ABSTRACT
Introduction
As well as improving population health, promoting equity in health is one of the key goals of health policy in low- and middle-income countries (LMICs). However, it is less clear how equity is defined, or how it may impact on resource allocation decisions. We investigated the degree to which health inequalities have been considered in economic evaluation of health interventions in LMICs, and what demographic or socioeconomic characteristics were used to define equity relevant subgroups.
Areas covered
We reviewed publications since 2010 from three main databases following the search strategy developed by including the key terms ‘health inequalities/health disparities/health equity,’ ‘economics’ and ‘low- and middle-income countries’ in the title or abstract. Twelve studies were identified, mainly focusing on interventions for the more vulnerable groups such as children and women.
Expert opinion
Some attempts have been made to assess interventions’ impact on health inequality and there is increasing interest in evaluating it, although research in this area is lacking. Population subgroups highlighted in the included studies were those differing in socioeconomic status. Most studies reported the results across subgroups to illustrate inequality impact, and the newly developed methods, extended cost-effectiveness analysis and distributional cost-effectiveness analysis, have also been applied.
1. Introduction
The past three decades have witnessed significant progress in improving the health of people in low- and middle-income countries (LMICs) such as reduced child mortality and increased life expectancy [Citation1]. Empirical studies of the differences in health between the poor and the better off found that the gap has remained appreciable, with the poor facing lower odds of receiving key health interventions and worse health outcomes [Citation2,Citation3]. As well as improving population health, promoting equity in health is one of the key goals of health policy in LMICs [Citation4–7].
Health equity includes equal access to healthcare services and fair health outcomes among population groups defined socially, economically, demographically or geographically. An increasing number of LMICs are currently offering or striving for universal healthcare coverage, aiming to provide equal care to all, but access to these services is still unequal, evidenced by the literature that explored the differences in access to healthcare in LMICs [Citation8–11]. The unfair health outcomes that are considered avoidable are referred to as ‘health inequality.’ This means poorer health, reduced health-related quality of life (HRQoL) and early death for the more disadvantaged people. Reducing these inequalities is a key feature of global health policy agendas, contributing to the sustainable development goals [Citation12,Citation13]. Economic evaluation methods, such as cost-effectiveness analysis (CEA), have been widely used to inform healthcare resource allocation decisions, but mainly focus on how the intervention or policy affects total health [Citation14]. Recent methodological developments have included health inequality concerns into economic evaluation to describe the distribution of health benefits, for example the extended cost-effectiveness analysis (ECEA) [Citation15], which provides breakdowns of health outcomes, out of pocket expenditure and financial risk protection by population group, and distributional cost-effectiveness analysis (DCEA) [Citation16], which focuses on the breakdown of health outcomes and opportunity costs, and provides summary measures of health inequality impact to inform potential trade-offs between increasing overall health and reducing health inequality.
More studies are applying the newly developed methods, ECEA or DCEA, in LMICs, such as in India [Citation15], Ethiopia [Citation17] and Malawi [Citation18]. We sought to develop an overview of the extent to which inequality impact has been considered in economic evaluations of health interventions or policies in LMICs before and after these methods became more widely known. We summarize what approaches have been used to describe the distribution or the different impact across the population groups, and what equity relevant groups were considered in the evaluation and what demographic or socioeconomic characteristics were used to characterize these groups.
Thus, through a systematic review, we would like to inform the following questions:
1. has the inequality impact been included in economic evaluation in LMICs?
2. what equity relevant groups were considered?
3. what approaches have been used to assess the impact?
2. Methods
The systematic review was conducted and reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [Citation19].
2.1. Search strategy
Three databases were searched: Ovid MEDLINE (1946 to 1 February 2021), Ovid EMBASE (1974 to 1 February 2021) and Global Health Cost-Effectiveness Analysis Registry (publication year: 1995 to 2020) (http://ghcearegistry.org/ghcearegistry/). All searches were conducted on 2 February 2021. The search strategy was developed by including the key terms ‘health inequalities/health disparities/health equity,’ ‘economics’ and ‘low- and middle-income countries’ and their synonyms in the title or abstract. We did not use the terms ‘economic evaluation’ or ‘cost-effectiveness analysis’ because a lot of commissioned studies for LMICs were cost-benefit analyses and social returns on investment, which may not be captured using this narrower strategy. A detailed search strategy is available in Appendix 1.
2.2. Eligibility criteria
After dropping duplicates, two reviewers independently screened the titles and abstracts of all the records identified from the database searches using the inclusion criteria detailed below.
Peer-reviewed journal articles, reports published by non-government organizations (NGOs) or health technology assessment (HTA) bodies, studies published in discussion papers by academic institutions.
Studies focused on the populations in LMICs, studies featuring multinational participants including LMICs and it is possible to isolate the results for these participants from LMICs.
Economic evaluation studies in which the health outcomes were reported or estimated.
Studies with a focus on health inequality in which the different health outcomes across population groups were assessed or discussed. The population groups should be defined based on non-clinical characteristics, e.g. ethnicity, sex, education.
Publications in the last 10 years (since 2010)
All other publication types, including conference abstracts, study protocols, commentaries, editorials, were excluded. The list of countries with low-income or middle-income economies compiled by the Organization for Economic Co-operation and Development was used [Citation20]. Reviews of prior studies were excluded, but references in review articles were screened to identify additional original studies missed by the search strategy. Studies including population groups defined by clinical characteristics, e.g. low-risk and high-risk, were excluded as the differences in health outcomes may not be avoidable.
After the screening of titles and abstracts, the two reviewers independently reviewed the full-text of any article that appeared to meet the eligibility criteria to reach a consensus on the final list of included studies. Any discrepancy in the reviewing process was resolved by discussion between the two reviewers and by consulting with a third reviewer if necessary.
The quality of included full-text studies was assessed using the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Consolidated Health Economic Evaluation Reporting Standards (CHEERS) 24-item checklist [Citation21].
2.3. Data extraction
Upon agreement on the final list of included studies, one reviewer extracted data from the included studies into a predefined Microsoft Excel form. Subsequently, another author validated the extracted data by checking them. The form was developed following the reporting guidelines for systematic reviews with a focus on health equity [Citation22], including information about authors, year of publication, country, target population, intervention, comparator, type of study, costs perspective, health outcomes, modeling, population subgroups, method, and main results (Appendix 2). Followed the PROGRESS-Plus criteria [Citation23], characteristics used in the included studies to characterize population subgroups related to equity were collected including place of residence, race/ethnicity/culture/language, occupation, gender/sex, religion, education, socioeconomic status, social capital and other associated characteristics (e.g. age, disability, excluded from school, other instances where a person may be temporarily at a disadvantage).
3. Results
3.1. Characteristics of the studies
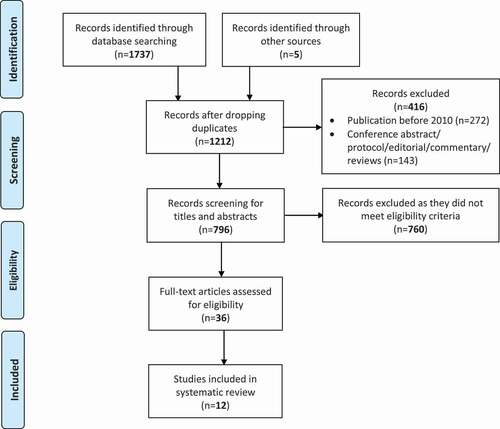
The search identified a total of 1742 records. After dropping duplicates, non-peered reviewed articles and publications before 2010, 796 records were screened for titles and abstracts and 36 were further screened for full-text. Finally, 12 studies met the inclusion criteria and were included in the systematic review (see , PRISMA diagram). summarizes the characteristics of all included studies.
Table 1. Summary of the included studies
Majority of the included studies (ten studies, 83.3%) were CEA, using Markov model [Citation24–26], dynamic transmission model [Citation15] or microsimulation [Citation27]. In the two studies which were not CEA [Citation28,Citation29], economic evaluations were conducted with health outcomes, but they did not report results on costs; both studies were included to extract the method used to estimate inequality impact. Mortality was most commonly included as main health outcome [Citation15,Citation17,Citation24,Citation26,Citation28–32]; generic metrics such as life years [Citation26–28], disability-adjusted life years (DALYs) [Citation18,Citation25,Citation28,Citation30–32], quality-adjusted life years (QALYs) [Citation24] and health-adjusted life years (HALYs) [Citation17], and other disease-specific outcomes, e.g. hepatitis B infections averted [Citation24], cervical cancer cases averted [Citation27] and obesity prevalence [Citation28], were also included as health outcomes.
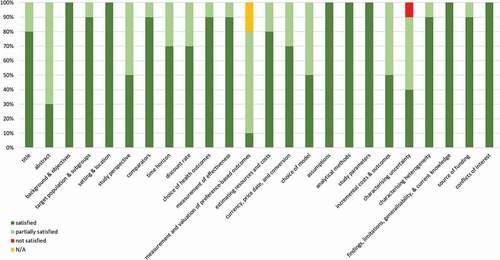
Quality of the included ten CEA studies was assessed and the total and individual CHEERs checklist scores are presented in and Tables S1-S2. In general, there was good adherence to best-practice reporting standards, with ‘satisfied’ or ‘partially satisfied’ in almost all the 24 items. It should be noted that among the 10 CEA studies, one study did not report results of uncertainty analysis [Citation26]; two studies conducted uncertainty analysis for the overall cost-effectiveness, rather than the impact on inequality [Citation24,Citation27]; two studies performed the uncertainty analysis to a range of assumptions [Citation17,Citation18]; four studies analyzed the uncertainty about the distribution of health benefits to support inequality impact assessment [Citation15,Citation30–32]; only one studies carried out full uncertainty analysis (including probabilistic sensitivity analysis) for the inequality impact and provided the confidence level of the conclusion about whether the intervention increases/reduces health inequality [Citation25].
3.2. Has the inequality impact been included in economic evaluation in LMICs?
As shown in , eight of the twelve included studies were published in the last three years (2018 onwards). This reflects an increasing focus on the impact, although only a few studies have attempted to assess the impact on health inequality.
Five studies (41.7%) assessed the impact in countries in Asia (China [Citation24], India [Citation15,Citation30], Pakistan [Citation31] and Laos [Citation32]), five studies (41.7%) in Africa (Uganda [Citation27], Ethiopia [Citation17,Citation26], Zambia [Citation28], and Malawi [Citation18]), one study (8.3%) in South America (Brazil [Citation25]), and one study (8.3%) evaluated the results in 41 LMICs [Citation29]. The studies were conducted in a wide variety of countries, nevertheless, concentrated in Asia and Africa. It implies that resource allocation and prioritization decisions in these countries may be informed by evidence on how the potential health intervention or strategy would affect health inequality.
Regarding the target populations and interventions or strategies assessed, more than half of the included studies (n = 7, 58.3%) focused on children or infants [Citation17,Citation24,Citation26,Citation29–32], assessing the impact of vaccination programs, e.g. nationwide hepatitis B vaccination [Citation24], rotavirus vaccination [Citation30–32] and vaccines for a wide range of antigens [Citation29], and children pneumonia treatment scale-up strategy [Citation26]; three studies (25.0%) focused on general population or adult population, covering complex interventions such as excise tax on sugar sweetened beverages [Citation28], population level essential health package (EHP) [Citation18] and community level primary care system intervention [Citation25]; one study (8.3%) focused on the impact of different cervical cancer screening strategies for women aged 30–49 years [Citation27] and one study (8.3%) assessed the effect of public finance intervention for tuberculosis treatment [Citation15].
3.3. What equity relevant groups were considered?
presents the characteristics used in all the included studies to define the equity relevant population subgroups. Socioeconomic status was most commonly used (n = 8, 66.7%), categorized by wealth quintiles based on household asset index [Citation17,Citation18,Citation30–32], household income [Citation29], an individual’s annual income [Citation15] or an area-based indicator of socioeconomic status (gross regional product) [Citation25]. Region was used in six studies, between states with different disease risks [Citation26,Citation30–32], states with different socioeconomic level [Citation25] or urban and rural areas [Citation18]. Region was used to combine with wealth quintiles to form more subgroups [Citation30] or as an alternative to indicate socioeconomic status [Citation18,Citation25]. Sex was used in two studies [Citation28,Citation30] and other associated characteristics, e.g. age [Citation24] and access to cancer screening [Citation27], were also used.
Table 2. Characteristics used in the included studies to describe the population subgroups related to equity*
3.4. What approaches have been used?
presents the methods and summary of inequality impact used in the included studies for estimating the distributional effect. Six studies conducted subgroup analysis and reported the breakdown cost-effectiveness results to demonstrate the different effect across population [Citation24,Citation28–32]. One study used pre-defined outcome measures to reflect equity concerns [Citation27], that is, ‘health disparity,’ which equals to difference in life expectancy between women with and without access to cervical cancer screening, and ‘distributional equity,’ which equals to difference between life expectancy in women with access to screening and population average life expectancy. One study applied the Gini coefficient, a measure of inequality, to life expectancy to describe interindividual and geographical inequality impacts [Citation26]. Four studies used the existing analysis methods, ECEA [Citation15] or DCEA [Citation17,Citation18,Citation25], to assess the intervention impact, but these were case studies, aiming to illustrate how the method can be applied for LMIC contexts. Among the three studies using DCEA, the metric for assessing inequality impact was equally distributed equivalence (EDE) health, a single index measure of health that combines concerns for health improvement and inequality reduction [Citation33].
Table 3. Outcomes and methods used in the included studies for estimating the distributional effect
4. Expert opinion
4.1. Challenges
Economic evaluation has been increasingly used in LMICs to assess the ‘value for money’ of health interventions. Whilst methodological advances have been made in equity-incorporated economic evaluation, there is still a big gap in applying these methods in practice in low-resource settings.
The identified studies have primarily focused on the interventions designed for improving health of the more vulnerable groups such as rotavirus vaccination for children and cervical cancer screening for women. This may indicate that these programs are the interventions that decision makers or funders are most interested in understanding the inequality impact. Although it is well recognized that vaccines have contributed significantly to the improvement of population health in the past few decades, how different population groups benefit from the vaccination programs has been less explored. Therefore, in future studies evaluating cost-effectiveness of these interventions, researchers are suggested to consider assessing the inequality impact as well, providing information about how the potential health benefits are spread, to better support decision making. The evaluation of vaccines or different vaccination programs would be an even more important issue during the COVID-19 pandemic. Abbas et al. [Citation34] assessed the impact on future mortality with vaccination clinics closed in Africa during lockdown and recommended that the routine children immunization should be sustained in Africa as much as possible. It is likely that the impact of these suspended vaccination programs, not only on health inequality, would be a focus of the future evaluations in LMICs.
Policy relevant population subgroups were those differing in socioeconomic status. Wealth quintiles were most often constructed using household asset indices, which have been widely used in literature to create wealth rankings and separate the rich from the poor for analyses [Citation35]. Generally, a household with better socioeconomic status is expected to spend more and possess more of the goods which are considered essential at a household level. However, the components of the asset index are to some degree related to the household’s preferences [Citation36], which may not fully reflect the socioeconomic status. The asset indices also appear to have low internal validity when used in rural areas, thus making rural asset holders look poorer than they should and exaggerating the urban-rural differences [Citation35]. Income level could be an alternative to define household socioeconomic status, as did in two of the included studies, but this requires high quality of data, which may be difficult in most LMICs. Respondents may have difficulty in remembering the exact income especially when there are several sources of income in the household; respondents might be unaware of the income of all household members [Citation37,Citation38]; income might not be stable during a period of time as the sources may depend on seasonal effects, e.g. farming and fishing. In view of these drawbacks, caution should be exercised when asset index or income level is used to categorize population subgroups relevant to equity concerns. The associated ambiguity may also make it challenging to describe the current level of health inequality between these subgroups and further weaken the value of estimates of distributional effects of the intervention. Region has been used in several studies to characterize policy relevant subgroups. Considering the remarkable differences between regions such as economic development level, population age structure and disease prevalence, it makes sense to think about region-related inequality as the potential intervention may be expected to achieve more benefits if it is firstly implemented in regions with higher risks and more disadvantaged. The results would inform policy makers of which regions to prioritize when considering intervention implementation. However, the focus on area-specific inequalities may add uncertainty to the estimation of the intervention impact. The newly developed method DCEA [Citation16] accounts for the fact that health expenditures would fall proportionally among population subgroups and favors the more disadvantaged. There is a lack of knowledge about how residents in different regions benefit from the health expenditures. Without such information, analysts have to make some assumptions, e.g. equal distribution, to enable the estimates of distributional effect, which may lead to over-/under-estimation of the health benefits from an intervention.
To describe the different impacts of health interventions across population, reporting results by subgroups is the most straightforward way. Although there are new methods available, the knowledge and application of these methods is not yet widespread in LMICs. This is most likely due to the lack of familiarity with these methods. Another obstacle to the application may be the unavailability of existing evidence in LMICs such as preference weights for health benefits of different subgroups. The evidence is required to aggregate the subgroup cost-effectiveness results into a single measure such as EDE health. Possible due to the unavailability, analysts prefer to present the results separately for each subgroup to describe the impact qualitatively rather than explicitly quantify it with some assumptions.
4.2. Recommendations
As previously discussed, the measures, such as asset index and income level, used to define equity relevant population subgroups may have limitations, and thus a stable, well-constructed and multidimensional measure might be preferred in LMICs. For example, an index of multiple deprivation is used in England which combines information from seven domains to produce an overall measure of deprivation [Citation39]. It might be worth exploring the feasibility of developing a similar measure suitable in the LMIC settings. The availability of such measure would enable more research into the role of socioeconomic status on people’s health and the distribution of health expenditures. All of these would contribute to the development and application of the methods assessing intervention impact on inequality in LMICs, to support evidence-based decisions.
Regarding the methods used to incorporate inequality impact in economic evaluations, we recommend the ECEA and DCEA methods to analysts and decision makers in LMICs who are interested in conducting an in-depth analysis of the intervention impacts on overall health and health inequality. Both ECEA and DCEA fundamentally build on standard CEA and extend the analysis to describe the distribution of health benefits by applying the social inequality aversion preference after estimating the costs and benefits for each subgroup (using the corresponding parameters). Previous applications have shown that the skills required lie within the capabilities of analysts currently conducting CEA and the information generated could provide decision makers with evidence that will enable them to think about equity issues in a more systematic and science-informed way [Citation16,Citation33,Citation40]. If the decision makers are also interested in developing equity ‘benchmarks’ to compare across interventions or policy choices, DCEA, which uses one single measure to show the trade-offs between equity and cost-effectiveness, can be particularly useful as a way to understand the impact of policy decisions and facilitate transparency and consistency of decision making.
Looking ahead, it is expected that there would be more applied economic evaluation studies using these new methods to describe the distribution of health benefits and thus inform policy makers with equity concerns in the LMIC setting. This requires evidence related to fundamental methodological issues such as current level of inequality between policy relevant groups and people’s preferences toward reducing inequalities compared to improving health, which might be the directions of future research.
5. Conclusions
This systematic review of economic evaluation studies of health interventions or strategies in LMICs shows that the intervention’s impact on inequality has been considered to inform policy makers with equity concerns, and that the evaluation studies mainly focused on interventions for the more vulnerable groups such as children and women. Two-thirds of the included studies were published within the last 3 years (2018–2020), suggesting an increasing trend to take inequality impact into account. Population subgroups were mainly defined by wealth quintiles or regions, which could reflect policy makers’ preference toward reducing inequalities resulted from socioeconomic status or geographic variations. In terms of the methods used to evaluate the inequality impact, most studies reported the cost-effectiveness results for population subgroups, and the newly developed methods, ECEA and DCEA, have also been applied in some studies, demonstrating the usefulness and advantages in the provision of scientific evidence. We expect that along with increasing capacity and experience in the LMIC setting, these methods would be more widely used to describe the distribution of health benefits and thus guide public health decisions, contributing to the development of stronger and more resilient health systems.
Article highlights
In low- and middle-income countries, the impact on health inequality has been considered in economic evaluation of health interventions.
The evaluation studies mainly focused on interventions for the more vulnerable groups such as children and women.
There is an increasing trend to consider inequality impact to inform public health policy makers.
Population subgroups characterized by socioeconomic status are most associated with of resource allocation and prioritization decisions.
Most studies reported the results across subgroups to illustrate inequality impact, and some studies have also applied the ECEA or DCEA method.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewers disclosure
Peer reviewers on this manuscript have no relevant financial relationships or otherwise to disclose.
Supplemental Material
Download MS Word (26.5 KB)Supplementary material
Supplemental data for this article can be accessed here
Additional information
Funding
References
- World Health Organisation. World health statistics 2020: monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization; 2020.
- Chao F, You D, Pedersen J, et al. National and regional under-5 mortality rate by economic status for low-income and middle-income countries: a systematic assessment. Lancet Glob Health. 2018;6(5):e535–e547.
- Wagstaff A, Bredenkamp C, Buisman LR. Progress on global health goals: are the poor being left behind? World Bank Res Obser. 2014;29(2):137–162.
- Zere E, Moeti M, Kirigia J, et al. Equity in health and healthcare in Malawi: analysis of trends. BMC Public Health. 2007;7(78). DOI:https://doi.org/10.1186/1471-2458-7-78
- Umuhoza SM, Ataguba JE. Inequalities in health and health risk factors in the Southern African Development Community: evidence from World Health Surveys. Int J Equity Health. 2018;17(1):52.
- Hosseinpoor AR, Bergen N, Kunst A, et al. Socioeconomic inequalities in risk factors for non communicable diseases in low-income and middle-income countries: results from the World Health Survey. BMC Public Health. 2012;12:912.
- Gattini C. Implementing national health observatories: operational approach and strategic recommendations. Implementing National Health Observatories: operational approach and strategic recommendations. 2009.
- Rezal RS, Hassali MA, Alrasheedy AA, et al. Prescribing patterns for upper respiratory tract infections: a prescription-review of primary care practice in Kedah, Malaysia, and the implications. Expert Rev Anti Infect Ther. 2015;13(12):1547–1556.
- Ewen M, Joosse HJ, Beran D, et al. Insulin prices, availability and affordability in 13 low-income and middle-income countries. BMJ Glob Health. 2019;4(3):e001410.
- Godman B, Basu D, Pillay Y, et al. Ongoing and planned activities to improve the management of patients with Type 1 diabetes across Africa; implications for the future. Hosp Pract (1995). 2020;48(2):51–67.
- Godman B, Basu D, Pillay Y, et al. Review of ongoing activities and challenges to improve the care of patients with type 2 diabetes across Africa and the implications for the future. Front Pharmacol. 2020;11(108). DOI:https://doi.org/10.3389/fphar.2020.00108
- Bosch-Capblanch X, Lavis JN, Lewin S, et al. Guidance for evidence-informed policies about health systems: rationale for and challenges of guidance development. PLoS Med. 2012;9(3):e1001185.
- World Health Organisation. Rio political declaration on social determinants of health. (Ed.^(Eds). World Conference on Social Determinants of Health. Rio de Janeiro, Brazil; 2011 Oct 19–21.
- Drummond MF, Sculpher MJ, Torrance GW, et al. Methods for the economic evaluation of health care programmes. Oxford (UK): Oxford University Press; 2005.
- Verguet S, Laxminarayan R, Jamison DT. Universal public finance of tuberculosis treatment in India: an extended cost-effectiveness analysis. Health Econ. 2015;24(3):318–332.
- Asaria M, Griffin S, Cookson R, et al. Distributional cost-effectiveness analysis of health care programmes--a methodological case study of the UK bowel cancer screening programme. Health Econ. 2015;24(6):742–754.
- Dawkins BR, Mirelman AJ, Asaria M, et al. Distributional cost-effectiveness analysis in low- and middle-income countries: illustrative example of rotavirus vaccination in Ethiopia. Health Policy Plan. 2018;33(3):456–463.
- Arnold M, Nkhoma D, Griffin S. Distributional impact of the Malawian essential health package. Health Policy Plan. 2020;35(6):646–656.
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
- Low- and middle-income countries. [cited 2021 Jun 20]. Available from: https://wellcome.org/grant-funding/guidance/low-and-middle-income-countries
- Husereau D, Drummond M, Petrou S, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS)--explanation and elaboration: a report of the ISPOR health economic evaluation publication guidelines good reporting practices task force. Value Health. 2013;16(2):231–250.
- Welch V, Petticrew M, Tugwell P, et al. PRISMA-equity 2012 extension: reporting guidelines for systematic reviews with a focus on health equity. PLoS Med. 2012;9(10):e1001333.
- Tugwell P, Petticrew M, Kristjansson E, et al. Assessing equity in systematic reviews: realising the recommendations of the commission on social determinants of health. BMJ. 2010;341:c4739.
- Hutton DW, So SK, Brandeau ML. Cost-effectiveness of nationwide hepatitis B catch-up vaccination among children and adolescents in China. Hepatology. 2010;51(2):405–414.
- Love-Koh J, Mirelman A, Suhrcke M. Equity and economic evaluation of system-level health interventions: a case study of Brazil’s family health program. Health Policy Plan. 2020.
- Olsen M, Norheim OF, Memirie ST. Reducing regional health inequality: a sub-national distributional cost-effectiveness analysis of community-based treatment of childhood pneumonia in Ethiopia. Int J Equity Health. 2021;20(1):9.
- Campos NG, Tsu V, Jeronimo J, et al. To expand coverage, or increase frequency: quantifying the tradeoffs between equity and efficiency facing cervical cancer screening programs in low-resource settings. Int J Cancer. 2017;140(6):1293–1305.
- Hangoma P, Bulawayo M, Chewe M, et al. The potential health and revenue effects of a tax on sugar sweetened beverages in Zambia. BMJ Glob Health. 2020;5(4). DOI:https://doi.org/10.1136/bmjgh-2019-001968
- Chang AY, Riumallo-Herl C, Perales NA, et al. The equity impact vaccines May have on averting deaths and medical impoverishment in developing countries. Health Aff (Millwood). 2018;37(2):316–324.
- Rheingans R, Anderson J, Anderson B, et al. Estimated impact and cost-effectiveness of rotavirus vaccination in India: effects of geographic and economic disparities. Vaccine. 2014;32(Suppl 1):A140–150.
- Rheingans R, Anderson J, Bagamian KH, et al. Effects of geographic and economic heterogeneity on the burden of rotavirus diarrhea and the impact and cost-effectiveness of vaccination in Pakistan. Vaccine. 2018;36(51):7780–7789.
- Rheingans R, Anderson J, Bagamian KH, et al. Effects of geographic and economic heterogeneity on rotavirus diarrhea burden and vaccination impact and cost-effectiveness in the Lao People’s Democratic Republic. Vaccine. 2018;36(51):7868–7877.
- Asaria M, Griffin S, Cookson R. Distributional cost-effectiveness analysis: a tutorial. Med Decis Making. 2016;36(1):8–19.
- Abbas K, Procter SR, van Zandvoort K, et al. Routine childhood immunisation during the COVID-19 pandemic in Africa: a benefit-risk analysis of health benefits versus excess risk of SARS-CoV-2 infection. Lancet Glob Health. 2020;8(10):e1264–e1272.
- Wittenberg M, Leibbrandt M. Measuring inequality by asset indices: a general approach with application to South Africa. Rev Income Wealth. 2017;63(4):706–730.
- Ucar B. The usability of asset index as an indicator of household economic status in Turkey: comparison with expenditure and income data. Social Indic Res. 2015;121(3):745–760.
- Øvensen G. An asset index for the Syrian 2003 unemployment survey. (Ed.^(Eds). Fafopaper. 2006.
- Rutstein SO, Johnson K. The DHS wealth index. DHS comparative reports no. 6. Calverton: ORC Macro; 2004.
- English indices of deprivation. 2019. [cited 2021 Jun 20]. Available from: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019
- Yang F, Angus C, Duarte A, et al. Impact of socioeconomic differences on distributional cost-effectiveness analysis. Med Decis Making. 2020;40(5):606–618.