ABSTRACT
Introduction
COVID-19 presented major challenges to undergraduate GP placement capacity and there was an increased reliance on clinical training using facilitated simulation. The authors present a novel comparison of the effectiveness and cost-effectiveness of delivering a one-week primary care course using entirely GP-facilitated clinical teaching outside the GP setting against traditional practice-based GP clinical education.
Methods
A one-week GP placement was redeveloped from a traditional teaching model (TT-M) to an exclusively facilitated teaching model (FT-M) delivered outside the GP practice setting, using principles of blended learning, flipped classroom methods, e-learning and simulation. Both teaching models, delivered in different locations during 2022 to pre-clinical students, were evaluated using student feedback surveys for attainment of learning outcomes and course satisfaction.
Results
The students reported their consultation skills and clinical knowledge (amalgamated mean score 4.36 for FT-M versus 4.63 for TT-M; P = 0.05), as well as preparation for the clinical phases (mean scores 4.35 for FT-M versus 4.41 for TT-M; P = 0.68), were well developed and similar for both courses. Students reported similar enjoyment across both teaching models (FT-M mean score 4.31 versus 4.41 for TT-M; P = 0.49). The costs for delivering teaching per 4-h session for 100 students were £1,379 and £5,551 for FT-M and TT-M, respectively.
Conclusion
Delivery of a one-week primary care attachment to third year medical students using an FT-M was similarly effective and more cost effective than delivering it by a TT-M. FT-M potentially offers an important adjunct to clinical learning and resilience to capacity challenges for GP placements.
Introduction
There have been increasing pressures on capacity for training healthcare professionals in primary care. These were exacerbated by the COVID pandemic through restricting access to learning in clinical environments and prioritising core clinical activities over medical training [Citation1]. In 2021, General Practice (GP) Specialty Training in England and Wales was reconfigured, increasing the training time in GP practices from 18 to 24 months [Citation2] in parallel to increased trainee numbers [Citation3], further straining training capacity.
A new clinical curriculum was introduced at Nottingham Medical School (NMS) in February 2022, which increased medical student exposure in primary care. This included Early Primary Care (EPC), a new one-week clinical placement in primary care for third-year medical students, to bridge the transition from pre-clinical training into a new clinical curriculum. Students’ clinical experiences to this point, during pre-clinical training at NMS, would normally have included five single days in general practice and seven half-day hospital visits. For the cohort of students in question however, this clinical experience had unfortunately been limited to 1 day in general practice and two short hospital visits, due to the impact of the COVID pandemic. EPC aimed to further develop clinical skills in GP practice settings, in particular history taking, before students entered full-time clinical training.
Undergraduate GP placement capacity challenges, linked to the above, peaked prior to implementation of the new clinical curriculum at NMS. Therefore, an alternative method for clinical training of third-year medical students was developed for EPC using an exclusively GP-facilitated teaching model. This contrasted with the traditional approach of learning primarily within GP practices.
This teaching evaluation describes how this novel course was re-developed and delivered to undergraduate medical students, and provides a comparison of the effectiveness and cost-effectiveness of using this exclusively GP-facilitated model of clinical training to traditional practice-based GP education.
Methods
The Early Primary Care (EPC) course
Learning outcomes
EPC aimed to help students refresh and further develop clinical skills of consulting, in particular history taking and basic diagnostic reasoning. Secondary aims were to enable students to recognise non-medical factors influencing health and patient responses to illness and develop greater awareness of the roles of non-GP multidisciplinary team members.
Learning outcomes were for students to be able to:
Demonstrate appropriate professional attitudes and behaviours
Build on basic skills of communication to communicate effectively with patients in primary care and begin to use targeted history taking to aid diagnosis and clinical decision making
Witness and be able to evaluate the psychological and sociological considerations that can affect patients’ health and their responses to illness and its management
Experience and analyse the different roles and consulting practices of other health care professionals working in the primary care team and how these contribute to the overall care of patients
Original EPC course
EPC was originally developed using a ‘traditional-teaching’ model (TT-M), with students mostly spending time within GP practices as part of a one-week placement (5 days/10 sessions/half days – ), comprising mostly of clinical learning in GP practices (patient encounters to develop consultation/history-taking skills) supplemented by up to 2 days of GP-facilitated small group teaching (SGT).
Figure 1. Timetables for delivery of facilitated teaching model (A) and traditional-teaching model (B).
EPC was designed in a backward process [Citation4,Citation5], beginning with focus groups exploring perceived student learning needs prior to clinical phase training and a modified Delphi exercise [Citation6] exploring GP educator views of student learning needs, to develop course aims and learning outcomes. An assessment strategy, using constructive alignment [Citation7], was developed which then informed learning and teaching methods.
Redesign to exclusively facilitated teaching course
Due to the aforementioned capacity pressures on GP medical student placements, EPC was redesigned to be delivered using an exclusively GP-facilitated teaching model (FT-M) delivered outside the practice setting. New teaching sessions were developed to replace the planned clinical learning within GP practices, drawing on previous faculty experiences of virtual clinical training [Citation8–13] and using principles of blended learning [Citation14,Citation15], flipped classroom methods [Citation16,Citation17], e-learning [Citation9,Citation12,Citation18] and simulation [Citation19,Citation20]. Teaching sessions were balanced for face-to-face and virtual interactions with educators and included GP-facilitated SGT (6–12 students), lectures and self-directed interactive e-learning ().
Students received two lectures (totalling one teaching session) given by GPs, three self-directed e-learning sessions and six GP-facilitated SGT sessions (). Clinical educators were Royal College of General Practitioners (RCGP) accredited GPs. Professional actors, used for simulated surgeries, and experienced patient volunteers were recruited from existing education networks.
Table 1. Comparison of teaching resources used in facilitated teaching (FT-M) and traditional teaching (TT-M) models for the delivery of Early Primary Care (EPC).
Evaluation of EPC
Survey methods
Student feedback, using surveys comprising closed Likert-scale and free-text open questions about perceived experiences, was used as a proxy measure for course effectiveness to attain learning outcomes. Questions asked students to rate their achievement of core learning outcomes/aims, enjoyment of EPC and its impact on preparing students for subsequent clinical training.
The Likert Scale questions, scored 1–5 (5=Excellent; 4=Good; 3=Neutral; 2=Poor; 1=Very Poor), were:
The [course] has helped me develop my consultation skills
The [course] has helped me develop my clinical knowledge
I have enjoyed the [course]
I feel better prepared to start [the clinical phase] as a result of the experiences I have had this week
The free-text open questions were:
Please state the aspects of the [course] you have found the most useful and enjoyable
Please state the aspects of the [course] that you would like to see changed or improved
Comparator for evaluation
The EPC course was delivered to students at Lincoln Medical School (LMS) at the same time. LMS is a geographically separate and new medical school but with curricula mapped to the NMS. At the time of EPC implementation, LMS did not experience placement capacity issues as NMS did. Therefore, EPC was delivered at LMS using the TT-M, allowing for comparative evaluation between TT-M and FT-M across two medical schools. The same feedback survey was used at both sites, apart from the first two questions being amalgamated into one at LMS (‘The course has helped me develop my consultation skills and clinical knowledge’). Surveys were disseminated in person for the TT-M and online for the FT-M, after each block of education.
Cost of education provision
The costs of delivering each education model considered how centralised health education funding, provided to English medical schools for student placement activities, were used to meet placement-based learning outcomes. These were calculated using local tariffs for the days students were placed in GP practices (£140 per student-day) compared to remuneration for clinical teaching staff which were £400 per day for GP educators and £95 per half-day for actors. Volunteer patients were not remunerated.
All face-to-face facilitated teaching was delivered in medical schools, thus not attracting room hire costs. The costs of developing and/or administering EPC were not calculated and assumed an academic operating cost funded by Higher Education Institutes. Therefore, the economic evaluation only includes costs of delivering the EPC courses.
Analyses
Survey response rates were calculated and summarised as numbers and percentages. Likert questions were summarised using means and standard deviations (SDs). Differences in response at Nottingham (FT-M) and Lincoln (TT-M) were compared using t-tests. The data were analysed using Stata SE v16. Free-text open questions were transcribed verbatim and thematically analysed [Citation21] for both education models.
Total costs of delivering EPC were calculated for both models. As the number of students and education methods were different, the costs of delivering education were standardised by calculating cost per teaching session (half-day) per 100 students, enabling meaningful comparisons.
Results
EPC delivery
Details of the resources used to deliver both courses are provided in . The FT-M and TT-M courses were delivered to 300 and 76 students, respectively. The FT-M utilised nearly double the taught activities than the TT-M model (83 per 100 students versus 44.7 per 100 students, respectively). Delivery of face-to-face education across both courses was similar (47 per 100 students versus 44.7 per 100 students for FT-M and TT-M, respectively). The FT-M supplemented education with 36 online taught activities per 100 students, whereas the TT-M used no online learning.
Table 2. Likert question feedback results for both teaching models.
Effectiveness of EPC
Feedback surveys were completed by 46/76 (61%) of students receiving the TT-M and 55/300 (18%) receiving the FT-M. Of these, 54/55 and 44/46 students gave free-text comments from the FT-M and TT-M, respectively.
Quantitative data for EPC evaluation are summarised in . The mean scores for student perceived attained learning outcomes were high (better experience) and similar irrespective of delivery method. Students for both courses felt that EPC developed their consultation skills, clinical knowledge and preparation for the clinical phases (mean scores for FT-M and TT-M: developing consultation skills and clinical knowledge (amalgamated) 4.36 versus 4.63; p = 0.05; preparation for clinical phases 4.35 versus 4.41; p = 0.68). Students reported similar enjoyment across both models (mean score 4.31 (FT-M) versus 4.41 (TT-M); p = 0.49).
Free-text comments triangulated with quantitative analyses, suggesting high-quality student experience for both delivery models (, ). For the ‘most useful and enjoyable aspects’ of EPC, three common themes emerged: clinical experience, style and setting of teaching, and GP educators. For aspects that could be ‘changed or improved’ two common themes emerged about the education provision: teaching delivery and placement experience.
Figure 2. Themes arising from free-text comments from student feedback for both models of teaching delivery.
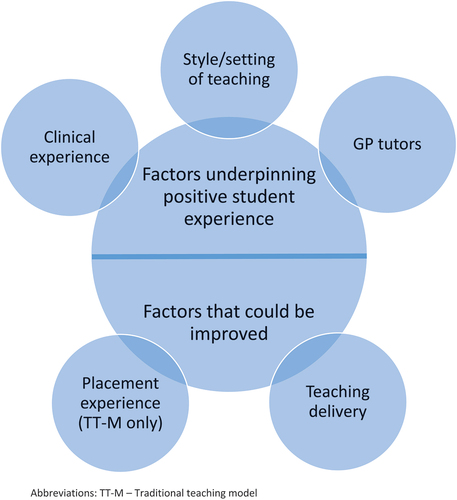
Table 3. Themes and free-text comments about student experiences.
Economic evaluation
The overall costs () of delivering the EPC course were £41,355 and £48,520 for the FT-M and TT-M, respectively. The costs for delivering EPC per session for 100 students were £1,379 and £5,551 for FT-M and TT-M, respectively.
Discussion
Exclusively, GP-facilitated clinical teaching outside of practices was successful for attaining student learning outcomes during a short, one-week primary care clinical attachment. Furthermore, an exclusive FT-M was as effective and more cost-effective than TT-M, where students spent time mostly within GP practices.
Strengths and limitations
To our knowledge, this is the first study directly comparing the effectiveness and cost-effectiveness of a course delivered exclusively using FT-M to a TT-M, for clinical training in primary care. A strength was the direct comparison of courses across two geographically separate medical schools, improving the validity of the findings. Triangulation of quantitative and qualitative data strengthens these findings. However, the lower response rate for FT-M students limits the generalisability of findings from this method of training. The difference in response rates observed likely relates to differing methods of data collection, with TT-M students being invited to complete feedback at the end of their final taught session, but FT-M students being emailed a survey at the end of their final day on the course. While we acknowledge that this is a limitation in itself, we feel this is a more likely explanation for the differing response rates, rather than it indicating a more positive experience in the TT-M group, although this cannot be excluded.
Perceived student experience was the outcome measure for effectiveness, and the study could have been strengthened by using objective measures of attainment. The cross-sectional design, however, did not allow for prospective associations with objective outcomes to be determined. Because of the very limited previous clinical exposure of these students, whilst the FT-M exposed students to a variety of learning, it is likely that the TT-M would encompass a greater richness of learning from exposure to entirely undifferentiated clinical care and other aspects of the ‘hidden curriculum’ experienced through everyday interactions with clinicians and patients. FT-M students’ appreciation of the benefits of this at their respective stages of training may have been lacking, and therefore not factored in to their subjective reporting of meeting the learning outcomes. For similar reasons, whether students would prefer an alternative delivery to the one they experienced was not explored as it was felt to be less relevant to the stage of learning, where students may not have had sufficient exposure to decide preferences. Future work that evaluates the delivery groups against objective measures of student attainment is warranted. Finally, there remains potential for residual confounding, given unadjusted analyses were undertaken.
Findings in broader context
Multiple reports describe how clinical teaching has been adapted in response to COVID with transition to online learning being a frequently adopted approach [Citation8,Citation10–12,Citation22–27]. Most studies, however, were in non-primary care settings. Studies have reported methods of supporting clinical learning, such as virtual ward rounds, to allow students to directly observe clinical encounters [Citation25]. Others included supervised telephone or video calls with facilitated feedback [Citation24,Citation26,Citation27]. This study utilised a range of approaches to support learning and may explain why students receiving the FT-M rated high levels of enjoyment.
Whilst studies have evaluated the effectiveness of specific components of online primary care education [Citation11], there is a lack of comparative evidence evaluating full courses to traditional practice-based placements [Citation12].
Simulation-based education has been shown to be effective in clinical training [Citation20,Citation28], with added benefits of equity in experience across large cohorts of learners, and is consistent with our findings. Furthermore, simulation allows for skills development without compromising patient safety, thus adding value to FT-M delivery [Citation19].
Student perspectives suggest that placement time matters, but key to them is patient interaction supporting the development of interpersonal skills and understanding of patient-centred care [Citation9]. Our FT-M included plentiful opportunity for patient interactions, thus creating positive learning experiences, to some degree similar to those within live-clinical environments. However, we acknowledge that planned patient interactions, involving actors or experienced patient educators, are not a complete substitute for the complexity and spontaneity of real patient encounters. Additional benefits included standardisation of experiences to ensure attainment of learning outcomes. Given all of the above, delivering primary care education using this type of model of exclusively facilitated teaching outside the clinical environment should be seen as a potential adjunct to support clinical learning, rather than a complete replacement for it.
A recent systematic review found role-modelling by GP-educators to be one of the most influential factors for students choosing to pursue careers within GP [Citation29]. As the FT-M used high contact time with GP-educators, it is plausible that the benefits of role modelling from traditional practice-based placements were retained. This study reported FT-M of learning to be cost-effective. This was driven by the economy of learning in groups, as opposed to TT-M of clinical training in GP practices, which often entails 1:1 supervision.
Conclusion
Delivery of a one-week primary care clinical attachment to third-year medical students using an exclusive FT-M was as effective and more cost-effective than TT-M of clinical learning. An exclusive FT-M of training undergraduates may be an important adjunct to support clinical learning whilst offering resilience to capacity challenges for hosting learners within primary care. Prospective studies investigating different methods of clinical training with summative outcomes and those identifying the optimal volume of the FT-M within curricula are warranted.
Ethical approval
This report presents the findings of an evaluation of education with only anonymous responses. It did not collate personal and/or identifiable data of participants. Therefore, formal ethical approval was not required.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- British Medical Association. Pressures in general practice data analysis. London: British Medical Association; 2022 [cited 2023 5th January]. Available from: https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/pressures/pressures-in-general-practice-data-analysis
- Health Education England. Everything you need to know about choosing GP Training. 2022 [cited 2023 17th February]. Available from: https://medical.hee.nhs.uk/medical-training-recruitment/medical-specialty-training/general-practice-gp/choose-gp/gp-training-key-facts#i%E2%80%99ve0
- Health Education England. Record number of 4,000 GPs accepted on training placements. 2021 [cited 2023 17th February]. Available from: https://www.hee.nhs.uk/news-blogs-events/news/record-number-4000-gps-accepted-training-placements
- Hunt L, Chalmers D, ProQuest. University teaching in focus [electronic resource] : a learning-centred approach/edited by Lynne Hunt and Denise Chalmers. Victoria, Australia: ACER Press; 2013.
- Moon J. The module and programme development handbook : a practical guide to linking levels, outcomes and assessment criteria. London, United Kingdom: Taylor & Francis Group; 2002.
- Page A, Potter K, Clifford R, et al. Prescribing for Australians living with dementia: study protocol using the Delphi technique. BMJ Open. 2015;5(8):e008048. DOI:10.1136/bmjopen-2015-008048
- Biggs J, Tang C. Teaching for Quality Learning at University. 3rd edition ed. Maidenhead, United Kingdom: Open University Press/McGraw-Hill Education; 2007.
- Dow N, Wass V, Macleod D, et al. ‘GP Live’- recorded General Practice consultations as a learning tool for junior medical students faced with the COVID-19 pandemic restrictions. Educ Primary Care. 2020 11 01;31(6):377–381.
- Lazzereschi L, Kirtley D. Provision of e-learning programmes to replace undergraduate medical students’ clinical general practice attachments during COVID-19 stand-down: a student perspective. Educ Primary Care. 2021 01 02;32(1):63.
- Moszkowicz D, Duboc H, Dubertret C, et al. Daily medical education for confined students during coronavirus disease 2019 pandemic: a simple videoconference solution. Clin Anat. 2020;33(6):927–928. DOI:10.1002/ca.23601
- Patel B, Taggar JS. Virtual teaching of undergraduate primary care small groups during Covid-19. Education for primary care: an official publication of the association of course organisers, national association of GP tutors, world organisation of family doctors. 2021 Sep;32(5):296–302. PubMed PMID: 34182891; eng. DOI:10.1080/14739879.2021.1920475
- Roskvist R, Eggleton K, Goodyear-Smith F. Provision of e-learning programmes to replace undergraduate medical students’ clinical general practice attachments during COVID-19 stand-down. Educ Primary Care. 2020 07 03;31(4):247–254.
- Taggar J, Saha R, Hopwood-Carr P, et al. Clinical placements in General Practice: concepts and considerations of implementing remote virtual placements in the COVID world. Educ Primary Care. 2021 07 04;32(4):237–244.
- McCutcheon K, Lohan M, Traynor M, et al. A systematic review evaluating the impact of online or blended learning vs. face-to-face learning of clinical skills in undergraduate nurse education. J Adv Nurs. 2015 Feb;71(2):255–270. PubMed PMID: 25134985; eng. DOI:10.1111/jan.12509
- Wilcha R-J. Effectiveness of virtual medical teaching during the COVID-19 crisis: systematic review. JMIR Med Educ. 2020 11 18;6(2):e20963. DOI:10.2196/20963.
- Chen F, Lui AM, Martinelli SM. A systematic review of the effectiveness of flipped classrooms in medical education. Med Educ. 2017;51(6):585–597.
- Hew KF, Lo CK. Flipped classroom improves student learning in health professions education: a meta-analysis. BMC Med Educ. 2018 03 15;18(1):38.
- Ruiz JG, Mintzer MJ, Leipzig RM. The impact of E-learning in medical education. Acad Med. 2006 Mar;81(3):207–212. PubMed PMID: 16501260; eng. DOI:10.1097/00001888-200603000-00002
- Khan K, Pattison T, Sherwood M. Simulation in medical education. Med Teach. 2011 01 01;33(1):1–3.
- Kim J, Park JH, Shin S. Effectiveness of simulation-based nursing education depending on fidelity: a meta-analysis. BMC Med Educ. 2016 May 23;16(1):152. PubMed PMID: 27215280; PubMed Central PMCID: PMCPMC4877810. eng. DOI:10.1186/s12909-016-0672-7
- Green J, Thorogood N. Qualitative methods for health research. 4th ed. London: SAGE Publications; 2018.
- Gordon M, Patricio M, Horne L, et al. Developments in medical education in response to the COVID-19 pandemic: a rapid BEME systematic review: bEME guide no. 63. Med Teach. 2020 11 01;42(11):1202–1215.
- Calhoun KE, Yale LA, Whipple ME, et al. The impact of COVID-19 on medical student surgical education: implementing extreme pandemic response measures in a widely distributed surgical clerkship experience. Am J Surg. 2020 Jul;220(1):44–47. PubMed PMID: 32389331 PubMed PMID: 32389331. DOI:10.1016/j.amjsurg.2020.04.024
- Chick RC, Clifton GT, Peace KM, et al. Using Technology to maintain the education of residents during the COVID-19 pandemic. J Surg Educ. 2020 Jul-Aug;77(4):729–732. PubMed PMID: 32253133; PubMed Central PMCID: PMCPMC7270491. eng. DOI:10.1016/j.jsurg.2020.03.018
- Hofmann H, Harding C, Youm J, et al. Virtual bedside teaching rounds with patients with COVID-19. Med Educ. 2020 Oct;54(10):959–960. PubMed PMID: 32403185; PubMed Central PMCID: PMCPMC7273015. eng. DOI:10.1111/medu.14223
- Johnston A, Barrick K, Jivraj F, et al. ‘The virtual check-in’: a tool to facilitate virtual patient interaction for early clinical learners in a longitudinal integrated clerkship. MedEdpublish. 2020;9(108):108. DOI:10.15694/mep.2020.000108.1
- Oldenburg R, Marsch A. Optimizing teledermatology visits for dermatology resident education during the COVID-19 pandemic. J Am Acad Dermatol. 2020 Jun;82(6):e229. PubMed PMID: 32283238; PubMed Central PMCID: PMCPMC7146655. eng. DOI:10.1016/j.jaad.2020.03.097
- Bray L, Krogh TB, Østergaard D. Simulation-based training for continuing professional development within a primary care context: a systematic review. Educ Primary Care. 2023;34(2):1–10.
- Lamb E, Burford B, Alberti H. The impact of role modelling on the future general practitioner workforce: a systematic review. Educ Primary Care. 2022;33(5):1–15.
