ABSTRACT
Background: GEMINI trials demonstrated the therapeutic efficacy of vedolizumab (VDZ) in Crohn’s disease (CD) and ulcerative colitis (UC).
Research design and methods: Aim of this study was to determine the real-life effectiveness of VDZ on endoscopic healing in the Hungarian nationwide cohort of inflammatory bowel disease (IBD) patients based on the changes on clinical and endoscopic scores. Every adult IBD patient in the country (121 UC and 83 CD) who completed the short-term VDZ therapy was enrolled, of which 72 UC and 52 CD patients could complete the long-term therapy.
Results: The rates of endoscopic healing were substantially higher in UC compared with CD patients during the short- and long-term therapy (52.9% vs. 21.7%, p < 0.0001, and 51.4% vs. 21.2%, p = 0.015, respectively). In CD, the rate of endoscopic healing was lower at week 14 compared with week 22 (14.5% vs. 37.0%, p = 0.026). Prior anti-TNF-α therapy (88.73%) was not associated with a significant decrease in therapeutic response. The average disease duration was significantly lower in CD patients achieving endoscopic healing at week 52 (11.75 vs. 5.27 years, p = 0.007).
Conclusions: VDZ therapy is an effective therapeutic option in anti-TNF-α refractory IBD. However, the endoscopic healing rate was substantially lower and showed a significant delay in CD compared with UC.
1. Introduction
Gut-specific vedolizumab (VDZ) is a fully humanized monoclonal antibody that specifically blocks α4β7 integrin, inhibiting adhesion and migration of leukocytes into the damaged intestinal mucosa. Previous randomized controlled trials demonstrated that VDZ has comparable therapeutic efficacy with tumor necrosis factor-α (TNF-α), blockers infliximab (IFX), and adalimumab (ADA) in both Crohn’s disease (CD) and ulcerative colitis (UC) but the only head-to-head comparison was made in the VARSITY trial [Citation1–Citation5]. In this trial, vedolizumab was superior to adalimumab in terms of achievement of clinical remission and endoscopic improvement in patients with moderately to severely active ulcerative colitis. LOVE-CD study verified that endoscopic remission (SES-CD score <4) was achievable in one-third of CD patients by week 52; in addition, the rate of histologic remission by week 26 was 64% [Citation6]. Nonetheless, in most countries, VDZ is frequently used as second-line therapy in patients with anti-TNF-α refractory disease.
In Hungary, VDZ has become an alternative option in the management of moderate and severe IBD since 2016, but the high treatment costs are currently limiting its availability. By 2019, all newly prescribed VDZ had to be based on an individualized treatment decision and approved by the steering committee of five Hungarian IBD-specialists. Because of this, only patients with long-standing disease showing inadequate response to conventional anti-TNF-α and/or immunosuppressant therapies could receive VDZ treatment. Only patients with relevant comorbidities (past medical history of cancer or tuberculosis, severe heart failure, chronic hepatitis B or C viral infection, etc.) and hence not candidates for other therapeutic options were eligible for VDZ treatment. Although several studies assessing VDZ effectiveness in real-life setting have been published, fewer data on its effect on endoscopic healing is available. Therefore, the aim of this observational study was to assess the effectiveness of short- and long-term VDZ treatment on IBD endoscopic healing in real-life setting.
2. Patients and methods
2.1. Patient enrollment, study protocol
This was a noninterventional, observational, multicenter cohort study using prospectively collected clinical records of all adult IBD patients in Hungary with moderate and severe disease activity who received and completed short-term VDZ therapy between July 2016 and December 2018. Concomitant immunosuppressant and corticosteroid treatment were allowed at inclusion, but combination therapy with another biological agent was not permitted. All enrolled patients received 300 mg VDZ as an intravenous infusion at 0, 2, and 6 weeks followed by an every-8-week maintenance regimen.
Study protocol was approved by the Regional and Institutional Human Medical Biological Research Ethics Committee of the University of Szeged (clinical trial registration number: 99/2017-SZTE). The study was carried out under the Declaration of Helsinki.
2.2. Response evaluation
The therapeutic response was assessed based on changes in clinical (Crohn’s Disease Activity Index [CDAI], Mayo score) and endoscopic (Simple Endoscopic Score for Crohn’s Disease [SES-CD], endoscopic Mayo score) activity scores. Clinical response was defined as a >3-point decrease in total Mayo score or a >100-point decrease in CDAI score from baseline. Remission was defined as Mayo score ≤2, with no individual subscores >1, or as CDAI score ≤150. Colonoscopy for endoscopic activity evaluation was performed immediately before therapeutic request submission and control examinations before initiation of maintenance and second-year therapies. Endoscopic healing was defined as Mayo endoscopic subscore ≤1 or SES-CD score ≤4.
The primary study endpoint was endoscopic healing rate by the end of short- and long-term VDZ treatment, based on endoscopic findings and scores. After September 2017, the timing of control examinations was changed due to modified Hungarian health insurance VDZ funding, which required a change in the definition of short-term efficacy. Before September 2017, it was defined as a therapeutic response to VDZ treatment at week 14. After this date, short-term efficacy assessment has been performed following the third VDZ infusion in UC and the fifth infusion in CD. Long-term therapeutic response was evaluated after the first year of treatment, at week 52. The co-primary study endpoint was determination of short- and long-term therapeutic response to VDZ. Patients’ clinical data were collected using the Hungarian IBD-specialist committee database, which is based on therapeutic request forms. Information about suspended treatments was provided by the physicians of IBD patients.
The secondary study endpoint was identification of potential predictors of therapeutic response and assessment of the impact of concomitant medication use on short- and long-term outcomes of VDZ treatment. Correlations between VDZ trough level (TL) changes, laboratory parameters (hematocrit [HCT], hemoglobin [HGB], C-reactive protein [CRP], white blood cell [WBC], platelet count [PLT]), and therapeutic response during follow-up were further examined.
Serum VDZ and antibody levels were evaluated during maintenance therapy. For that purpose, blood samples were collected immediately before regular VDZ infusion (TL) administration. Serum samples were tested by quantitative enzyme-linked immunosorbent assay (ELISA) with LISA-TRACKER Duo Vedolizumab (Theradiag, France). VDZ-TLs and anti-VDZ antibodies are quantified using a specific biotinylated antibody directed against the idiotype of VDZ, and a biotinalyted VDZ against anti-VDZ antibody. The assay range for VDZ-TL is between 2 μg/mL and 60 μg/mL, and anti-VDZ is between 35 ng/mL and 500 ng/mL.
2.3. Statistical analysis
Statistical tests were performed using R statistical software version 3.6.0 (R Foundation) and SPSS software version 24 (SPSS Inc., Chicago, Illinois, USA), with p < 0.05 considered statistically significant. Chi-squared and Fisher’s exact tests were applied to compare categorical variables, and t-test was used to compare continuous variables between groups. Depending on the results of Levene’s test for homogeneity of variances, one-way analysis of variance and Tukey’s honest significant difference or Dunnett’s T3 post hoc test were used to compare laboratory parameters. Paired t-test was applied to evaluate mean changes in clinical and endoscopic activity indices during short and long-term treatment. Missing data were imputed using the last observation carried forward approach. Q–Q plot (quantile–quantile plot) and density plot were used for checking normality of data visually. Disease duration cutoff was determined by receiver operating characteristic (ROC) curve analysis, using endoscopic healing as a classification variable to calculate the area under the ROC curve.
3. Results
3.1. Patient baseline characteristics
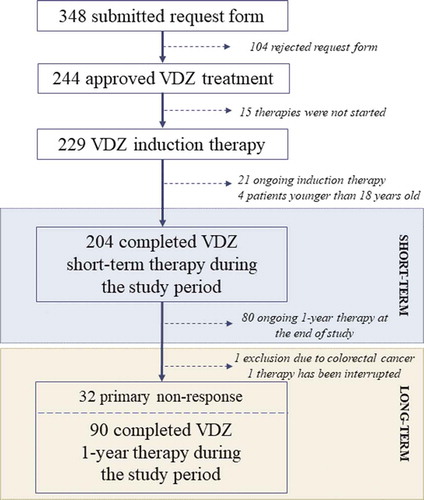
A total of 348 VDZ therapeutic application requests were submitted between July 2016 and December 2018 in Hungary, from which 244 (70.11%) were approved (). VDZ treatment eventually did not start in 15 cases because of earlier therapeutic switching or surgical interventions required due to severe disease activity. Twenty-one patients with ongoing short-term therapy and four pediatric IBD patients were excluded from the study. All 204 enrolled cases (121 UC and 83 CD) had completed short-term VDZ treatment. Although in 124 cases (60.78%; 72 UC and 52 CD) the 1-year treatment could potentially be finished during the study period, maintenance treatment was not approved in 32 cases (25.8%) due to primary nonresponse. One patient moved to abroad, therefore VDZ therapy was interrupted, and in one case, colorectal cancer was found by control endoscopy at week 14. Ninety patients (58 UC and 32 CD) received VDZ maintenance therapy. summarizes the clinical and demographical data of enrolled IBD patients. The average disease duration was 10.04 ± 7.40 years, being less than 3 years only in 26 cases (12.75%). A total of 181 patients (88.73%) received previous anti-TNF-α therapy (80.88% IFX; 71.08% ADA; 1.47% golimumab). A switch to another anti-TNF-α or to VDZ was required in 43 cases of primary nonresponse and in 192 cases of response loss. Adverse events were observed in 67 cases, the most frequent being infusion reactions (N = 42; 20.59%), infections (N = 5; 2.45%), reactivation of tuberculosis (N = 3; 1.47%), and hematological effects (N = 3; 1.47%). Only 23 patients (11.27%) were naïve to anti-TNF-α inhibitors: in 7 cases, past medical history of malignancy contraindicated the use of these agents; in 7 and 4 cases, severe comorbidities and high risk for infections (cystic fibrosis, renal transplantation), respectively, required the use of gut-selective biological agents; and 5 patients were young (<20 years old) with newly diagnosed, severely active IBD.
Table 1. Clinical and demographic data of enrolled inflammatory bowel disease patients.
3.2. Endoscopic healing
Significant differences in endoscopic healing rates were observed between UC and CD subgroups by the end of short- and long-term therapy (52.9% vs. 21.7%, p < 0.0001, and 51.4% vs. 21.2%, p = 0.015, respectively). Clinical response and mucosal regeneration during VDZ treatment are very fast in UC, which was supported by the fact that the proportion of partial or complete endoscopic healing detected by control colonoscopy after the third (week 6) and fourth (week 14) infusions did not substantially differ (44.19% vs. 57.69%, p = 0.185). In CD, although lower rates of endoscopic healing were not observed, healing rates were significantly delayed compared with UC, with substantial endoscopic healing differences detected by weeks 14 and 22 (14.5% vs. 37.0%, p = 0.026). At the end of short-term therapy, none of the examined clinical or demographical data predicted therapy outcomes on endoscopic healing; however, in CD, the average disease duration was significantly lower in patients achieving complete endoscopic remission compared with patients not achieving endoscopic healing (11.75 vs. 5.27 years, p = 0.007). () ()
Figure 2. (a) This is a half violin with each observation records displayed in dots. In Crohn’s disease, the average disease duration was significantly higher in patients with complete endoscopic remission compared with patients without endoscopic healing during long-term vedolizumab therapy (11.75 vs. 5.27, p < 0.007). (b) ROC curve shows 83.9% of patients correctly attributed to the endoscopic healing group using 6.5-year disease duration cutoff.
Table 2. Assessment of endoscopic healing predictors during short- and long-term vedolizumab therapy (L, location of disease; L1, ileal; L2, colonic; L3, ileocolonic; B, behavior of disease; B1, inflammatory; B2, stricturing; B3, penetrating; 5-ASA, 5-amino-salicilate; anti-TNF-α, anti-tumor necrosis factor-α).
Average endoscopic activity index values significantly dropped during the study period compared with baseline: in UC, the mean eMayo score decreased from 2.80 to 1.41 by the end of short-term treatment and to 1.40 at week 52 (p < 0.0001); in CD, mean SES-CD decreased from 20.89 (95% CI, 16.52–25.26) to 13.48 (95% CI, 9.09–17.86) at weeks 14–22 in the short-term subgroup and from 19.49 (95% CI, 17.07–21.91) to 12.80 (95% CI, 10.11–15.50) at week 52 (p < 0.0001).
3.3. Therapeutic response
By the end of short-term VDZ therapy, the rate of clinical response was substantially higher in the UC compared with CD subgroup (84.30% vs. 61.45%; p < 0.0001), but this difference lost by week 52 (65.28% vs. 42.31%; p = 0.307). No significant differences were found in the proportion of clinical remission and steroid-free remission between UC and CD subgroups by the end of short-term treatment (49.59% vs. 51.81%, p = 0.777, and 27.27% vs. 37.35%, p = 0.167, respectively) or at 1-year follow-up (47.22% vs. 32.69%, p = 0.825, and 44.44% vs. 30.77%, p = 0.826, respectively) (). Modification in the definition of short-term efficacy did not result in a substantial change in VDZ clinical response rate, either in UC (at week 6 [N = 43] vs. at week 14 [N = 78]) or CD (at week 14 [N = 56] vs. at week 22 [N = 27]) subgroup (83.72% vs. 84.62%, p = 1.000, and 58.93% vs. 66.67%, p = 0.6615, respectively). By the end of short-term VDZ treatment, steroids could be tapered and ceased in 52.46% of patients receiving systemic corticosteroids at inclusion, with this rate increasing to 68.13% at 1-year follow-up. Mean activity scores significantly decreased during follow-up compared with baseline (). Neither disease duration and phenotype nor concomitant medication (azathioprine, cyclosporine A, methotrexate, or systemic corticosteroid) uses influenced short- and long-term VDZ outcomes, and previous anti-TNF-α treatment was not associated with higher risk of primary nonresponse.
Figure 3. Short- and long-term efficacy of vedolizumab therapy on clinical response, remission, steroid-free remission, and endoscopic healing (UC, ulcerative colitis; CD, Crohn’s disease).
Figure 4. (a–b) Mean Crohn’s Disease Activity Index (CDAI: in short-term subgroups 303.58 [95% CI, 289.59–317.57] vs. 157.66 [95% CI, 145.80–189.52] and in long-term subgroup CDAI: 309.67 [95% CI, 294.83–324.52] vs. 172.65 [95% CI, 145.32–199.99] vs. 184.08 [95% CI, 154.61–213.54]) and Mayo score (in short-term subgroup 9.74 [95% CI, 9.48–9.99] vs. 4.33 [95% CI, 3.82–4.84] and in long-term subgroups 9.60 [95% CI, 9.24–9.95] vs. 4.38 [95% CI, 3.51–4.80] vs. 4.38 [95% CI, 3.61–5.14]) significantly decreased during short- and long-term vedolizumab therapy compared with baseline. (c) Mean Simple Endoscopic Score for Crohn’s Disease (SES-CD) significantly decreased from 20.89 (95% CI, 16.52–25.26) to 13.48 (95% CI, 9.09–17.86) in short-term subgroup and from 19.49 (95% CI, 17.07–21.91) to 12.04 (95% CI, 9.54–14.54) by the end of short-term and to 12.80 (95% CI, 10.11–15.50) by the end of long-term vedolizumab therapy in the long-term subgroup. (d) Percentage component bar chart shows the distribution of different endoscopic Mayo (eMayo) scores in the study population at baseline and at the end of short- and long-term vedolizumab treatment.
![Figure 4. (a–b) Mean Crohn’s Disease Activity Index (CDAI: in short-term subgroups 303.58 [95% CI, 289.59–317.57] vs. 157.66 [95% CI, 145.80–189.52] and in long-term subgroup CDAI: 309.67 [95% CI, 294.83–324.52] vs. 172.65 [95% CI, 145.32–199.99] vs. 184.08 [95% CI, 154.61–213.54]) and Mayo score (in short-term subgroup 9.74 [95% CI, 9.48–9.99] vs. 4.33 [95% CI, 3.82–4.84] and in long-term subgroups 9.60 [95% CI, 9.24–9.95] vs. 4.38 [95% CI, 3.51–4.80] vs. 4.38 [95% CI, 3.61–5.14]) significantly decreased during short- and long-term vedolizumab therapy compared with baseline. (c) Mean Simple Endoscopic Score for Crohn’s Disease (SES-CD) significantly decreased from 20.89 (95% CI, 16.52–25.26) to 13.48 (95% CI, 9.09–17.86) in short-term subgroup and from 19.49 (95% CI, 17.07–21.91) to 12.04 (95% CI, 9.54–14.54) by the end of short-term and to 12.80 (95% CI, 10.11–15.50) by the end of long-term vedolizumab therapy in the long-term subgroup. (d) Percentage component bar chart shows the distribution of different endoscopic Mayo (eMayo) scores in the study population at baseline and at the end of short- and long-term vedolizumab treatment.](/cms/asset/a7528e80-d6fb-416c-a324-1cc19048095c/iebt_a_1699529_f0004_oc.jpg)
Only one patient had adverse, mild allergy-like reaction during the second VDZ infusion which required systemic corticosteroid and antihistamine administration before the following three VDZ infusions. VDZ therapy was suspended after the short-term treatment due to primary non-response. In one case, cytomegalovirus infection was observed during induction therapy, but presumably this infection had been acquired before initiation of VDZ.
3.4. Laboratory parameters and VDZ trough levels
Serum CRP levels, PLT counts, and HGB concentrations were checked before the initiation of long-term therapy, and their role in clinical response was investigated. CRP was significantly higher in short-term VDZ responders compared with primary nonresponders. In CD, clinical response was associated with a significant change in average PLT values, but this decrease was not detected in UC. HGB levels were independent of clinical response. ()
Figure 5. Serum C-reactive protein (CRP) decreases during short-term vedolizumab (VDZ) therapy was significantly higher in clinical responders compared with nonresponders. However, correlation between platelet count (PLT) and clinical response was only observed in Crohn’s disease (CD). Hemoglobin levels did not significantly differ between responders and nonresponders by the end of short-term treatment. (UC, ulcerative colitis).
VDZ antibodies were not detected in any of the 54 examined (47 nonresponders and 7 responders) cases. VDZ-TL measurements were performed in 47 cases of during maintenance therapy (41 responders and 6 nonresponders). No correlation was found between VDZ-TLs and either clinical response or endoscopic healing. Mean VDZ-TL values were higher in nonresponders compared with responders (35.32 μg/mL vs 21.73 μg/mL) and in patients not achieving compared with those achieving endoscopic healing (25.95 μg/mL vs. 20.39 μg/mL). shows clinical response and endoscopic healing according to 15 μg/mL VDZ-TL cutoff.
Table 3. Correlation between therapeutic response and vedolizumab trough (VDZ-TL) levels using 15 μg/mL cutoff value.
4. Discussion
The present multicenter cohort study assessed the effectiveness of VDZ therapy on endoscopic healing in moderate and severe active IBD. The most important advantage of this investigation is that it involved all patients receiving VDZ treatment in the entire country. In addition, VDZ special regulations and health insurance funding—which required confirmation of therapeutic response by endoscopic examination—allowed evaluation, not only of clinical response but also of endoscopic healing in real-life setting. The strict, two-phase VDZ approval process can be considered as both an advantage and disadvantage of the study, as it resulted in the selection of a particularly difficult-to-treat population with long-standing anti-TNF-α and/or immunosuppressant resistant disease. At the same time, our results cannot be generalized, and might not be applied to other countries, where VDZ is available as first-line treatment and can also be applied in patients who have better prognostic factors.
The results of this study suggest that both short-term and 1-year long-term maintenance VDZ therapy is an effective and safe therapeutic option in this difficult-to-treat population. However, significant differences were observed between UC and CD subgroups in terms of therapeutic effectiveness. Lower and delayed therapeutic response was achieved in CD compared with UC, which was evident also in the lower endoscopic healing rate. This observation correlates with the results of most previously published studies [Citation5,Citation7]. The GEMINI 1 and 2 randomized controlled trials found substantially greater response and remission rates in UC compared with CD, both at week 6 (47.1% and 16.9% vs. 31.4% and 14.5%) and week 52 (56.6% and 41.8% vs. 39.0% and 43.5%) [Citation1,Citation3]. In addition, Sands et al. found that VDZ was not more effective than placebo on clinical remission at week 6 among patients with TNF antagonist-refractory CD. In this case, therapeutic benefits were detectable only after week 10 [Citation8]. The reason for the therapeutic response difference between CD and UC patients is still not clearly understood, but it may be presumably related with the transmural nature of CD and mechanism of action of VDZ. VDZ is a gut-specific antibody against α4β7 integrin, which is expressed on the surface of mononuclear cells such as T-lymphocytes. This integrin binds to mucosal addressing cell adhesion molecule-1 (MAdCAM.1) expressed by the endothelial cells in venules within the gastrointestinal tract and on high endothelial venules in gut-associated lymphoid tissue, including Peyer’s patches and mesenteric lymph nodes [Citation9,Citation10]. Th1-cells promote the proliferation of mononuclear phagocytes, neutrophil granulocytes, and the maturation of M1 proinflammatory macrophages and natural killer (NK) cells, which leads to colonic epithelial damage in IBD [Citation11]. VDZ by blocking the α4β7 integrin inhibits adhesion and migration of T-cells into the damaged intestinal mucosa. Some authors assume that VDZ may be less effective in cases of deep mural inflammation due to mechanism of action [Citation12]. In contrast with this hypothesis, some recently published studies found no difference in VDZ effectiveness among UC and CD patients [Citation13,Citation14].
In our UC patient cohort, endoscopic remission was achievable in every second case during short-term and every third case during long-term treatment; however, in cases of CD, the rate of endoscopic remission was significantly lower compared with UC, about 20% at both checkpoints. This is partly similar to the results of a recently published Belgian real-life, retrospective observational study in which 56.1% of UC and 39.1% of CD patients achieved the endoscopic endpoint [Citation15]. In most clinical trials, the endoscopic remission rate in CD was almost twice as high as our results that can be explained by the fact that only difficult-to-treat patients could receive vedolizumab in our cohort who showed primary non-response or loss-of-response to at least one biological agent and/or immunomodulator [Citation6,Citation15–Citation17]. The post hoc analysis of GEMINI 1 and 2 trials suggested that previous medication, especially prior biological therapy, substantially influenced VDZ effectiveness, with VDZ appearing to have greater benefits in anti-TNF-α-naïve IBD patients when effectiveness and health-related quality of life indicators were assessed [Citation2,Citation18,Citation19]. Nonetheless, among patients who responded to VDZ induction therapy at week 6, a high percentage remained on maintenance therapy and achieved remission by week 104 regardless of prior anti-TNF-α exposure, with no considerable differences between UC and CD in this regard (88% and 83%, respectively) [Citation20,Citation21]. Similar results have been recently reported by Swedish (SWIBREG), Finnish (FINVEDO), Japanese, British (REVIVE), and Scottish nationwide cohort studies, among others [Citation13,Citation22–Citation25]. In the Hungarian cohort, prior anti-TNF-α exposure was not associated with lower clinical response rates by the end of short-term VDZ therapy; however, the anti-TNF-α-naïve sample size may have been too small to detect a statistically significant difference. In addition, concomitant azathioprine, cyclosporine, and systemic corticosteroid therapy were not associated with an increased benefit, in contrast with results from GEMINI 2 and 4 and other studies [Citation26–Citation29].
The highest effectiveness of VDZ therapy can be achieved when it is used as a first-line agent shortly after the onset of disease in patients who failed conventional therapies, such as immunosuppressants, 5-aminosalicylates, cyclosporine, and corticosteroids [Citation30–Citation32]. In these cases, the therapeutic effect of VDZ and other biologics is almost the same in UC and CD, and VDZ fistula closure rate is close to that of IFX and ADA [Citation33]. Post hoc analysis of GEMINI 2 detected 28% of fistula closure rate at week 14 and 33% at week 52 with VDZ treatment [Citation34]. However, a retrospective study by Yamada et al. found a higher postoperative endoscopic recurrence in CD with VDZ than with anti-TNF-α agents [Citation35]. In this study, the low number of perianal CD did not allow assessment of VDZ effectiveness on fistula healing. However, no differences were found in clinical response and mucosal healing rates between anti-TNF-α-refractory and -naïve IBD patients.
Contradictory data about the clinical relevance of VDZ-TL and VDZ-directed antibody measurements exist. Pouillon et al., Yacoub et al., and Hanžel et al. found that histological healing is associated with higher VDZ-TL during maintenance therapy in UC, and the 18–25 μg/mL TL threshold proved to be optimal in predicting histological healing [Citation36–Citation38]. A meta-analysis published in 2019, which assessed the results of five cohort studies, concluded that VDZ concentration >20 μg/mL at week 6, and >12 μg/mL during maintenance may be associated with better outcomes [Citation39]. In contrast, the study by Al-Bawardy et al. did not detect an association between VDZ-TL and mucosal healing [Citation40]. GEMINI long-term safety study found that antibodies against VDZ developed in only 5% of patients, and there was no relationship between immunogenicity and safety [Citation41]. In this study, VDZ-TL showed no correlation with clinical response or mucosal healing, and antibody formation against VDZ was not detectable in any case.
The most important limitation of this study is the fact that it is a noninterventional, observational trial with open-label design and no control groups. Enrolled patients were from different institutions, and as such, some heterogeneity in clinical response and endoscopic activity assessment may exist. On the other hand, this also represents the real-life nature of the study. Only therapeutic efficacy of VDZ on clinical activity and endoscopic healing was determined, and the effect of VDZ therapy for extraintestinal manifestations and perianal activity of CD was not evaluated. The measurement of VDZ trough levels and antibody against VDZ were available only in two clinical centers, so they are not representative for the whole study population. Therefore, it allowed only to assess whether measurement of these parameters helped to determine the therapeutic response.
5. Conclusion
This study confirms that both short-term and first-year maintenance VDZ therapy is a safe and effective therapeutic option in anti-TNF-α failing or intolerant IBD patients with moderate or severe disease activity, with no significant differences observed between UC and CD subgroups. Endoscopic healing was achieved in half of UC and only a fifth of CD patients by the end of the two evaluation time points in this difficult-to-treat population. As disease duration is an important predictive factor of endoscopic healing in CD, the optimal effect of VDZ in this population may be achieved with early therapy, starting less than 5 years after disease diagnosis. In addition, due to delayed response, evaluation of VDZ therapeutic effect is not yet possible after induction therapy. VDZ-TL measurement did not help to predict therapeutic response and endoscopic healing.
Author contributions
Conception and design of the study, supervision of patient selection: Bor R, Molnár T, Miheller P, Vincze Á, Szamosi T, Palatka K. Acquisition of data: Bor R, Fábián A, Szepes Z, Farkas K, Rutka M, Szántó K, Zsigmond F, Bálint A, Nagy F, Milassin Á, Tóth T, Zsigmond F, Bajor J, Lakner L, Müllner K, Papp M, Salamon Á, Horváth G, Sarang K, Schäfer E, Sarlós P.
Drafting of the manuscript: Bor R, Fábián A, Szepes Z, Molnár T. Critical revision for important intellectual content: Szepes Z, Vincze Á, Miheller P, Palatka K, Molnár T. Analysis and interpretation of data: Matuz M, Bor R. All authors have approved the final draft submitted.
Declaration of interest
The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial relationships or otherwise to disclose.
Additional information
Funding
References
- Sandborn WJ, Feagan BG, Rutgeerts P, et al. Vedolizumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2013;369(8):711–721.
- Feagan BG, Patel H, Colombel J-F, et al. Effects of vedolizumab on health-related quality of life in patients with ulcerative colitis: results from the randomised GEMINI 1 trial. Aliment Pharmacol Ther. 2017;45(2):264–275.
- Feagan BG, Rutgeerts P, Sands BE, et al. Vedolizumab as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2013;369(8):699–710.
- Sands BE, Peyrin-Biroulet L, Loftus EV, et al. Vedolizumab versus adalimumab for moderate-to-severe ulcerative colitis. N Engl J Med. 2019;381(13):1215–1226.
- Amiot A, Serrero M, Peyrin-Biroulet L, et al. One-year effectiveness and safety of vedolizumab therapy for inflammatory bowel disease: a prospective multicentre cohort study. Aliment Pharmacol Ther. 2017;46(3):310–321.
- Löwenberg M, Vermeire S, Mostafavi N, et al. Vedolizumab induces endoscopic and histologic remission in patients with Crohn’s disease. Gastroenterology. 2019;157(4):997–1006.e6.
- Chaparro M, Garre A, Ricart E, et al. Short and long-term effectiveness and safety of vedolizumab in inflammatory bowel disease: results from the ENEIDA registry. Aliment Pharmacol Ther. 2018;48(8):839–851.
- Sands BE, Feagan BG, Rutgeerts P, et al. Effects of vedolizumab induction therapy for patients with Crohn’s disease in whom tumor necrosis factor antagonist treatment failed. Gastroenterology. 2014;147(3):618–627.e3.
- McLean LP, Cross RK. Pharmacodynamic assessment of vedolizumab for the treatment of ulcerative colitis. Expert Opin Drug Metab Toxicol. 2016;12(7):833–842.
- Rogler G. Mechanism of action of vedolizumab: do we really understand it? Gut. 2019;68(1):4–5.
- Zundler S, Neurath MF. Immunopathogenesis of inflammatory bowel diseases: functional role of T cells and T cell homing. Clin Exp Rheumatol. n.d.;33(4 Suppl 92):S19–28.
- Lam MC, Bressler B. Vedolizumab for ulcerative colitis and Crohn’s disease: results and implications of GEMINI studies. Immunotherapy. 2014;6(9):963–971.
- Eriksson C, Marsal J, Bergemalm D, et al. Long-term effectiveness of vedolizumab in inflammatory bowel disease: a national study based on the Swedish National Quality Registry for Inflammatory Bowel Disease (SWIBREG). Scand J Gastroenterol. 2017;52(6–7):722–729.
- Shelton E, Allegretti JR, Stevens B, et al. Efficacy of vedolizumab as induction therapy in refractory IBD patients. Inflamm Bowel Dis. 2015;21(12):2879–2885.
- Verstockt B, Mertens E, Dreesen E, et al. Influence of drug exposure on vedolizumab-induced endoscopic remission in anti-TNF naïve and anti-TNF exposed IBD patients. J Crohns Colitis. 2019;pii: jjz151. DOI:10.1093/ecco-jcc/jjz151.
- Kotze PG, Ma C, Almutairdi A, et al. Real-world clinical, endoscopic and radiographic efficacy of vedolizumab for the treatment of inflammatory bowel disease. Aliment Pharmacol Ther. 2018;48(6):626–637.
- Arijs I, De Hertogh G, Lemmens B, et al. Effect of vedolizumab (anti-α4β7-integrin) therapy on histological healing and mucosal gene expression in patients with UC. Gut. 2018;67(1):43–52.
- Feagan BG, Rubin DT, Danese S, et al. Efficacy of vedolizumab induction and maintenance therapy in patients with ulcerative colitis, regardless of prior exposure to tumor necrosis factor antagonists. Clin Gastroenterol Hepatol. 2017;15(2):229–239.e5.
- Sands BE, Sandborn WJ, Van Assche G, et al. Vedolizumab as induction and maintenance therapy for Crohnʼs disease in patients naïve to or who have failed tumor necrosis factor antagonist therapy. Inflamm Bowel Dis. 2017;23(1):97–106.
- Vermeire S, Loftus EV, Colombel J-F, et al. Long-term efficacy of vedolizumab for Crohn’s disease. J Crohn’s Colitis. 2016;109(4):jjw176.
- Loftus EV, Colombel J-F, Feagan BG, et al. Long-term efficacy of vedolizumab for ulcerative colitis. J Crohn’s Colitis. 2016;11(4):jjw177.
- Ylisaukko-Oja T, Aaltonen J, Nuutinen H, et al. High treatment persistence rate and significant endoscopic healing among real-life patients treated with vedolizumab - a finnish nationwide inflammatory bowel disease cohort study (FINVEDO). Scand J Gastroenterol. 2018;53(2):158–167.
- Motoya S, Watanabe K, Ogata H, et al. Vedolizumab in Japanese patients with ulcerative colitis: a phase 3, randomized, double-blind, placebo-controlled study. PLoS One. 2019;14(2):e0212989.
- Cummings F, Gaya DR, Levison S, et al. A retrospective observational study of early experiences of vedolizumab treatment for inflammatory bowel disease in the UK. Medicine (Baltimore). 2019;98(9):e14681.
- Plevris N, Chuah CS, Allen RM, et al. Real-world effectiveness and safety of vedolizumab for the treatment of inflammatory bowel disease: the scottish vedolizumab cohort. J Crohn’s Colitis. 2019;13:1111–1120.
- Allegretti JR, Barnes EL, Stevens B, et al. Predictors of clinical response and remission at 1 year among a multicenter cohort of patients with inflammatory bowel disease treated with vedolizumab. Dig Dis Sci. 2017;62(6):1590–1596.
- Szántó K, Molnár T, Farkas K. New promising combo therapy in inflammatory bowel diseases refractory to anti-TNF agents: cyclosporine plus vedolizumab. J Crohn’s Colitis. 2018;12(5):629.
- Sands BE, Van Assche G, et al. Vedolizumab in combination with corticosteroids for induction therapy in Crohn’s disease: a post hoc analysis of GEMINI 2 and 3. Inflamm Bowel Dis. 2019;25(8):1375–1382.
- Danese S, Sandborn WJ, Colombel J-F, et al. Endoscopic, radiologic, and histologic healing with vedolizumab in patients with active Crohn’s disease. Gastroenterology. 2019;157(4):1007–1018.e7.
- Hanauer SB, Feagan BG, Lichtenstein GR, et al. Maintenance infliximab for Crohn’s disease: the ACCENT I randomised trial. Lancet. 2002;359(9317):1541–1549.
- Colombel J, Sandborn WJ, Rutgeerts P, et al. Adalimumab for maintenance of clinical response and remission in patients with Crohn’s disease: the CHARM trial. Gastroenterology. 2007;132(1):52–65.
- Sandborn WJ, van Assche G, Reinisch W, et al. Adalimumab induces and maintains clinical remission in patients with moderate-to-severe ulcerative colitis. Gastroenterology. 2012;142(2):257–265.e3.
- Sands BE, Blank MA, Diamond RH, et al. Maintenance infliximab does not result in increased abscess development in fistulizing Crohn’s disease: results from the ACCENT II study. Aliment Pharmacol Ther. 2006;23(8):1127–1136.
- Feagan BG, Schwartz D, Danese S, et al. Efficacy of vedolizumab in fistulising Crohn’s disease: exploratory analyses of data from GEMINI 2. J Crohns Colitis. 2018;12(5):621–626.
- Yamada A, Komaki Y, Patel N, et al. The use of vedolizumab in preventing postoperative recurrence of Crohn’s disease. Inflamm Bowel Dis. 2018;24(3):502–509.
- Pouillon L, Rousseau H, Busby-Venner H, et al. Vedolizumab trough levels and histological healing during maintenance therapy in ulcerative colitis. J Crohn’s Colitis. 2019;13(8):970–975.
- Yacoub W, Williet N, Pouillon L, et al. Early vedolizumab trough levels predict mucosal healing in inflammatory bowel disease: a multicentre prospective observational study. Aliment Pharmacol Ther. 2018;47(7):906–912.
- Hanžel J, Sever N, Ferkolj I, et al. Early vedolizumab trough levels predict combined endoscopic and clinical remission in inflammatory bowel disease. United Eur Gastroenterol J. 2019;7(6):741–749.
- Singh S, Dulai PS, Vande Casteele N, et al. Systematic review with meta-analysis: association between vedolizumab trough concentration and clinical outcomes in patients with inflammatory bowel diseases. Aliment Pharmacol Ther. 2019;50(8):848–857.
- Al-Bawardy B, Ramos GP, Willrich MAV, et al. Vedolizumab drug level correlation with clinical remission, biomarker normalization, and mucosal healing in inflammatory bowel disease. Inflamm Bowel Dis. 2019;25(3):580–586.
- Wyant T, Yang L, Lirio R, et al. P441 long-term immunogenicity of vedolizumab in ulcerative colitis and Crohn’s disease (GEMINI programme). J Crohn’s Colitis. 2019;13(Supplement_1):S331–S331.