ABSTRACT
Introduction
Suboptimal medication adherence is common among patients with cardiovascular diseases. We sought evidence on non-pharmacological interventions used to support adherence for patients with hypertension and/or dyslipidemia.
Methods
We searched MEDLINE, EMBASE, MEDLINE In-Process, ClinicalTrials.gov, EUCTR, and conference proceedings from July 2011 to July 2021 to identify trials evaluating effects of health education, phone reminders, or digital interventions on medication adherence or persistence of adult patients with hypertension and/or dyslipidemia. Risk of bias was assessed using the Cochrane Risk of Bias Assessment Tool v2.
Results
Of 64 studies, 62 used health education approaches (e.g. educational interviews, motivational meetings, advice from physicians, and mobile health content), 16 phone reminders (e.g. text reminders, electronic pill-box linked reminders, bi-directional text messaging), and 10 digital applications as interventions (e.g., various self-management applications). All studies assessed medication adherence; only two persistence. Overall, 30 studies (83%) assessing health education approaches alone and 25 (78%) combined with other strategies, 12 (75%) phone reminders and eight studies (80%) digital applications combined with other strategies reported improved medication adherence. Two studies assessing health education approaches reported improved persistence.
Conclusions
Our findings indicate non-pharmacological interventions may positively impact adherence. Therefore, ‘beyond the pill’ approaches could play a role in preventing cardiovascular diseases.
1. Introduction
Sustained adherence to prescribed therapy is the primary determinant of treatment success [Citation1–3]. This medication-taking behavior encompasses both ‘medication adherence,’ defined by the World Health Organization (WHO) as ‘the extent to which patient behavior corresponds with agreed recommendations from their healthcare provider’ [Citation4], and ‘medication persistence,’ the accumulated time from initiation to discontinuation of therapy [Citation3]. Non-adherence may worsen therapeutic and economic outcomes due to an increased risk of cardiovascular events, increased frequency of healthcare provider consultations, higher rates of hospitalization, and increased healthcare costs [Citation1,Citation4–6]. Non-adherence among patients with chronic conditions, including cardiovascular conditions, is estimated at 40–50% [Citation4,Citation7].
The underlying determinants of adherence are complex [Citation8]. Adherence to long-term treatment for chronic conditions may be influenced by socioeconomic and healthcare system-related factors (e.g. quality of provider-patient communication, healthcare access), factors related to the condition being treated (e.g., disease severity), therapy-related factors (e.g., cost, mode of administration, number of medications being taken, dosing frequency, side effects), and patient-related factors (e.g., patients’ own beliefs, constraints of everyday life, swallowing problems) [Citation8–11]. Furthermore, adherence behavior can be affected by deliberate and non-deliberate actions, such as inability to take medications due to misunderstanding instructions [Citation4,Citation12].
Numerous interventions have been used to improve patient adherence to therapy in chronic disease [Citation13,Citation14]. A range of strategies have been investigated in cardiovascular disease prevention and control, including education brochures, reminder tools, telephone follow-up, individualized telephone feedback, patient web portals, and smartphone/wearable device applications, among others [Citation15–20]. The approaches can be implemented as simple, ‘single-component’ interventions, or as a combination of strategies (i.e., ‘multi-component’ interventions). Strategies employed within a multi-component intervention may include components of the same broad type (e.g., different forms of health education) or components of more than one type (e.g., health education plus reminders to take medication).
There is a growing body of literature on non-pharmacological interventions to improve medication adherence [Citation21]. However, to date, reviews on digital applications, phone reminders, and educational programs that included patients with hypertension/dyslipidemia have not specifically focused on these patient populations, were focused only on interventions delivered by pharmacists, or are outdated [Citation5,Citation6,Citation22–25].
In this review, we therefore aimed to identify and synthesize evidence on health education, digital applications, and phone reminder interventions to improve medication adherence and/or persistence in adult patients with hypertension and/or dyslipidemia.
2. Methods
This systematic review was reported according to the standards of the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) 2020 Statement [Citation26]. This study was not registered in a public systematic review registry. The full review protocol is available upon request.
2.1. Search strategy and eligibility criteria
A systematic search was performed in MEDLINE, EMBASE (via Embase.com; Elsevier), MEDLINE, and MEDLINE In-Process (via PubMed; National Institute of Health National Library of Medicine) from database inception to 6 July 2021 (Table S1). In addition, we searched trial registries (ClinicalTrials.gov, EU Clinical Trials Register), and Google Scholar in September 2021 for relevant studies. We also searched conference proceedings for eligible studies published in the last three years (Table S2). Bibliographies of included publications were scrutinized for additional relevant studies.
We initially formulated broad eligibility criteria to identify evidence published in English on the impact of non-pharmacological interventions on adherence and persistence in adult patients with dyslipidemia, hypertension and/or angina. The review was then focused on studies with a randomized controlled trial (RCT) design because this represents the highest quality of study design. RCTs that enrolled < 50 patients, or published prior to July 2011 were excluded (Table S3).
2.2. Study selection
Selection of eligible publications was conducted in two stages: 1) screening of titles and abstracts, and 2) screening of full texts of publications deemed potentially relevant in the first step. Both stages were conducted by two reviewers in parallel. Discrepancies were resolved by discussion with a third reviewer.
2.3. Data extraction
A single reviewer extracted data from included publications into a standardized Excel® form. Data on study design, patient demographics, setting, interventions and comparators, medication adherence, and persistence were extracted. As interventions to increase medication adherence and persistence can be complex [Citation27], we categorized the types of interventions and their components as shown in Table S4.
2.4. Risk of bias assessment
One reviewer assessed the risk of bias using version 2 of the Cochrane Risk of Bias Assessment Tool (RoB 2) [Citation28]. Another reviewer independently validated the risk of bias assessments (low risk, some concern, high risk) for 25% of the studies.
2.5. Data synthesis
We summarized data in tabular form, and further synthesized the data according to intervention categories and outcomes to develop an effect direction plot [Citation29]. Meta-analysis was not considered appropriate due to the variation in study designs and in the context, types, and delivery of interventions.
3. Results
The electronic database search yielded 4,654 records, from which 848 duplicates were removed. After screening titles and abstracts, 368 reports were retrieved for full-text review. According to the final selection criteria, 57 publications were included. An additional seven reports were included from the other searches. Therefore, 64 publications, each reporting on a different study, were included in this review ().
Figure 1. PRISMA flow diagram showing the literature screening process. Abbreviation: RCT: randomized controlled trial. *Studies published before July 2011 (n = 50); studies with number of patients < 50 (n = 20) of which seven were published before 2011. †Sixteen registered studies had no results published.
The study characteristics are listed in Supplementary Table S5. Fifty-two studies were RCTs and 12 were cluster RCTs. Studies were conducted in the Asia-Pacific region (n = 24), North America (n = 21), Europe (n = 11), South America (n = 6), and Africa (n = 2). Most studies were conducted in the United States (n = 21), China (n = 8), or Spain (n = 6).
Sixty studies assessed patients with hypertension and four assessed patients with dyslipidemia. No relevant studies on patients with angina were identified. The study sample size ranged from 52 participants [Citation30] to 25,388 participants [Citation31]. The length of follow-up ranged from one month [Citation32–34] to 60 months [Citation35].
All 64 studies evaluated medication adherence. The most frequently used methods to assess medication adherence were: the Morisky Medication Adherence Scale (MMAS; n = 30 studies), followed by the High Blood Pressure Compliance Scale (HBCS)/Hill-Bone Medication Adherence Scale (HBMAS; n = 5), the proportion of days covered (PDC; n = 4), Medication Adherence Rating Scale (MARS; n = 3), Medication Adherence Self-Efficacy Scale (MASES; n = 2), Medication Possession Ratio (MPR; n = 2) and the Brief Medication Questionnaire (BMQ; n = 2) (Table S6). Sixteen studies did not specify the method used to assess adherence. Two studies assessed persistence [Citation36,Citation37], defined as mean treatment duration [Citation37] or treatment discontinuation [Citation36].
Health education was assessed either as a single intervention type, or with other types of intervention components, whereas phone reminders or digital applications were always included with other types of intervention approaches. Health education was the most frequently evaluated intervention (n = 62). The health education components included educational interviews, sessions with trained healthcare workers or researchers, group activities, educational mobile health content, phone-based sessions, online training, and printed materials. Twenty-nine studies assessed the impact of health education alone, in either single (n = 11) or multicomponent (n = 18) interventions. Thirty-three studies assessed interventions that included health education in addition to components from other category(ies), which included phone reminders, digital applications, blood pressure (BP) monitor, electronic medical record (EMR) platform, and other interventions.
Altogether, 16 studies assessed the impact of phone reminders as part of multiple intervention categories, which included health education, digital application, BP monitor, and electronic pill bottles. The components of phone reminders included text reminders for medication intake, prescription refills, and bi-directional text messaging requiring a confirmation from the patient.
Ten studies assessed the impact of digital applications as part of approaches that employed more than one of the intervention categories, which included health education, phone reminders, or BP monitor use. The components of digital applications included a range of self-management applications with varying functionalities.
Thirty studies [Citation34,Citation36,Citation38–65] explicitly mentioned an underlying theory or model, most often motivational interviewing (n = 7) [Citation36,Citation38,Citation47,Citation49,Citation52,Citation57,Citation61], the trans-theoretical model of behavioral change (n = 5) [Citation36,Citation44,Citation51,Citation52,Citation61], social cognitive theory (n = 4) [Citation41,Citation51,Citation52,Citation63], health belief model (n = 3) [Citation34,Citation49,Citation55], self-management theory (n = 3) [Citation45,Citation47,Citation65], or the chronic care model (n = 3) [Citation50,Citation53,Citation64].
Of the 64 included studies, 11 were classified as having a low risk of bias, 33 with some concerns of risk of bias, and 20 at high risk of bias ().
Figure 2. Effect direction plot summarizing medication adherence and persistence in all studies. Abbreviations: BP: blood pressure; DAPP: digital application; EMR: electronic medical record; HE: health education; PR: phone reminders; RCT: randomized controlled trial; CRCT: cluster randomized controlled trial. Effect direction: upward arrow ▲= positive health impact, downward arrow ▼= negative health impact, sideways arrow ◄►= no change/mixed effects/conflicting findings. Sample size: final sample size (individuals) in intervention group; large arrow▲ >300; medium arrow▲100–300; small arrow ▲ <100. Study quality: denoted by row color:green = low risk of bias; amber = some concerns; red = high risk of bias.
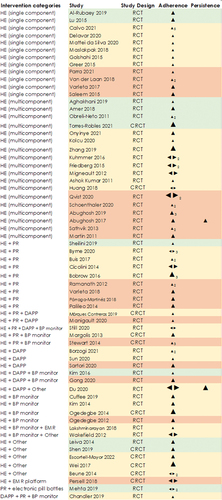
Medication adherence and persistence reported by all included studies are summarized in the effect direction plot in . Of the 62 studies assessing the impact of health education, 52 (84%) reported improved medication adherence. All 11 studies (100%) that assessed health education as a single-component interventions showed improved medication adherence. Of the 18 studies evaluating the impact of more than one health education component within an intervention, 13 (72%) reported improved medication adherence. Of the 32 studies assessing the impact of health education as part of an intervention with other intervention categories, 25 (78%) reported improved medication adherence. Among most of the studies measuring adherencing with self-reported questionnaires, the improvements were singificnat for studies assessing health education. Out of all studies four reported adherence after less than 3 months of follow-up. Across three studies health education was given as a single component intervention and results showed significantly improved adherence. One study investigating health education as a multiple component intervention non-significant improvement were reported in the study.
Of the 16 studies assessing phone reminders as part of the intervention, 12 (75%) reported improvement in medication adherence, regardless of the methods used to measure adherence. Among the 10 studies assessing digital applications as part of the intervention, eight (80%) reported improved medication adherence and the majority measured adherence using MMAS.
Only two studies [Citation36,Citation37] reported on medication persistence. One study [Citation36] conducted among US patients enrolled in the Medicare Advantage Plan reported that patients who received a motivational interviewing-based telephone intervention were less likely to discontinue statin therapy in 6 months follow-up compared to controls who did not receive the interventions (adjusted odds ratio [OR]: 0.38; 95% CI: 0.19–0.76). Another study [Citation37] was a phase IV trial that investigated a smartphone-based patient support tool to promote adherence in patients who were newly prescribed rosuvastatin. This tool allows patients to receive feedback on their treatment and disease support, as well as information on treatment and lifestyle choices. This study reported that patients using the support tool had a longer treatment duration than those using a smartphone-based control application that was limited to data collection only with no patient support (mean 157 days vs 146 days; p = 0.0019).
4. Discussion
This systematic review describes a decade of published research on non-pharmaceutical interventions and suggests that health education, digital applications, and phone reminders can have a positive impact on the medication adherence and persistence in patients with hypertension or dyslipidemia, regardless of the delivery approach (as a single intervention category or part of multiple intervention categories). Some authors have suggested that combining multiple types of approach may be more successful than a single intervention category (e.g., health education) or in some cases necessary because of the complexity of adherence behavior [Citation66–68]. However, several studies identified in this review reported that interventions based on only one intervention category led to significant improvement in medication adherence compared to usual care [Citation31,Citation36,Citation38,Citation43,Citation45,Citation61,Citation64,Citation69–73].
Health education was the most widely used intervention and was frequently found to result in significant improvement compared to usual care. The identified evidence broadly supports the value of educational interventions on medication-taking behavior. Eighty-seven percent of all included studies showed improvement in adherence of the intervention groups over the comparator groups and more than 92% included health education as part of the intervention. Two previous reviews [Citation74,Citation75] focused broadly on healthcare professional-led or verbal education approaches reported similar findings in patients with hypertension, dyslipidemia, or diabetes mellitus. Authors of both reviews suggested that educational sessions improved health literacy, which is important for optimal disease management including adherence.
Among the 16 studies that assessed phone reminders, 80% (n = 12) reported improved medication adherence. Three studies [Citation57,Citation58,Citation76] reported no significant improvement and one [Citation77] reported a conflicting result. Similar findings were reported in the review by Vervloet et al. [Citation24], that included 13 controlled clinical trials evaluating the effectiveness of interventions using electronic reminders in improving medication adherence in patients with chronic conditions. This review provided evidence for short-term effectiveness (follow-up period <6 months) of electronic reminders, especially Short Message Service (SMS) reminders, but concluded that long-term effects (follow-up period ≥6 months) of phone reminders were unclear. In a meta-analysis by Tao et al. [Citation25] that included most of the studies from Vervloet et al. [Citation24], electronic reminders were associated with a significant improvement in medication adherence. Another recent review [Citation78] reported that SMS reminders were most effective for BP management when they involve two-way communication, content tailored to the individual patient, and a combination of other support practices.
All the studies that assessed digital application interventions reported a trend toward improved medication adherence. The extent of improvement in adherence may depend on numerous factors, including specific characteristics of the application and its delivery [Citation79]. Other factors, such as the involvement of healthcare providers in the intervention administration and the characteristics of the target population, might also influence the success of any particular intervention. Findings of this review are in accordance with a previous review [Citation80] that included studies with varying study designs and outcomes and provided evidence of the benefits of mobile health interventions (based on sending text messages or using a smartphone application). This review states that 65% of the studies reported improved adherence and concluded that sending medication reminders and health education messages together was more beneficial than sending only medication reminders. A recent systematic review and meta-analysis [Citation81] published in 2021 reported similar findings that included 16 RCTs assessing patients with cardiovascular diseases. This review found that nine of the included RCTs reported statistically significant improvements in medication adherence.
Difficulty in reliably measuring adherence has been highlighted in previous publications [Citation8,Citation82]. There is currently no recognized ‘gold standard’ approach for assessing medication adherence. One suggested means to address this is using at least two different methods to evaluate adherence within the same study [Citation83]. However, we found that 45 of 64 studies only used one method. Challenges in measuring adherence were also highlighted by studies in which several methods were used, as our review identified four studies [Citation39,Citation57,Citation77,Citation84] reporting conflicting findings when using more than one tool to measure adherence. Altogether, the identified evidence emphasizes the lack of consensus regarding the most appropriate means to measure adherence.
In this review, only one study [Citation62] out of 34 studies published since 2018 reported medication adherence in accordance with the International Society for Medication Adherence (previously named ESPACOMP) Medication Adherence Reporting Guideline (EMERGE) checklist [Citation85], which became available in 2018 [Citation85]. We also noted other studies published since 2018 reported at least some details on the implementation process of the intervention under investigation [Citation32,Citation33,Citation35,Citation37,Citation38,Citation40–43,Citation47,Citation56,Citation58,Citation59,Citation61,Citation62,Citation64,Citation70–73,Citation86–92] or the relevance to their application into general practice [Citation32,Citation38,Citation43,Citation62,Citation64,Citation69–73,Citation88–91,Citation93–96]. Nevertheless, insufficient details were reported by many studies on the technical implementation processes and message delivery, which are required to have a precise understanding of an intervention and its implementation [Citation97].
Not all studies stated whether the interventions were based on a particular theory, model, or framework. When reported, most of the theories and models targeted individuals rather than systems, families, or communities. Most also focused on cognitive factors such as perceptions, beliefs, knowledge, attitudes, or expectations. Although many articles noted that interventions were developed based on theories, generally insufficient details were provided to ascertain their implementation of the theories. However, our findings are broadly aligned with Conn et al. [Citation98] who found that theory- and model-linked interventions can have a modest but significant effect on medication adherence.
Despite the promising future of mobile Health (mHealth) in emerging economies, where smartphones are increasingly widely used [Citation99], most of the evidence on the use of digital applications or phone text message reminders was from high-income countries. Five studies from developing countries [Citation100] included a digital application as part of an intervention [Citation37,Citation40,Citation59,Citation86,Citation101]. The limited evidence from these few studies supports the benefits of a range of mHealth approaches in improving medication adherence in developing countries.
This review has several strengths and limitations. We performed a structured, systematic search, focusing on randomized controlled trials, which are considered sources of high-quality evidence according to the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) guidelines [Citation102]. Limitations include restricting to English-language publications and limiting to studies published from July 2011 onwards. Furthermore, heterogeneity in definitions of adherence and methods to measure medication adherence limited comparability across identified studies, as did the wide range of intervention types and contexts in which studies were conducted [Citation103–108].
Our review provides a global picture of the evidence generated in the last 10 years on the use and impact of non-pharmacologic interventions on medication adherence and persistence. A ‘beyond the pill’ approach, employing non-pharmacological interventions to support medication adherence can play a crucial role along with pharmacological therapies to treat chronic diseases. Future research is warranted on non-pharmacological interventions, in particular in the form of studies with high-quality design, large sample sizes, and standardized conduct in terms of definitions and reporting.
Non-standard abbreviations and Acronyms
| BMQ | = | Brief Medication Questionnaire |
| BP | = | Blood pressure |
| EMR | = | Electronic medical record |
| GRADE | = | Grading of Recommendations, Assessment, Development and Evaluations |
| HBCS | = | High Blood Pressure Compliance Scale |
| HBMAS | = | Hill-Bone Medication Adherence Scale |
| MARS | = | Medication Adherence Rating Scale |
| mHealth | = | Mobile health |
| MMAS | = | Morisky Medication Adherence Scale |
| MPR | = | Medication Possession Ratio |
| PDC | = | Proportion of days covered |
| PRISMA | = | Preferred Reporting Items for Systematic Review and Meta-Analysis |
| RCT | = | Randomized controlled trial |
| RoB2 | = | Risk of Bias 2 tool |
| SMS | = | Short Message Service |
| WHO | = | World Health Organization |
Declaration of interest
JB Brière is an employee of Servier. IA Gudiña, X. Jiang, P. Kodjamanova, and L. Bennetts are employees of Amaris Consulting, which received funding from Servier for the study. ZM Khan is a paid consultant for Servier. AP Kengne received an honorarium for support in contributing to the study protocol and interpretation of results. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Author contributions
Manuscript concept and design: JB Brière, A. Kengne, I. Asensio Gudiña, P. Kodjamanova, and L. Bennetts; Drafting of manuscript: S. Ridhurkar; Critical reviews: A. Kengne, JB Brière, ZM Khan, and L. Bennetts; all authors approved and agree for the final version of the manuscript to be published.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Supplemental Material
Download PDF (68.9 KB)Supplemental Material
Download MS Word (236.4 KB)Acknowledgments
The authors thank Sudipta Ridhurkar, PhD, from Amaris Consulting, Barcelona, Spain for providing medical writing assistance. This assistance was funded by Servier.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/14737167.2024.2319598.
Additional information
Funding
References
- Jimmy B, Jose J. Patient medication adherence: measures in daily practice. Oman Med J. 2011;26(3):155. doi: 10.5001/omj.2011.38
- Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497. doi: 10.1056/NEJMra050100
- Burnier M. Medication adherence and persistence as the cornerstone of effective antihypertensive therapy. Am J Hypertens. 2006;19(11):1190–1196. doi: 10.1016/j.amjhyper.2006.04.006
- World Health Organization. Adherence to long-term therapies: evidence for action [Internet]. Sabaté E, editor. World Health Organization; 2003. Available from: https://apps.who.int/iris/handle/10665/42682
- Demonceau J, Ruppar T, Kristanto P, et al. Identification and assessment of adherence-enhancing interventions in studies assessing medication adherence through electronically compiled drug dosing histories: a systematic literature review and meta-analysis. Drugs. 2013;73(6):545–562. doi: 10.1007/s40265-013-0041-3
- Armitage LC, Kassavou A, Sutton S. Do mobile device apps designed to support medication adherence demonstrate efficacy? A systematic review of randomised controlled trials, with meta-analysis. BMJ Open [Internet]. 2020;10(1):e032045. Available from: https://bmjopen.bmj.com/content/10/1/e032045.abstract
- Kleinsinger F. The unmet challenge of medication nonadherence. Perm J. 2018;22(3):18–33. doi: 10.7812/TPP/18-033
- Kardas P, Lewek P, Matyjaszczyk M. Determinants of patient adherence: a review of systematic reviews. Front Pharmacol [Internet]. 2013;4. Available from: https://www.frontiersin.org/articles/10.3389/fphar.2013.00091
- DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med care. 2004 Apr 13;42(3):200–209.
- Vermeire E, Hearnshaw H, Van Royen P, et al. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Therapeutics. 2001;26(5):331–342. doi: 10.1046/j.1365-2710.2001.00363.x
- Baroletti S, Dell’orfano H. Medication adherence in cardiovascular disease. Circulation. 2010;121(12):1455–1458. doi: 10.1161/CIRCULATIONAHA.109.904003
- Maxwell CJ, Stock K, Seitz D, et al. Persistence and adherence with dementia pharmacotherapy: relevance of patient, provider, and system factors. Can J Psychiatry. 2014;59(12):624–631. doi: 10.1177/070674371405901203
- Dean AJ, Walters J, Hall A. A systematic review of interventions to enhance medication adherence in children and adolescents with chronic illness. Arch Dischildhood. 2010;95(9):717–723. doi: 10.1136/adc.2009.175125
- Milosavljevic A, Aspden T, Harrison J. Community pharmacist-led interventions and their impact on patients’ medication adherence and other health outcomes: a systematic review. Int J Pharm Pract. 2018;26(5):387–397. doi: 10.1111/ijpp.12462
- Shore S, Ho PM, Lambert-Kerzner A, et al. Site-level variation in and practices associated with dabigatran adherence. JAMA. 2015 Apr 15;313:1443–1450.
- Desteghe L, Vijgen J, Koopman P, et al. Telemonitoring-based feedback improves adherence to non-vitamin K antagonist oral anticoagulants intake in patients with atrial fibrillation. Eur Heart J. 2018 Jan 05;39(16):1394–1403. doi: 10.1093/eurheartj/ehx762
- Márquez-Contreras E, Martell-Claros N, Márquez-Rivero S, et al. Strategies for improving dabigatran adherence for stroke prevention in patients with non-valvular atrial fibrillation: education and drug intake reminders (FACILITA study). Curr Med Res Opin. 2018 Feb 01;34(7):1301–1308. doi: 10.1080/03007995.2018.1435519
- Senoo K, Miki T, Ohkura T, et al. A smartphone app to improve oral anticoagulation adherence in patients with atrial fibrillation: prospective observational study. JMIR Mhealth Uhealth. 2022;10(1):e30807. doi: 10.2196/30807
- Conn VS, Ruppar TM, Chase J-A, et al. Interventions to improve medication adherence in hypertensive patients: systematic review and meta-analysis. Curr Hypertens Rep. 2015;17(12):1–15. doi: 10.1007/s11906-015-0606-5
- Ferdinand KC, Senatore FF, Clayton-Jeter H, et al. Improving medication adherence in cardiometabolic disease: practical and regulatory implications. J Am Coll Cardiol. 2017;69(4):437–451. doi: 10.1016/j.jacc.2016.11.034
- Kini V, Ho PM. Interventions to improve medication adherence: a review. JAMA. 2018;320(23):2461–2473. doi: 10.1001/jama.2018.19271
- Anderson LJ, Nuckols TK, Coles C, et al. A systematic overview of systematic reviews evaluating medication adherence interventions. Am J Health Syst Pharm. 2020;77(2):138–147. doi: 10.1093/ajhp/zxz284
- Peng Y, Wang H, Fang Q, et al. Effectiveness of mobile applications on medication adherence in adults with chronic diseases: a systematic review and meta-analysis. J Managed Care Specialty Pharm. 2020;26(4):550–561. doi: 10.18553/jmcp.2020.26.4.550
- Vervloet M, Linn AJ, van Weert JC, et al. The effectiveness of interventions using electronic reminders to improve adherence to chronic medication: a systematic review of the literature. J Am Med Inform Assoc. 2012;19(5):696–704. doi: 10.1136/amiajnl-2011-000748
- Tao D, Xie L, Wang T, et al. A meta-analysis of the use of electronic reminders for patient adherence to medication in chronic disease care. J Telemed Telecare. 2015;21(1):3–13. doi: 10.1177/1357633X14541041
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):1–11. doi: 10.1186/s13643-021-01626-4
- Guise J-M, Chang C, Viswanathan M, et al. Systematic reviews of complex multicomponent health care interventions [internet]. Rockville (MD) USA: Scientific Resource Center, Portland (OR) USA; 2014. (Report No.: 14-EHC003-EF). Available from: https://www.ncbi.nlm.nih.gov/books/NBK194846/.
- Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898
- Boon MH, Thomson H. The effect direction plot revisited: application of the 2019 cochrane handbook guidance on alternative synthesis methods. Res Synth Methods. 2021;12(1):29–33. doi: 10.1002/jrsm.1458
- Ramanath K, Balaji D, Nagakishore C, et al. A study on impact of clinical pharmacist interventions on medication adherence and quality of life in rural hypertensive patients. J Young Pharm. 2012 Jul 04;4(2):95–100. doi: 10.4103/0975-1483.96623
- Wei X, Walley JD, Zhang Z, et al. Implementation of a comprehensive intervention for patients at high risk of cardiovascular disease in rural China: a pragmatic cluster randomized controlled trial. PloS One. 2017;12(8):e0183169. Available from: https://embase.com/search/results?subaction=viewrecord&id=L617792312&from=export
- Aghakhani N, Parizad N, Soltani B, et al. The effect of the blended education program on treatment concordance of patients with hypertension: a single-blind randomized, controlled trial. J Vasc Nurs. 2019 Dec 19;37(4):250–256. doi: 10.1016/j.jvn.2019.08.001
- Al-Rubaey MG, Shwaish MI. Impact of hypertension education on treatment compliance among hypertensive patients in Baghdad 2017. J Pak Med Assoc. 2019;69:S9–S12.
- Buis L, Hirzel L, Dawood RM, et al. Text messaging to improve hypertension medication adherence in African americans from primary care and emergency department settings: results from two randomized feasibility studies. JMIR mHealth uHealth. 2017 Feb 06;5:e9.
- Qvist I, Lindholt JS, Søgaard R, et al. Randomised trial of telephone counselling to improve participants’ adherence to prescribed drugs in a vascular screening trial. Basic Clin Pharmacol Toxicol. 2020;127(6):477–487. doi: 10.1111/bcpt.13459
- Abughosh S, Wang X, Serna O, et al. A motivational interviewing intervention by pharmacy students to improve medication adherence. J Manag Care Spec Pharm. 2017 Apr 28;23(5):549–560. doi: 10.18553/jmcp.2017.23.5.549
- Du X, Jörntén-Karlsson M, Karlson BW, et al. eHelp China: a randomized trial evaluating the benefits of a smartphone-based patient support tool. Int J Clin Res Trials [Internet]. 2020;6. Available from: https://www.graphyonline.com/archives/archivedownload.php?pid=IJCRT-158
- Abughosh SM, Vadhariya A, Johnson ML, et al. Enhancing statin adherence using a motivational interviewing intervention and past adherence trajectories in patients with suboptimal adherence. J Manag Care Spec Pharm. 2019 Sep 27;25(10):1053–1062. doi: 10.18553/jmcp.2019.25.10.1053
- Beune EJ, Moll van Charante EP, Beem L, et al. Culturally adapted hypertension education (CAHE) to improve blood pressure control and treatment adherence in patients of African origin with uncontrolled hypertension: cluster-randomized trial. PloS One. 2014 Mar 07;9(3):e90103. doi: 10.1371/journal.pone.0090103
- Bozorgi A, Hosseini H, Eftekhar H, et al. The effect of the mobile “blood pressure management application” on hypertension self-management enhancement: a randomized controlled trial. Trials [Internet]. 2021;22. Available from: https://embase.com/search/results?subaction=viewrecord&id=L2012909041&from=export
- Byrne JL, Dallosso HM, Rogers S, et al. Effectiveness of the Ready to Reduce Risk (3R) complex intervention for the primary prevention of cardiovascular disease: A pragmatic randomised controlled trial. BMC Med [Internet]. 2020;18. Available from: https://embase.com/search/results?subaction=viewrecord&id=L632442171&from=export
- Chandler J, Sox L, Kellam K, et al. Impact of a culturally tailored mhealth medication regimen self-management program upon blood pressure among hypertensive Hispanic adults. IJERPH. 2019;16(7):1226. Available from: https://embase.com/search/results?subaction=viewrecord&id=L2001904288&from=export
- Delavar F, Pashaeypoor S, Negarandeh R. The effects of self-management education tailored to health literacy on medication adherence and blood pressure control among elderly people with primary hypertension: a randomized controlled trial. Patient Educ Couns. 2020;103(2):336–342. doi: 10.1016/j.pec.2019.08.028
- Friedberg JP, Rodriguez MA, Watsula ME, et al. Effectiveness of a tailored behavioral intervention to improve hypertension control: primary outcomes of a randomized controlled trial. Hypertension. 2015;65(2):440–446. doi: 10.1161/HYPERTENSIONAHA.114.03483
- Golshahi J, Ahmadzadeh H, Sadeghi M, et al. Effect of self-care education on lifestyle modification, medication adherence and blood pressure in hypertensive adults: randomized controlled clinical trial. Adv Biomed Res. 2015 Nov 26;4:204.
- Greer DB, Ostwald SK. Improving adherence in African American women with uncontrolled hypertension. J Cardiovasc Nurs. 2015;30(4):311–318. doi: 10.1097/JCN.0000000000000152
- Huang B, Li Z, Wang Y, et al. Effectiveness of self-management support in maintenance haemodialysis patients with hypertension: a pilot cluster randomized controlled trial. Nephrology. 2018;23(8):755–763. doi: 10.1111/nep.13098
- Kim KB, Han HR, Huh B, et al. The effect of a community-based self-help multimodal behavioral intervention in Korean American seniors with high blood pressure. Am J Hypertens. 2014;27(9):1199–1208. doi: 10.1093/ajh/hpu041
- Leiva A, Aguiló A, Fajó-Pascual M, et al. Efficacy of a brief multifactorial adherence-based intervention in reducing blood pressure: a randomized clinical trial. Patient Preference Adherence. 2014;8:1683–1690. doi: 10.2147/PPA.S66927
- Margolis KL, Asche SE, Bergdall AR, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA. 2013;310(1):46–56. doi: 10.1001/jama.2013.6549
- Martin MY, Kim YI, Kratt P, et al. Medication adherence among rural, low-income hypertensive adults: a randomized trial of a multimedia community-based intervention. Am J Health Promot. 2011 Jul 05;25:372–378.
- Migneault JP, Dedier JJ, Wright JA, et al. A culturally adapted telecommunication system to improve physical activity, diet quality, and medication adherence among hypertensive African–Americans: a randomized controlled trial. Ann Behav Med. 2012;43(1):62–73. doi: 10.1007/s12160-011-9319-4
- Ogedegbe G, Tobin JN, Fernandez S, et al. Counseling African Americans to control hypertension: cluster-randomized clinical trial main effects. Circulation. 2014;129(20):2044–2051. doi: 10.1161/CIRCULATIONAHA.113.006650
- Ogedegbe GO, Boutin-Foster C, Wells MT, et al. A randomized controlled trial of positive-affect intervention and medication adherence in hypertensive African Americans. Arch Internal Med. 2012;172(4):322–326. doi: 10.1001/archinternmed.2011.1307
- Sathvik BS, Karibasappa MV, Nagavi BG. Self-reported medication adherence pattern of rural Indian patients with hypertension. Asian J Pharm Clin Res. 2013;6:49–52.
- Schoenthaler A, de la Calle F, Pitaro M, et al. A systems-level approach to improving medication adherence in hypertensive latinos: a randomized control trial. J Gen Intern Med. 2020;35(1):182–189. doi: 10.1007/s11606-019-05419-3
- Stewart K, George J, Mc Namara KP, et al. A multifaceted pharmacist intervention to improve antihypertensive adherence: a cluster-randomized, controlled trial (HAPPy trial). J Clin Pharm Therapeutics. 2014;39(5):527–534. doi: 10.1111/jcpt.12185
- Still CH, Margevicius S, Harwell C, et al. A community and technology-based approach for hypertension self-management (COACHMAN) to improve blood pressure control in African Americans: results from a pilot study. Patient Prefer Adherence. 2020 Dec 03;14:2301–2313.
- Sun YQ, Jia YP, Lv JY, et al. The clinical effects of a new management mode for hypertensive patients: a randomized controlled trial. Cardiovasc Diagn Ther. 2020;10(6):1805–1815. doi: 10.21037/cdt-20-589
- Svarstad BL, Kotchen JM, Shireman TI, et al. Improving refill adherence and hypertension control in black patients: wisconsin TEAM trial. J Am Pharm Assoc. 2013;53(5):520–529. doi: 10.1331/JAPhA.2013.12246
- Torres-Robles A, Benrimoj SI, Gastelurrutia MA, et al. Effectiveness of a medication adherence management intervention in a community pharmacy setting: a cluster randomised controlled trial. BMJ Qual Saf. 2021;31(2):105–115. doi: 10.1136/bmjqs-2020-011671
- van der Laan DM, Elders PJM, Boons C, et al. Effectiveness of a patient-tailored, pharmacist-led intervention program to enhance adherence to antihypertensive medication: the CATI study. Front Pharmacol. 2018 Oct 16;9:1057.
- Varleta P, Acevedo M, Akel C, et al. Mobile phone text messaging improves antihypertensive drug adherence in the community. J Clin Hypertens. 2017;19(12):1276–1284. doi: 10.1111/jch.13098
- Zhang Y, Liu S, Sheng X, et al. Evaluation of a community-based hypertension self-management model with general practitioners. Int J Health Plann Manage. 2019;34(3):960–974. doi: 10.1002/hpm.2867
- Kim JY, Wineinger NE, Steinhubl SR. The influence of wireless self-monitoring program on the relationship between patient activation and health behaviors, medication adherence, and blood pressure levels in hypertensive patients: a substudy of a randomized controlled trial. J Med Internet Res. 2016;18(6):e116. doi: 10.2196/jmir.5429
- Foster BJ. Multicomponent interventions improve adherence —where do we go from here? Am J Transplant. 2020;20(1):5–6. doi: 10.1111/ajt.15632
- Gohil S, Majd Z, Sheneman JC, et al. Interventions to improve medication adherence in inflammatory bowel disease: a systematic review. Patient Educ Couns. 2021;105(7):1731–1742. doi: 10.1016/j.pec.2021.10.017
- Wiecek E, Tonin FS, Torres-Robles A, et al. Temporal effectiveness of interventions to improve medication adherence: a network meta-analysis. PloS One. 2019;14(3):e0213432. doi: 10.1371/journal.pone.0213432
- Kolcu M, Ergun A. Effect of a nurse-led hypertension management program on quality of life, medication adherence and hypertension management in older adults: a randomized controlled trial. Geriatrics Gerontology Int. 2020;20(12):1182–1189. doi: 10.1111/ggi.14068
- Amer M, Rahman N, Nazir SR, et al. Impact of pharmacist’s intervention on disease related knowledge, medication adherence, HRQoL and control of blood pressure among hypertensive patients. Pak J Pharm Sci. 2018 Dec 28;31:2607–2616.
- Maslakpak MH, Rezaei B, Parizad N, et al. Does family involvement in patient education improve hypertension management? A single-blind randomized, parallel group, controlled trial. Cogent Med. 2018;5(1):1–13. doi: 10.1080/2331205X.2018.1537063
- da Silva Ât M, de Fátima Mantovani M, Castanho Moreira R, et al. Nursing case management for people with hypertension in primary health care: a randomized controlled trial. Res Nurs Health. 2019 Nov 12;43(1):68–78. doi: 10.1002/nur.21994
- Shen Y, Wang T, Gao M, et al. Effectiveness of low-cost reminder package combined with case-based health education to improve hypertensive patients’ medication adherence: a clustered randomized controlled trial. Pat Pref Adh. 2019;13:1083–1092. doi: 10.2147/PPA.S194667
- Tan JP, Cheng KKF, Siah RC. A systematic review and meta‐analysis on the effectiveness of education on medication adherence for patients with hypertension, hyperlipidaemia and diabetes. J Adv Nurs. 2019;75(11):2478–2494. doi: 10.1111/jan.14025
- Ampofo AG, Khan E, Ibitoye MB. Understanding the role of educational interventions on medication adherence in hypertension: a systematic review and meta-analysis. Heart & Lung. 2020;49(5):537–547. doi: 10.1016/j.hrtlng.2020.02.039
- Cicolini G, Simonetti V, Comparcini D, et al. Efficacy of a nurse-led email reminder program for cardiovascular prevention risk reduction in hypertensive patients: a randomized controlled trial. Int J Nurs Stud. 2014;51(6):833–843. doi: 10.1016/j.ijnurstu.2013.10.010
- Bobrow K, Farmer AJ, Springer D, et al. Mobile phone text messages to support treatment adherence in adults with high blood pressure (SMS-Text adherence support [StAR]): a single-blind, randomized trial. Circulation. 2016 Jan 16;133:592–600.
- Vargas G, Cajita MI, Whitehouse E, et al. Use of short messaging service for hypertension management: a systematic review. J Cardiovasc Nurs. 2016/04/26 ed. 2017;32:260–270. doi: 10.1097/JCN.0000000000000336
- Mummah SA, Robinson TN, King AC, et al. IDEAS (integrate, design, assess, and share): a framework and toolkit of strategies for the development of more effective digital interventions to change health behavior. J Med Internet Res. 2016 Dec 16;18(12):e5927. doi: 10.2196/jmir.5927
- Anglada-Martinez H, Riu-Viladoms G, Martin-Conde M, et al. Does mHealth increase adherence to medication? Results of a systematic review. Int J Clin Pract. 2015;69(1):9–32. doi: 10.1111/ijcp.12582
- Al-Arkee S, Mason J, Lane DA, et al. Mobile apps to improve medication adherence in cardiovascular disease: systematic review and meta-analysis. J Med Internet Res. 2021;23(5):e24190. doi: 10.2196/24190
- Obreli-Neto PR, Guidoni CM, de Oliveira Baldoni A, et al. Effect of a 36-month pharmaceutical care program on pharmacotherapy adherence in elderly diabetic and hypertensive patients. Int J Clin Pharm. 2011 May 06;33:642–649.
- Anghel LA, Farcas AM, Oprean RN. An overview of the common methods used to measure treatment adherence. Med Pharm Rep. 2019;92:117. doi: 10.15386/mpr-1201
- Calvo E, Izquierdo S, Castillo R, et al. Can an individualized adherence education program delivered by nurses improve therapeutic adherence in elderly people with acute myocardial infarction?: a randomized controlled study. Int J Nurs Stud. 2021;120:103975. doi: 10.1016/j.ijnurstu.2021.103975
- De Geest S, Zullig LL, Dunbar-Jacob J, et al. ESPACOMP medication adherence reporting guideline (EMERGE). Ann internal med. 2018;169(1):30–35. doi: 10.7326/M18-0543
- Gong K, Yan YL, Li Y, et al. Mobile health applications for the management of primary hypertension: a multicenter, randomized, controlled trial. Medicine. 2020;99(16):e19715. doi: 10.1097/MD.0000000000019715
- Cuffee YL, Sciamanna C, Gerin W, et al. The effectiveness of home blood pressure on 24-hour blood pressure control: a randomized controlled trial. Am J Hypertens. 2019;32(2):186–192. doi: 10.1093/ajh/hpy160
- Persell SD, Karmali KN, Lazar D, et al. Effect of electronic health record–based medication support and nurse-led medication therapy management on hypertension and medication self-management: a randomized clinical trial. JAMA Intern Med. 2018;178(8):1069–1077. doi: 10.1001/jamainternmed.2018.2372
- Lakshminarayan K, Westberg S, Northuis C, et al. A mHealth-based care model for improving hypertension control in stroke survivors: pilot RCT. Contemp Clin Trials. 2018 May 16;70:24–34.
- Manigault KR, McKinley D, Patel S, et al. The impact of a pharmacist‐designed mobile application on blood pressure control and medication adherence in patients with hypertension. J Am Coll Clin Pharm. 2020;3(7):1286–1295. doi: 10.1002/jac5.1296
- Márquez Contreras E, Márquez Rivero S, Rodríguez García E, et al. Specific hypertension smartphone application to improve medication adherence in hypertension: a cluster-randomized trial. Curr Med Res Opin. 2019;35(1):167–173. doi: 10.1080/03007995.2018.1549026
- Párraga-Martínez I, Escobar-Rabadán F, Rabanales-Sotos J, et al. Efficacy of a combined strategy to improve low-density lipoprotein cholesterol control among patients with hypercholesterolemia: a randomized clinical trial. Revista Española de Cardiología (English Edition). 2018;71:33–41. doi: 10.1016/j.rec.2017.05.029
- Parra DI, Guevara SLR, Rojas LZ. ‘Teaching: individual’ to improve adherence in hypertension and type 2 diabetes. Br J Community Nurs. 2021;26(2):84–91. doi: 10.12968/bjcn.2021.26.2.84
- Onyinye UKB, Ogochukwu AM, Victoria UC. Effect of a pharmacist intervention on self management practices among hypertensive-diabetic patients receiving care in a nigerian tertiary hospital. Int J Pharm Pharm Sci. 2021;13:58–61. doi: 10.22159/ijpps.2021v13i5.40987
- Escortell-Mayor E, Del Cura-Gonzalez I, Ojeda-Ruiz E, et al. A primary healthcare information intervention for communicating cardiovascular risk to patients with poorly controlled hypertension: the education and coronary risk evaluation (educore) study — A pragmatic, cluster-randomized trial. PloS One. 2020;15(1):e0226398. Available from: https://embase.com/search/results?subaction=viewrecord&id=L2004703276&from=export
- Mehta SJ, Volpp KG, Troxel AB, et al. Electronic pill bottles or bidirectional text messaging to improve hypertension medication adherence (way 2 text): a randomized clinical trial. J Gen Intern Med. 2019;34(11):2397–2404. doi: 10.1007/s11606-019-05241-x
- Möhler R, Köpke S, Meyer G. Criteria for reporting the development and evaluation of complex interventions in healthcare: revised guideline (CReDECI 2). Trials. 2015;16(1):1–9. doi: 10.1186/s13063-015-0709-y
- Conn VS, Enriquez M, Ruppar TM, et al. Meta-analyses of theory use in medication adherence intervention research. Am J Hlth Behav. 2016;40(2):155–171. doi: 10.5993/AJHB.40.2.1
- Taylor K, Silver L Smartphone ownership is growing rapidly around the world, but not always equally [internet]. Washington (DC) USA: Pew Research Center; 2019. Available from: https://www.pewresearch.org/global/wp-content/uploads/sites/2/2019/02/Pew-Research-Center_Global-Technology-Use-2018_2019-02-05.pdf.
- International Monetary Fund. World economic outlook: database — WEO groups and aggregates information [internet]. World economic and financial surveys. International Monetary Fund; 2022 [cited 2022 Aug 11]. Available from: https://www.imf.org/external/pubs/ft/weo/2022/01/weodata/groups.htm.
- Sartori AC, Rodrigues Lucena TF, Lopes CT, et al. Educational intervention using WhatsApp on medication adherence in hypertension and diabetes patients: a randomized clinical trial. Telemed J E Health. 2020;26(12):1526–1532. doi: 10.1089/tmj.2019.0305
- Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clinical Epidemiol. 2011;64(4):401–406. doi: 10.1016/j.jclinepi.2010.07.015
- Kuhmmer R, Lazzaretti RK, Guterres CM, et al. Effectiveness of multidisciplinary intervention on blood pressure control in primary health care: a randomized clinical trial. BMC Health Serv Res. 2016;16(1):1–13. doi: 10.1186/s12913-016-1703-0
- Saleem F, Hassali MA, Shafie AA, et al. Pharmacist intervention in improving hypertension-related knowledge, treatment medication adherence and health-related quality of life: a non-clinical randomized controlled trial. Health Expect. 2015;18(5):1270–1281. doi: 10.1111/hex.12101
- Lu C-H, Tang ST, Lei YX, et al. Community-based interventions in hypertensive patients: a comparison of three health education strategies. BMC Public Health. 2015;15(1):33. doi: 10.1186/s12889-015-1401-6
- Wakefield BJ, Holman JE, Ray A, et al. Outcomes of a home telehealth intervention for patients with diabetes and hypertension. Telemed J E Health. 2012;18(8):575–579. doi: 10.1089/tmj.2011.0237
- Ashok Kumar M, Elayaraja J, Shailaja K, et al. Improving medication adherence and clinical outcomes of hypertensive patients through patient counseling. Res J Pharm Biol Chem Sci. 2011;2(3):231–241.
- Palileo L. Effectiveness of SMS text reminders to improve blood pressure among patients with hypertension. National Library of Medicine; 2014. Available from: https://clinicaltrials.gov/ct2/show/NCT01255436
