ABSTRACT
Objectives
To conduct cost-utility and budget impact analysis of providing Continuous Positive Airway Pressure (CPAP) therapy versus no treatment for moderate to severe obstructive sleep apnea (OSA) in Colombia from a third-party payer perspective.
Methods
We used a Markov model to assess the cost-utility and budget impact analysis of CPAP in patients over 40 years old with moderate to severe OSA. Data on effectiveness and utility values were obtained from published literature. A discount rate of 5% was applied for outcomes and costs. ICER was calculated and compared against the threshold estimated for Colombia, which is 86% of the GDP per capita.
Results
Over a lifetime horizon, the base case analysis showed the incremental cost per quality-adjusted life-years (QALYs) gained with CPAP therapy was COP$3,503,804 (USD$1,011 in 2020 prices). The budget impact analysis showed that the adoption of CPAP therapy in the target population would lead to a cumulative net budget impact of COP$411,722 million (USD$118,784,412 in, 2020 prices) over five years of time horizon.
Conclusions
CPAP was cost-effective compared to no-treatment in OSA. According to the budget impact analysis, adopting this technology would require a budget allocation that is partially offset by reduced number of strokes and traffic accident events.
1. Introduction
Obstructive sleep apnea (OSA) is a common chronic breathing disorder characterized by complete or partial upper airway obstruction during sleep [Citation1,Citation2]. OSA presents different states of severity measured by the apnea-hypopnea index (AHI), which evaluates the event frequency of apnea/hypopnea per hour, classifying them as mild (5 to 14.9 events/hour), moderate (15 to 29.9 events/hour) and severe (≥30 events/hour) [Citation1,Citation2].
OSA has a negative impact on overall health due to its association with several pathologies such as heart failure, arterial hypertension, acute coronary syndrome, atrial fibrillation, diabetes mellitus, dyslipidemia, and cardiovascular mortality [Citation3]. Sleep fragmentation can lead to daytime sleepiness and a decrease in cognitive function that impact the quality-of-life scores, productivity at work and a significant risk of road traffic and occupational accidents [Citation1,Citation4,Citation5]. Evidence suggests that OSA contributes to poor health outcomes and is linked to a high economic burden [Citation6].
The prevalence of OSA relates to several risk factors such as obesity, gender, race, geographical location, and age. The worldwide prevalence is estimated to be 936 million people between 30 and 69 years old. Based on the extrapolation of data from 16 countries and taking 2015 as a reference year, the prevalence in Colombia was calculated as 49.6% [Citation6]. In an observational study conducted in three Colombian cities based on population projections for 2012, it was estimated that 19% of the population had a high risk of OSA according to the Berlin questionnaire and 26.9% according to STOP-Bang questionnaire [Citation7].
OSA treatment includes lifestyle change recommendations that involve changes in sleep habits, physical activity, and weight reduction when it is needed, and medical and surgical interventions [Citation8]. Medical treatments include mandibular advancement devices, positional therapy, and positive airway pressure (PAP) devices as the first-line therapy [Citation8,Citation9]. Surgical treatments include airway surgeries and electric stimulation of the hypoglossal nerve [Citation9]. In Colombia, there is no official clinical practice guideline available, so experts use international guidelines as a reference, particularly those of The American College of Physicians and the American Academy of Sleep Medicine. In these guidelines, continuous positive airway pressure (CPAP) therapy is recommended as a first-line treatment for patients diagnosed with moderate to severe OSA and those with mild OSA with any of the following factors: increased cardiovascular risk, excessive sleepiness, poor sleep-related quality of life or presence of comorbidities [Citation1,Citation8].
Despite the fact that OSA represents a public health problem with a high burden, economic evaluation in the Colombian context is scarce. Therefore, this study aimed to perform a cost-utility and budget impact analysis of CPAP therapy in patients diagnosed with moderate to severe obstructive sleep apnea compared with no treatment in Colombia from the third-party payer perspective. The cost-utility analysis helped to identify whether the CPAP therapy represents good value for money and the budget impact analysis allows policy makers to allocate budget for the immediate and short-term provision cost of CPAP therapy to the patients that can benefit from its use.
2. Methods
2.1. Setting, comparator, target population
A Markov model was developed to conduct a cost-utility and budget impact analysis of CPAP therapy for treating moderate to severe OSA compared to no treatment in the Colombian setting considering the first-line treatment for moderate to severe OSA is PAP therapy. In Colombia, insurance coverage is almost universal, and most health-care expenses are covered with public funds [Citation10]. Therefore, the economic evaluations were conducted from the third-party payer perspective, the Colombian Health System perspective. The study population were patients over 40 years old diagnosed with moderate to severe OSA [Citation11,Citation12]. Although patients with mild OSA with increased cardiovascular risk, excessive sleepiness, poor sleep-related quality of life or presence of comorbidities are eligible to CPAP therapy, they were not included in the model due to the difficulty of identifying the proportion of OSA patients matching the criteria. In the analysis, we followed the methodological recommendations of the Institute of Health Technology Assessment (IETS, by its acronym in Spanish) [Citation13].
2.2. Model design
We adopted a Markov model developed by the manufacturer (ResMed) and previously submitted to NICE [Citation14]. The Markov model was structured in terms of four health states (Patients with OSA, non-fatal stroke, non-fatal AMI and death) and three events (stroke, acute myocardial infarction-AMI, or road traffic accident) as illustrated in . Patients in the OSA state at baseline can remain in this state after one cycle (1 year) without developing an event, proceeding to one of the three events or death state. Patients with OSA who have had a traffic accident can return to an event-free OSA state in subsequent years. Once a patient has suffered an AMI or stroke, the only transition possibility is to a death state or the state of post-event (non-fatal stroke, non-fatal AMI). Patients who are post-stroke have a risk of developing an AMI, and those in post-AMI could have a stroke or a traffic accident. It was assumed that stroke patients should not have a traffic accident because such patients are not expected to drive after the event. Transition probabilities were obtained from a recent network meta-analysis and representative clinical trials [Citation15–23] and converted to the cycle length (1-year) ().
Figure 1. Structure of the model. Abbreviations: RTA: Road traffic accident; AMI: Acute miocardial infarction; OSA: Obstructive sleep apnea.
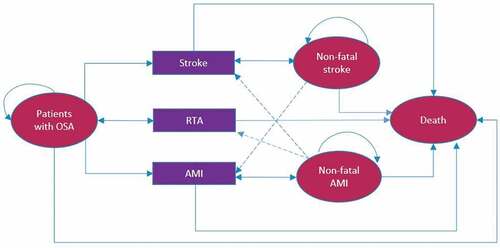
Table 1. Parameters adopted in the economic model.
2.3. Cost and resource data
The intervention costs included the costs of CPAP rental and the disposable supplies (mask, tubing, headgear) and the additional monitoring required for these patients. Filter cost was not included since it is not covered by the health insurance plan. In the model, the CPAP cost is applied every five years, considering the device’s lifetime [Citation25,Citation26]. The mask is factored in as a maintenance cost. During the first year, device titration process for therapy initiation, comprehensive care by health professionals, and initial education on device use costs were included. After the first year, the patient only requires a follow-up visit to a specialized physician and respiratory therapist. Details of the monitoring costs can be found in the supplementary material (Tables S1 and S2).
The healthcare resource utilization for the health events identified through the literature search were validated by clinical experts [Citation27–31]. The costs of health events were estimated using the bottom-up approach – unit costs of all medical procedures and treatments aggregated to obtain the total costs of a health event – and only direct medical costs were included in this analysis because the analysis was conducted from a third-party payer perspective. The valuation of unit resources included in the costs of the health events was performed according to the IETS recommendations [Citation13]. For health-care professional visits, laboratory and imaging tests and hospital stay, the national tariff manual (known as ISS Citation2001) was used with an increase of 30% as instructed in the guidelines [Citation13,Citation32]. Regarding medicines, the costs were obtained from the Drug Price Information System (Sismed) [Citation33]. All costs were expressed in 2020 Colombian pesos (COP$) and American dollars (USD$). The exchange rate used in the analysis was COP$ 3,466 per dollar. In the model, once the patient presents an event such as stroke or AMI, acute event costs were used, and then, in survivors, the cost of care required during the health state defined as post-event was applied. Detailed information regarding the use of resources and cost of each event can be found in the Supplementary Material (Table S3-S6). An overview of costs used in the economic evaluation is shown in .
2.4. Cost-utility analysis
The cost-utility analysis was conducted for a lifetime horizon, and a discount rate of 5% per annum was applied for both costs and outcomes as recommended by IETS [Citation13]. The outcomes were combined into a single metric, quality-adjusted life years (QALY). The utility values for the OSA patients with and without CPAP were obtained from a study previously published by McDaid et al and measured by EQ-D instrument (EuroQoL Group) [Citation11,Citation14]. In the absence of no reported utilities for OSA patients with stroke and AMI, the utility values of the stroke and AMI states were calculated as a fraction of that of the OSA state (treated and not treated) by applying adjustment factors of 0.8 and 0.9, respectively. The rational for applying these multipliers is based on the reported reduction in utilities for stroke and AMI compared to full health state [Citation14,Citation34]. To estimate utility associated with road traffic accidents (RTA), the same assumption of the original model was applied, which was to consider an average between AMI and OSA status, both in treated and untreated patients [Citation14]. The measure of cost-utility was incremental cost-effectiveness ratio (ICER) expressed as the additional cost per QALY gained when one therapy is compared to another. ICER allows to judge whether an intervention is cost-effective by comparing with the maximum willingness to pay (cost-effectiveness threshold) defined by the policy makers. ICER was calculated and compared against the cost-effectiveness threshold estimated for Colombia, which is 86% of the GDP per capita according to the first approximation of the supply-based cost-effectiveness threshold under a managed health system made in the study by Espinosa et al. [Citation10]. As suggested by the IETS, the GDP per capita reported by the Central Bank data was considered (COP$ 23,060,457, USD$ 6,653 preliminary data for 2021) [Citation35], resulting in a threshold of COP$ 19,831,993 (USD$ 5,722).
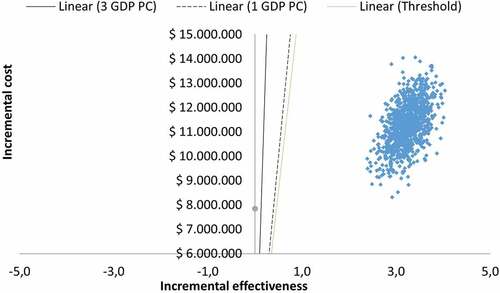
In the cost-utility analysis, patient’s adherence (using therapy as prescribed) to the therapy and compliance (proportion of patients who continue with their CPAP) is assumed to be 100%, but a sensitivity analysis was included to evaluate the impact of different levels of compliance to treatment on the results (). A sensitivity analysis was conducted for a more conservative horizon of 5 years. A univariate deterministic sensitivity analysis was performed to analyze the impact of uncertainty in the transition probabilities of CPAP use. A deterministic multivariate sensitivity analysis was also performed, where a scenario was modeled by increasing the transition probabilities of events where CPAP had a lower transition probability compared to no treatment, in that case, all the upper limits of the 95% confidence intervals (CI) of the transition probabilities for CPAP were taken to obtain a new result. A scenario analysis was also performed, in which the utilities of the events were assumed to be identical (the non-treatment utilities were taken). A probabilistic sensitivity analysis was developed through second-order Monte Carlo simulations (1,000 iterations) to understand the uncertainty around the estimated ICER value. The probabilistic sensitivity analysis took into account the variability of all variables within their probability distributions, including transition probabilities. A gamma distribution was used for variables whose values are greater than zero, and a beta distribution was used for those ranging from zero to one.
2.5. Budget impact analysis
For the budget impact analysis, a 5-year period was considered covering years 2022–2026. For the calculation of eligible patients (≥40 years of age), the population projections of the National Administrative Department of Statistics (DANE) were considered. The rate of insured population was reported as 92% in the affiliate’s database (BDUA) [Citation36].
The prevalence of OSA was obtained from the study by Ruiz et al [Citation7] (19.0%) and a sensitivity analysis was conducted by using a higher prevalence rate reported by Benjafield et al [Citation6] (49.6%). The underdiagnosis rate of OSA is reported in the range of 94–99% [Citation37–40]. Recent research developed in the United States refers to an underdiagnosis of 80% [Citation41]. Given the high coverage levels of the healthcare system, a lower rate of underdiagnosis is expected in the Colombian context; therefore, we used the 80% in our analysis. The literature search identified that 52–71% of the cases are moderate to severe, as reported in studies conducted in Latin America [Citation6,Citation42–45]. For the present analysis, an input of 52% was used, which corresponded to the data reported for Colombia by Benjafield et al [Citation6].
The budget impact analysis of providing CPAP therapy to the defined patient cohort in Colombia with an assumption of market uptake of 20%, 30%, 40%, 50%, and 60% over the five years was conducted. A compliance rate (proportion of patients who continue with their CPAP) of 79% as reported in different studies was considered [Citation14]. For compliant patients, the costs of the device and monitoring throughout the analysis horizon were included in the calculations. For non-compliant patients, only the costs of the device and monitoring during the first year were included. The total cost of the device was assumed in the first year considering the lifetime of the device (5 years). The subsequent years, only follow-up visit to a specialized physician, respiratory therapist and consumable costs were considered.
The risk of developing RTA, stroke and AMI for non-compliant patients is assumed to be equal to untreated patients.
2.6. Key model assumptions
Key assumptions of the model included the following: 1) The patient who survives the event of a road traffic accident returns to the OSA health state so that no other permanent sequelae related to RTA were modeled. 2) Transition probabilities were obtained from the literature and are not discriminated by severity level. 3) Probabilities of events (AMI, stroke, traffic accidents) are assumed constant over time. 4) Adverse events were not included because previous studies have reported that they are mild and have a low cost. Therefore, they were excluded from the analysis. 5) Due to the need to change the device every five years, the acquisition costs were included in the model every five cycles (years). 6) Diagnostic costs were not included as this is a cost applicable to both the intervention and the comparator.
3. Results
3.1. Cost-utility analysis
Cost-effectiveness analysis showed an incremental cost of COP$ 11,254,346 (USD$ 3,247) and a gain of 2.85 LYs and 3.21 QALYs with the CPAP therapy compared to no treatment (ICER: COP$ 3,503,804, USD$ 1,011). Results showed that CPAP was a cost-effective intervention compared to no treatment in the Colombian setting since the ICER obtained was below the threshold of 86% of GDP per capita ().
Table 2. Discounted base case cost-effectiveness results (outcomes and costs discounted at 5% per year).
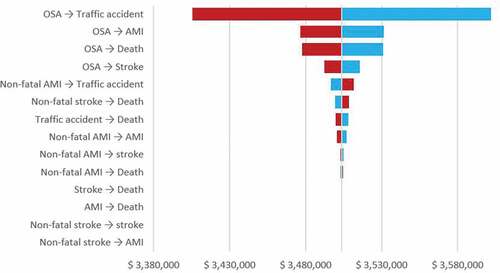
When sensitivity analysis was conducted for a more conservative horizon of 5 years, CPAP continued to be a cost-effective intervention compared to no treatment (ICER: COP$ 5,067,733, USD$1,462 per QALY gained). The univariate deterministic sensitivity analysis shows that the probability of suffering a traffic accident without any previous event has the greatest impact on the uncertainty of the outcome (). When multivariate analysis is performed taking the upper bounds of the CI of the CPAP transition probabilities CPAP continues to be a cost-effective intervention compared to no treatment (ICER: COP$ 3,659,757, USD$1,056 per QALY gained).
When a scenario analysis is performed in which the event utilities were assumed to be identical, CPAP continued to be a cost-effective intervention compared to no treatment (ICER: COP$ 5,295,373, USD$1,528 per QALY gained). The ICER was inversely proportional to compliance, and the results were more favorable as the proportion of compliant patients increases ().
Table 3. Influence of patient compliance with the CPAP therapy on results.
A probabilistic sensitivity analysis (PSA) was also performed to understand the uncertainty around the estimated ICER value. Based on the probabilistic sensitivity analysis, all simulations () are in the northeast quadrant and below the willingness-to-pay threshold. Therefore, CPAP was a cost-effective alternative from the perspective of the third-party payer. The probability of being a cost-effective intervention was 100%, even for the lowest willingness to pay evaluated (Figure S1 of the Supplementary material)
3.2. Budget impact analysis
Budget impact analysis estimated that 348,440 to 384,298 patients would be candidates for CPAP for the year 1 and 5, respectively (). Under the proposed scenario, the use of CPAP in patients with OSA would have a net budget impact of COP$ 411,722 million (USD$ 118,784,412) in the period 2022 to 2026. This value represented an investment of COP$ 4,383 (USD$ 1.30) per member per year. The savings were related to fewer health events (stroke and road traffic accidents). In the sensitivity analysis, we considered a higher prevalence rate of moderate to severe OSA (25.8%), which then would require an investment of COP$11,443 (USD$ 3.30) per member per year
Table 4. Budget impact of CPAP for the treatment of OSA in the Colombian Health System.
4. Discussion
Our analysis showed that CPAP therapy is a cost-effective intervention for treating OSA from the third-party payer perspective in the Colombian setting. According to the sensitivity analysis, the intervention has a high probability of being cost-effective with the recently proposed threshold (86% GDP [Citation10]). We used the ‘no treatment’ as a comparator arm to assess CPAP benefits. This comparison is acceptable because CPAP is the recommended first-line therapy in patients with moderate to severe OSA [Citation46,Citation47].
To the best of our knowledge, this study is the first of its kind that evaluates the cost-effectiveness of CPAP therapy in patients with OSA in Colombia. CEA already published have found that CPAP is a cost-effective alternative versus no treatment in patients with moderate to severe OSA [Citation48–50]. For example, in the study carried out in the United States, the ICER obtained was USD$ 15,915 per QALY gained (2008 prices) [Citation48]. In a similar study conducted in Australia, the cost per DALY avoided was USD$ 12,495 over a 5-year horizon (2017–18 prices) [Citation49]. In the UK context, the cost-effectiveness of CPAP versus no treatment over a 14-year horizon reported that after two years, it started to be cost-effective with an ICER of £10,000 or less and became a dominant intervention after a 13-year horizon [Citation50]. The most influential parameters in those studies were the cost of CPAP therapy and the proportion of patients who continue using CPAP.
In the model, we only considered the effects of the intervention on the most common health conditions, although other studies have evaluated the impact on depression, diabetes and occupational accidents [Citation49]. The potential of reduction in these events with CPAP therapy when included in the analysis might lower the cost-utility ratio and budget impact. The costs of health events were estimated using the bottom-up approach.
The costs obtained, particularly for stroke and AMI events, were very similar to those reported in other studies [Citation51,Citation52]. Only direct medical costs were included in this analysis because the analysis was conducted from third-party payer perspective. The burden of the disease could be higher from a social perspective, considering the indirect costs related to the loss of productivity which were not included in our analysis and could be an opportunity for future research. In the current analysis, only the costs of emergency care and hospitalization were included for road traffic accidents. They may be underestimated because the long-term treatment and rehabilitation costs were not included. This might have led to lower estimation of cost savings due to reduction in traffic accidents.
The main problem with CPAP treatment is non-acceptance, low adherence and low compliance due to discomfort or nasal problems [Citation1,Citation9,Citation53]. In the base case cost-utility analysis, patient compliance to CPAP was considered 100% because in integrated patient care programmes provided to these patients, periodic follow-up is performed, and the device is discontinued for those who do not comply adequately [Citation54].
There are some other limitations related to our study. In Colombia, CPAP is approved for the treatment of patients with OSA who meet the criteria for PAP therapy [Citation8]. Those criteria include moderate to severe and mild patients with excessive sleepiness, impaired sleep-related quality of life, and hypertension as comorbidity [Citation8]. In our analysis we only included moderate to severe patients and excluded eligible mild patients which might lead to lower estimate of the target population. Therefore, the results of the study should be interpreted with this in mind and updated as new evidence becomes available.
For the cost-effectiveness analysis, the utility values were based on previously published studies as there is no published information on the preferences of the Colombian population, which limits the generalizability of the results. Likewise, the worsening quality of life of the spouse is one of the critical aspects in quality of life estimation, since OAS can deteriorate relationships and affect their quality of sleep. This is a limitation of this study, which could be complemented in the future with epidemiological and quality of life information applicable to the local context. For the budget impact analysis, there are some limitations in the sources considered to quantify the target population. Although the target population defined for the baseline scenario might be underestimated – due to exclusion of eligible mild patients – it was considered acceptable since most of the patients prescribed with CPAP are moderate to severe cases. This limitation was addressed through a sensitivity analysis in which a higher prevalence of OSA is considered [Citation6]. The underdiagnosis of OSA in the local context has not been measured, so studies developed in other regions were considered. There is an uncertainty around the underdiagnosis rate used in our calculations which might not reflect the true underdiagnosis rate in Colombia. In the absence of regional information, the lowest value reported was used due to the high health-care system coverage [Citation36].
5. Conclusions
Our study showed that treatment of OSA with CPAP was cost-effective compared to no treatment. The estimated incremental cost-effectiveness ratio is below the threshold of 86% of 1 GDP per capita and could therefore be considered for funding by the health system. In the proposed scenario, adopting CPAP therapy would require a budget allocation that was partially offset by reducing strokes and traffic accidents. Cost-effectiveness analysis alongside a clinical trial in the Colombian setting could be considered as future research to identify more accurate cost-effectiveness and budget impact estimates.
Declaration of interest
Funding by this project was provided from ResMed Colombia. The research and reporting of the findings were in no way dictated or otherwise influenced by ResMed Colombia. Grants were paid to IQVIA. Y Gil-Rojas, D Amaya, F Hernandez and A Robles are employees of IQVIA, the company that was awarded the contract to conduct the study. F Escobar-Cordoba, M Venegas, J Echeverry and S Zabala declare a relationship with ResMed Colombia in all support for the present manuscript (e.g. funding, provision of study materials, medical writing, article processing charges, etc.). S Restrepo declare a disclosure for Advisory board RESMED to ACMES. M Bazurto-Zapata declare that ResMed paid ACMES for advisory board (Colombian Sleep Medicine Association). M Deger is a ResMed employee and owns ResMed Stocks. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Author contributions
A Robles contributed to the concept and design of the manuscript, acquisition, analysis, and interpretation of data and statistical analysis. Y Gil-Rojas and D Amaya contributed to acquisition, analysis and interpretation of data, drafting of the manuscript and statistical analysis. F Hernandez contributed to the concept and design of the study, logistic support, supervision and critical revision of the manuscript. F Escobar-Cordoba, M Venegas, S Amado, S Restrepo, J Echeverry and F Marin were involved in acquisition, analysis and critical revision of the manuscript. M Bazurto-Zapata, S Zabala, M Deger contributed to the concept and design of the study, acquisition of data, analysis and critical revision of the manuscript. All the authors and were involved in revising it critically for intellectual content and agreed with the final version of the manuscript to be published.
Supplemental Material
Download MS Word (95.8 KB)Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/14737167.2023.2181792
Additional information
Funding
References
- Labarca G, Cruz R, Jorquera J. Continuous positive airway pressure in patients with obstructive sleep apnea and non-alcoholic steatohepatitis: a systematic review and meta-analysis. J Clin Sleep Med. 2018;14(1):133–139.
- Mediano O, González N, Jm M, et al. Documento internacional de consenso sobre apnea obstructiva del sueño. Archivos de Bronconeumología. cited 2021 October 11 1–17. https://www.sciencedirect.com/science/article/pii/S0300289621001150
- Labarca G, Cruz N, Descalzi F. Multisystemic involvement in obstructive sleep apnea. Rev Méd Chile. 2014;142(6):748–757.
- Bioulac S, Franchi J-AM, Arnaud M, et al. Risk of motor vehicle accidents related to sleepiness at the wheel: a systematic review and meta-analysis. Sleep. 2017 1–10. [cited 2021 Oct 4]; https://academic.oup.com/sleep/article/40/10/zsx134/4049536?login=true
- Garbarino S, Guglielmi O, Sanna A, et al. Risk of occupational accidents in workers with obstructive sleep apnea: systematic review and meta-analysis. Sleep. 2016 39(6):1211–1218. [cited 2021 Sept 10]; https://academic.oup.com/sleep/article/39/6/1211/2453952?login=true
- Benjafield AV, Ayas NT, Eastwood PR, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019 7(8):687–698. [cited 2021 Oct 4]; https://www.sciencedirect.com/science/article/abs/pii/S2213260019301985
- Ruiz AJ, MAR S, Martínez PH, et al. Prevalence of sleep complaints in Colombia at different altitudes. Sleep Sci. 2016 9(2):100–105. [cited 2021 Oct 12]; https://pubmed.ncbi.nlm.nih.gov/27656274/
- Patil SP, Ayappa IA, Caples SM, et al. Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2019 15(2):335–343. https://jcsm.aasm.org/doi/pdf/10.5664/jcsm.7640
- Cortés-Reyes E, Parrado-Bermúdez K, Escobar-Córdoba F. New perspectives in the treatment of obstructive sleep apnea–hypopnea syndrome. Colombian J Anesthesiol. 2017 62–71. [cited 2021 Oct 4]; https://www.sciencedirect.com/science/article/pii/S2256208716300475
- Espinosa O, Rodriguez-Lesmes P, Orozco L, et al. Estimating cost-effectiveness thresholds under a managed healthcare system: experiences from Colombia. Health Policy Plan. 2022 [2021 Dec 08]; 37:(3):359–368. [cited 2021 Oct 8]; https://www.ncbi.nlm.nih.gov/pubmed/34875689
- Mar J, Rueda J-R, Durán-Cantolla J, et al. The cost-effectiveness of nCPAP treatment in patients with moderate-to-severe obstructive sleep apnoea. Eur Respir J. 2003 21(3):515–522. [cited 2021 Sept 10]; https://erj.ersjournals.com/content/21/3/515.short
- Salomon JA. Valuing Health States, Techniques for. Encycloped Health Econ. 2014;3:454–458.
- Instituto de Evaluación Tecnológica en Salud. Manual para la elaboración de evaluaciones económicas en salud Bogotá D.C: IETS 2014. Available from: https://www.iets.org.co
- McDaid C, Griffin S, Weatherly H, et al. Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea-hypopnoea syndrome: a systematic review and economic analysis. Health Technol Assess. 2009 25(62):1–162. [cited 2009 Sept 10]; https://europepmc.org/article/NBK/nbk56861
- Kim Y, Koo YS, Lee HY, et al. Can continuous positive airway pressure reduce the risk of stroke in obstructive sleep apnea patients? A systematic review and meta-analysis. PLoS One. 2016 1–14. [cited 2021 Sept 10]; https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0146317
- Khan SU, Duran CA, Rahman H, et al. A meta-analysis of continuous positive airway pressure therapy in prevention of cardiovascular events in patients with obstructive sleep apnoea. Eur Heart J. 2018 39(24):2291–2297. [cited 2021 Sept 10]; https://academic.oup.com/eurheartj/article/39/24/2291/4563763?login=true
- Antonopoulos CN, Sergentanis TN, Daskalopoulou SS, et al. Nasal continuous positive airway pressure (nCPAP) treatment for obstructive sleep apnea, road traffic accidents and driving simulator performance: a meta-analysis. Sleep Med Rev. 2011 15(5):301–310. [cited 2021 Oct 4]; https://www.sciencedirect.com/science/article/abs/pii/S1087079210001309
- Fu Y, Xia Y, Yi H, et al. Meta-analysis of all-cause and cardiovascular mortality in obstructive sleep apnea with or without continuous positive airway pressure treatment. Sleep Breathing. 2017;21(1): 181–189.
- Kim H, Joo E, Suh S, et al. Effects of long‐term treatment on brain volume in patients with obstructive sleep apnea syndrome. Hum Brain Mapp. 2016 37(1):395–409. [cited 2021 Sept 10]; https://onlinelibrary.wiley.com/doi/full/10.1002/hbm.23038
- Nadeau SE, Rose DK, Dobkin B, et al. Likelihood of myocardial infarction during stroke rehabilitation preceded by cardiovascular screening and an exercise tolerance test: the Locomotor Experience Applied Post-Stroke (LEAPS) trial. Int J Stroke. 2014 9(8):1097–1104. [cited 2021 Sept 10]; https://journals.sagepub.com/doi/abs/10.1111/ijs.12354
- Witt BJ, Ballman KV, Brown JRD, et al. The incidence of stroke after myocardial infarction: a meta-analysis. Am J Med. 2006 1–9. [cited 2021 Sept 10]; https://www.sciencedirect.com/science/article/abs/pii/S0002934305010715
- Smolina K, Wright FL, Rayner M, et al. Long-term survival and recurrence after acute myocardial infarction in England, 2004 to 2010. Circulation Cardiovasc Qual Outcomes. 2012 532–540. [cited 2021 Sept 10]; https://www.ahajournals.org/doi/full/10.1161/CIRCOUTCOMES.111.964700
- Ascari RA, Chapieski CM, da Silva OM, et al. Perfil epidemiológico de vítimas de acidente de trânsito. Revista de Enfermagem da UFSM. 2013 112–121. [cited 2021 Sept 10]; https://periodicos.ufsm.br/index.php/reufsm/article/view/7711
- Comunicación de aceptación de oferta convocatoria mínima cuantia MI 0044-DMORI-2021 [Internet]. [ cited August 30, 2021]. Available from: https://community.secop.gov.co.
- Replacement schedules for medicare continuous positive airway pressure supplies [Internet]. 2013 [cited 2021 Nov 8]. Available from: https://oig.hhs.gov/oei/reports/oei-07-12-00250.pdf.
- ResMed. CPAP replacement guidelines 2021 [2021 Nov 8]. Available from: https://www.resmed.com/en-us/healthcare-professional/products-and-support/monitoring-and-data-management/resupply/replacement-guidelines/
- Marques R, Mendes A, Leite MG, et al. Custos da cadeia de procedimentos no tratamento do infarto agudo do miocárdio em hospitais brasileiros de excelência e especializados. Revista da Associação Médica Brasileira. 2012 104–111. [cited 2021 Sept 8]; http://linkinghub.elsevier.com/retrieve/pii/S0104423012704761
- Escosteguy CC, Portela MC, RdA M, et al. O Sistema de Informações Hospitalares e a assistência ao infarto agudo do miocárdio. Revista de Saúde Pública. 2002 36(4):491–499. [cited 2021 Sept 8]; www.fsp.usp.br/rsp
- Araújo DV, Teich V, Passos RBF, et al. Análise de custo-efetividade da trombólise com alteplase no acidente vascular cerebral. Arq Bras Cardiol. 2010 95(1):12–20. [cited 2021 Sept 3]; http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0066-782X2010001100003&lng=pt&nrm=iso&tlng=en
- Christensen MC, Valiente R, Silva GS, et al. Acute treatment costs of stroke in Brazil. Neuroepidemiology. 2009 32(2):142–149. [cited 2021 Sept 3]; https://www.karger.com/Article/FullText/184747
- Gamboa AEH, Ardila YA. Clasificación de lesionados en tránsito, oportunidad en la atención y gasto hospitalario en una institución de salud de alta complejidad en el departamento de Santander (Colombia). Archivos de Medicina (Col). 2017;17(2):350–360.
- Instituto de Seguridad Social (ISS). Acuerdo N° 256 de 2001. Manual de tarifas TARIFAS de la entidad promotora de salud del seguro social EPS-ISS. Consejo directivo del instituto de seguros sociales. 2001. Available from: https://lexsaludcolombia.files.wordpress.com/2010/10/tarifas-iss-2001.pdf
- Consulta Pública de Precios de Medicamentos en la Cadena de Comercialización - Circular 2 de 2010. [Internet]. Available from: [ cited December 26, 2021]. https://web.sispro.gov.co.
- Torrance GW, Feeny D. Utilities and quality-adjusted life years. Int J Technol Assess Health Care. 1989;5(4):559–575.
- Producto Interno Bruto (PIB) [Internet]. Available from: [ cited September 6, 2021]. https://www.banrep.gov.co/es/estadisticas/producto-interno-bruto-pib.
- Bodega de datos Sispro: base de datos única de afiliados - BDUA [Internet]. 2021.
- Young T, Evans L, Finn L, et al. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep. 1997 20(9):705–706. [cited 2021 Nov 8]; https://academic.oup.com/sleep/article/20/9/705/2731634?login=true
- Durán-Cantolla J, Mar J, GdLT M, et al. El síndrome de apneas-hipopneas durante el sueño en España. Disponibilidad de recursos para su diagnóstico y tratamiento en los hospitales del Estado español. Archivos de Bronconeumología. 2004 259–267. [cited 2021 Nov 8]; https://www.sciencedirect.com/science/article/abs/pii/S0300289604755179
- Redline S, Sotres-Alvarez D, Loredo J, et al. Sleep-disordered breathing in Hispanic/Latino individuals of diverse backgrounds. The Hispanic community health study/study of Latinos. Am J Respir Crit Care Med. 2014 189(3):335–344. [cited 2021 Nov 8]; https://www.atsjournals.org/doi/full/10.1164/rccm.201309-1735OC
- Tan A, Cheung YY, Yin J, et al. Prevalence of sleep‐disordered breathing in a multiethnic Asian population in Singapore: a community‐based study. Respirology. 2016 21(5):943–950. [cited 2021 Nov 8]; https://onlinelibrary.wiley.com/doi/abs/10.1111/resp.12747
- Hidden health crisis costing America billions. Underdiagnosing and undertreating obstructive sleep apnea draining healthcare system [Internet]. 2016 Available from: [cited 2021 Nov 8]. https://aasm.org/resources/pdf/sleep-apnea-economic-crisis.pdf.
- Bakker JP, Weng J, Wang R, et al. Associations between obstructive sleep apnea, sleep duration, and abnormal fasting glucose. The multi-ethnic study of atherosclerosis. Am J Respir Crit Care Med. 2015 192(6):745–753. [cited 2021 Nov 8]; https://www.atsjournals.org/doi/full/10.1164/rccm.201502-0366OC
- Togeiro SM, Carneiro G, Ribeiro Filho FF, et al. Consequences of obstructive sleep apnea on metabolic profile: a population‐based survey. Obesity. 2013 21(4):847–851. [cited 2021 Nov 8]; https://onlinelibrary.wiley.com/doi/full/10.1002/oby.20288
- Ferreira E, Martinez D, Lasalvia A, et al. Exploring the STOP-BANG questionnaire for obstructive sleep apnea screening in seniors. J Clin Sleep Med. 2020 199–206. [cited 2021 Nov 8]; https://jcsm.aasm.org/doi/full/10.5664/jcsm.8166
- Tufik S, Santos-Silva R, Taddei JA, et al. Obstructive sleep apnea syndrome in the Sao Paulo epidemiologic sleep study. Sleep Med. 2010 11(5):441–446. [cited 2021 Nov 8]; https://www.sciencedirect.com/science/article/abs/pii/S1389945710000948?via%3Dihub
- Hidalgo-Martínez P, Lobelo R. Epidemiología mundial, latinoamericana y colombiana y mortalidad del síndrome de apnea-hipopnea obstructiva del sueño (SAHOS). Revista de la Facultad de Medicina. 2017;65(1Sup):17–20.
- Ám GÁ, Vélez van Meerbeke A, Venegas Mariño MA, Proceso clínico-administrativo para el diagnóstico de los pacientes con SAHOS: duración y costos. Acta Neurol Colomb. 2006;22:12–24. Available from: [ cited2021 Sep 10]. https://repository.urosario.edu.co/handle/10336/26801
- Pietzsch JB, Garner A, Cipriano LE, et al. An integrated health-economic analysis of diagnostic and therapeutic strategies in the treatment of moderate-to-severe obstructive sleep apnea. Sleep. 2011 695–709. [cited 2021 Sept 10]; https://academic.oup.com/sleep/article/34/6/695/2656963?login=true
- Streatfeild J, Hillman D, Adams R, et al. Cost-effectiveness of continuous positive airway pressure therapy for obstructive sleep apnea: health care system and societal perspectives. Sleep. 2019 ;1–11. Available from: [cited 2021 Sept 10]. https://academic.oup.com/sleep/article/42/12/zsz181/5546946?login=true
- Guest JF, Helter MT, Morga A, et al. Cost-effectiveness of using continuous positive airway pressure in the treatment of severe obstructive sleep apnoea/hypopnoea syndrome in the UK. Thorax. 2008;63(10):860–865. Available from: [cited 2021 Sept 10]. https://thorax.bmj.com/content/63/10/860.short
- Mendoza-Sánchez JA, Silva FA, Rangel-Celis LM, et al. Modelo de costos asociados al ataque cerebrovascular y los eventos adversos en pacientes con fibrilación auricular no valvular tratados con warfarina. Revista Colombiana de Cardiología. 2019 ;26(3):125–132. Available from: [cited 2021 Sept 10]. https://www.sciencedirect.com/science/article/pii/S0120563319300312
- Mendoza F, Romero M, Lancheros J, et al. Carga económica de la fibrilación auricular en Colombia. Revista Colombiana de Cardiología. 2020;27(6):538–544. Available from: [cited 2021 Sept 10]. https://www.sciencedirect.com/science/article/pii/S0120563319301937
- Bazurto MA, Herrera K, Vargas L, et al. Subjective factors associated with cpap non-adherence in patients with sleep apnea hypopnea syndrome. Acta Medica Colombiana. 2013;71–75. Available from: [cited 2021 Oct 11]. http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0120-24482013000200007
- Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnea: implications for future interventions. Indian J Med Res. 2010 1533;245–258. PubMed Central; PMCID: PMCPMC2972705. [cited 2010 Sept 10]; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2972705/