1. First, Julie, tell us about yourself! what’s your background and how did you get into the field of health economics?
I am a trained economist; I have a bachelor’s and master’s degree in economics, both from the University of Montreal. I have always been captivated by the health sector. My mother is a pharmacist, from a long line of pharmacists and health-care professionals, she instilled in me the importance of putting the patient first (she was promoting patient-centeredness even in the 60s). My father is an award-winning veterinarian. He has always told us to fight for our dreams and not to be afraid to go on the path less traveled.
I loved medicine but hated chemistry. I love people. Human beings fascinate and inspire me. I always wanted to make a difference. Not surprising that I love psychology, but I did not see myself as a therapist. I love numbers. I love making correlations between them whether they are on a license plate, an address, or on a credit card. When I attended my first microeconomic class, I fell in love with the field. Not surprising as this science combines ‘numbers’ and ‘behaviors.’ When my father asked me what I was going to do with this diploma, I told him I had no idea, but I just had to know more. It captivated me even more when I attended my 1st class of economic evaluation and realized that I could choose it as a specialty. At the time, I was in a student rotation program at Sandoz (now Novartis), and the term ‘pharmacoeconomic’ was a mystic buzz word that everyone was talking about but only a minority really understood it (not surprisingly, I am experiencing the same trend now with value-based health care (VBHC)). I eventually attended a class entitled behavioral economics. This is when I understood that I was a behavioral economist. I was not fascinated by the result or the complex process of generating it, but by the spectrum around results and the factors involved in the study, and thus interested in the questions ‘Why did we reach this result’? ‘Can we do better, if yes, how’? Clearly, one size fits all does not work in health care and we must move toward personalized medicine that works for all health-care stakeholders, including, most importantly, patients, as we are not treating budgets but patients with a health condition first. This field attracted me as it was regrouping all my interests: health, people, psychology, and numbers. There was so much to learn and explore to really make a difference for improving health-care systems. By the way, my favorite question has always been ‘why’? And it still is today.
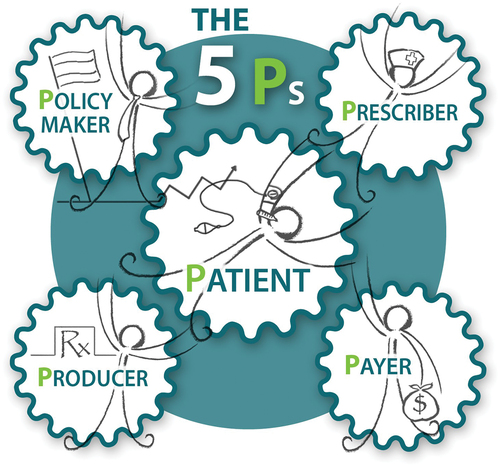
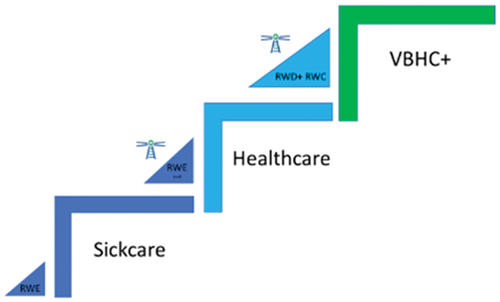
My career began as a student in the late 80s, working in outpatient medical clinics, pharmaceutical industry, followed by a period at the Québec Hospital association. I eventually became a consultant in the late 90s. I have worked on projects in Canada, U.S.A., Europe, Japan, and Oceania. I realized through my global experience that these health-care systems, although different, all encounter similar issues since they were all designed to address the need of sick care. It is not surprising that OECD wrote health reform recommendations in 2017 [Citation1] so that we can move from an acute care system (sick care) to manage value-based populational health. I also worked on one of the most exciting projects in the late 90s: the ICONS study [Citation2]. It has been one of my great inspirations for building TOWWERS™, with and for the 5Ps (). This study showed me that if designed properly, it was feasible to implement complex collaborative public-private initiatives to improve populational health and disability, where all stakeholders would benefit from this initiative. Being an iconic project for me, its name could not have been more suited.
I also had the privilege of teaching health economics at an MBA level for students specializing in the bio-industry. This was a breakthrough for me. For a long time, I was seeing more of a parallel between pharmacoeconomics and accounting (putting the right information in the right structure), rather than with economics alone. Through the students’ great questions, I realized that my passion and vision was about ‘health economics’, using a dynamic collaborative VBHC approach rather than pharmacoeconomics, which I was applying intuitively. This wasn’t surprising, as it was my training.
Economics, when applied to health, is a systemic approach about optimizing the collective utility curves of the stakeholders in the delivery of care over time using a Maxi-Min approach (maximizing the populational health subject to existing constraints – Appendix). My true passion has always been to design collaborative, meaningful post-market surveillance, through real-world evidence, patient management, and disease management programs. Why? It addresses the need of real-world actors that are struggling to manage uncertainty in terms of clinical relevance, value, and sustainability, and improve care gaps through a structured approach. Therefore, in my mind, it makes no sense that post-market surveillance is not mandatory to validate the alignment between the clinico-economic model results and real-world evidence designed to address the question: did we reach the goal? How can we close the gap? What is the goal of spending if we are not managing whether we reached the expected therapeutic goal? I truly believe that sub-therapeutic achievement is a greater enemy than over-treatment as it results in disease progression, and thus spiraling costs and significant distress on patients’ lives.
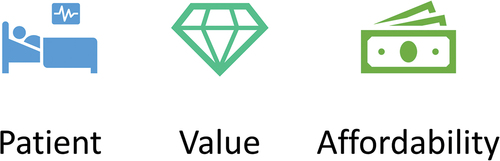
A great researcher once stated that ‘imperfect information is better than no information.’ I totally agree with that statement when we begin a process. This is why we need economic models to enlighten potential clinical and efficiency relevance. But models are models. They are usually based on randomized controlled trials (RCTs) and many, many, many clinical and economic assumptions need to be validated, or at least, the most significant KPIs leading to the expected value assessment. That works as a first step prior to moving on to the next generation of evidence. Most agree that we need to accelerate relevant innovation to the patient’s bedside. It is particularly frustrating for patients to wait many years for the reimbursement of a regulatory approved innovation that could be beneficial for them and for society now. A patient advocacy group once published: what is more frustrating? To be in the desert and being thirsty? Or being in the desert, thirsty and not being able to reach a bottle of water in front of you? We clearly need a smart system enabling to accelerate innovation to patient bedside, however the process must be respectful of the 5Ps (), within a triple aim approach (patient-centeredness, value, and affordability) (), or else it cannot remain sustainable.
Over the last 30 years of my career, I realized that the microeconomic theory of the relationship between the consumer, the producer, and the government can be translated to health care. I eventually evolved it to be the relationship between the 5Ps, the real-world actors involved in the process of optimizing health subject to the triple aim: Patients, Prescribers, Policymakers, Payers, and Producers of innovation.
Health evolves over time with complex conditions to diagnose and to treat, such as COVID-19, chronic disorders, cancer, and rare diseases. Developed countries implemented sick care half a century ago. Over the last 30 years, with the spiraling growing impact of chronic disorders and cost, most actors realized the importance of moving from a sick care toward a value-based health care (VBHC) [Citation1,Citation3] (). We need to modernize our health-care system to the reality of the 21st century – chronic disorders, the 5Ps, data, and the triple aim. It is impossible to move toward a health-care system if we do not have relevant health markers. It is unlikely that we will be able to reach a Pareto optimal state if the process toward VBHC is undertaken without structured collaboration, with and for the 5Ps, and measuring relevant KPIs.
By applying all my economic training and experience, as well as collaborating with visionaries over the past 10 years, my organization, Data 4 Actions, was able to create a system that could gradually transform a sick care into a collaborative VBHC anchored on real-world data (RWD) () reaching toward the triple aim, with and for the 5Ps. The first step for implementing this system is the willingness of the health-care government to move toward this goal and undertake structured collaboration with and for the 5Ps. We are privileged that the province of Québec believes in the importance of our vision. The first formal therapeutic indication endorsed was COVID-19. The wheels are now fully in motion as a new therapeutic indication is in discussion, where we will be addressing the issue of rare disorders and outcome-based agreements. We are excited to begin this new chapter, and dialogs are being open with other countries.
2. How are the 5Ps integral to TOWWERS™? What obstacles stand in the way of their goals?
Since the 80s, there has been a rapid rise in chronic disease and multiple morbidities, which is becoming one of the most pressing public health concern [Citation4]. The burden of illness has shifted significantly. Chronic and mental health conditions can represent up to 90% of a nation’s health expenditure [Citation5]. Unfortunately, meeting the complex needs of these patients is the single greatest challenge facing health-care systems. Meeting the triple aim appears to be an impossible task as costs are rising and many reports have revealed that sizable proportions of chronically ill patients have poor disease control, suffer financial toxicity [Citation6] and above all, are unhappy with their care.
The problem with chronic disorders is that if management is sub-optimal, it will impact on the triple aim as the chronic disorder is at higher risk of progressing and generating patient distress, requiring greater use of resources, and thus spiraling costs. I truly believe that ‘the best approach to cost savings is to improve health status,’ as reported by Dr Wanger in 1998 [Citation7]. We can no longer manage health by ignoring the existence of the 5Ps as a unit, the triple aim, and the need for data.
The 5Ps is an acronym for the five ecosystems representing real-world actors involved in the process of optimizing health-care value, where each ‘P’ as designated as the Patients, the Prescribers/Providers of health care (individuals or establishments), the Producers (Pharmaceutical companies, biotech’s, and medical device makers, digital health), Policymakers (not just governments) and Payers.
The biggest obstacle the 5Ps face is that they all have different business missions. Therefore, most believe that it is impossible to collaborate in a sustainable manner. I strongly believe that it is feasible to build such a system, the TOWWERS™ system for instance, where they all have an incentive to row in the same team, moving toward a common goal: C-VBHC-RWE () reaching for the triple aim, as the 5Ps all agree on these underlying assumptions:
The starting point is the patient, rather than budgets.
We need populational data for managing uncertainty and delivering outcomes that matter with and for the 5Ps.
We need to aim for clinical relevance – if a treatment pattern is prescribed to the patient, the goal is to reach a complete therapeutic response.
We should be asking ourselves if we are spending wisely (clinico-economic relevance)
We need to recognize that health, or a given health condition, is a priority but not the only priority for a society (e.g. education, transportation,…) and that funds are not illimited (sustainability/affordability).
Very often we ask the question, ‘value for who?.’ As reported by WHO [Citation3], value should not be limited to certain dimensions or stakeholders, but value for the 5Ps. The diversity of the group, through structured collaboration and data, is what will enable us to aim for a Pareto optimal journey. So how do we tackle this? By building a structured approach, with and for the 5Ps, to address the following questions, for each therapeutic indication:
What are the goals?
What are the KPIs?
Did we reach the goal?
How can we close the gap? How can we do better?
Are we spending wisely?
As reported by WHO [Citation3], ‘moving towards a value-based health system will often be a gradual process, focusing first of all on the areas where it might make the biggest difference.’
3. Can you explain the aims and mission statement of TOWWERS™?
Our systems have been designed 50 years ago to address sick care for acute care events, where chronic disorders and digital era were just a blur, silos appearedFootnote1 adequate for managing acute care, and health-care budgets were much more reasonable, representing 10% of today’s budget [Citation8].
Imagine if we managed the success of students based on the amount of time they were out of school, went to see the school principal or went to detention. This is how we manage health. Data tells us what is happening in the health-care system, but it does not tell us how well we are doing. The health-care industry is data rich but information poor. In the education system, we have a specific test per subject. Clearly, we will not have the same exam in French and in math. Just like we will not have the same KPIs to assess the therapeutic success of diabetes and cancer.
When we address chronic disorders, we should understand that the 5Ps are part of a unit, a team, to optimize the triple aim. The unit is fragmented into pieces. As reported by WHO, an ‘effective governance of the whole health system is needed to ensure that stakeholder perspectives and policy levers are aligned to promote a common concept of health system value and, ultimately, of societal wellbeing’ [Citation3]. This is what we refer to as structured collaboration so that we can all be aligned to act as a system. Just like American football, each player must be aligned for the success of each play, or it could significantly hinder the success of the play tactic if one player chooses to do otherwise.
Hence, TOWWERS™ is a Real-World System. Our mission is to bring relevant people and data together to solve the complex problem of transforming health-care systems to the reality of the 21st century, by reaching for the triple aim, in a progressive manner, over time, respectful of the 5Ps. The aim of the TOWWERS™ System is to deliver Real-World Evidence and structured governance, with and for the 5Ps, and then transform this information to guide the Real-World Actors toward meaningful improvements.
4. What are some of the early achievements of TOWWERS™?
In 2017, ISPOR’s 21st annual international meeting theme was ‘Value, affordability, and patient centeredness: Can we have it all’? () and CADTH was ‘Measuring value in theory and the real world’ (). The answer to both themes, yes, it is feasible if we modernize how we collaborate and how we manage real-world data. Our first step was to show that it is feasible, in theory.
Our system enables us to balance the triple aim, with and for the 5Ps, making it Pareto optimal (win–win) for the 5Ps.
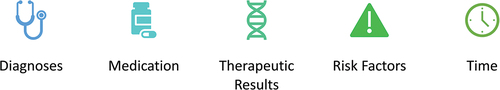
This system has been endorsed by the Québec government to begin this initiative. The first therapeutic indication, COVID-19, was our MVP for registering patients and health-care providers, and generating various dashboards and real-world evidence. The platform enables us to link diagnoses, therapeutic plans, health results, and risk factors for all officially open therapeutic indications.
A 3in1 RWD platform has been developed:
Patient portal that enables to track patient journey over time
Shared decision-making tool [Citation9] (by linking relevant health-care providers to the patient portal)
Value-based health-care platform to link therapeutic plan to therapeutic results (Value-based-RWE)
Establishing the first and only populational Real-World System built with and for the 5Ps that allows health data and information to follow the patient over time.
Getting the support from key stakeholders in the health sector such as governments, medical associations, patient advocacy groups, several big pharma companies, and other champions [Citation10].
Hosting and serving the first strategic committee involving the 5P+ so that we can begin to gradually implement transformation of our sick care C-VBHC-RWE. The highlights of this meeting can be read in Expert Review of Pharmacoeconomics & Outcomes Research [Citation10].
TOWWERS™ is invited to present in Japan, U.S.A., Columbia, multiple provinces in Canada, patient advocacy groups and academic environment.
We are in the process of opening a new therapeutic indication (rare disorders) to tackle a strategy leading to outcome-based agreements.
Discussions with various recognized leaders to implement our showcase project.
5. Are there any achievements that stand out to you as being particularly instrumental to the success of TOWWERS™?
All moments leading up to the first patients enrolled have been equally important, and each step has been conditional for the next step to happen. Creating the action plan from the OECD reform [Citation1] was already a significant achievement.
Our biggest hurdle was the quote: ‘Perfection is the enemy of done.’ Too often, people mistake progress for perfection. We are grateful to champions that were able to convince other champions of the need to begin the process on a solid basis and improve as we move forward.
Finally, maybe my most significant achievement is when I explain to citizens and organizations what we do and many answer: ‘it’s about time!.’ I always take this moment to ask my favorite question: ‘why’? This really gives me the courage to keep moving forward and improving the process.
6. Why do patient access issues remain an enigma?
In my opinion, patient access issues exist for four key reasons.
It requires much time, work, and clinical knowledge to complete some of these health profiles. This is why patients can fill their health profile, and it can be validated by their health-care professionals with whom they are linked in the portal. It is a good start for becoming an informed patient partner.
The patient seldom benefits from all the work they put into it. It serves others involved: Physicians, Payers, Policymakers, Innovators, so why bother?
The lack of data that enables us to manage uncertainty, and that enables us to link therapeutic plans to therapeutic results over time. Stakeholders need to recognize that real-world actors need information to optimize decision-making. It was important to build a system that would be beneficial and respectful for all parties and patients first.
Data privacy. We considered these points carefully when developing our platform and its data governance that aims the highest standards designed with and for the 5Ps. When signing up in TOWWERS™, the patient can fill out the complete questionnaire in less than 3 min. The patient instantly receives their personal health profile, COVID-19 Vulnerability Index, and their Ideal Health Index to aim toward. The portal is free and aims to serve the patient throughout their life. All their health information can be in one place. TOWWERS™ is easy to find, and easy to share with a caregiver or various health-care professionals. But the personal information belongs to them, and only to them, unless they choose to share it with the health-care providers of their choice, who are registered within the TOWWERS™ platform. At any time, patients can revoke this link, with one or all their providers.
7. How have you overcome concerns regarding data privacy?
As for data privacy, we take this point very seriously. Ethics and Cybersecurity are at the heart of our priorities. Using my 30 years’ experience, including working on post-market surveillance trials of all sorts, I have tried to make TOWWERS™ as agile as possible, to get the best of the data the 5Ps need while always respecting ethics and privacy as our number one concerns. We use a consent form and explain to patients that data from TOWWERS™ is aggregated to identify trends. It is very important that patients, and other stakeholders, are educated about TOWWERS™ and its trend data. We worked to find the most secure system possible to store our data, which was designed by a Google architect, but the system has always been owned by us.
Today, with modern platforms, there is no reason to go into the database, see and manipulate the data, if the database architecture has been accurately designed. Through algorithms and analytical AI, we can make all the queries within a safe environment. The platform was designed using the most modern systems. We are also continuing our data governance structure, through our strategic committee that will respect the highest ethics with regard to data without compromising the ability to produce meaningful dashboards and real-world evidence to close our health-care system’s care gaps for reaching C-VBHC-RWE balancing the triple aim. At the core, we are patients first focused on outcomes, as we are building a patient portal so that they can optimize their health over time.
8. How can TOWWERS™ help reduce waste involved in health-care?
Advances in science and technology drive health care forward fast. Unfortunately, if we don’t understand how to value these advancements, and how much each innovation is worth [Citation11], then we are driving a beautiful sports car with our eyes closed, as reported by one of our experts during TOWWERS™ 1st strategic committee [Citation10].
As Peter Druker would state, ‘what gets measured gets managed.’ If we do not have a structured system that enables us to track and define therapeutic response, it becomes complicated to manage waste, where we define waste management as maintaining the patient with a given therapeutic plan that generates suboptimal results.
To fully realize the promise of science and ensure patient benefit, structured real-world collaboration is necessary. With the 5Ps united around clear goals they have set to reach, TOWWERS™ can assess wastage by determining the proportion of responders to an intervention:
Complete responders
Partial responders (where we can have many levels)
Non-responders
As you can gather by the logo and by its name (), TOWWERS™ is a lighthouse. We intend to help reduce waste involved in health care by lighting the road toward the set goals by the 5Ps. By identifying them we can cast our light on exactly where it is needed (via data transformed into information) and keep each real-world actor aware of the lit path without getting lost or left behind.
TOWWERS™ is a lighthouse: illuminate the path, guide toward a safe haven to improve the care gaps so that we can get back on the road toward yet again a new journey. To do so, we need to bring all the relevant stakeholders around the table and assess:
What are the goals? Did we reach the goal? How can we close the gap?
We need to flip our thinking from spending to clinical relevance and then question the clinico-economic relevance and sustainability.
9. How can TOWWERS™ help support future innovation on a sustainable scale? And how can working with real-world data be utilized to resolve uncertainty?
TOWWERS™ is supporting future innovations on a sustainable scale by enabling a structured risk- management agreement, based on RWD where goals and KPIs specific to therapeutic indications will be established with and for the 5Ps. By establishing a clear, structured monitoring process real-world issues are mitigated, and the acceleration of innovations to the patient bedside is optimized in a Pareto efficient state.
The story behind TOWWERS™ is that three projects that I was working on were refused by three different HTA organizations. Rejection was not only based on the clinico-economic results but mostly on disagreement about clinical and economic assumptions. In the rejection of these three projects, it was clear to me that we needed patient representation (alongside physicians and government) in the form of a collaborative committee, to ensure that patient outcomes were centered in these decisions. I am convinced that if we had the TOWWERS™ system, these great products would be making a difference for many patients.
My dream is that TOWWERS™ can eventually lead to quicker regulatory approval and almost immediate HTA approval thereafter, where these would be conditional to post-market surveillance according to a structure that would be validate with and for the 5P for reaching the triple aim. Why? Because it can align actors and manage uncertainty. The FDA and other regulators have employed this accelerated approval conditional to post-market surveillance for medical devices for some time. The same process has been observed for COVID-19 vaccines. Unfortunately, governments did not impose post-market surveillance to track health outcomes over time. A system such as TOWWERS™ could have brought significant value to all real-world actors by easily capturing real-world data, and by linking public health and clinical care during this pandemic. For instance, by having a better profile of ghosted high-risk patients (those with non-controlled or multiple chronic disorders [Citation12]), tracking and assessing persistent symptom status and finally tracking asymptomatic patients that develop over time new symptoms that lead to premature chronic disorders.
We need a system where we can build a bridge to innovators, health-care providers, and patients so that the innovation can cross the ‘valley of death,’ the bridge linking therapeutic plans to therapeutic results. This bridge must represent a structured system that enables us to address uncertainties between the innovators and the other real-world actors, including policymakers (regulators). This system must be implemented for and with these real-world actors so that we can transform subjective facts (‘I think that …’) into objective facts (‘it has been shown that …’). Moreover, it is critical that we can understand why we reached these suboptimal results and determine whether we can close the care gap, not be a victim of the initial results. Economics is not a static science as it aims to optimize results over time. In health care there are many players and silos that could impede the expected health outcome. The TOWWERS™ system aims to capture important parameters that can be simply captured by patients and health-care providers to assess trends and address the question: are we reaching the goal? Eventually, we really hope that TOWWERS™ will be able to trigger more interoperability between the systems and thus empowering the information captured within the system.
TOWWERS™ aims to become the real-world system for real-world actors during the C-VBHC journey to improve health and wealth of a nation. The system that enables us to first ask the question: ‘what are the goals?’ Rather than ‘how much?’ and then optimize the implementation process to answer the question and close the care gap to balance the triple aim.
The biggest opportunity cost is not spending too much, the biggest opportunity cost is not reaching the goal as these patients are at higher risk of complications and disease progression. Spending too much can then become the next quest for patients that reached their goals. Real waste is a sub-optimal therapeutic achievement as we are spending blindly.
10. Do you anticipate any difficulties transitioning TOWWERS™ from a regional level to a national level?
All health-care systems are different, but all systems are encountering the same issues since they were all designed to address the need for sick care.
We converted our data collection form and modeling experience to generate a system that could be exportable. We track diagnoses, therapeutic plans, health markers (results), and risk factors. These are all international parameters, non-healthcare system specific.
Obviously, some minor adjustments will be required to adapt to the reality of each jurisdiction. At this point in time, we do not expect any structural difficulties.
TOWWERS™ system is a completely new structure that eventually leads to inter-operability when policymakers will feel comfortable with data governance and underlying standards to optimize cybersecurity features. We are aware that change management will be the most important factor to manage over time in line with building data and collaboration governance. It then becomes important to begin with countries that are willing to modernize how we manage data and collaboration and adapt to the reality of the 21st century. It is a process wherein we must tailor the speed accordingly to the readiness for change for the real-world actors. Change is not easy. However, the feedback is so encouraging that it gives us wings and courage to move forward. There is an African proverb that says ‘if you want to go fast, go alone. If you want to move far, go together.’ Our goal is to build the journey where TOWWERS™ will become the standard and where actors will be asking ‘what were do doing before TOWWERS,’ just like people are asking the same question with cell phones.
Our process involves presenting and publishing the ongoing evolution of the TOWWERS™ system on regular basis with and for the 5Ps. Interest in opening new therapeutic indications and discussions with various policymakers in various countries over time clearly shows the willingness to add a new system to improve health and wealth of a nation.
11. Looking further afield from COVID-19 and the pandemic, what other therapy areas do you hope TOWWERS™ might be able to have success in?
COVID-19 could not have been a better first therapeutic indication to begin the exercise. Data are rather straight-forward, and there is a clear need for the 5Ps for data on:
Vaccination outcomes over time.
COVID-19 outcomes over time. Will persistent symptoms translate into chronic disorders? Do asymptomatic patients eventually develop symptoms or chronic disorders?
Linking public health and clinical care: prevention and managing persistent symptoms.
COVID also showed that it is possible to have all the 5Ps working toward an agreed common goal.
Serious discussions are underway to open a new therapeutic indication, rare diseases, where we will tackle the process to optimize outcome-based agreements. Some serious discussions have also started with a country in South America to open cancer therapeutic indication. Finally, other discussions have begun to tackle racial disparities for managing primary care. These are all such exciting endeavors that we are looking forward to improving tomorrow’s health.
So how do we tackle health-care transformation? The same way we eat an elephant: one bite a time. Thus, in this case, one therapeutic indication at a time. One country at a time.
12. What are the next steps and future goals for TOWWERS?
We opened the first therapeutic indication for TOWWERS for our MVP: COVID-19 in the province of Québec. We are really interested in the long tail with COVID-19. What happens to patients that had COVID-19; persistent symptoms, vaccination health trends over time (health, development, etc.)? Our goal is also to open new jurisdictions not only in Canada but globally.
One of our next steps is to promote the importance of longitudinal populational data (health and economic) not specific to science but to inform real-world actors (the 5Ps): ‘Did we reach the goal’? If no, ‘how can we close the gap’?
Our aspiration? We want to become the partner of success of all countries that wish to move toward VBHC reaching for the triple aim through structured collaboration and data.
Amongst the OECD’s recommendations is the adoption of innovation. We believe that the TOWWERS™ system can enable a mechanism where we can accelerate time to market, time to reimbursement by managing uncertainty (clinical and economic) through a structured dynamic post-market surveillance process where all the 5Ps will reach for the triple aim and all will reside in a win–win).
Disclaimer
The opinions expressed in this interview are those of the interviewee and do not necessarily reflect the views of Taylor & Francis.
Declaration of interest
J Frappier is the president and founder of TOWWERS™ and Data 4 Actions Inc. The author has no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or conflict with the subject matter or materials discussed in this manuscript apart from those disclosed.
Acknowledgments
This interview was conducted by Sophia Aldwinckle, Commissioning Editor of Expert Review of Pharmacoeconomics & Outcomes Research. Thanks to Edward Spofford (Taylor & Francis) for preparing the questions and support. Thanks to Priti Nagda (Taylor & Francis) and Rayya Hajjar (Taylor & Francis) for support.
Additional information
Funding
Notes
1. “Appeared » being the relevant term as we still know today that some acute events are big problems that are we still trying to address such as antibiotic resistance and opioid crisis.
References
- OECD H. The next generation of health reforms: ministerial statement. Paris; 2017. https://scholar.google.ca/scholar?hl=en&as_sdt=0%2C5&q=The+next+generation+of+health+reforms+ministerial+statement&btnG=
- Montague T, Cox J, Kramer S, et al. Improving cardiovascular outcomes in Nova Scotia (ICONS): a successful public-private partnership in primary healthcare. Hosp Q. 2003;6(3):32–38. doi: 10.12927/hcq.16498
- Smith PC, Sagan A, Siciliani L, et al. Building on value-based health care: towards a health system perspective. 2021.
- Geda NR, Janzen B, Pahwa P. Chronic disease multimorbidity among the Canadian population: prevalence and associated lifestyle factors. Arch Public Health. 2021;79(1):60. doi: 10.1186/s13690-021-00583-7
- Buttorff C, Ruder T, and Bauman M. Multiple chronic conditions in the United States. Vol. 10. Rand Santa Monica CA; 2017. https://scholar.google.ca/scholar?hl=en&as_sdt=0%2C5&q=Buttorff+Ruder+Bauman+Mutliple+chronic+conditions+in+the+united+states+2017&btnG=
- Abrams HR, Durbin S, Huang CX, et al. Financial toxicity in cancer care: origins, impact, and solutions. Transl Behav Med. 2021;11(11):2043–2054. doi: 10.1093/tbm/ibab091
- Wagner EH. Chronic disease management: what will it take to improve care for chronic illness?. Effective Clinical Practice. 1998;1(1).
- ICIS-CIHI. Tendances des dépenses nationales de santé, 2022. 3 nov 2022; Available from: https://www.cihi.ca/fr/tendances-des-depenses-nationales-de-sante-2022-analyse-eclair
- The SHARE approach—achieving patient-centered care with shared decisionmaking: a brief for administrators and practice leaders https://www.ahrq.gov/health-literacy/professional-training/shared-decision/tool/resource-9.html
- Frappier J, Krelenbaum M, Villalba E, et al. Kick-off meeting of the TOWWERS showcase project: 1 st collaborative value-based healthcare anchored on real-world data involving the 5P+. Expert Rev Pharmacoecon Outcomes Res. 2022;22(5):711–715. doi: 10.1080/14737167.2022.2055549
- Jimenez J. Why the approach to drug pricing has to change now. forbes. com. 2016 Nov;1.
- Shmerling RH. COVID-19: if you’re older and have chronic health problems, read this, H.H.P.-H.M. shcool, Editor. 2020.
- Frappier J. The ABC,s of pharmacoeconomics: a reference guide. 2001 Nov.
- Berwick DM. Measuring NHS productivity. BMJ. 2005;330(7498):975–976. doi: 10.1136/bmj.330.7498.975
- Teisberg E, Wallace S, O’Hara S. Defining and implementing value-based health care: a strategic framework. Acad Med. 2020;95(5):682. doi: 10.1097/ACM.0000000000003122
Appendix
Textbook micro-economics is about the relationship between three ecosystems: consumers, producers, and governments. Economics is an efficiency concept. The underlying premise is that resources are scarce and that stakeholders must make choices/trade-offs, implicitly or explicitly. Therefore, economics is a science that analyses the different choices in order to optimize the well-being of a given stakeholder or a collective group subject to existing constraints [Citation13]. “The economic theory comprised two sub-concepts, both of which respected the efficiency criteria depending on the primary established goal: The Mini-Max and the Maxi-Min. The Mini-Maxi approach is most used in the current healthcare system” [Citation10]. “One first establishes the allowable budget and then aims to achieve the best possible result with the given funds. TOWWERS™ seeks to transform this vision and invert the process by implementing the second, Maxi-Min. approach. The initiation point is no longer “how much money is available?” but rather, “what is the goal?”, and with that goal in mind, what are the reasonable resources that are required to achieve that intended goal?, as stated by Berwick [Citation14]. Most importantly, the maxi-min asks the question: did we reach the goal? If not, how can we close the gap, if required? Hence, the Maxi-Min economic theory forms the basis of what we currently refer to as VBHC and has been well described by Teisberg [Citation15].