ABSTRACT
Introduction: Although in some countries, palliative care (PC) still remains poorly implemented, its importance throughout the course of Parkinson’s disease (PD) is increasingly being acknowledged. With an emergence of Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) pandemic, growing emphasis has been placed on the palliative needs of people with Parkinson’s (PwP), particularly elderly, frail, and with comorbidities.
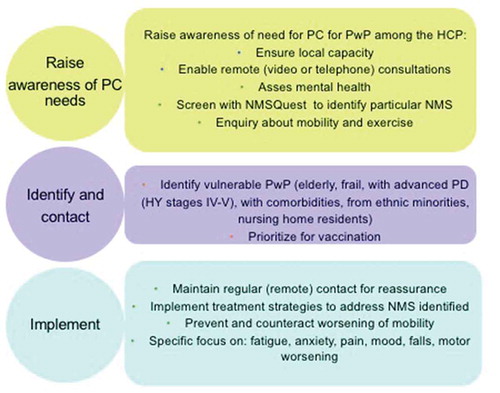
Areas covered: The ongoing COVID-19 pandemic poses an enormous challenge on aspects of daily living in PwP and might interact negatively with a range of motor and non-motor symptoms (NMS), both directly and indirectly – as a consequence of pandemic-related social and health care restrictions. Here, the authors outline some of the motor and NMS relevant to PC, and propose a pragmatic and rapidly deployable, consensus-based PC approach for PwP during the ongoing COVID-19 pandemic, potentially relevant also for future pandemics.
Expert opinion: The ongoing COVID-19 pandemic poses a considerable impact on PwP and their caregivers, ranging from mental health issues to worsening of physical symptoms – both in the short- and long-term, (Long-COVID) and calls for specific, personalized PC strategies relevant in a lockdown setting globally. Validated assessment tools should be applied remotely to flag up particular motor or NMS that require special attention, both in short- and long-term.
1. The need for a unified palliative care pathway for PwP during the COVID-19 pandemic with implications for the future pandemics
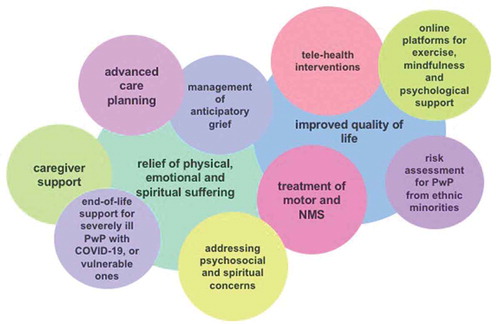
The importance of palliative care (PC) throughout the course of Parkinson’s disease (PD) has now increasingly been recognized. PC prioritizes quality of life (QoL) and focuses on prevention and relief of physical, emotional and spiritual suffering through a multidisciplinary approach, and in a holistic manner, being ‘patient-centered’ rather than ‘disease-centered’ intervention [Citation1,Citation2]. By contrast, traditional model of care for people with Parkinson’s (PwP), based on a patient-neurologist dyad, present in most countries, may not be sufficient to tackle the burden of motor and non-motor symptoms (NMS), both key determinants of QoL in PD [Citation3]. The emphasis on the palliative needs of PwP has gradually unfolded with the emergence of Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) pandemic, and its potential detrimental effect on PwP, particularly those at the advanced, complex phase of the condition [Citation4–6].
Emerging evidence outlines that the societal and physical impacts of the ongoing COVID-19 pandemic might interact negatively with a range of motor and NMS, and particularly with frailty associated with the advanced stages of PD. These effects may be attributable to the COVID-19 pandemic both directly and indirectly and call for specific, personalized strategies relevant in a lockdown setting over the globe [Citation7]. Furthermore, the development of such strategies may also allow for an intervention to be available for delivery and implementation, should there be a pandemic of a similar nature in the future [Citation7].
Here, we propose a clinically orientated and rapidly deployable, consensus-based, pragmatic palliative care approach for PwP relevant to the landscape of the ongoing COVID-19 pandemic and set a roadmap for future use globally. The proposed approaches detailed here are based on personally adopted strategies in several countries across different continents, as represented in the authorship of this paper.
2. Specific palliative care needs in PwP during the COVID-19 pandemic
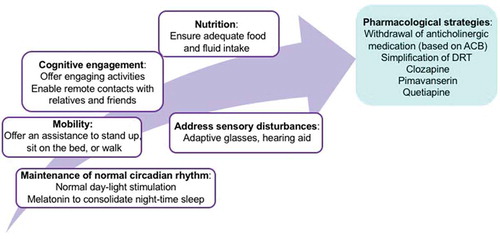
As highlighted in , two main principles form the foundation of the PC approach for PwP during the COVID-19 pandemic: the improvement of QoL, and the prevention and relief of physical, emotional and spiritual suffering. Of note, unlike the traditional postulation that PC is only relevant at the late stage of PD, we advocate for implementation of PC strategies earlier in the course of PD, at its moderate stages – ‘early integration of PC’. We propose that the enablers of these two principles can be mediated through the following interventions:
Figure 1. The possible enablers of patient-centered, holistic approach to palliative care for people with Parkinson’s during the COVID-19 pandemic. NMS – Non-motor symptoms, PwP – People with Parkinson’s
2.1. Clinical interventions to ensure adequate management of motor symptoms (worsening bradykinesia, akinesia and poor quality ‘off’ state) and prevention of deterioration
Available publications (a case study and several community-based studies) highlighted worsening of motor symptoms, particularly aggravation of bradykinesia and reduced mobility in PwP, particularly those at late stage and with associated frailty, during the COVID-19 pandemic [Citation4,Citation6]. Management strategies thus need to focus on preventing and counteracting the worsening of rigidity and tremor and decreasing mobility, considering the increased requirements for dopamine replacement therapy (DRT) in a personalized manner. Improved motor status can also indirectly enhance the patients’ ability to combat an infection [Citation7]. In frail, elderly PwP with an acute COVID-19 infection in a hospital environment, akinetic crisis mimicking a neuroleptic malignant-like syndrome (NMS) or Parkinson hyperpyrexia syndrome might occur – this calls for urgent restoration of dopamine balance and supportive measures (e.g., hydration, antipyretics, non-oral use of DRT) [Citation8].
2.2. Prevention and management of delirium
In elderly, frail PwP, COVID-19 infection itself possess a risk of delirium; personal protective equipment (PPE), limited cognitive stimulation and mobility and restricted social interactions may act as further contributing factors. For example, due to restricted visiting policies, loss of access to face to face interpreters might aggravate confusion in PwP whose native language differs from the one in the country they are residing in. In turn, delirium may lead to increased morbidity, prolonged hospital stays and increased mortality. Thus, systematic assessment and early recognition of delirium are essential [Citation9–11]. Proposed strategies for the prevention and management of delirium(both hypo- and hyperactive) in PwP affected by COVID-19 are summarized in .
2.3. Management of non-motor symptoms
Current evidence suggests worsening of a range of NMS associated with COVID-19 infection, with a particularly severe impact on PwP at late, palliative stages of PD. These symptoms are listed in . and range from neuropsychiatric issues to pain [Citation4,Citation5,Citation12]. Worsening of NMS such as pain, anxiety and depression could also be an indirect consequence of the pandemic and related restrictions [Citation13–15]. Of note, a detailed discussion on interventions for optimal treatment of particular NMS is beyond the scope of this paper; an International Parkinson and Movement Disorders Society Evidence-based Medicine (MDS-EBM) Task Force guidelines should be followed [Citation16]. In addition, management of non-motor complications in a late stage PD has been extensively reviewed recently [Citation17].
Figure 3. Worsening of particular non-motor symptoms in PwP during the COVID-19 pandemic. PwP – People with Parkisnon’s, NMS - Non-motor symptoms,NMSQuest – Non-motor Symptoms Questionnaire
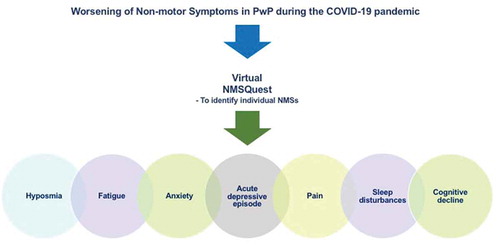
We advocate for the use of validated tools, such as the self-completed NMS Questionnaire (NMSQuest), which can be applied remotely and allows for time-efficient staging of NMS burden, while also flagging up particular NMS occurring as an integral part of ‘COVID-19 PD Syndrome’ that require special attention, both in short- and long-term [Citation18–20]. . Once a specific NMS is identified using NMSQuest, symptom-specific instruments may be used to further delineate and quantify the problem (e.g., MOCA in the case of cognitive deterioration) [Citation21].
Some of the specific NMS of importance for PC are highlighted below.
Fatigue: Fatigue has been identified as one of the NMS dominating the acute COVID-19 infection [Citation4,Citation5]. Several reports described a chronic post-viral fatigue syndrome after COVID-19 infection, marked by an overwhelming sense of tiredness and lack of energy, that might possibly continue for a long time, now being recognized as an integral part of the ‘Long-COVID’ syndrome [Citation22,Citation23].
Anxiety: Anxiety was at the forefront of symptoms reported in the initial case series by Antonini et al. and continues to be reported in PwP affected by COVID-19 [Citation4]. In addition, anxiety, particularly in PwP at late stages of the disease, is a common consequence of prolonged shielding, homestay and lack of exercise. Uncertainty related to, for example, the deployment of clinical staff to the frontline, which has led to restricted access to established care pathways for PwP in many countries, might be an additional contributing factor [Citation4,Citation5,Citation13,Citation15,Citation24].
Depression: During the COVID-19 pandemic, prevalence and severity of depression, as measured by Hospital Anxiety and Depression Scale (HADS) is higher among PwP than in healthy population [Citation25]. Periods of acute depressive episodes have been witnessed in late stage PD, often coinciding with anxiety. Furthermore, mood disturbances (depression and anxiety) are one of the major aspects of the clinical expression of the ‘Long-COVID’ syndrome [Citation22].
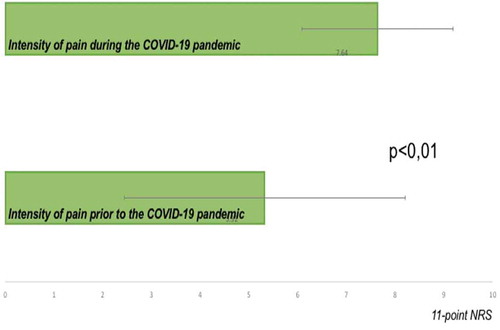
Pain: A substantial proportion of PwP affected by COVID-19 suffers from musculo-skeletal pain, while in those non-infected, worsening of pre-existing PD-related pain amid the ongoing COVID-19 pandemic has been reported [Citation5,Citation13,Citation15]. Data capture from tele-health consultations for PwP during the lockdown in a UK center found significant worsening of pain in PwP, most likely attributable to social isolation and lifestyle changes associated with shielding. 64% of PwP across all Hoehn and Yahr (HY) stages declared worsening of pain amid the ongoing COVID-19 pandemic. On the 11-point Numeric Rating Scale, patients scored the pain present at the time point of the assessment significantly higher than the pain they were experiencing prior to the pandemic (7.64 ± 1.55 vs. 5.32 ± 2.88; p < 0,01) [Citation26,Citation27]. .
Figure 4. Worsening of PD-related pain during the COVID-19 pandemic – King’s experience. NRS – Numeric rating scale
Sleep disturbances: In PwP, particularly those at later stages of the disease, pandemic-related social isolation and home confinement may adversely affect the quality of nighttime sleep. Importantly, worsening of pre-existing or a new onset of sleep disturbances might possibly further contribute to secondary worsening of motor and NMS [Citation28]. Thus, addressing both primary and secondary insomnia, rapid eye movement sleep behavior disorders (RBD) and excessive daytime sleepiness should be an integral part of PC for PwP during the COVID-19 pandemic.
Cognitive impairment: COVID-19-related restrictions might possibly lead to a degree of a decline in cognitive performances in a proportion of PwP; possibly even causing the conversion from mild cognitive impairment to significant cognitive impairment in some patients at the late or palliative stage of PD [Citation29]. Worryingly, worsening of cognition has emerged as a symptom integral to the Long-COVID syndrome and may be specifically relevant for PwP .
3. Risk assessment for patients from ethnic minorities
Individuals from ethnic minorities have been affected by COVID-19 in a disproportionate manner, with higher mortality and morbidity reported [Citation7,Citation30]. In British hospitals, COVID-19 mortality rate is 3.5 times higher in people of Black African descent, than in White patients [Citation31]. Of note, in individuals with an ethnic minority background, PC interventions need to be tailored in accordance with the cultural, religious and spiritual beliefs of the communities involved.
4. Outcome measures in palliative care for people with Parkinson’s
Patient centered PC outcome measures might aid the recognition of complex PC needs in PwP, beyond those related solely to physical symptoms.
Frequently used for general PC purposes, the Palliative Outcome Scale (POS) comprises two parts: a staff-completed and a patient-completed form, with 10 questions addressing physical, psychological, and spiritual domains of life within the remit of PC. An open section at the end of the scale provides the opportunity to list the main problems as an additional input. With an estimated completion time of less than 10 minutes, this scale is brief and simple to administer [Citation32]. Based on the POS, the IPOS-Neuro S8 was designed and validated specifically for individuals with progressive long-term neurological conditions, and could aid remote clinical assessments, although specific validation in PwP is awaited [Citation33].
5. Addressing psychosocial and spiritual concerns and management of anticipatory grief
These issues are prevalent in PwP, similarly to many other patients of differing conditions. Spiritual care is an openness toward spiritual dimension and acknowledges both patients’ and caregivers’ resources and needs, while also being tolerant toward and accepting patients’ and caregivers’ wish not to discuss spiritual needs and concerns with healthcare providers [Citation34–36]. Spiritual care in palliative care pays attention to spirituality via presence, empowerment, and bringing peace [Citation37].
During the pandemic, the need to recommit to spiritual care as an essential component of whole-person PC may not have been fully respected in some settings. For instance, reduced ability to engage in one’s usual religious community has been a source of spiritual distress for many of our patients. Furthermore, there are also concerns about the future, spanning finances, personal appearance, identity and social relationships. Coping strategies, such as meditation and prayer, are important sources of strength for some PwP and might have important implications in the management of psychosocial and spiritual distress and anticipatory grief [Citation14,Citation38]. Moreover, certain religious communities favor dying at home rather than in a hospice or hospital, while for others, visiting at death or washing the body after death is obligatory. Where practicable, such requirements need to be accommodated in clinical pathways in order to mitigate further distress.
6. Advanced care planning
In the landscape of COVID-19 pandemic, advanced care planning (ACP) is necessary in order to meet patient’s care goals and avoid potentially unwanted interventions, such as intubation, ventilation and intensive care unit admissions in the case of irreversible worsening. Health-care professionals should review the ACP and discuss goals of care with PwP and their families during the routine consultations. If PwP contract COVID-19 and a hospital admission is necessary, the advance directive should accompany the patient [Citation39]. In certain countries, ACP forms may include a free text area allowing clinicians to document patient’s and family’s expressed goals beyond a level of care designation.
7. End-of-life support
There has been a substantial variability in the reported mortality rates among PwP affected by COVID-19. For example, in a dual center case series including hospitalized PD patients affected by COVID-19 (mean age 78.3 years, mean disease duration 12.7 years, mainly living in a nursing home), mortality rate was 40% [Citation4]. Overall, mortality rate in elderly and frail PwP at late stages of PD appears to be high. For example, in another cohort-based study, mortality rate was as high as 75% [Citation40]. End of life support strategies based on PC approach in this subset of patients are therefore an imperative and currently an unmet need [Citation13,Citation41–44].
In addition, the COVID-19 pandemic might have an indirect effect on the mortality in PwP, and higher-than-expected rate of deaths in hospitalized PwP, irrespective of the infection with SARS-CoV-2, has been reported during this period [Citation45].
However, notably, a ‘one size fits all’ approach toward rationing scarce resources such as ventilation is not appropriate for all PD patients, as there is a broad consensus that long term outcome in PwP at HY stage 1 or 2 may be substantially different thanin those on HY stages 4 and 5. Thus, generic restrictions of ventilatory support, based solely on the PD diagnosis itself, as per current jurisdictions in certain countries, should not occur. Instead, a clear plan regarding end of life decision making process needs to be made on a case by case basis.
8. Caregiver support
Caregivers of PwP have considerable needs that need to be addressed through PC approach [Citation38]. Of note, PwP’s motor and NMS are important predictor of caregivers’ QoL, which might therefore be diminished in the current pandemic [Citation46]. In turn, higher caregiver burden is associated with adverse outcomes, whereas presence of caregiver reduces spiritual distress and improves QoL in PwP [Citation47,Citation48]. During the ongoing COVID-19 pandemic, shielding at home and restrictions of home care packages increase caregiver burden and there might be a need for a special task forces to tackles the issues caregivers might be facing (e.g. burn out, depression) and provide a platform for exchange [Citation49]. Domestic stress might be aggravated during periods of forced lockdown, adding an additional layer of stress for both caregivers and PwP [Citation49]. Specific plans regarding support of caregivers in this situation are therefore important and should be integral to the overall PC strategy.
9. Vaccination
As of December 2020, vaccination is available against COVID-19 infection and late and particularly palliative stage PwP should be considered a priority group to be vaccinated, along with their caregivers. Vaccination is identified as safe for PwP, and it does not interfere with a course of the disease. A similar strategy in relation to vaccination of vulnerable subjects with multiple sclerosis has been proposed and can be adopted for palliative PD [Citation50].
10. ‘Long-COVID’ in PD – implications for long-term care
The UK National Institute for Health and Care Excellence issued guidelines for management of long-term effects of COVID-19, referred as ‘Long-COVID’, and comprising signs and symptoms with an onset during or after the acute COVID-19 illness, persistent for more than 12 weeks, and not explained by an alternative underlaying diagnosis [Citation51]. Wide range of symptoms may occur after an acute COVID-19 illness; they may fluctuate in severity and change their nature over time. In PwP, post-COVID-19 syndrome may interact negatively with common NMS, unmasking fatigue, pain, sleep disturbances and cognitive impairment and the evaluation of these aspects using validated screening tools is of paramount importance [Citation52,Citation53].
11. Expert opinion
Despite certain differences in opinions, PwP, particularly those with an advanced disease, are now widely recognized as a vulnerable group, with higher mortality rates of COVID-19 being reported. Several studies suggest that elderly and frail PwP, or those with significant additional cardiovascular, metabolic or respiratory comorbidities might be particularly vulnerable and may thus fall under the umbrella of palliative care. The specific symptomatic approach to care for PwP during the ongoing COVID-19 pandemic needs to recognize and address a potential worsening of, or emergence of, specific PD features, both motor and non-motor, as outlined in this paper.While the management of NMS such as fatigue, insomnia, anxiety and pain may be of a particular relevance in the short term, PwP affected by COVID-19 may potentially require further interventions for ‘Long-COVID’ related symptoms in the long run – namely, a personalized care approach might be required to tackle the cognitive decline, a common symptom of the ‘Long-COVID’. A unified and personalized PC approach should seek to combine successful symptomatic relief of both motor and NMS, while also addressing issues related to end-of-life care in those critically ill, providing management of psycho-social concerns and spiritual beliefs, specifically if there is vaccine uptake hesitancy, and offer a clear pathway for caregiver support.
A composite, modern and time relevant PC strategy therefore needs to consider the above strands of care, as well as allow personalization considering the needs of each individual, local pathways of care and clinical team preferences. The delivery of this care pathway becomes even more difficult during the pandemic, as face-to-face consultations or home visits may be restricted, or even impossible in many countries. The consequent effect on vulnerable patients and their caregivers is considerable and ranges from mental health issues to worsening of physical symptoms. Therefore, a feasible care plan that can be delivered virtually and tackles the above concerns as far as possible needs to be developed and implemented. Where the infrastructure permits to do so, ‘virtual clinics’ or consultations have been implemented. However, in some countries, this may not be possible and alternative routes must be sought via the use of smartphone apps or telephone contact to reach the ‘hard-to-reach’ population. For example, a hotline for stress relief for PwP and their families might serve as a front door approach, ameliorating a degree of initial stress and identifying those who may need urgent medical care. Aspects of NMS, such as anxiety, and loneliness can be helped by tele-health consultations while exercise strategies to help motor state, or support for speech, could be delivered through online platforms by trained therapists. The adjustments of the dopaminergic and other medication can be performed remotely to improve the motor and non-motor status of the patient, thus default helping the caregiver as well. The clinical decision making here might be aided by wearable sensors which allow for continuous remote monitoring of symptoms. Specific screening tools, such as NMS Questionnaire (NMSQuest), POS, IPOS-Neuro S8,PDQ-8 or PD Sleep Scale (PDSS) can be administrated remotely to assess certain NMS and should be encouraged [Citation18,Citation54,Citation55,Citation32,Citation33]. Only a concerted effort by key stakeholders, clinicians, allied health specialists, patients, caregivers and policymakers would make optimal palliative care delivery for the most vulnerable PD patients possible and prepare for future pandemics, should they arise.
Article highlights
Palliative care (PC) prioritizes quality of life (QoL) and focuses on the prevention and relief of physical, emotional and spiritual suffering through a multidisciplinary approach, and in a holistic manner; it is ‘patient-centered’ rather than ‘disease-centered’
The current COVID-19 pandemic might interact negatively with a range of motor and non-motor symptoms (NMS) people with Parkinson’s disease (PD, PwP) experience.
Validated screening tools, such as the self-completed NMS Questionnaire (NMSQuest), should be applied remotely for staging of NMS burden and flagging up of particular NMS, while symptom-specific instruments may be used to further delineate and quantify the problem
PC approaches for PwP during the COVID-19 pandemic should address the management of psychosocial and spiritual distress and anticipatory grief
During the COVID-19 pandemic, shielding at home and restrictions of home care packages might enhance caregiver burden
Advanced care planning (ACP) is necessary in order to meet patient’s care goal and avoid potentially unwanted interventions such as intubation, ventilation and intensive care unit admissions in the case of irreversible worsening; a clear plan regarding end-of-life decision-making process needs to be made on a case by case basis.
Declaration of interest
K Ray Chaudhuri has acted on advisory board for AbbVie, UCB, GKC, Bial, Cynapsus, Novartis, Lobsor, Stada, Medtronic, Zambon, Profile, Sunovion, Roche, Therevance, Scion and Britannia, and has received honoraria for lectures from AbbVie, Britannia, UCB, Mundipharma, Zambon, Novartis, Boeringer Ingelheim, and grants (Investigator Initiated) from Britania Pharmaceuticals, AbbVie, UCB, GKC, Bial, Academic grants: EU, IMI EU, Horizon 2020, Parkinson’s UK, NIHR, PDNMG, EU (Horizon 2020), Kirby Laing Foundation, NPF, MRC, Welcome Trust. K Rukavina is supported by NIHR-BRC and has received personal fees from Britannia Pharmaceuticals Ltd. And from Profile Pharma, and consultancy fee from Valid Insght. A Antonini has received compensation for consultancy and speaker-related activities from UCB, Boehringer Ingelheim, Britannia, AbbVie, Kyowa Kirin, Zambon, Bial, Neuroderm, Theravance Biopharma, Roche; he receives research support from Chiesi Pharmaceuticals, Bial, Lundbeck, Horizon 2020 - Grant 825,785, Horizon2020 Grant 101,016,902, Ministry of Education University and Research (MIUR) Grant ARS01_01081, Cariparo Foundation. He serves as consultant for Boehringer–Ingelheim for legal cases on pathological gambling. R Walker has received the following grants: NIHR Research and Innovation for Global HealthTransformation NIHR 200,134 - Epilepsy Pathway Innovation in Africa (EPInA), Global Health Research Group on Dementia Prevention and Enhanced Care (DePEC), Global Health Research group on estimating the prevalence, quality of life, economic and societal impact of arthritis in Tanzania, MRC GACD Mental Health Call – Cognitive Stimulation Therapy for Dementia: International Implementation in Brazil, India and Tanzania (CST – International), Parkinsons UK, Trial of Ondansetron as a Parkinson’s Hallucinations treatment (TOP HAT), General Research Fund (GRF) and Early Career Scheme (ECS), University of Hong Kong - ‘Mindfulness in stillness’ or ‘mindfulness in motion’, Parkinson’s UK - Non-drug approaches: A wearable device for cueing for the management of drooling, and monitoring of symptoms, in people with Parkinson’s. R Bhidayasiri receives salary from Chulalongkorn University and stipend from the Royal Society of Thailand, has received consultancy and/or honoraria/lecture fees from Abbott, Boehringer-Ingelheim, Britannia, Ipsen, Novartis, Teva-Lundbeck, Takeda, and Otsuka pharmaceuticals; he has received research funding from the Newton Fund, the UK Government, Thailand Science and Research Innovation Bureau, Thailand Research Fund, Crown Property Bureau, Chulalongkorn University, and the National Science and Technology Development Agency; he holds patents for laser-guided walking stick, portable tremor device, nocturnal monitoring, and electronic Parkinson’s disease symptom diary as well as copyright on Parkinson’s mascot, dopamine lyrics and teaching video clips for common nocturnal and gastrointestinal symptoms for Parkinson’s disease. SY Lim reports lecturing honoraria from the International Parkinson and Movement Disorder Society, Medtronic, and the Shanghai 2020 Ruijin Forum for Translational Neurodegeneration; stipend (Working Group Co-Lead Award) from the Michael J. Fox Foundation; consultation fees from Lundbeck; and Research funding from the Michael J. Fox Foundation. JM Miyasaki is supported through the University Hospital Foundation, Alberta by the Dennis and Doreen Erker Fund. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or conflict with the subject matter or materials discussed in this manuscript apart from those disclosed.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgments
The authors would like to thank all the health care workers and patient support groups for their efforts during the pandemic.
Additional information
Funding
References
- Kluger BM, Miyasaki J, Katz M, et al. Comparison of integrated outpatient palliative care with standard care in patients with Parkinson disease and related disorders: A randomized clinical trial. JAMA Neurol. 2020;77(5):551–560.
- Prizer LP, Gay JL, Wilson MG, et al. A mixed-methods approach to understanding the palliative needs of Parkinson’s patients. J Appl Gerontol. 2020;39(8):834–845.
- Martinez-Martin P, Rodriguez-Blazquez C, Kurtis MM, et al. The impact of non-motor symptoms on health-related quality of life of patients with Parkinson’s disease. Mov Dis. 2011;26(3):399–406.
- Antonini A, Leta V, Teo J, et al. Outcome of Parkinson’s disease patients affected by COVID-19. Mov Disord. 2020;35(6):905–908.
- Cilia R, Bonvegna S, Straccia G, et al. Effects of COVID-19 on Parkinson’s disease clinical features: a community-based case-control study. Mov Disord. 2020;35(8):1287–1292.
- Fasano A, Cereda E, Barichella M, et al. COVID-19 in Parkinson’s disease patients Living in Lombardy, Italy. Mov Disord. 2020 July;35(7):1089–1093.
- Sulzer D, Antonini A, Leta V, et al. COVID-19 and possible links with Parkinson’s disease and parkinsonism: from bench to bedside. NPJ Parkinson’s Dis. 6(1):18. 2020.
- Hocker S, Kenney DL, Ramar K. Parkinsonism-hyperpyrexia syndrome: broadening our differential diagnosis in the ICU. Neurol Clin Pract. 2013;3(6):535–538.
- Zazzara MB, Penfold RS, Roberts AL, et al. Probable delirium is a presenting symptom of COVID-19 in frail, older adults: a cohort study of 322 hospitalised and 535 community-based older adults. Age Ageing. 2021;50(1):40–48.
- Syed S, Couse M, Ojha R. Management challenges in patients with comorbid COVID-19 associated delirium and serious mental illness - A case series. Int J Psychiatry Med. 2021;91217420985979. 10.1177/0091217420985979
- Radhakrishnan NS, Mufti M, Ortiz D, et al. Implementing Delirium prevention in the Era of COVID-19. JAD. 2021;79(1):31–36.
- Guo D, Han B, Lu Y, et al. Influence of the COVID-19 pandemic on quality of life of patients with Parkinson’s Disease. Parkinsons Dis. 2020;2020:1216568.
- Brown EG, Chahine LM, Goldman SM, et al. The effect of the COVID-19 pandemic on people with Parkinson’s Disease. J Parkinsons Dis. 2020;10(4):1365–1377.
- Helmich RC, Bloem BR. The impact of the COVID-19 pandemic on Parkinson’s Disease: hidden sorrows and emerging opportunities. J Parkinsons Dis. 2020;10(2):351–354.
- Van Der Heide A, Meinders MJ, Bloem BR, et al. The impact of the COVID-19 pandemic on psychological distress, physical activity, and symptom severity in Parkinson’s Disease. J Parkinsons Dis. 2020;10(4):1355–1364.
- Seppi K, Ray Chaudhuri K, Coelho M, et al. Update on treatments for nonmotor symptoms of Parkinson’s disease-an evidence-based medicine review. Mov Disord. 2019;34(2):180–198.
- Rukavina K, Batzu L, Boogers A, et al. Non-motor complications in late stage Parkinson’s disease: recognition, management and unmet needs. Expert Rev Neurother. 2021;21(3):335–352.
- Chaudhuri KR, Martinez-Martin P, Schapira AH, et al. International multicenter pilot study of the first comprehensive self-completed nonmotor symptoms questionnaire for Parkinson’s disease: the NMSQuest study. Mov Disord. 2006;21(7):916–923.
- Van Wamelen DJ, Martinez-Martin P, Weintraub D, et al. The non-motor symptoms scale in Parkinson’s disease: validation and use. Acta Neurol Scand. 2021 January;143(1):3–12.
- Chaudhuri KR, Sauerbier A, Rojo JM, et al. The burden of non-motor symptoms in Parkinson’s disease using a self-completed non-motor questionnaire: a simple grading system. Parkinsonism Relat Disord. 2015;21(3):287–291.
- Nasreddine ZS, Phillips NA, Bedirian V, et al. The montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699.
- Williams FMK, Muirhead N, Pariante C. Covid-19 and chronic fatigue. BMJ. 2020;370:m2922.
- Lazcano-Ocampo C, Wan YM, Van Wamelen DJ, et al. Identifying and responding to fatigue and apathy in Parkinson’s disease: a review of current practice. Expert Rev Neurother. 2020;20(5):477–495.
- Salari M, Zali A, Ashrafi F, et al. Incidence of anxiety in Parkinson’s disease during the coronavirus disease (COVID-19) Pandemic. Mov Disord. 2020 July;35(7):1095–1096.
- Xia Y, Kou L, Zhang G, et al. Investigation on sleep and mental health of patients with Parkinson’s disease during the coronavirus disease 2019 pandemic. Sleep Med. 2020;75:428–433.
- Farrar JT, Young JP Jr., LaMoreaux L, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158.
- Hoehn MM, Yahr MD. Parkinsonism: onset, progression, and mortality. Neurology. 1967;17(5):427–442.
- Kumar N, Gupta R, Kumar H, et al. Impact of home confinement during COVID-19 pandemic on sleep parameters in Parkinson’s disease. Sleep Med. 2021;77:15–22.
- Palermo G, Tommasini L, Baldacci F, et al. Impact of coronavirus disease 2019 pandemic on cognition in Parkinson’s disease. Mov Disord. 2020;35(10):1717–1718.
- https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/892376/COVID_stakeholder_engagement_synthesis_beyond_the_data.pdf
- Otu A, Ahinkorah BO, Ameyaw EK, et al. One country, two crises: what Covid-19 reveals about health inequalities among BAME communities in the United Kingdom and the sustainability of its health system? Int J Equity Health. 2020;19(1):189.
- Hearn J, Higginson IJ. Development and validation of a core outcome measure for palliative care: the palliative care outcome scale. Palliative care core audit project advisory group. Quality in health care: QHC. 1999;8(4):219–227.
- Gao W, Crosby V, Wilcock A, et al. Psychometric properties of a generic, patient-centred palliative care outcome measure of symptom burden for people with progressive long term neurological conditions. PloS One. 2016;11(10):e0165379.
- Best M, Leget C, Goodhead A, et al. EAPC white paper on multi-disciplinary education for spiritual care in palliative care. BMC Palliat Care. 2020;19(1):9.
- Frick E. Spiritual Care – how does it work? Spiritual Care. 2017;6(2):223–224.
- Paal P, Lorenzl S. Patients with Parkinson’s disease need spiritual care. Ann Palliat Med. 2020 March;9(2):144–148.
- Gijsberts M-JHE, Liefbroer AI, Otten R, et al. Spiritual care in Palliative care: a Systematic review of the recent European Literature. Med Sci. 2019;7(2):25.
- Boersma I, Jones J, Coughlan C, et al. Palliative care and Parkinson’s disease: Caregiver perspectives. J Palliat Med. 2017;20(9):930–938.
- Subramanian I, Christina LV. Hoping for the best, planning for the worst: palliative care approach to Parkinson disease during the COVID-19 pandemic. In: Parkinsonism & related disorders. 2020;80:203-205.
- Artusi CA, Romagnolo A, Imbalzano G et al. COVID-19 in Parkinson’s disease: report on prevalence and outcome. Parkinsonism & related disorders. 2020;80:7–9
- Fasano A, Elia AE, Dallocchio C, et al. Predictors of COVID-19 outcome in Parkinson’s disease. Parkinsonism Relat Disord. 2020;78:134–137.
- Sainz-Amo R, Baena-Alvarez B, Parees I, et al. COVID-19 in Parkinson’s disease: what holds the key? J Neurol. 2020;24:1–5.
- Del Prete E, Francesconi A, Palermo G, et al. Prevalence and impact of COVID-19 in Parkinson’s disease: evidence from a multi-center survey in Tuscany region. J Neurol. 2021 April;268(4):1179–1187.
- Miyasaki JM, Long J, Mancini D, et al. Palliative care for advanced Parkinson disease: an interdisciplinary clinic and new scale, the ESAS-PD. Parkinsonism Relat Disord. 2012;18(Suppl 3):S6–9.
- Kobylecki C, Jones T, Lim CK, et al. Phenomenology and outcomes of in-patients with Parkinson’s disease during the Coronavirus disease 2019 pandemic. Mov Dis. 2020;35(8):1295–1296.
- Klietz M, Schnur T, Drexel S, et al. Association of motor and cognitive symptoms with health-related quality of life and Caregiver burden in a German Cohort of advanced Parkinson’s disease patients. Parkinsons Dis. 2020;2020:5184084.
- Prizer LP, Kluger BM, Sillau S, et al. The presence of a caregiver is associated with patient outcomes in patients with Parkinson’s disease and atypical parkinsonisms. Parkinsonism Relat Disord. 2020;78:61–65.
- Macchi ZA, Koljack CE, Miyasaki JM, et al. Patient and caregiver characteristics associated with caregiver burden in Parkinson’s disease: a palliative care approach. Ann Palliat Med. 2020;9(Suppl 1):S24–S33.
- Schmotz C, Richinger C, Lorenzl S. High burden and depression among late-stage idiopathic Parkinson disease and progressive supranuclear palsy caregivers. J Geriatr Psychiatry Neurol. 2017;30(5):267–272.
- Reyes S, Ramsay M, Ladhani S, et al. Protecting people with multiple sclerosis through vaccination. Pract Neurol. 2020;20(6):435–445.
- https://nice.org.uk/guidance/ng188
- Tancheva L, Petralia MC, Miteva S, et al. Emerging neurological and psychobiological aspects of COVID-19 infection. Brain Sci. 2020;10(11):11.
- Leta V, Rodríguez-Violante M, Abundes A et al. Parkinson's Disease and Post-COVID-19 Syndrome: The Parkinson's Long-COVID Spectrum. Mov Disord. 2021 Apr 22. doi:10.1002/mds.28622. Epub ahead of print. PMID: 33890344.
- Chaudhuri KR, Pal S, DiMarco A, et al. The Parkinson’s disease sleep scale: a new instrument for assessing sleep and nocturnal disability in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2002;73(6):629–635.
- Jenkinson C, Fitzpatrick R, Peto V, et al. The Parkinson’s disease questionnaire (PDQ-39): development and validation of a Parkinson’s disease summary index score. Age Ageing. 1997;26(5):353–357.