a retrospective case note review of electronic and paper databases looking at all children receiving a unilateral CI whose contralateral ear was audiologically outside current UK (CitationNICE, 2009) guidelines for implantation. The primary aim was to assess improvement in hearing performance following unilateral CI in children outside current audiological guidelines in the contralateral ear. The secondary outcome measured was compliance, which we reported as full, or part-time use, of their CI and HA. Due to the influences of maturation on language development, only improvements in auditory processing using pre- and post-operative CAP scores on these patients have been reported (best score = 9). Post-operative CAP scores reported here reflect the most recent CAP score at annual review (ranging from 12 months to 4 years). Pre- and post-operative CAP scores were assessed by a speech and language therapist familiar with each child and possessing the clinical skills to determine if the child was able to comprehend conversation appropriate to their age. Statistical analysis was carried out using StatsDirect Medical Statistics Software. Subjective assessment of benefit was assessed using the BAPP questionnaire.
Results
Forty-seven consecutive children were identified with a unilateral CI with the contralateral ear falling outside of current implant candidacy. Of these, 31 were male and 16 were female. 13/47 (27.7%) were found to be congenitally deaf, 11/47 (23.4%) were found to have wide vestibular aquaducts, and 4/47 (8.5%) were post-meningitic. The remaining 19/47 (40.4%) were due to various other underlying pathologies. Average age at referral was 4.1 years (range from 1 month to 11 years 9 months). Average age at implantation was 5.2 years (range from 1 year 1 month to 14 years 3 months). Average time between referral and implantation was 1 year. Patients were defined into two groups based on their audiological results; Group 1 with hearing thresholds between 50 and 70 dB HL at 2 and 4 kHz (n = 10) and Group 2 with hearing thresholds between 70 and 90 dB HL at 2 and 4 kHz (n = 37) in the non-implanted ear, respectively. The mean pre-operative CAP score was 5.02. The mean post-operative CAP score was 7.22. The pre- and post-operative CAP scores are summarized in Fig. and Table .
Figure 1 Pre- and most recent post-operative CAP scores. This demonstrated a statistically significant improvement in hearing performance following unilateral CI and persistent use of a conventional HA in the better hearing ear.
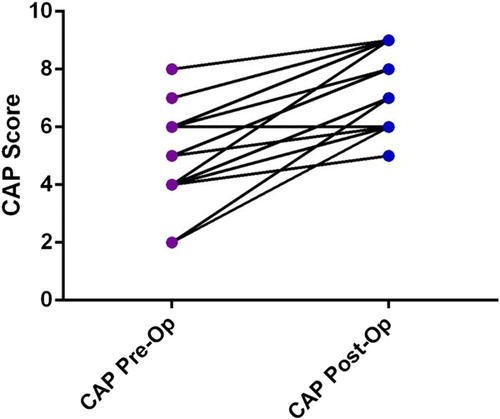
Table 1 Pre and post-operative CAP scores demonstrating the progression of children from CAP scores ≤ 6 pre-implantation to CAP scores of ≥6 post-implantation
Of the 47 children, only one child subsequently rejected their CI. 9/10 (90%) in Group 1 were fully compliant with both their CI and HA. 5/37 (13.5%) children in Group 2 subsequently changed the pattern of hearing aid use to either intermittent or non-use. Analysis of parental opinion for the adolescent subset of our patient population (n = 6) demonstrated that 5/6 (83.3%) reported subjective benefit based on the BAPP questionnaire.
Discussion
For children with asymmetrical losses with ‘aidable’ thresholds in the contralateral ear, definitive indications for CI are still in evolution. At present, the number of children referred for CI with asymmetric hearing loss is small. This possibly reflects a selection bias or lack of awareness of the potential benefits of CI in children who have one ear out of audiological criteria. Many of these are able to function with a noticeable asymmetry, with varying degrees of hearing in the contralateral ear (CitationMok et al., 2010). In these scenarios, traditionally, the poorer ear will not have been considered for CI due to the presence of a better hearing contralateral ear. As such, auditory input remains markedly asymmetric, with resultant loss of the ability to restore binaural processing.
Bilateral stimulation to the auditory system is critical for auditory processing, including spatial hearing, spectral distance, head shadow effect, binaural squelch and binaural summation (CitationBronkhorst and Plomp, 1989). Previous studies have demonstrated that, even when the better hearing ear has normal thresholds, hearing with just one ear results in impaired speech understanding in noise (CitationAbel et al., 1982) and reduced sound localization (CitationBovo et al., 1988). This loss is all the more relevant in children with asymmetric hearing loss, since their better hearing ear often does not have normal hearing thresholds. Previous studies have demonstrated that children with a unilateral hearing deficit show disadvantages in communication and educational settings compared to those who have intact binaural hearing (CitationLitovsky et al., 2006; CitationVerschuur et al., 2005). Additionally, children with symmetrical hearing loss are similarly disadvantaged if they only use one HA (CitationScherf et al., 2009a) or one CI (CitationScherf et al., 2009b) and no device contralaterally.
Analysis of pre- and post-implantation CAP scores demonstrated benefit. Even though the pre-operative CAP scores were commonly 5–6/9, the addition of the CI allowed children to cope better in more challenging listening environments. In addition, 5/6 (83.3%) of the teenage patients in our cohort reported subjective benefit from their CI, often preferring it over their HA. Only 1 teenage child rejected her CI. Following surgery, this patient's thresholds in the non-implanted ear improved significantly, such that she was unable to assimilate acoustic and electric stimuli.
All but one (90%) of the children in Group 1 were fully compliant with both their CI and HA. These children, just under a fifth of our cohort (19.1%), are 20–40 dB thresholds outside of current audiological guidelines for implantation in the contralateral ear. In addition, 32/37 (86.5%) of children in Group 2 were fully compliant with both their CI and HA. These figures indicate that children are able to successfully assimilate the electrical signal from a CI with the acoustic signal from their HA. 2/37 children in Group 2 became non-users of their HA. Of these, the older child, with access to language, told us that he preferred listening with his implant and did not like the sound he got from his HA. The younger child was poorly compliant with her HA pre-implant and her family have not pursued full-time use at home. 3/37 children in Group 2 used their HA intermittently. This is partly because their educational institutions insist on HA use while at school. All three of these children persistently removed their HA at home and their families are currently not pursuing on-going use. Additionally, these three children are presently too young to tell us why they do not want to wear their HA.
These findings highlight the need for holistic assessment of a child, taking into consideration their educational needs, progress and co-morbidities, rather than focussing on audiological thresholds alone.
In terms of study limitations, CAP scores are not ear-specific making it difficult to ascertain exactly what proportion of improvement was due to the addition of the CI. In the absence of a control group, it would be extremely difficult to determine with confidence the effect of potential confounding factors such as time progression and natural language development. Beyond level 6 on the CAP score, the functional priority is more related to coping in complex listening environments. Our hypothesis is children have difficulty doing this while accessing just one ear. As an example, some of the teenagers in our cohort stalled at level 6 on the pre-operative CAP for a considerable length of time prior to CI, and have since made significant progress following implantation.
The present results indicate that even though the better ear performance did not meet traditional CI candidacy criteria, the majority of participants received benefit from a CI in the poorer hearing ear, as measured by CAP and subsequent compliance with the CI and contralateral HA. Assessment of each ear separately and treatment with the most appropriate amplification device available for an individual ear may be prudent, if the goal is optimal hearing in daily living. This is especially true given that we do not fully understand the critical time period for acquiring binaural processing and to what extent binaural abilities can be achieved in the presence of asymmetrical hearing loss (CitationHarrison et al., 2005).
Conclusion
It has previously been reported that children have difficulty assimilating electrical and acoustic stimulation from a CI and HA (CitationCrew et al., 2015). Within the current patient cohort, CAP scores demonstrated an improvement in hearing performance following unilateral CI and persistent use of a conventional HA in the better hearing ear. In addition, the excellent compliance demonstrated by 97.9% and 89.5% of children being fully compliant with their CI and HA, respectively, indirectly suggests that these children are able to gain benefit from listening bimodally. We would suggest that assessing candidacy in individual ears and subsequent unilateral CI, has given these children a benefit they may not otherwise have acquired if they only had bilateral HA.
Disclaimer statements
Contributors None.
Conflict of interest None.
Ethics approval None.
Additional information
Funding
References
- Abel, S.M., Birt, D., Mclean, J.A. 1982. Sound localization in hearing-impaired listeners. In: Gatehouse, R.W. (ed.), Localization of sound: theory and applications. Groten, CT: Amphora Press, pp. 207–219.
- Bovo, R., Martini, A., Agnoletto, M., Beghi, A., Carmignoto, D., Milani, M., et al. 1988. Auditory and academic performance of children with unilateral hearing loss. Scandinavian Audiology. Supplementum, 30: 71–74.
- Bronkhorst, A.W., Plomp, R. 1989. Binaural speech intelligibility in noise for hearing-impaired listeners. The Journal of the Acoustical Society of America, 86: 1374–1383. doi: 10.1121/1.398697
- Crew, J.D., Galvin III, J.J., Landsberger, D.M., Fu, Q.-J. 2015. Contributions of electric and acoustic hearing to bimodal speech and music perception. PLoS ONE, 10(3): e0120279. doi:10.1371/journal.pone.0120279.
- Harrison, R.V., Gordon, K.A., Mount, R.J. 2005. Is there a critical period for cochlear implantation in congenitally deaf children? Analyses of hearing and speech perception performance after implantation. Developmental Psychobiology, 46(3): 252–261. doi: 10.1002/dev.20052
- Litovsky, R.Y., Johnstone, P.M., Godar, S.P. 2006. Benefits of bilateral cochlear implants and/or hearing aids in children. International Journal of Audiology, 45(S1): 78–91. doi: 10.1080/14992020600782956
- Mok, M., Galvin, K., Dowell, R., McKay, C. 2010. Speech perception benefit for children with a cochlear implant and a hearing aid in opposite ears and children with bilateral cochlear implants. Audiology and Neurotology, 15(1): 44–56. doi: 10.1159/000219487
- National Institute for Health and Care Excellence Technology Appraisal Guidance. 2009. Cochlear implants for children and adults with severe to profound deafness. NICE technology appraisal guidance [TAG166]. Available January 29, 2016 from http://www.nice.org.uk/ta166.
- Scherf, F., Van Deun, L., Van Wieringen, A., Wouters, J., Desloovere, C., Dhooge, I., et al. 2009a. Three-year postimplantation auditory outcomes in children with sequential bilateral cochlear implantation. Annals of Otology, Rhinology and Laryngology, 118(5): 336–344. doi: 10.1177/000348940911800504
- Scherf, F., Van Deun, L., Van Wieringen, A., Wouters, J., Desloovere, C., Dhooge, I., et al. 2009b. Functional outcome of sequential bilateral cochlear implantation in young children: 36 months postoperative results. International Journal of Pediatric Otorhinolaryngology, 73(5): 723–730. doi: 10.1016/j.ijporl.2009.01.009
- Verschuur, C.A., Lutman, M.E., Ramsden, R., Greenham, P., O'Driscoll, M. 2005. Auditory localization abilities in bilateral cochlear implant recipients. Otology & Neurotology, 26(5): 965–971. doi: 10.1097/01.mao.0000185073.81070.07
