1. Introduction
The misdiagnosis of epilepsy is and has always been common in both adults and children [Citation1,Citation2]. Approximately 30% of patients with drug-resistant seizures seen at epilepsy centers do not have epilepsy and have been misdiagnosed [Citation3]. Often, the erroneous diagnosis is based on normal EEG patterns misinterpreted as epileptiform [Citation4].
Epilepsy is a clinical diagnosis and heavily relies on accurate history, as many patients with epilepsy may have normal MRIs and normal routine EEGs [Citation5,Citation6]. The diagnosis of epilepsy can be and (usually is) accurately made without EEG-video or imaging when the history is appropriately suggestive of seizures, while a definitive diagnosis will require capturing the seizure on EEG-video monitoring. Although tests should not paramount clinical judgment; an erroneous diagnosis is often made due to a vague history and an overread (thus misread) EEG, with overemphasis on EEG [Citation6]. The most common reason for over-reading EEGs is the misinterpretation of normal variants or normal fluctuations of background rhythms [Citation3–Citation7].
2. Definition of phase reversals
One of the most misunderstood EEG patterns is the phase reversal [Citation8]. There are two types of montages: bipolar (when each electrode is linked to the next along a chain) and referential (when each electrode is compared to a common reference) [Citation9]. Based on basic principles of polarity and localization [Citation3,Citation9], on a bipolar montage the maximum voltage (negativity or positivity) is indicated by a phase reversal. Phase reversals are useful in that they are eye-catching and valuable in localizing the maximum voltage on bipolar montages (where the discharge is), but they do not carry any information regarding the nature of a voltage (what the discharge is). Phase reversals are indicative of the location of the maximum voltage and are especially useful in the localization of focal epilepsies when the discharge has met the criteria of epileptiform (with its morphology, duration, background disruption, etc.). However, by themselves, phase reversals do not indicate epileptogenicity or abnormality, and the correct utility of phase reversals lies only in the localization of where the maximum voltage is coming from on a bipolar montage. As shown in , the mention of phase reversals (in reports) is often implied to mean that a discharge is epileptogenic (suggestive of epilepsy). As illustrated in , they are seen in artifacts (physiologic and extra-physiologic), and normal rhythms. Because most epileptic discharges are surface-negative, negative phase reversals are the ones that are most often misinterpreted.
Figure 1. Excerpts of EEG reports, which erroneously imply that phase reversals are abnormal and indicative of epilepsy.
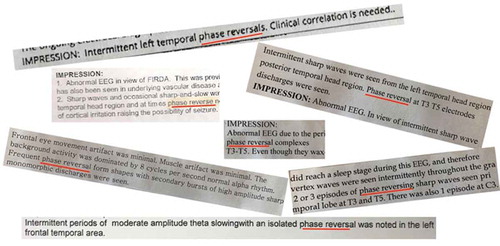
Figure 2. Montages are bipolar longitudinal for a, b, c, d, and transverse for e.

3. Artifacts with phase reversals
Artifacts, such as electrode ‘pops’ (a) often show phase reversals. Electrode ‘pops’ are caused by a sudden change in electrode impedance in a single electrode. Generally, discharges seen at only one contact should be considered artifactual until proven otherwise. Lateral eye movements and lateral rectus spikes (b) also show phase reversals due to the polarity of the eyeball. Eye movements are often mistaken for frontal lobe activity as the eye is electrically charged and any eye movement will be recorded from anterior leads. Positive cornea will move toward the temple to the side of gaze, resulting in positivity at that electrode and negativity on the contralateral side. Again, the presence of phase reversal here will only be a localizing tool.
4. Normal variants with phase reversals
Many normal variants cause phase reversals and are often confused for epileptiform activity. Small sharp spikes (SSS) (c) are small (<50 microV) and spiky (<50 msec) potentials in the temporal region during light sleep. They can shift from side to side with a normal EEG background. They can be confused with epileptiform discharges given their sharp appearance and the common misconception of phase reversals. It should be noted that SSS disappear in deep sleep, while epileptiform discharges tend to increase. Wicket spikes (d) are single or brief trains of sharply contoured waves in the temporal region during light sleep, and are common. They can be differentiated from epileptiform activity by their monomorphic morphology, absence of a following slow wave, and occurrence as part of a rhythm of the same frequency. Vertex waves (e) are another example of normal waveforms that can generate phase reversals, especially in a transverse montage. Vertex waves can be sharp, spike-like, and may occur in repetitive runs especially in children. Even a normal alpha rhythm can show phase reversals. Fast alpha variant and slow alpha variant are harmonic frequencies of the posterior dominant rhythm, often mistaken for seizures. When many frequencies are added together (harmonic) or cancel each other (subharmonic) they create a rhythmic waveform that can be mistaken for seizures.
5. Discussion
While the fallacy of phase reversals is probably the most common reason for over-reading EEGs as epileptiform, it is not the only one. Another contributing factor is the ‘history bias [Citation3–Citation7]’. When the history states ‘seizures,’ the reader tries too hard to find abnormalities [Citation5]. In addition to this, clinicians may be prone to over-read EEGs as they feel missing a diagnosis of epilepsy is riskier than over-diagnosing [Citation5]. Perhaps the most fundamental cause of overreading EEGs is the lack of mandatory EEG training in neurology residency [Citation5,Citation7].
Over-reading EEGs resulting in the misdiagnosis of epilepsy has life-changing consequences for patients on employment, driving, insurance, psycho-social wellbeing, and their overall quality of life. It also results in unwarranted treatments [Citation5]. In addition, once a misread EEG labels a patient as having epilepsy, this can be difficult to undo even with subsequent normal EEGs. The only way to undo the misdiagnosis is to review the ‘abnormal’ EEG; which can be challenging as recordings may not be available or digital system compatible [Citation6,Citation7].
It is reasonable for the lay public and non-neurologists to assume that all neurologists are trained to read EEGs, but that is obviously not the case [Citation4], at least in the US and some European countries [Citation10]. There is a need for guidelines on training and minimum requirements for neurologists to read EEGs.
6. Expert Opinion
Would the medical community and patients accept cardiologists not be formally trained to read EKGs? Of course not. Our non-neurology colleagues and the public assume, as they should, that all neurologists are trained to interpret EEGs. It is a little-known fact (and well-kept secret) that, at least in the US, there is no mandatory training in EEG during neurology residency. As a result, many neurologists have little to no training in EEG, even though they routinely interpret EEGs in their practice. As is always the case when a physician is inexperienced and uncomfortable with a particular test, the result is “over-reading” (calling abnormal what is normal). The same would happen if we as neurologists had to interpret chest CTs or liver MRIs. Phase reversals are but one example of misinterpretation, and only a small part of the larger issue of EEG over-interpretation and the subsequent misdiagnosis of seizures. Epilepsy is a life-changing diagnosis, and it is imperative that formal certification be required for neurologists who interpret EEGs.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Chadwick D. The misdiagnosis of epilepsy. BMJ. 2002 Mar 2;324(7336):495–496.
- Uldall P, Alving J, Hansen LK, et al. The misdiagnosis of epilepsy in children admitted to a tertiary epilepsy centre with paroxysmal events. Arch Dis Child. 2006;91(3):219–221.
- Benbadis SR. The EEG in nonepileptic seizures. J Clin Neurophysiol. 2006;23:340–352.
- Benbadis SR. Just like EKGs! Should EEGs undergo a confirmatory interpretation by a clinical neurophysiologist? Neurology. 2013;80(Suppl 1):S47–51.
- Amin U, Benbadis SR. The role of EEG in the erroneous diagnosis of epilepsy. J Clin Neurophysiol. 2019;36:294–297.
- Benbadis SR. The tragedy of over-read EEGs and wrong diagnoses of epilepsy. Expert Rev Neurother. 2010;10:343–346.
- Benbadis SR. Errors in EEGs and the misdiagnosis of epilepsy: importance, causes, consequences, and proposed remedies. Epilepsy Behav. 2007;1:257–262.
- Zemina K, Pennington ABenbadis SR. 2019. Phasing out the fallacy of phase reversals. Eur Neurol:. doi: 10.1159/000503627.
- Benbadis SR. Introduction to EEG. In: Lee-Chiong T, editor. Sleep: A comprehensive handbook. Hoboken, NJ: Wiley & Sons; 2006. p. 989–1024.
- Benbadis SR, Thomas P. When EEG is bad for you (Editorial). Clin Neurophysiol. 2017;128(4):656–657.
