 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
The current study was conducted on a sample of 91 patients diagnosed with diastolic dysfunction (DD) with preserved systolic function caused by a painful chronic ischaemic cardiopathy – angina pectoris stable at the effort. The diagnosis was established following anamnesis, electrocardiogram, and echocardiography. Myeloperoxidase (MPO) serum levels were assessed in all patients and then these values were correlated with some of the echocardiography parameters that proved the mentioned diagnosis.
In conclusion, the execution of this investigation triad (electrocardiogram, echocardiography, and MPO) allows:
Stratifying the patients depending on the disease risk by early detecting of any possible DD with preserved systolic function.
The use of the MPO increased circulating levels as a biomarker for diagnosis and risk due to the statistically significant correlation between those and the results of the other two aforementioned paraclinical investigation.
Introduction
The myocardial contractile function is affected at a relatively early point during the evolution of cardiac diseases, on account of which the latest European medical regulations for heart failure considers as necessary, even in the subclinical stage, to assess the efficiency of not only the systolic but also the diastolic functionCitation1,Citation2.
Regardless of whether the systolic debit is preserved or not, early detection of risk factors is useful for effective prevention strategies in avoiding premature cardiac insufficiency (CI) and in providing adequate treatment, including aetiological therapy. Clinical studies on CI reveal that myocardial performance depends on the left ventricle (LV) diastolic function, which is primordially dependent on the relaxation ability of the heart muscleCitation3,Citation4. In regard to this last process, it is known that the lusitropic status is determined by both biochemical and biomechanical (active relaxation) influences, as well as by biophysical properties of the heart (passive rigidity)Citation4–6.
Since 1991, the medical practice has recognised a new clinical form of heart failure, diastolic dysfunction (DD)Citation7. DD is defined as a clinical syndrome connected pathogenically to anomalous ventricular filling and relaxation, especially affecting the LV, which manifests initially with preserved systolic function (PRESYF). The defining characteristic of the disease is the preservation of the systolic debit (>45% than normal), whereas there are alterations in the diastolic functionCitation8.
According to the incidence rates, the main pathogenic mechanism responsible for the onset of CI with normal LV ejection fraction is myocardial ischaemia that slows down the heart muscle relaxation, reduces the diastolic distension, and remodels the heart concentrically increasing the width/radius ratio. Under hypoxia/ischaemia conditions, the LV distension problems arise as an expression of healthy arias and ischaemic, even fibrous lesions coexisting in the heart muscle, which alter the relaxation process and generate a delay and inhomogeneity of relaxation – increasing the phenomena, especially during effortCitation9,Citation10.
Cellular oxidative stress is defined as the biological state characterised by an excess concentration of oxidative agents (reactive oxygen species (ROS) and reactive nitrogen species (RNS)), which results as a consequence of either intensified synthesis or decreased antioxidant systems activityCitation9,Citation11–13.
In medical practice the pathogenesis induced by oxidative stress on the organic level is functionally evaluated to quantify the participation share, without regard of its primary source:
Local production of oxidant agents by implicating the cell structures of the particular organ or/and the cells migrated or infiltrated at that level.
Systemic synthesis in other tissues and organsCitation10,Citation13,Citation14.
In the case of ischaemic cardiomyopathy induced by coronary atherosclerosis in the first category, that of the local sources producing oxidant agents, there are the myocardial fibres, myocytes, endothelial cells from the regional vessels, whereas in the other class, the one of the migrated cells or the figurate elements implicated in inflammatory processes are placed neutrophils and especially monocytes turned into macrophagesCitation9–11,Citation15,Citation16. The monocyte activation process includes the following three steps:
Mobilisation of resident/responsive monocytes, from the central axis of laminar blood, flow into passing in the interstitial space by diapedesis.
Initiating the stimulating process on the monocytes, which results in their partial activation.
Complete activation of monocytes, which allows them to metamorphose into macrophagesCitation9,Citation11,Citation13,Citation16.
Through the production of chemoattractant factors, the activated monocytes have implications in the myocardial oxidative stress evolution, ensuring the persistence and expand of inflammation that generates other chemoattractant factors on its own. The structural–functional destructive processes in the ischaemic heart muscle are mediated by at least 24 such factors among which are tumour necrosis factor (TNF), interleukin-1 (IL-1), and stimulating factors such as granulocyte-monocyte colony-stimulating factor (GM-CSF), granulocyte colony-stimulating factor (G-CSF), and monocyte colony-stimulating factor (M-CSF)Citation9,Citation11,Citation13.
Although the consulted medical literature recognises unanimously the myeloperoxidase (MPO) serum levels as a biomarker for oxidative stress and endothelial dysfunction in CI, there are limited studies available on the possible significance of MPO as an indicator of inflammation and heart muscle remodelling processesCitation15. Histochemically, the myocytes that are subject to ischaemia undergo lysis due to both autophagy (catalysed by the enzymes released by the myocardial fibre itself) and necrosis, produced by the mononuclear phagocytic system cellsCitation11,Citation13,Citation16. Although the last one is triggered as a local reconstructive process, it represents a destructive mechanism with implications in further inflammation development and fibrotic matrix proliferation. As MPO is a lysosomal monocyte-macrophage enzyme, it catalyses the reaction between hydrogen peroxide and chloride ion, leading to hypochlorite (ClO–), which turns into hypochlorous acid (HClO) and gains lytic properties over the cellsCitation10,Citation14.
Materials and methods
On the basis of the overall acceptance of serum MPO among the markers used in endothelial dysfunction management, the present study is aiming to investigate the possible signification of serum MPO as a biomarker for CI with DD and preserved ejection fraction ().
Table 1. Cardiac insufficiency (CI) biomarkers classification after the pathophysiological mechanism they are involved inCitation15.
The research sample consisted of 91 patients with a positive diagnosis of DD with preserved ejection fraction (PRESYF), having a unique aetiology caused by the only one aetiological factor, namely chronic ischaemic painful cardiopathy (CICD).
The preservation of the systolic debit was an important condition imposed on the participants in the study to limit the sources of oxidant agents production, only to those on the myocardial level, in the case of mal-irrigation. Because of the fact that it is demonstrated and universally acknowledged that in chronic CI with reduction of the systolic flow there occurs a decrease in the organ debit, in these conditions all structures of the organism are forced to function under state of hypoxia. From pathogenic point of view, the consequence is the appearance of new sources of ROS and NOS production – a possibility that has been avoided through the selection of patients with ischaemic cardiopathy, but conserved systolic debitCitation13.
For each one of the 91 patients (35 women and 56 men) in the study sample, the aetiological diagnosis of the myocardial contraction deficiency (ischaemic cardiopathy) is justified by the presence of stable angina pectoris at effort, reported during anamnesis, and the paraclinical exploration results. To evaluate the functional condition of the ventricular myocardium during diastole all participants underwent:
Resting state electrocardiogram and supplementary effort test if the first could not demonstrate any ischaemic modifications.
Echocardiography – bi-dimensional evaluation, M-mode, pulsed Doppler (PW), and tissue pulsed Doppler (TDI). Referring to the clinical utility of echocardiography, the specialized literature considers this to be the best non-invasive method for assessing DD and LV filling pressure. The M-mode used in the current study was limited because the DD is suggested indirectly. In comparison, the other echocardiographic techniques such as the transmitral blood flow Doppler and the tissue Doppler are more sensitive and more specific, which allows them to prove and stage the DDCitation1. The practical contribution of the Doppler tests enables a positive diagnosis to be still made at the latent phase of evolution when the DD does not have clinical manifestationsCitation6. The determined echocardiography parameters are shown in .
Table 2. Main analysed echocardiography parameters and the standard values.
Formula Devereux R.B. used to calculate the mass of LVCitation6:
In order to include in the research sample only those patients with chronic ischaemic cardiopathy and preserved left ventricular ejection fraction (LVEF) (≥50%) (PRESYF), it was necessary to evaluate the global systolic function of LV. For this purpose the Simpson modified method was applied, with the use of the following formula:
On the next stage of positive diagnosis establishment, for the selection of the required study sample, in the conditions of confirmed normal ejection fraction values and absence of any associated diseases, excluding of course the ischaemic cardiopathy, the LV diastolic function was assessed, practically the existence of DD. The DD diagnosis was made on the base of the following 3 obligatory criteria given by the European Study Group on Diastolic Heart Failure:
Signs and symptoms of CI:
• Symptoms: dyspnoea and/or arterial hypertension during effort states.
• Signs: gallop rhythm, respiratory sounds – pulmonary crepitation and even acute pulmonary oedema.
Normal or slightly affected systolic function.
Abnormalities in diastolic relaxation, filling, distensibility, or stiffnessCitation17,Citation18.
The successive executions of the aforementioned phases enabled the selection of sample patients with a positive diagnosis of DD with PRESYF, with the unique aetiology of chronic ischaemic painful cardiopathy (stable angina pectoris of effort).
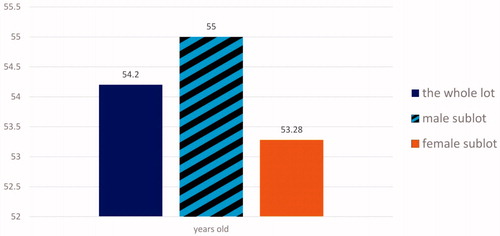
An essential criterion imposed for including patients in the study sample was their age. It was necessary because the medical literature unanimously acknowledges the interdependence between CI by DD and age, acquiring variable rates of this positive age-correlation (in general 55–65%). The research did not cover people older than 60 years, hence, the average age of the sample was 54.2 years old with subsamples according to .
Figure 1. Average age of the patients from the research sample; comparison between the subsamples depending on sex.
The lack of voluntary participation of patients older than 60 years is based on the scientific demonstrated argument that although elderly people experience precocious alterations in the ventricular passive filling, the global filling is conserved due to the arterial systole contribution. It is universally accepted that after the age of 60, the participation share of the atrial systole in the ventricular diastolic filling reaches 30% of the cardiac debitCitation2,Citation3. In addition, the elderly suffer modification in the values of some of the analysed echographical parameters, such as the E/A ratio or the E′ velocityCitation6.
The body mass index (BMI) of the patients accepted in the current research presented variations within the margins of 26 ± 3 kg/m2, which corresponds to a body mass value considered normal or with 10% ponderal excess and associated with a minimum riskCitation3. The introduction of this criterion was obligatory to avoid the possibility to influence some of the analysed echographic parameters.
In addition, for the purpose of the study, there were not accepted patients with arterial hypertension or with tachycardia/tachyarrhythmia, because these diseases, as well as the age, are predictors for some of the examined echocardiographic parameters – E/A ratio and TDECitation19.
Results
The patients from the study sample underwent laboratory tests on venous blood, the outcome of which is shown in , among the sample distribution of the determined values.
Table 3. Serum tests results of the patients analysed in the present research.
Whereas the main study objective was the MPO serum levels research, it was obligatory to include its determination among the conducted laboratory investigations. The reasoning of its establishment was that increased serum concentrations of this enzyme in patients with DD are an indicator for the existence of an inflammatory process that develops not only on the coronary level but also on myocardial one in the hypoxic/ ischaemic state.
The analysis approach applied for quantifying MPO was the immunoenzymatic fluorescence method (FEIA) that uses as an antigen purified MPO enzyme acquired from human neutrophils. The method allows the anti-MPO antibodies detection, which according to the specialised literature data are implicated particularly in the vascular inflammatory pathogenesis, because of their role as co-participants responsible for the set of vascular dysfunction by atherosclerosis.
The data from the analysed parameters that will be further referred to in Discussion section were evaluated using t-Student’s test, with statistical signification being affirmed for values of p < .05.
Discussion
From the symptomatological point of view, the diagnosis of DD among the patients in the research sample was based on the following ():
Table 4. Symptoms incidence and defining signs of DD in the study sample.
For the patients with chronic ischaemic cardiopathy but with no evident symptomatology (asymptomatological patients), the DD diagnosis was established based on the data from the echo-Doppler test.
To establish the diagnosis of DD according to the three recommendations of the European Study Group on Diastolic Heart Failure and to highlight abnormalities in relaxation, filling, distensibility, or stiffness of the LV the values of the echographical parameters from the list below were interpreted:
LA volume index
LV mass index
Relative thickness SIV, respectively, PPVS
E-wave speed
Transmitral flux, calculated by the E/A ratio
E-wave deceleration time
TDE
E/E′ ratio between the E-wave and E′-wave speedCitation5,Citation20.
With the use of “symptoms and signs of CI” criteria recommended by The European Study Group on Diastolic Heart Failure, the patients from the study sample were sorted in different classes of inotropic deficiency, after the classification of NYHA ().
Table 5. NYHA classification of cardiac insufficiencyCitation10.
The basic criterion of the NYHA classification is the symptomatology, which made it quite difficult to sort the participants in the research sample in the respective classes of the myocardial contractile deficit, considering that patients with DD and preserved systolic function present imprecise symptomatology – a particular aspect that is referred to in the specialised literature. In the same respect, it can be mentioned the existence of patients in the study that lacked symptoms of CI.
In accordance with the NYHA classification aspects, the classes of the myocardial contractile deficit were as shown in Citation1,Citation21,Citation22.
Table 6. Incidence of myocardial contractile deficit cases in the study, based on NYHA classification criteria.
As evaluating the signification of MPO serum values is the main objective of the study, it was necessary to establish the blood level of this enzyme. Serum concentrations above the negative result of 7 U/mL were detected in 67 patients (73.1%). The amount of cases is 2.7 times higher than the negative result, which corresponds to a positive correlation in 2 from 3 situations ().
Even if the number of cases in the current study is considered relatively small, the results in determining MPO serum levels represent a strong argument to support the fact that MPO can be used as a biomarker for diagnosis and risk estimation of DD, occurring as chronic ischaemic cardiopathy with conserved systolic debit volume.
To endorse the previous suggestion there is also the protocol recommended by Cleveland Heart Lab to use the multi-biomarker CVD Inflammatory profile test with the purpose of DD diagnosis. The latter includes two of the serum parameters measured in the present study, namely (MPO and hs-CRP), but also 4 additional ones: oxidised lipoproteins, A2 phospholipase (lp-PLA2), F2-isoprotan, and microalbuminuriaCitation23.
In comparison with the standard values the following echographic parameters showed pathological deviations in the patients of the research sample:
E-wave deceleration time, TDE, increased in 83 cases = 91.1%.
Relative thickness SIV and PPVS, respectively, in 35 cases = 71.4%.
LV mass – increased in 56 cases = 61.5%.
LV index mass – increased in 59 cases = 64.8%.
E/A ratio – abnormal in 78 cases = 85.7%.
The next stage of the study consisted of identifying possible correlations between MPO serum concentration and the determined values of some of these echocardiography parameters. Therefore, the serum MPO was compared with TDE, LV mass index, and E/A ratio. Therefore, the direction of level variation of the circulating MPO serum concentration variations was compared with that of the following echographic parameters’ variations: TDE, LV mass index, and E/A ratio.
Referring to DD, the medical literature reports that the first echographic parameter to become abnormal by increasing its value is TDE. Incidence of values above 240 ms reaches 91.1% in the study sample, occupying the first place among the selected echographical parameters. The correlation between the TDE values and the MPO serum concentration showed a ratio of 83 cases/67 cases = 91.15/73.1%.
The concordance in the proportion of ¾ of the analysed cases between these two parameters allows elaborating the following statements:
Patients with DD and PRESYF MPO serum concentration above 7 U/mL is significantly correlated statistically with relaxation and even ventricular compliance modifications in the advanced stages of the disease. The thoroughgoing study based on the results from the present research, by conducting investigations on numerically significant samples of patients, possess high chances of proving and accepting the utility of serum MPO as a biomarker for DD with PRESYF.
The fact that in 16 cases were reported prolonged TDE values while presenting normal MPO serum concentration (<7 U/mL), can be interpreted as caused by:
the increased sensibility of the TDE parameter in identifying the existence of delayed relaxation in comparison with the circulating MPO levels that raise at a later phase during the disease evolution.
The large accordance rate between these two parameters can also be used as an argument for supporting their association, as a complex biomarker, the information rendered by the two in medical practice being useful for the fact that they support each other, at the same time completing each other.
In medical practice, the elevated SIV, PPVS, LV mass, and LV mass index values are considered an illustration of concentric cavity remodelling, but at the same time also an indication for myocardial hypertrophy, as a functional expression of modifications in the LV myocardial complianceCitation10,Citation24,Citation25.
In the current research, the increased incidence of LV mass index (59 cases = 64.8%) was corroborated with that of LV walls relative thickness (SIV + PPVS) reported in 65 cases (71.4%), which had moderately higher values than those accepted as normal. Without taking into account the patients’ sex, the echographic existence of modifications in the aforementioned variables indicates that in at least 2/3 of the DD cases with PRESYF the ventricular concentric hypertrophy was present.
In all 59 cases with increased LV mass index, there was also detected an increase in the serum MPO concentration ≥7 U/mL.
The 100% accordance between the two parameters makes it possible to consider that the circulating MPO level can be recognised as an indicator for the onset of LV myocardial hypertrophy developing process and therefore can be accepted as a marker for DD.
Conclusions
Despite DD being a relatively light medical condition, it possesses a prognostic importance, proving the existence of certain cardiovascular risk, with the possibility of installing a clinical syndrome of CI. Therefore, the interest in developing new laboratory and paraclinical non-invasive examinations for the detection of DD as early as possible is completely justified.
The current study shares this aim and the obtained results allow the statement that MPO serum level, independently or in correlation with the echographic data, can become a useful investigation for the medical practice as a biomarker of DD with PRESYF.
During the clinical track of DD with PRESYF evolution, between the two respective parameters, the informational value of the enzymatic serum concentration has a relatively delayed sensibility, whereas there are echographically evident signs of delayed or incomplete relaxation. Consequently, if it is not possible to perform the echocardiography, MPO serum concentration dosage is useful in diagnosing and evaluating the risk for DD with PRESYF.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Anton F. Characteristic features of heart failure with preserved left ventricle systolic function. Clujul Medical 2012;85:302–9. [In Romanian].
- Rude MK, Duhaney TA, Kuster GM, et al. Aldosterone stimulates matrix metalloproteinases and reactive oxygen species in adult rat ventricular cardiomyocytes. Hypertension 2005;46:555–61.
- Manole G. Clinical physiology. Vol. 2. Bucharest (Romania): National Company Printers, Coresi S.A. Publishing; 2007. [In Romanian].
- Villars PS, Hamlin SK, Shaw AD, Kanusky JT. Role of diastole in left ventricular function, I: biochemical and biomechanical events. Am J Crit Care 2004;13:394–403.
- Nanea TI, Gheorghe SG, IlieÈiu MA, et al. Noninvasive evaluation of myocardial viability in ischemic cardiopathy – 2nd Part. Ro J Med Pract 2010;2:133–7.
- Radu R, Stătescu C, Arsenescu-Georgescu C. Left ventricular diastolic function in patients with uncomplicated arterial hypertension. Med Interna 2011;3:342–51. [In Romanian].
- Grossman W. Diastolic dysfunction in congestive heart failure. N Engl J Med 1991; 325:1557–64.
- Hamlin KSh, Kanusky TJ, Penelope ZS, Shaw DA. Role of diastole in left ventricular function, II: diagnosis and treatment. Am J Crit Care 2004;13:453–68.
- Dincă VG, Manole G, Cochior D, Dincă AL. Paraoxonase (PON1) possible biomarker for risk of heart failure. Rev De Chimie 2016;67:854–7.
- Manole G. General clinical pathophysiology. Pathophysiology organs. Bucharest, Romania: National Company Printers, Coresi S.A. Publishing; 2003. [In Romanian].
- Dincă VG, Dincă AL, Căpitănescu C, Manole G. Cardiomyocyte membrane pathogenetic mechanisms and biochemical-induced endothelial-coronare in chronic ischemic heart disease. Int J Curr Res 2017;9:48435–9.
- Bălăeţ C, Coculescu BI, Manole G, et al. Gamma-glutamyltransferase, possible novel biomarker in colon diverticulosis: a case-control study. J Enzyme Inhib Med Chem 2018;33:428–32.
- Dincă VG, Manole G, Cochior D, Dincă AL. Considerations regarding the biomarker value of circulant concentration of PON1 in patients with heart failure through chronic ischemic cardiomyopathy. JEPE BENA 2016;17:407–13.
- Bălăeţ C, Coculescu BI, Bălăeţ M, et al. Haemolytic anaemia and hepatocitolysis associated with hypermagnesaemia by repeated exposures to copper calcium fungicides. J Enzyme Inhib Med Chem 2018;33:184–9.
- Braunwald E. Biomarkers in heart failure. N Engl J Med 2008;358:2148–59.
- Duchen MR. Mitochondria and calcium: from cell signalling to cell death. J Physiol 2000;529:57–68.
- How to diagnose diastolic heart failure. European Study Group on Diastolic Heart Failure. Eur Heart J 1998;19:990–1003.
- Macin SM, Perna ER, Cimbaro Canella JP, et al. Differences in clinical profile and outcome in patients with decompensated heart failure and systolic dysfunction or preserved systolic function. Rev Esp Cardiol 2004;57:45–52.
- Muller-Brunotte R, Kahan T, Malmqvist K, Edner M. Blood pressure and left ventricular geometric pattern determine diastolic function in hypertensive myocardial hypertrophy. J Hum Hypertens 2003;17:841–9.
- Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2016;17:1321–60.
- Redfield MM. Heart failure with normal ejection fraction. In: Libby PP, Bonow RO, Mann DL, Zipes DP, eds. Braunwald’s heart disease: a textbook of cardiovascular disease medicine. 8th ed. Philadelphia: Saunders; 2007:641–64.
- Varela-Roman A, Gonzales-Juanatey JR, Basante P, et al. Clinical characteristics and prognosis of hospitalised in patients with heart failure and preserved or reduced left ventricular ejection fraction. Heart 2002;88:249–54.
- Hughes S, Wood S. A multibiomarker test for predicting CVD: Has its time arrived? 2012. Available from: https://www.medscape.com/viewarticle/791243 [last accessed 10 Jan 2018].
- Evangelista A, Flachskampf F, Lancellotti P, et al. European Association of Echocardiography. European Association of Echocardiography recommendations for standardization of performance, digital storage and reporting of echocardiographic studies. Eur J Echocardiogr 2008;9:438–48.
- Sapojnic N. Left ventricular diastolic function and its role in myocardial performance. Arta Medica 2009;4:35–8.
