1. Introduction
Because one of the functions of the immune system is to protect against tumors [Citation1], the occurrence of cancer could be a reflection of an improperly functioning immune system. While this has been the prevailing paradigm for decades, this now has changed. Tumor cells have different ways to escape attack by the immune system. One way is by preventing detection by T-lymphocytes through downregulating MHC molecules expressed on the cell membrane [Citation2,Citation3]. Another way is by inhibiting activation of the immune system, such as through the expression of a PD-1 ligand (PD-L1), which prevents the activation of tumor infiltrating T-lymphocytes (TILs) [Citation3]. Immunotherapy directed against the blockade of checkpoint inhibitors would prevent this mode of inhibition and thereby allow for the generation of an effective anti-tumor response by the host.
Indeed, it has been shown that treatment of melanoma [Citation4], non-small cell lung carcinoma [Citation5], or cervical carcinoma patients [Citation6] with the anti-PD-1 antibodies pembrolizumab or nivolumab is effective in allowing the host immune system to eradicate the tumor. A combination therapy with antibodies directed against CTLA-4 (ipilimumab) increases the effect [Citation7,Citation8]. Anti-PD-1 therapy has also been combined with other checkpoint inhibitors such as CD134 and CD137 [Citation9]. To illustrate, anti-CTLA-4 and anti-PD-1 therapy has been associated with an increase of TILs with a specificity against mutant neopeptides [Citation10–Citation12] and an augmented presentation and recognition of mutant neopeptides by T-lymphocytes [Citation13].
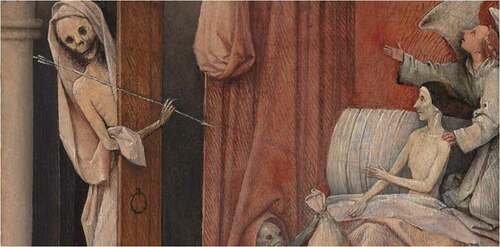
1.1. Death and the Miser
The somewhat miserly characteristics of tumor cells and the ruthlessness of the immune system, once properly activated, may, in a way, resemble the medieval theory memento mori (Latin: ‘remember that you have to die’). Jheronimus Bosch, a Dutch painter from the late 15th century, visualized this theme in this ‘Death and the Miser’ painting, where the Miser lies in his bed when Death knocks at the door (). It is crystal clear for whom Death has come, however, the Miser tries to escape, or, at least, delay Death. Jheronimus Bosch provides the Miser with two options: to call to God for help with the assistance of an Angel, or to try and pay-off Death by offering money, assisted by a Devil. Near the end of the fifteenth century, this theme was popular and inspired by the book Ars Moriendi (Latin: ‘the Art of Dying’) [Citation14]. The second chapter of Ars Moriendi describes the five temptations of a dying man: lack of faith, despair, impatience, spiritual pride, and greed. For the Miser, the last temptation must have hurt most. If we would consider the Miser to be the tumor cell and Death the attack of the immune system, none of the five temptations would be helpful. Ars Moriendi does not provide the recipe to become immune to death.
Figure 1. Death and the Miser painted by Jheronimus Bosch between 1485 and 1490. It is part of a divided triptych that also include ‘The Ship of Fools’ and ‘Allegory of Gluttony and Lust’. National Gallery of Art, Washington, D.C Source Wikimedia Commons. https://commons.wikimedia.org/wiki/Death_and_the_Miser_by_Hieronymus_Bosch, accessed 26 June 2019.
2. Gut microbiota influence the response to checkpoint inhibition immunotherapy
Last year, a series of three independent papers were published in Science on the apparent influence of the gut microbiota on the effectivity of checkpoint inhibition immunotherapy in cancer. Dysregulation of the gut microbiome was already known to be associated with several inflammatory diseases, including inflammatory bowel disease, multiple sclerosis, allergic asthma and rheumatoid arthritis [Citation15]. These three studies found significant differences in gut microbiome composition between the patients that did respond to the checkpoint inhibition immunotherapy and those who did not.
Matson et al. [Citation16] found that in the feces of metastatic melanoma patients, there was a higher abundance of Bifidobacterium longum, Collinsella aerofaciens, and Enterococcus faecium, whereas Gopalakrishnan et al. [Citation17] found abundance of bacteria of the Ruminococcaceae family in responding melanoma patients. Lastly, Routy et al. [Citation18] found a relative abundance of Akkermansia muciniphila in responding non-small cell lung carcinoma, renal cell carcinoma, and urothelial carcinoma patients as compared to non-responding patients and that in patients with a T-cell response targeting A. muciniphila and Enterococcus hirae the progression-free interval was longer. Furthermore, Routy et al. [Citation18] found that antibiotics diminish the clinical benefit of checkpoint inhibition therapy. Earlier, Vétizou et al. [Citation19] already noted the effect of anti-CTLA-4 therapy was dependent on distinct Bacteroides species. Specifically, the occurrence of T-lymphocytes targeting B. thetaiotaomicron or B. fragilis was associated with the better response to this therapy [Citation19]. It is therefore evident that a particular gut microbiota composition is associated with the response to checkpoint inhibition therapy. However, thus far, this evidence is associative and causality and exact mechanism will have to be demonstrated.
Gut dysbiosis-related diseases, such as C. difficile infections, are nowadays treated with fecal microbiome transplantation (FMT), a procedure in which stool samples from healthy donors are transferred to the patient in the form of orally administered capsules containing freeze-dried samples of donor microbiota that have been carefully screened. For recurrent C. difficile infections, FMT reaches success rates of over 90% [Citation20,Citation21].
To validate their hypothesis that the gut microbiome may play a role in the response to immune checkpoint inhibition therapy, Matson et al. [Citation16], Gopalakrishnan et al. [Citation17], and Routy et al. [Citation18] transferred feces from responding and non-responding patients into germ-free mice implanted with human tumor cells. These studies found the mice that received FMT from responding patients, had a better response to anti-PD-1 treatment than the mice that received FMT from non-responding patients [Citation16–Citation18]. Furthermore, studies in mice models show that oral gavage with a combination of A. municiphilia and E. hirae elicits a change in mesenteric and tumor draining lymph nodes, as CD4+ central memory T-cells expressing the chemokine receptors CCR9 or the CXCR-3 accumulate in the mesenteric lymph nodes within 48 h after administration of the bacterial strains and they are also observed in tumor draining lymph nodes and in tumor beds upon killing [Citation18].
Tanoue et al. [Citation22] identified a consortium of 11 bacterial strains from gut microbiota of healthy individuals, which upon introduction in germ-free mice enhance the anti-tumor response, especially the induction of CD8 + T-cells, which are potent producers of IFN-γ. It was further demonstrated that the number of TILs was increased after the ingestion of these 11 strains in tumor-bearing germ-free mice, leading to a reduction in tumor volume of over 50%, which increased even further when applied in combination with anti-PD-1 therapy.
In the meantime, more than nine stool banks are now open worldwide [Citation23]. FMT has been proven a safe treatment even in high-risk patient groups including cancer patients [Citation24] and solid organ transplant recipients [Citation25]. In fact, the majority of adverse events of FMT are self-limiting and gastrointestinal in nature [Citation26]. Potential long-term effects are, however, yet unknown.
2.1. Mechanisms of interaction between commensal bacteria and the immune system
Although the exact mechanisms of influence on the immune system by commensal bacteria are unknown, it is known that metabolites such as small-chain fatty acids of the gut microbiome may influence the balance between pro- and anti-inflammatory cells [Citation27]. To illustrate, butyrate has shown to potentiate extrathymic differentiation of Foxp3+ Treg cells [Citation27]. However, Kespohl et al. [Citation28] showed that butyrate-mediated expansion of Foxp3+ Treg cells requires the presence of TGF-β1, whereas in the absence of additional stimuli, butyrate treatment of CD4+ cells is sufficient for robust induction of Th1-associated factors IFN-γ and T-bet [Citation28]. Furthermore, Sivan et al. attributed their higher response rates in mice with more abundant Bifidobacterium to an increase in IFN- γ production and maturation, activation, and shift in the function of dendritic cells [Citation29]. Also, suggestive of an interaction between bacterial metabolites and the immune system is the observation by Gopalakrishnan et al. [Citation17] that responders have a metabolic inclination toward anabolic pathways as compared to non-responders [Citation17].
An inevitable side effect of immune checkpoint inhibition is the occurrence of immune-related autoinflammatory diseases, notably colitis [Citation26]. In a case report of two patients (one with urothelial carcinoma, one with prostate cancer) who both suffered from severe colitis as a side effect of checkpoint inhibition therapy, complete resolution of clinical symptoms was achieved following treatment with FMT [Citation30]. More recently, in a mouse model of this condition, the probiotic bacterial strain Lactobacillus reuteri has been shown to inhibit the development and progression of colitis [Citation31]. So apart from stimulating the function of the immune system in patients undergoing checkpoint inhibition therapy, microbiota could also reduce the side-effects of the therapy.
3. Conclusion and Expert Summary
Although the studies discussed above still only provide circumstantial evidence, their findings are promising. Using donor feces from the best responding patients with the least side effects for FMT prior to immune checkpoint inhibition therapy, the response rate to anti-PD-1 therapy could be increased. It may take some time, however, before the exact cellular and molecular mechanisms underlying the beneficial effects of gut microbiota on the outcome of immune checkpoint inhibition therapy will be fully elucidated. In the meantime, the potential of this otherwise safe and relatively simple form of adjuvant therapy has already started: in Pittsburgh, Pennsylvania, and London Ontario, clinical trials are recruiting patients on PD-1 therapy to receive concurrent FMT (see NCT03341143, NCT03772899 at clinicaltrials.gov for details). In Israel, a study is ongoing in which melanoma patients who failed anti-PD-1 therapy now receive an FMT (NCT03353402). It is hoped and to be expected that in the near future the most potent bacteria, as well as their functional metabolites will be identified to further improve the success rate of immune checkpoint inhibition therapy. The last days of the Miser are near.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Peer reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Zamora AE, Crawford JC, Thomas PG. Hitting the target: how T cells detect and eliminate tumors. J Iimmunol. 2018 Jan 15;200(2):392–399.
- Aptsiauri N, Ruiz-Cabello F, Garrido F. The transition from HLA-I positive to HLA-I negative primary tumors: the road to escape from T-cell responses. Curr Opin Immunol. 2018 Apr;51:123–132.
- Concha-Benavente F, Srivastava R, Ferrone S, et al. Immunological and clinical significance of HLA class I antigen processing machinery component defects in malignant cells. Oral Oncol. 2016;58:52–58.
- Schachter J, Ribas A, Long GV, et al. Pembrolizumab versus ipilimumab for advanced melanoma: final overall survival results of a multicentre, randomised, open-label phase 3 study (KEYNOTE-006). Lancet. 2017 Oct 21;390(10105):1853–1862.
- Cooper MR, Alrajhi AM, Durand CR. Role of immune checkpoint inhibitors in small cell lung cancer. Am J Ther. 2018 May/Jun;25(3):e349–e356.
- Borcoman E, Le Tourneau C. Pembrolizumab in cervical cancer: latest evidence and clinical usefulness. Ther Adv Med Oncol. 2017 Jun;9(6):431–439.
- Lugowska I, Teterycz P, Rutkowski P. Immunotherapy of melanoma. Contemp Oncol. 2018 Mar;22(1a):61–67.
- Pakkala S, Owonikoko TK. Immune checkpoint inhibitors in small cell lung cancer. J Thorac Dis. 2018 Feb;10(Suppl 3):S460–s467.
- Homet Moreno B, Mok S, Comin-Anduix B, et al. Combined treatment with dabrafenib and trametinib with immune-stimulating antibodies for BRAF mutant melanoma. Oncoimmunology. 2016 Jul;5(7):e1052212.
- Snyder A, Makarov V, Merghoub T, et al. Genetic basis for clinical response to CTLA-4 blockade in melanoma. N Engl J Med. 2014 Dec 4;371(23):2189–2199.
- Rizvi NA, Hellmann MD, Snyder A, et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. 2015 Apr 3;348(6230):124–128.
- McGranahan N, Furness AJ, Rosenthal R, et al. Clonal neoantigens elicit T cell immunoreactivity and sensitivity to immune checkpoint blockade. Science. 2016 Mar 25;351(6280):1463–1469.
- Luksza M, Riaz N, Makarov V, et al. A neoantigen fitness model predicts tumour response to checkpoint blockade immunotherapy. Nature. 2017 Nov 23;551(7681):517–520.
- Espi Forcen F, Espi Forcen C. Ars Moriendi: coping with death in the late Middle Ages. Palliative Supportive Care. 2016 Oct;14(5):553–560.
- Kim D, Zeng MY, Nunez G. The interplay between host immune cells and gut microbiota in chronic inflammatory diseases. Exp Mol Med. 2017 May 26;49(5):e339.
- Matson V, Fessler J, Bao R, et al. The commensal microbiome is associated with anti-PD-1 efficacy in metastatic melanoma patients. Science. 2018 Jan 5;359(6371):104–108.
- Gopalakrishnan V, Spencer CN, Nezi L, et al. Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science. 2018 Jan 5;359(6371):97–103.
- Routy B, Le Chatelier E, Derosa L, et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science. 2018 Jan 5;359(6371):91–97.
- Vetizou M, Pitt JM, Daillere R, et al. Anticancer immunotherapy by CTLA-4 blockade relies on the gut microbiota. Science. 2015 Nov 27;350(6264):1079–1084.
- Silverman MS, Davis I, Pillai DR. Success of self-administered home fecal transplantation for chronic Clostridium difficile infection. Clin Gastroenterol Hepatol. 2010 May;8(5):471–473.
- Merenstein D, El-Nachef N, Lynch SV. Fecal microbial therapy: promises and pitfalls. J Pediatr Gastroenterol Nutr. 2014 Aug;59(2):157–161.
- Tanoue T, Morita S, Plichta DR, et al. A defined commensal consortium elicits CD8 T cells and anti-cancer immunity. Nature. 2019 Jan;565(7741):600–605.
- Terveer EM, van Beurden YH, Goorhuis A, et al. How to: establish and run a stool bank. Clin Microbiol Infect. 2017 Dec;23(12):924–930.
- Hefazi M, Patnaik MM, Hogan WJ, et al. Safety and efficacy of fecal microbiota transplant for recurrent Clostridium difficile infection in patients with cancer treated with cytotoxic chemotherapy: a single-institution retrospective case series. Mayo Clin Proc. 2017 Nov;92(11):1617–1624.
- Cheng YW, Phelps E, Ganapini V, et al. Fecal microbiota transplantation for the treatment of recurrent and severe Clostridium difficile infection in solid organ transplant recipients: a multicenter experience. Am J Transplant. 2019 Feb;19(2):501–511.
- Baxter M, Colville A. Adverse events in faecal microbiota transplant: a review of the literature. J Hosp Infect. 2016 Feb;92(2):117–127.
- Arpaia N, Campbell C, Fan X, et al. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature. 2013 Dec 19;504(7480):451–455.
- Kespohl M, Vachharajani N, Luu M, et al. The microbial metabolite butyrate induces expression of Th1-associated factors in CD4(+) T Cells. Front Immunol. 2017;8:1036.
- Sivan A, Corrales L, Hubert N, et al. Commensal Bifidobacterium promotes antitumor immunity and facilitates anti-PD-L1 efficacy. Science. 2015 Nov 27;350(6264):1084–1089.
- Wang Y, Wiesnoski DH, Helmink BA, et al. Fecal microbiota transplantation for refractory immune checkpoint inhibitor-associated colitis. Nat Med. 2018;24(12):1804–1808.
- Wang T, Zheng N, Luo Q, et al. Probiotics Lactobacillus reuteri abrogates immune checkpoint blockade-associated colitis by inhibiting group 3 innate lymphoid cells. Front Immunol. 2019;10:1235.
