Abstract
In the recent past, inclusion criteria for cochlear implant surgery expanded to patients with ever more residual acoustic hearing in the low frequencies. By applying the meticulous hearing preservation surgical strategy and specifically designed atraumatic electrode arrays, residual hearing can be preserved to a meaningful extent in a large majority of patients. In this paper, we describe two female patients suffering from mechanically evoked tinnitus after hearing preservation cochlear implantation surgery with MEDEL flex electrodes. The occurrence of audible perceptions through mechanical stimulation in the region of the external ear is believed to be due to the direct transmission of movements via the electrode array to the basilar membrane of the inner ear. In both cases, the mechanically evoked tinnitus led to revision surgery with immobilization of the array in the mastoid cavity. Despite eliminating the tinnitus, the revision surgery led to a loss of residual hearing in one patient, whereas the relatively poor residual hearing in the other revision case remained unchanged. The presence of mechanically evoked tinnitus seems to be associated with increased fragility of inner ear structures and hearing function, possibly due to direct mechanical contact of the electrode array with the basilar membrane. Consequently, the electrode array needs to be carefully immobilized in the mastoid cavity at a distance from soft tissue to prevent mechanical damage of inner ear structures, particularly in female patients with fine muscular tissue.
Introduction
Cochlear implantation (CI) has become the gold standard treatment in patients suffering from bilateral and unilateral profound sensorineural hearing loss. Recently, indication criteria expanded to patients with important residual hearing in the low frequencies and sloping high-frequency hearing loss (Carlson, Citation2020). Preservation of useful residual hearing is feasible following meticulous hearing preservation surgery in around 80% of cases (Perkins et al., Citation2021). When stimulating the residual low-frequency hearing acoustically with a hearing aid and the high-frequency range electrically with the CI, aided hearing is typically in the highest possible range, outperforming electrical stimulation alone (Sargsyan et al., Citation2021). The advent of new therapies may also bring about new forms of complications, as we will show here with a mini-series of two patients with mechanically induced tinnitus after CI with preservation of low-frequency hearing. The occurrence of audible perceptions through mechanical stimulation in the region of the outer ear is believed to be due to the direct transmission of movements via the electrode array into the inner ear.
Material and methods
As of the end of 2020, a total of 558 CIs have been performed in the Geneva University hospital since the beginning of the program in 1985. For many years, all patients in Geneva have been operated with the hearing preservation soft surgery technique, independent of the presence or absence of residual hearing to minimize cochlear trauma and to promote cochlear health and thereby optimal long-term performance of the cochlear implant (Pfingst et al., Citation2015). The surgical technique at the level of the round window implies either a round window insertion of a suitable, small and flexible electrode array or an insertion through a minimally traumatic cochleostomy antero-inferiorly to the round window membrane, depending on the local anatomy (Adunka et al., Citation2010). At the level of the mastoid, the electrode array is secured below bony overhangs and the musculo-periosteal layer sutured in a watertight fashion. A new and unusual complication with mechanically induced tinnitus has been recently observed in two patients, implanted for partial deafness with residual hearing in the low frequencies.
Case presentations
Patient 1
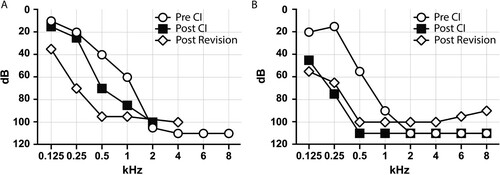
A 47-year-old female presented with progressive bilateral sensorineural hearing loss of unknown origin beginning at age 20. In her professional life, she had to participate in telephone conversations and group meetings for which her hearing aid had become insufficient. A Medel Synchrony implant with a flex 24 electrode was implanted on the right side. At the end of the procedure and at first fitting, all electrophysiological parameters were optimal, hearing was nicely preserved through surgery (A). Speech perception and hearing performance rapidly improved with the cochlear implant in the following weeks.
Figure 1 Unaided hearing thresholds tested for patient 1 (A) and patient 2 (B) before cochlear implantation (white circles), after cochlear implantation (black squares), and after revision surgery (white rectangles).
At the 6-month follow-up visit, the patient started to complain about hearing a noise every time she touched her right ear. Sleep was disturbed by the noise each time she laid her operated ear on the pillow. The electrodes were confirmed to be functional through impedance and telemetry testing, the hearing performance remained highly satisfactory and there was no sign of a local complication. Palpation of the conchal cartilage revealed a wiry resistance. Exteriorization of the electrode lead was suspected and revision surgery was planned. The site at the mastoid was revised via a retroauricular approach and the electrode array was carefully dissected from the sinodural angle. A partial extrusion of the electrode array through the very thin musculo-periosteal layer at the level of the mastoid cortex was found (A). The array was gently liberated from the surrounding soft tissue (B) and secured with a titanium mini-plate (C). The patient did not perceive any more mechanically evoked tinnitus after the revision and sleep was undisturbed. Unfortunately, the residual hearing dropped a few weeks after the revision (A).
Patient 2
A 77-year-old female patient with progressive sensorineural hearing loss of unknown origin was implanted with a Medel Synchrony flex 28 device on the right side with partial preservation of residual hearing (B). Two years after the implantation, she complained of hearing a disturbing noise when touching her ear. Sleep was disturbed each time she changed position to lay on the implanted ear. The hearing performance remained unchanged, as well as the electrophysiological parameters. The palpation revealed a wiry resistance at the posterior wall of the external auditory meatus and the CT-scan confirmed the extrusion of the array loop beyond the bony mastoid border (). At revision surgery, a part of the electrode array was found to be in direct contact with the remarkably thin external auditory canal soft tissue. The array was repositioned in the mastoid (with maximal care taken to avoid movements of the intracochlear part) and maintained in position by a non-resorbable suture placed in a bony burr canal. Residual hearing remained roughly unchanged and the mechanically evoked tinnitus disappeared completely after the revision (B).
Figure 3 Computed tomography scans of patient 2 at day 2 post initial CI surgery (A), at 10 months post initial CI surgery at onset of symptoms (B) and after revision with fixation of the array and resolution of symptoms (C). The electrode array has worked itself out of the bony mastoid cavity borders (B) and was stably placed back into the cavity with a non-resorbable suture (C).

Discussion
We have described two cases with mechanically evoked tinnitus as a new form of complication after hearing preservation cochlear implant surgery. The main goal of this article is to understand the situation better and to transfer the new evidence to peers in order to avoid the complication, to recognize it if present and to propose a possible solution.
Cochlear implantation has become a highly efficient and safe treatment in recent years. According to ten larger studies, which are summarized by Carlson, the overall prevalence of complications is estimated to be around 12% with a prevalence of major complications below 3% (Carlson, Citation2020). Complications related to the electrode array are rare; nevertheless, electrode migration is the second most frequent cause for reimplantation after device failure (Wang et al., Citation2014). Most of the described electrode-related complications are migrations of the intracochlear part of the array leading to a decline in auditory performance or non-acoustic stimulation such as pain, electrical shocks and facial nerve stimulation (Connell et al., Citation2008). It seems that many cases of electrode extrusion can remain undetected (van der Marel et al., Citation2012) and according to one recent study, the rate of electrode extrusion can be as high as 6% (Dietz et al., Citation2016). If the intracochlear array remains well in position, hearing with the implant remains stable. Few cases with exposure of the array in the context of a tympanic retraction, a cholesteatoma formation or at the level of the bony external ear canal have been reported (Mishu et al., Citation2017). These cases typically present with an infectious episode and have been probably observed by many colleagues without having been reported.
The two cases presented in this article are different, as the extrusion across overlaying tissues occurred more laterally at the level of the mastoid cortex, causing a new clinical presentation. The position of the electrodes in the cochlea and the hearing performance remained stable, as confirmed by hearing tests, electrophysiological measurements and computed tomography of the temporal bone. No infectious events occurred at the level of the tympanic or mastoid cavity. Over time, the initially well-covered electrode array worked itself across the musculo-periosteal cover, coming close to the overlaying conchal cartilage (patient 1) or the subcutaneous tissue of the external meatus (patient 2). Laying directly under the mobile external ear, the electrode array itself became mobile. The mechanical movements of the soft tissues of the ear (while turning the head on the pillow, for example) now caused unusual, disturbing sound perceptions for the patient.
We cannot completely rule out the possibility that due to the good residual hearing the friction between the electrode array and the soft tissues could have been perceived as sound by simple air transmission. However, during revision surgery any contact of the electrode array with the ossicular chain could be excluded. In addition, the revision surgery was performed under local anesthesia in one patient and she perceived the slightest touch of the electrode array through the entire repositioning procedure and even after having separated the electrode from soft tissues as a loud and disturbing noise which was not audible to the surgeon.
As usual, the round window membrane incision, as well as the posterior tympanotomy, were secured with free soft tissue grafts. During the revision surgery a small amount of fibrosis, which did not contact the ossicular chain, was observed at this level. This would likely have been unable to prevent micro-movements that could then be transmitted to the cochlear structures. We hypothesize that the sound was actually originating within the inner ear, at least in part, through direct mechanical stimulation of the mechano-transducing elements in the cochlea, probably through a contact of the intracochlear electrode array with the basilar membrane. We believe that the occurrence of a mechanically induced tinnitus may be a warning sign for the integrity of intracochlear structures. The hypothesized proximity between the intracochlear array and the basilar membrane may indicate a mechanical stress prior to penetration of the membrane and loss of residual hearing. Again, this concept remains speculative, as the cone-beam CT scan does not offer a sufficient resolution of the intracochlear compartments to formally prove the assumption.
It is noteworthy to mention that both female patients described here seem to present an anatomical predisposition for extramastoidal electrode migration. Both women have very thin muscles and minimal adipose tissue as well as a relatively wide, almost rolling angle between the mastoid cortex and the external auditory canal, which made it difficult to leave a sufficient bony overhang for visualization of the posterior tympanotomy during initial surgery.
To avoid electrode array extrusion at the level of the mastoid cortex and to avoid the presented complication, the well-known recommendation to secure the array below one or several bony overhangs can only be corroborated based on our experience, particularly in patients with thin musculo-periosteal tissue. In addition, other methods can be used to secure the array at the mastoid surface such as bony bridges, clips, miniplates and non-resorbable sutures, among others, if judged necessary (Alexander et al., Citation2011; Balkany and Telischi, Citation1995; Cohen and Kuzma, Citation1995).
Conclusion
Patients with residual hearing after cochlear implant surgery may present with mechanically evoked tinnitus, if the electrode array has been exposed at the level of the musculo-periosteal or subcutaneous layer of the outer ear region enabling transfer of mechanical energy to the mechano-sensitive inner ear structures. This new complication corroborates an old wisdom, the cochlear implant needs to be immobilized and protected safely in the mastoid cavity under bony overhangs or through artificial fixation methods to avoid well-known and new complications.
Disclaimer statements
Contributors None.
Conflicts of interest None.
Ethics approval None.
Additional information
Funding
Notes on contributors
Lenka Vankatova
Lenka Vankatova - after graduating from the First Faculty of Medicine, Charles University in Prague in 2012. Lenka Vankatova has completed her Otorhinolarygology - Head and Neck Surgery residency (2019) and Phoniatrics fellowship (2022) in the Service of ORL and HNS in Geneva University Hospitals.
Julien Wen Hsieh
Julien Wen Hsieh received his MD degree in 2012 from the University Of Geneva in Switzerland where he worked on human olfaction following nasal surgery and the control of genome expression in yeast cells. In 2013, he carried out an Ear, Nose and Throat (ENT) residency at Luxembourg Hospital Center in Luxembourg. He won the “Junior Scientific Excellence Prize” for the development of a Smell and Taste clinic in Luxembourg to treat chemosensory disorders and promote research in this field. In 2014, he joined the Rockefeller University Hospital in New York (USA) as an instructor in clinical investigation (clinical scholar) at the Vosshall's Laboratory of Neurogenetics and behavior. There, he worked with Andreas Keller and Leslie Vosshall and invented SMELL-RS, a universal smell test that may help diagnose patients with olfactory dysfunction. In 2017, he returned to Geneva to continue his ENT residency at the Geneva University Hospitals (Switzerland) and trained with Basile Landis, an expert in clinical olfaction. In 2019, he was promoted young physician-scientist by the University of Geneva - Faculty of medicine with 50% protected time to conduct research at the bench and patient's bedside. In Pascal Senn's Inner Ear and Olfaction Laboratory, he carried out research on olfactory neuroregeneration to find a cure for patients with post-traumatic smell loss. He received several international awards such as the “European Chemoreception Research Organization Young Investigator Award” in 2018 and the “Clinical olfactory working group - German ENT society Award” in 2019.
Dimitrios Daskalou
Dimitrios Daskalou received his medical degree from the Aristotle University of Thessaloniki School of Medicine, Greece, in 2018, where he also attended a master's program in Medical Research Methodology. He is currently an ENT medical resident in Geneva university hospitals with a primary focus on otology and especially on medical and surgical management of hearing loss.
Pascal Senn
Pascal Senn, MD has graduated from the University of Bern in 1997 and is currently professor and chairman of the Service of ORL, HNS at the University hospitals of Geneva, Switzerland with a clinical focus on ear surgery and cochlear implantation.
References
- Adunka, O.F., Pillsbury, H.C., Buchman, C.A. 2010. Minimizing intracochlear trauma during cochlear implantation. Advances in Otorhino-laryngology, 67: 96–107. Available from: https://doi.org/10.1159/000262601
- Alexander, N.S., Caron, E., Woolley, A.L. 2011. Fixation methods in pediatric cochlear implants: retrospective review of an evolution of 3 techniques. Otolaryngology—Head and Neck Surgery, 144(3): 427–430. Available from: https://doi.org/10.1177/0194599810390336
- Balkany, T., Telischi, F.F. 1995. Fixation of the electrode cable during cochlear implantation: the split bridge technique. The Laryngoscope, 105(2): 217–218. Available from: https://doi.org/10.1288/00005537-199502000-00022
- Carlson, M.L. 2020. Cochlear implantation in adults. New England Journal of Medicine, 382(16): 1531–1542. Available from: https://doi.org/10.1056/NEJMra1904407
- Cohen, N.L., Kuzma, J. 1995. Titanium clip for cochlear implant electrode fixation. The Annals of Otology, Rhinology & Laryngology. Supplement, 166: 402–403. Available from: https://www.ncbi.nlm.nih.gov/pubmed/7668723
- Connell, S.S., Balkany, T.J., Hodges, A.V., Telischi, F.F., Angeli, S.I., Eshraghi, A.A. 2008. Electrode migration after cochlear implantation. Otology & Neurotology, 29(2): 156–159. Available from: https://doi.org/10.1097/MAO.0b013e318157f80b
- Dietz, A., Wennstrom, M., Lehtimaki, A., Lopponen, H., Valtonen, H. 2016. Electrode migration after cochlear implant surgery: more common than expected? European Archives of Oto-rhino-laryngology, 273(6): 1411–1418. Available from: https://doi.org/10.1007/s00405-015-3716-4
- Mishu, C., Klodd, D.A., Redleaf, M. 2017. Cochlear implant electrode array exposure: a delayed complication. Ear, Nose, & Throat Journal, 96(7): E40–E43. Available from: https://doi.org/10.1177/014556131709600708
- Perkins, E., Lee, J., Manzoor, N., O'Malley, M., Bennett, M., Labadie, R., et al. 2021. The reality of hearing preservation in cochlear implantation: who is utilizing EAS? Otology & Neurotology, 42(6): 832–837. Available from: https://doi.org/10.1097/MAO.0000000000003074
- Pfingst, B.E., Zhou, N., Colesa, D.J., Watts, M.M., Strahl, S.B., Garadat, S.N., et al. 2015. Importance of cochlear health for implant function. Hearing Research, 322: 77–88. Available from: https://doi.org/10.1016/j.heares.2014.09.009
- Sargsyan, G., Kanaan, N., Lenarz, T., Lesinski-Schiedat, A. 2021. Comparison of speech recognition in cochlear implant patients with and without residual hearing: a review of indications. Cochlear Implants International, 22(5): 257–264. Available from: https://doi.org/10.1080/14670100.2021.1898111
- van der Marel, K.S., Verbist, B.M., Briaire, J.J., Joemai, R.M., Frijns, J.H. 2012. Electrode migration in cochlear implant patients: not an exception. Audiology & Neuro-otology, 17(5): 275–281. Available from: https://doi.org/10.1159/000338475
- Wang, J.T., Wang, A.Y., Psarros, C., Da Cruz, M. 2014. Rates of revision and device failure in cochlear implant surgery: a 30-year experience. The Laryngoscope, 124(10): 2393–2399. Available from: https://doi.org/10.1002/lary.24649

