ABSTRACT
Introduction: Extending the benefits of vaccination against infectious diseases from childhood throughout the entire life-span is becoming an increasingly urgent priority in view of the world’s aging population, emergence and reemergence of infectious diseases, and the necessity to invest more on prevention versus cure in global healthcare.
Areas covered: This perspective discusses how life-course immunization could benefit human health at all stages of life. To achieve this, the current vaccination paradigm should be changed and all stakeholders have a role to play.
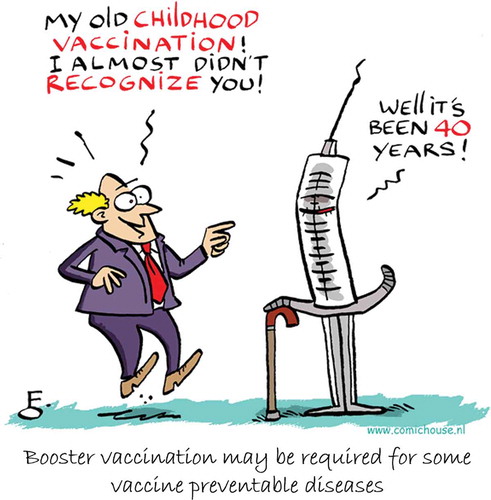
Expert commentary: To enhance immunization confidence in the population, it is essential that stakeholders eliminate complacency toward infectious diseases, improve vaccination convenience, remove barriers among different healthcare specialties, and address prevention as a single entity. They must also consider societal and cultural mindsets by understanding and including public viewpoints. A new “4Cs’ model encompassing convenience, confidence, complacency, and cultural acceptance is proposed to convert ‘vaccine availability’ to ‘vaccination acceptance’ throughout life. Life-course vaccination should become the new social norm of a healthy life-style, along with a healthy diet, adequate physical exercise, and not smoking. We are ‘all in’ to make life-course immunization a gateway for all people to lead longer, healthier lives.
1. Introduction
Due to a combination of factors, including increasing life-span and decreasing birth rates, the world’s population is aging [Citation1]. Disease prevention strategies are urgently needed to maintain the health and independence of this aging population. Vaccination is one of these strategies. It is considered one of the ten most effective public health achievements [Citation2] and vaccines are estimated to save 2–3 million lives each year worldwide [Citation3]. Public perception of vaccination is commonly associated with preventing diseases of infancy and childhood and, although pediatric vaccination remains crucial, it can no longer be the only focus of vaccination programs, since there remains a significant, unaddressed burden of these diseases in adults [Citation4]. Indeed, protection needs to be expanded to older age groups as new diseases are emerging (e.g. Zika virus) and old diseases are reemerging (e.g. measles and pertussis) in adults, and because of the growing necessity of healthcare systems to invest more in prevention rather than treatment if they are to remain effective in the face of an aging population.
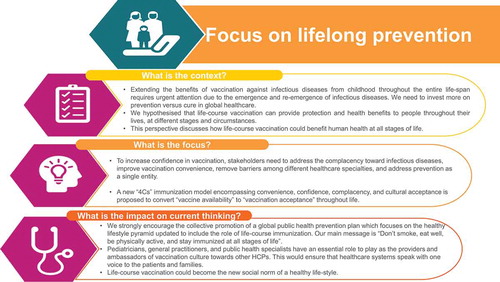
Life-course immunization is the concept of vaccination providing protection and health benefits to people throughout their lives, at different stages and circumstances. This need to extend the benefits of vaccination beyond childhood has captured the attention of physicians and policymakers as part of a global interest in disease prevention as a means of improving health and reducing healthcare costs. Whereas most vaccines have been developed primarily for children, vaccines against a wide range of pathogens are available for use in adolescents, pregnant women, adults, older adults, and travelers (). In addition to licensed vaccines, the vaccine industry is gaining momentum as new vaccines are being developed to address unmet needs against challenging pathogens and to prevent disease in specific populations, such as pregnant women and individuals with immunocompromising conditions or comorbidities.
Figure 1. Licensed vaccines support immunization for all age groups. BCG, Bacillus Calmette Guérin; HPV, human papillomavirus.
The purpose of this perspective is to discuss how life-course immunization can benefit human health throughout life and why all stakeholders have a role to play in changing the current paradigm. To reduce the growing burden on healthcare systems, vaccination needs to become part of the new social norm of a healthy lifestyle, as is screening of chronic diseases, healthy diet, physical exercise, and not smoking. To achieve this paradigm change, we need to remove the barriers to life-course vaccination among different healthcare specialties and listen to the public in order to understand and address their questions and concerns about vaccines.
2. Why is life-course immunization needed?
In addition to infants and children, healthy adolescents or adults may also need to receive vaccine booster doses or complete their vaccination schedule so that protection against infectious diseases can continue into adulthood. Such individuals may also need new vaccinations due to their occupation or travels. Specific populations such as older adults, pregnant women, and individuals with chronic or immunocompromising conditions require additional strategies to prevent or reduce the substantial morbidity and mortality caused by vaccine-preventable diseases [Citation5].
2.1. Older adults
Given that life expectancy is increasing worldwide, improving the health and quality of life of older adults has become an important issue. By 2030, almost 1 billion people will be over 65 years of age and, for the first time in history, this age group will outnumber children below the age of five [Citation1]. In 2002, the World Health Organization (WHO) developed a policy framework on ‘active aging’ to promote interventions that improve health throughout life [Citation6].
Many infectious diseases (e.g. seasonal influenza, pneumococcal disease, and herpes zoster) have their greatest incidence and/or severity in older adults [Citation7]. This is usually because comorbidities and immunosenescence (age-associated progressive dysregulation and dysfunction of the immune system) are more frequent in this population [Citation8]. Infectious diseases in older adults may also worsen existing comorbidities and accelerate the loss of functionality, increase frailty, and hasten death [Citation9,Citation10]. Furthermore, due to the success of childhood vaccination programs, the burden of some infectious diseases has greatly decreased in children, shifting the bulk of the disease burden to older age groups. As a result, in regions such as Europe with good vaccine coverage in children, tetanus and diphtheria are now primarily seen in unvaccinated older adults [Citation11].
Because infectious diseases are an important cause of morbidity and mortality in older adults, disease prevention through vaccination is an effective means of promoting healthy aging [Citation12]. Following the WHO, several health authorities have launched healthy aging programs that encourage older adults to remain healthy, active, and independent for as long as possible [Citation6,Citation9,Citation10,Citation13–Citation15]. Notably, in April 2017, the WHO’s annual European Immunization Week focused on the importance and benefits of immunization at every stage of life under the slogan ‘#VaccinesWork’ [Citation16]. As the WHO recognizes, this is a global problem – some low and middle-income countries are already facing similar questions over aging populations as high income countries but must deal with it under even more constrained circumstances. For these countries, effective vaccination – which is one of the most cost effective of all health interventions – is likely to play an even more important role. However, so far, most data on adult burden of vaccine-preventable diseases and on interventions to deal with it come from high-income countries. These observations will be the focus of the following discussion – but it should be remembered that a paradigm shift in attitudes is needed to get the most out of life-course vaccination.
The first moves in this direction can already be seen. In Italy, to contain disease resurgence and reverse the trend toward lower vaccination rates, a life-course immunization approach was implemented in the 2017–2019 national vaccination plan, with childhood, adolescent, adult, and older adult vaccinations all being prioritized [Citation17]. This was put in place after extensive internal discussion between different health specialties and public health bodies making Italy one of only a few countries to explicitly make life-course vaccination a priority [Citation18–Citation20]. While other countries (e.g. France, or Australia) have recently taken action to boost vaccination, by launching national consultations or mandating consequences for refusing vaccination, the primary focus has remained within pediatric vaccination programs [Citation21,Citation22].
Several vaccines are recommended for adults, depending on age, underlying medical conditions, vaccination history, treatments, occupation, or planned travels, but these recommendations differ between countries [Citation5,Citation23]. Although many countries consider a person to be elderly when they have reached 65 years of age, this view is often disputed because of improving life expectancy, quality of life, and level of occupation within an older population. There is considerable variation among countries in defining older adults, elderly, geriatrics, or frail elderly [Citation24,Citation25]. The WHO recommends annual vaccination with the seasonal inactivated influenza vaccine for persons aged ≥ 65 years [Citation26]. In the United States, the Advisory Committee on Immunization Practices recommends influenza, tetanus-diphtheria or tetanus-diphtheria-pertussis (Tdap), herpes zoster, and pneumococcal vaccines for this age group [Citation27,Citation28]. In Australia and the United Kingdom, influenza, herpes zoster, and pneumococcal vaccines are provided free to older adults [Citation29,Citation30]. All countries in the European Union and the European Economic Area recommend seasonal influenza vaccination to older age groups, with the age ranging from ≥ 50 to ≥ 65 years [Citation31].
In addition to increasing the susceptibility to infections, the gradual deterioration of the immune system brought on by natural age advancement, known as immunosenescence, can also reduce effectiveness of some vaccines [Citation8]. For instance, the efficacy of the live attenuated herpes zoster vaccine decreases with age. It is 70% in adults aged 50–59 years, 64% in adults aged 60–69 years, 41% in adults aged 70–79 years, and 18% in those aged ≥ 80 years [Citation32,Citation33]. Consequently, there is a need for specifically designed vaccines to overcome immunosenescence in older adults. In one such case, a new adjuvanted subunit vaccine has been developed specifically for older adults to prevent herpes zoster and its complications. Its efficacy in preventing herpes zoster does not appear to decrease with increasing age [Citation34,Citation35].
2.2. Pregnant women
The strategy of maternal immunization is a three-pronged approach to enhance protection of mothers, their unborn children, and young infants in their first months of life by increasing the concentrations of maternal antibodies that can pass through the placenta [Citation36,Citation37]. This approach is not new but has recently gained more attention from both the general population and healthcare professionals. The reasons for it include the success of reducing neonatal tetanus by vaccinating women during pregnancy, reducing pertussis cases in infants in the first few months after birth, and the positive effect of seasonal and pandemic influenza immunization for both mothers and children [Citation36].
In 2012, the WHO recommended that all pregnant women receive influenza vaccination regardless of the stage of pregnancy, and identified pregnant women as the highest priority group for countries considering to initiate or expand seasonal influenza vaccination programs [Citation26]. Currently, inactivated influenza, tetanus, and pertussis vaccines are recommended during pregnancy in several countries [Citation38]. A growing body of evidence suggests that maternal immunization has an acceptable safety profile, is well tolerated, and is effective in pregnant women and their infants [Citation36,Citation39]. New vaccines are also being developed for maternal immunization to prevent neonatal infectious diseases such as respiratory syncytial virus (RSV) and group B streptococcus (GBS), for which no vaccines are currently available [Citation36].
2.3. Adolescents, adults, and travelers
Adolescents require additional protection because of the natural peak in incidence of meningococcal disease, the risk of sexually transmitted HPV, and the need to extend protection against pertussis derived from childhood vaccinations [Citation40]. United Kingdom has one of the highest annual incidence rates of meningococcal disease in Europe, with more than a third of cases occurring in people ≥ 10 years of age [Citation41]. Overall, the case fatality rate of meningococcal B disease was 4.2% but it was more than twice as high in teenagers and adults than in infants [Citation41]. In many countries, meningococcal and human papillomavirus (HPV) vaccines and Tdap boosters are recommended for adolescents and, in some of them, also in adults [Citation42]. For travelers, pre-travel immunization with vaccines such as hepatitis A, yellow fever, typhoid fever, and quadrivalent meningitis ACYW135 vaccines may be recommended, or even required, depending on the destination and the activities planned.
2.4. Emerging and reemerging diseases
Whereas some vaccines induce life-long immunity, others do not, and require additional doses or regular boosters. Notable examples of the latter include tetanus, diphtheria, and pertussis vaccines [Citation43–Citation45]. Ideally, all individuals should receive priming doses of tetanus and diphtheria toxoid-containing vaccine in childhood, followed by regular boosters during adulthood to provide long-term protection. Influenza vaccination is recommended annually because the viruses in circulation frequently change and because protective immunity is of short duration [Citation46]. Measles outbreaks due to incomplete coverage for the first or the second vaccine dose are becoming more and more frequent in adolescents and young adults. These outbreaks have impacted the WHO’s objectives to reduce global measles mortality by 95% from the 2000 estimate and to eliminate measles in five out of six WHO regions before 2020 [Citation47]. Between 2000 and 2015, measles vaccines administered through routine immunization programs worldwide decreased estimated measles mortality by 84% and prevented an estimated 20.3 million deaths [Citation48]. Pertussis vaccination is another example in which regular boosters are now needed in adults and older adults because the protection obtained either from the disease or from vaccination is not life-long. Also, the new threats caused by Zika, Ebola, and pandemic influenza viruses have shown how needs for immunization may be changing.
2.5. Community immunity
To interrupt virus or bacteria circulation in a given population, high vaccination coverage (typically > 90–95%) is needed [Citation49]. When the vaccination rate drops below this threshold, preventable infectious diseases may reappear. This has been recently illustrated by measles outbreaks in several regions of the world. From 2014 to 2015, the number of reported measles cases increased by 33% in Africa, 18% in the Eastern Mediterranean region, and 83% in Europe [Citation48].
The phenomenon generally known as herd immunity occurs when a sufficient proportion of a population is immune to an infectious disease (through vaccination or natural infection), which prevents its spread from person to person [Citation50,Citation51]. Thus, the benefits of vaccination programs can extend beyond the target population to include unvaccinated individuals, such as newborns and immunocompromised individuals, who are conferred some protection because the disease has little opportunity to spread within the community [Citation51]. This indirect effect has been illustrated by the decrease in invasive pneumococcal disease in adults aged ≥ 65 years after pneumococcal conjugate vaccines were introduced into childhood immunization programs [Citation52,Citation53]. However, for some people who question the efficacy and safety of vaccines, the term ‘herd immunity’ may invoke the idea that people who get vaccinated are ‘mindless sheep’ who follow the recommendations of governments, pharmaceutical companies, or physicians, without thinking [Citation54]. Instead, we favor the use of the term ‘community immunity’ [Citation49,Citation50], which conceptualizes vaccine acceptors as a group of people who value vaccination for themselves and for others [Citation55]. It is therefore imperative that the community immunity protections offered by routine immunization programs are not eroded by the factors affecting vaccine uptake that we explore in the next section.
3. Current barriers to life-course immunization
Health recommendations worldwide are increasingly addressing the topic of life-course immunization. However, lack of knowledge of the benefits of adult vaccination, low vaccine coverage, lack of confidence, and limited convenience remain major hurdles in most countries, contributing to poor vaccination coverage among pregnant women, adults, and older adults. In Europe, the fact that the vaccines recommended for adults vary by country is another factor that may confuse healthcare providers (HCPs) and the general public regarding the necessity to vaccinate. In less developed countries globally, health systems’ capacities to implement life-course immunization is stymied by a lack of economic, social, and governance resources. In such contexts, childhood vaccination programs remain the oldest, most visible and most well-known intervention, potentially limiting the rollout of schemes for adults. However, institutions like WHO, are already looking at a road-map on how to integrate the life-course approach to better sustain their healthy aging programs for adults worldwide [Citation56].
3.1. Complacency
The past successes of vaccination programs have virtually eliminated most vaccine-preventable infectious diseases in industrialized countries (e.g. tetanus, diphtheria, and polio), and these diseases have rarely resurfaced in decades. These successes have, however, contributed to vaccination complacency in these countries [Citation57,Citation58]. Perception of the risk of infectious diseases has diminished, while attention to potential adverse effects of vaccines has been amplified in a society that expects zero risks from medical interventions. For this reason, some people now fear the risk of vaccination more than the risk of disease [Citation42]. Moreover, many do not perceive the need for vaccines and do not value vaccination, potentially leading to vaccine hesitancy or refusal. Social science may thus help propose strategies to address complacency. For instance, influenza vaccination rates in adults increased by 4% when a ‘nudge’ was used to influence the opportunity of action of the individuals. This nudge consisted of a mailed reminder that included a prompt to get vaccinated [Citation59].
3.2. Vaccine hesitancy and refusal
A WHO Strategic Advisory Group of Experts (SAGE) working group has defined vaccine hesitancy as a delay in acceptance or refusal of vaccination despite availability of vaccination services [Citation57]. They explain that vaccine hesitancy is influenced by factors such as complacency (people may not perceive a need for a vaccine), convenience (vaccine accessibility or simplicity of the ‘vaccination journey’), and confidence (people may not trust vaccines or providers), represented in the ‘3Cs’ model [Citation57]. However, hesitancy as it is generally understood is not the only, or often even the major barrier to vaccination. Cost, accessibility and social norms also can play major roles. We therefore advocate that the term ‘vaccine hesitancy’ be applied only to individuals who are undecided and not to logistical or opportunity-related factors [Citation60]. Although vaccine hesitancy has existed since the advent of vaccines, it is now supported and amplified by information easily available on the internet. Indeed, the Internet and social networks have recently emerged as important providers of health information for the general public and are challenging traditional sources of medical education and advice, such as physicians [Citation61,Citation62]. ‘Dr. Google’ and social media are thus changing the way people make decisions and prepare for medical appointments [Citation58,Citation61,Citation63]. The anti-vaccine lobby is firmly entrenched in the internet and increasingly competes with the influence of the medical community and public health authorities who have evidence-based information to share [Citation64–Citation67]. This ‘post-truth’ movement [Citation68] is likely responsible for much vaccine hesitancy. Post-truth relates to circumstances in which people are more likely to accept an argument based on their emotions and beliefs, rather than one based on facts. People do not rely only on HCPs or health authorities to make their choice but also on what they read on the internet, what they discuss with friends and their community. Of course, dialogue is still part of medical practice but people have become the central actors regarding decision-making about their own health, and the displacement of medical expertise within this paradigm is a concern.
3.3. Free-riding
Vaccination has both individual and collective benefits. The collective benefits derive from community immunity [Citation69]. However, high vaccination coverage may encourage ‘free-riding’, in which people who do not contribute to the collective effort still benefit from it without any potential adverse events of vaccination [Citation70]. This means that vaccine-rejecting parents may be able to make their vaccination decisions without fear that their children are at risk of catching the diseases. Qualitative studies in industrialized countries have found that some parents made their decisions not to vaccinate in part because they could rely on community immunity [Citation71,Citation72]. Some of these free-riders see the collective effort as something that is authoritarian and controlling and against an individual’s choice and freedom [Citation73]. This may lead to suboptimal vaccine coverage in the community, and therefore a higher risk of disease for all. Although they are not trying to harm anybody, people who choose not to be vaccinated put both themselves and others in their community at risk by not contributing to community immunity.
Other individuals may also choose not to be vaccinated based on what others do (i.e., bandwagoning) [Citation74]. This phenomenon can lead to clusters of unvaccinated individuals that facilitate local outbreaks of infectious diseases despite high overall vaccination coverage [Citation75].
3.4. Low vaccine coverage
Vaccines have dramatically decreased morbidity and mortality from infectious diseases in children, but they have not had the same impact in adults so far, primarily due to low vaccine uptake or low vaccine effectiveness, as observed for influenza and pneumococcal vaccines [Citation23,Citation76–Citation78]. In 2015, 69% of US adults aged ≥ 65 years had received an influenza vaccine in the previous 12 months and only 34% had received the herpes zoster vaccine [Citation79]. In Italy, < 50% of adults aged ≥ 65 years were vaccinated during the 2014–2015 influenza season, despite availability of the vaccine free of charge [Citation80]. European national surveys suggest that improved understanding of barriers to influenza vaccination is needed to increase vaccine uptake and reverse negative trends [Citation81]. Although influenza and Tdap vaccines are recommended for all pregnant women in the United States, coverage rates remain low at around 53% for each vaccine [Citation82,Citation83]. Among US adolescents, 88% received a Tdap booster but only 39% received their second meningococcal vaccine dose and only 43% were up to date with the HPV vaccination series [Citation84].
Incomplete or delayed vaccination reduces community immunity and allows diseases to reemerge, as illustrated by recent measles outbreaks in Europe and the United States [Citation85,Citation86]. Measles is one of the most contagious diseases of humans but it is preventable and can be eliminated by vaccination. A second vaccine dose, usually provided in the second year of life or at school entry, is needed to protect children who might not have developed protective immunity after the first dose [Citation47]. In 2015, the worldwide coverage was estimated as 85% for the first measles vaccine dose but only 64% for the second dose, with disparities between world regions [Citation87]. Tetanus and diphtheria are other examples. The WHO recommends a primary vaccination series against tetanus and diphtheria during childhood and regular booster vaccinations throughout life [Citation43,Citation45] and many countries recommend these vaccines throughout adulthood, sometimes in combination with pertussis vaccine [Citation11,Citation28]. However, coverage rates remain below 75% [Citation23]. The classical approach used so far has not achieved high vaccine coverage in adolescents and adults (); thus, additional strategies are needed so that toddlers, adolescents, and adults complete their vaccination courses or receive the necessary boosters.
Figure 2. Booster vaccination may be required for some vaccine preventable diseases. © Comic House Amsterdam BV. Used with permission.
The leading causes of low vaccine uptake are poor access due to lack of resources or appropriate infrastructures, and lack of vaccine knowledge in the general public and in HCPs [Citation88]. Many HCPs do not actively encourage vaccine use in adulthood, even if they acknowledge its value [Citation77,Citation89]. However, HCP attitude toward vaccination is perhaps the strongest influence on the decision-making of parents and patients [Citation90], as suggested by studies performed in the United States [Citation82,Citation91,Citation92], the United Kingdom [Citation93], and Australia [Citation94,Citation95]. In one study that evaluated factors associated with influenza vaccine uptake in pregnant women, the main reason cited for receiving the vaccine was recommendation from a general practitioner, whereas non-recommendation and lack of knowledge were cited as the main reasons for not receiving the vaccine [Citation95].
In addition to not encouraging vaccination among their patients, some HCPs do not receive vaccines themselves. HCPs are at high risk of not only acquiring but also transmitting infections through continual contact with patients and other HCPs [Citation96,Citation97]. Consequently, vaccination of HCPs in hospitals and geriatric settings is an important measure to control transmission of infectious diseases. However, vaccination coverage is often low among HCPs despite vaccination recommendations being in place for more than three decades in many countries [Citation98]. In the United States, the vaccination coverage rate among HCPs was 42% for Tdap in 2014 and 79% for seasonal influenza vaccine during the 2016–2017 season [Citation99,Citation100]. Notably, the most frequent reason for HCPs not receiving vaccine was fear of adverse events [Citation101], underlining the need to better inform and educate HCPs on this matter. However, it is reassuring to see that targeted quality improvement initiatives can modify the HCP behavior and increase Tdap uptake from 58% to 90% over an 18-month period [Citation102].
3.5. Challenges in vaccinating special populations
Historically, randomized controlled trials were designed to recruit a homogenous group of healthy subjects, from which pregnant women, subjects with chronic conditions, and frail subjects were systematically excluded [Citation103]. Currently, health authorities are requesting that clinical trials also be performed in these susceptible populations to gather specific data on immunogenicity, efficacy, and safety. For clinical trials in older adults, segmenting studies according to the frailty index [Citation104] could help generate useful data on the impact of vaccination based on the subjects’ different baseline conditions [Citation103]. Obtaining more specific data in special populations could help optimize policies and recommendations.
Most current vaccines indicated for adults are not specifically indicated during pregnancy because they were not studied in pregnant women in prelicensure trials [Citation105]. However, many post-licensure studies have evaluated vaccine safety and effectiveness in pregnant women. These studies have shown that many currently available vaccines have a favorable benefit-risk profile in pregnancy, for both mothers and infants [Citation36,Citation105]. Based on these results, the WHO and an increasing number of health authorities worldwide recommend maternal immunization against influenza, tetanus, and pertussis [Citation36]. Nevertheless, HCPs and pregnant women are still cautious about any intervention including vaccines during pregnancy [Citation106]. The situation has changed in recent years, several new candidate vaccines are specifically being developed for pregnant women, and clinical trials are increasingly being conducted in pregnant women to ensure, before licensure, that vaccine candidates are effective and well tolerated in this population and that these vaccines, once licensed, are indicated for this particular population. Unfortunately, enrolment into such trials is often low because of concerns from both HCPs and pregnant women due to this old paradigm of not vaccinating in a ‘vulnerable population,’ suggesting more education and awareness initiatives are needed. Another option states can consider is to increase mandatory vaccines for workers in key public-facing sectors in order to protect the health of those with whom they interact.
4. Improving vaccination culture requires a paradigm shift
4.1. Pediatricians as ambassadors of vaccine culture
Concerns about vaccination reflect the perceptions of vaccination in specific cultures. Medical anthropologists have identified local ‘vaccination cultures’ in diverse settings around the globe [Citation107]. Vaccination acceptance depends on local context, which may be influenced by health practices, knowledge and beliefs about vaccination, and past experiences with vaccinations. In today’s world, we suggest that a cohesive vaccine culture should emerge, with an important role afforded to pediatricians and public health officers, the individuals who are historically most involved with vaccinations, plus general practitioners, because they are closest to the individuals and families in most healthcare systems. Using an interdisciplinary perspective, we have the capacity to enhance and extend this culture to other health professionals and the public in order to build support for vaccination at all stages of life regardless of cultural differences in healthcare systems and societal structures.
While there are inevitably national and regional differences, in general the culture and knowledge of vaccines and vaccination are mostly restricted to pediatricians, general practitioners and public health officers. These key players are, therefore, the logical gateways to discussions on life-course immunization with families and other HCPs such as geriatricians, obstetricians-gynecologists, cardiologists, pharmacists, nurses, and midwives. In some countries, the role of specialists may be less, while other HCPs such as health visitors and vaccination teams already playing an expanded role in vaccination advocacy. Because communication about the importance of vaccination, vaccine safety, and efficacy is complex and sometimes controversial, it warrants innovative solutions that must be tailored to local conditions. Such solutions should start with mutual respect and accounting for the needs, concerns, and underlying motives of patients, parents, and physicians [Citation108]. Involving other HCPs besides pediatricians and general practitioners will be essential for reaching out to older populations and for sending clear messages to the public. Interprofessional collaboration in education and practice was identified as an innovative strategy by the WHO and its partners in diminishing the challenges faced by global health systems [Citation109]. Successful collaboration between different medical societies has already led to the new life-course vaccination plan in Italy [Citation17]. We therefore propose that pediatricians and general practitioners become ambassadors of vaccination culture toward other HCPs and families, so that vaccination becomes part of a healthy lifestyle at all ages, like other preventive measures. Pediatricians and general practitioners liaise with obstetricians, community midwives, and neonatal teams on a fairly regular basis and are well placed to pursue the transferability of vaccination expertise to their fellow professionals. Discussion on immunization with parents and the extended family during a pediatric consultation would be an inclusive approach to communicate the importance of life-course immunization in day-to-day clinical practice. Moreover, public health professionals should catalyze the cultural and professional exchange of knowledge between different sectors of the healthcare system. Breaking the barriers (i.e. the silos) between different prevention services and programs may allow a better implementation of interdisciplinary activities. As an example, communication on vaccination could be part of a smoking-cessation program as well as other programs, such as promoting physical activity in older adults or fighting obesity among adolescents.
4.2. Improving vaccine convenience
Vaccination coverage rates are generally much lower for adults than for children [Citation11,Citation23,Citation76]. A frequent cause of low vaccine uptake in adults is poor accessibility due to lack of resources or appropriate infrastructures, or a complex vaccination ‘journey’ that discourages individuals from completing it [Citation88]. Depending on the healthcare system, reimbursed or free-of-charge vaccinations and well-designed delivery systems are needed to improve vaccine convenience. One way to increase vaccine access for adults is by providing vaccination in the workplace and at the pharmacy, as tested for influenza vaccination [Citation110,Citation111]. Recall or reminder programs (e.g. by phone calls, text messages, or postcards) have been shown to increase vaccination rates [Citation59,Citation112]. According to the nudge theory, small improvements in the way vaccinations are scheduled could increase the likelihood of adults getting vaccinated [Citation59]. Therefore, governments, policymakers, and HCPs should work together to find creative ways to ensure vaccines are more easily available for all.
The pharmaceutical industry, which is involved in the entire vaccination process, should also ensure, together with governments and health authorities, that appropriate vaccines are available, with improvements such as combinations with other vaccines, fewer doses, ease of administration, and affordability for the targeted populations. Therefore, health outcome assessments are increasingly considered to support vaccine recommendation and procurement negotiations. An adequate vaccine supply is another important determinant for successful vaccination campaigns. This requires a continuous conversation between manufacturers, health authorities, and providers to make sure supply forecasts are reliable and sustainable in view of the complexity and length of the vaccine manufacturing and delivery process.
4.3. Addressing vaccine uptake by understanding and including public viewpoints – a new ‘4Cs’ model
Although widespread vaccine hesitancy is an important hurdle to attaining optimal vaccination coverage, it is far from being the only obstacle: other factors such as accessibility and public health support may be as important or more important [Citation60]. Nonetheless, in terms of changing perception and support for vaccination it cannot be ignored. Existing scholarship argues that health stakeholders need to act on three levels, represented in the ‘3Cs’ model: confidence, complacency, and convenience [Citation57]. They need to enhance the population’s confidence about vaccines, remove the complacency about infectious diseases, and improve convenience by ensuring vaccines are affordable and easily available. We have suggested that convenience factors should not be included with hesitancy and prefer to frame the ‘Cs’ model as providing ways of addressing vaccine uptake. We propose that a fourth ‘C’ for ‘cultural acceptance’ should be added to this toolkit, producing a ‘4Cs’ model to enhance uptake (). Being mindful of cultural aspects could be an important aspect in converting ‘vaccine availability’ to ‘vaccination acceptability’. Patients’ or parents’ vaccination uptake often derives from a mix of sociocultural, religious, psychological, and political factors in addition to scientific and economic factors [Citation113,Citation114]. In Nigeria and Pakistan, implementation of polio vaccination campaigns have been hampered by rumors circulated by some political and religious leaders who claimed that the oral polio vaccine was contaminated with pork (the consumption of which is forbidden by Islam) or HIV or could cause sterilization in those vaccinated [Citation115,Citation116]. Better understanding of the cultural specificities of the target population is therefore necessary to sustain or restore confidence in vaccines [Citation113].
Figure 3. How healthcare workers can influence vaccination uptake – the ‘4Cs’ model 4Cs: Convenience, Confidence, Complacency, and Cultural acceptance.
Several specific measures could help limit vaccine hesitancy. Appropriate communication strategies toward at-risk populations and HCPs should be implemented. Transparent and timely communication to the media and general public about vaccine safety and efficacy should be a core responsibility of HCPs [Citation117]. Regular proactive communication on the role of vaccines in the disappearance of certain infectious diseases would also help fight complacency [Citation118]. To help national health authorities in this task, the WHO has provided a series of documents to build and restore confidence in vaccines and vaccination, both when infectious diseases are under control and during crises [Citation119]. These documents present the scientific evidence behind the WHO’s recommendations and provide practical guidance for specific situations. Adapting the communication and language to the current evolution of societal dynamics and preferences is also pivotal. Using cartoons or comics may be an innovative strategy to attract attention and curiosity, or to demystify vaccination concepts for the general public. Compared to text-based flyers, comics were shown to have positive effects on adult and teenage attitudes toward the scientific concepts underlying infectious diseases and vaccination [Citation120,Citation121]. The general tone, format, and language of communications need to be adapted to harness the current behavior change strategies available in our society to make a difference. This is why behavioral science is increasingly considered in the implementation of preventive measures, including immunization [Citation72,Citation122].
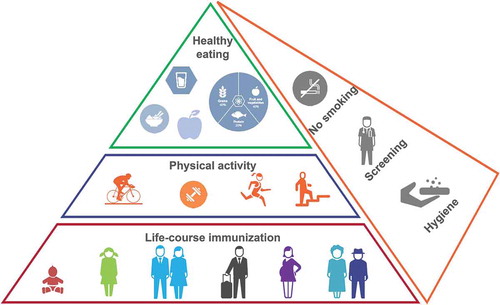
Because vaccine decisions are likely to be influenced by social contacts, the trends of free-riding and bandwagoning can have negative epidemiological effects. Policy makers must therefore understand the causes, magnitude, and implications of these behaviors for disease control. Potential responses to free-riding include making exemptions to mandatory vaccines for religious or philosophical objections more difficult, providing incentives to vaccinate, and restricting unvaccinated children’s participation in social activities [Citation70,Citation123], Policymakers at national and sub-national levels of government in a range of international settings are introducing such strategies. For example, while Italy’s new National Vaccine Plan focuses on a range of factors pertinent to life-course immunization, the introduction of financial penalties for parents who do not vaccinate their children directly addresses parents’ contribution to community immunity. Early indications that the policy was driving the uptake of catch-up vaccines invite close attention, as the new government has now weakened the mandatory policy [Citation20,Citation124,Citation125]. Different policies recently introduced in Germany, France, Australia, and various US states provide natural experiments enabling scholars to observe the effects of policy design and implementation on uptake, although the ethics and efficacy of mandatory policies remain topics of contention [Citation126]. To avoid the risk of bandwagoning, the idea that vaccination is the social norm should be reinforced. Making vaccination a social norm for a healthy lifestyle, in the same way as healthy eating and adequate physical exercise, could be one way to make it more acceptable across all age groups ().
Figure 4. Life-course immunization as an integral part of a healthy lifestyle pyramid. © 2018 the GSK group of companies.
To make life-course immunization part of the social norm for a healthy lifestyle, vaccination topics have to be more embedded in our daily life, on digital channels, at school, in the workplace, or in leisure time. Only a direct dialogue between authorities, HCPs, and public will make it possible. It is essential to listen, understand, and include public viewpoints to increase vaccine awareness and uptake and change the culture of vaccination in our societies.
Vaccination expertise exists primarily among pediatricians, general practitioners, and public health specialists. These groups should disseminate their knowledge to other HCPs through interdisciplinary information sharing to improve the acceptance of national recommendations among the target populations [Citation58]. Awareness campaigns could also be used to promote vaccine uptake among different age groups by having all the impacted healthcare specialties gathered together and supported by these ambassadors of the vaccination culture.
To help achieve higher vaccination coverage among HCPs, workplace strategies such as vaccination requirements or promotion of free on-site vaccinations may be needed [Citation99]. Campaigns aimed at educating HCPs about the benefits of vaccination for themselves, with an emphasis on patient protection as a fundamental responsibility, could help overcome HCP hesitancy [Citation127]. Groups of HCPs not previously involved in this discussion, such as medical or nursing students, should also be targeted because vaccinology is still not a main course in many education programs. Obstetricians-gynecologists, midwives, and general practitioners are key to ensuring that pregnant mothers are informed about recommended vaccines. Recommendations from HCPs and vaccine availability in antenatal clinics are effective ways to improve vaccine uptake among pregnant mothers [Citation37]. New interventions to improve education and communication of maternal vaccination delivered by midwives and obstetricians may reduce vaccine hesitancy among women during pregnancy and post-delivery periods [Citation128]. However, because education of HCPs is unlikely to be sufficient, parents should also be targeted through specific public awareness campaigns or individual interventions during standard care. This is of particular importance because the process of vaccine decision-making begins prenatally and, often, first-time mothers are initially hesitant and undecided [Citation128]. Pregnant women who reported higher levels of vaccine hesitancy regarding themselves were also less likely to have fully vaccinated their child after delivery [Citation128]. Several surveys have shown that parents view vaccination fundamentally as something for their child and that vaccinating their child for the good of the community is not a significant reason for vaccination [Citation73,Citation129]. Increasing awareness that vaccination provides health benefits for their children and for the community as well is necessary. Therefore, better understanding of sociological and anthropological factors that impact human behavior and decision-making is important to have the right approach to vaccination.
5. Expert commentary
Immunization programs are key preventive measures that have largely contributed to reducing the burden of infectious diseases over the last century. Well-functioning childhood vaccination programs have largely eliminated many formerly common infections in children, showing what is possible with good coverage levels. Improving coverage in adolescents, adulthood and the later stages of the life span (i.e. adolescents, adults, and older adults) offers the potential to achieve similar gains in health in the face of changing dynamics in infectious diseases and the world’s aging population. Furthermore, it aligns with the need to increase disease prevention in current healthcare systems. An aging population is associated with a higher incidence of chronic, degenerative, and infectious diseases, all of which have a substantial impact on health expenditures. Life-course immunization would be key part of healthy aging and would, as a direct result, help keep health expenditures under control [Citation130].
Beside demographic changes, population behaviors regarding healthcare are also changing. Research and technological development are becoming ever faster-paced. Technologies such as the internet, smartphones, and social media have revolutionized the relationship between healthcare providers and patients. People increasingly search for health information online, meaning that patients have direct access to health information and are thus increasingly becoming central actors in maintaining their own health [Citation67].
Despite the recommendations, immunization rates in adolescents and adults remain suboptimal in many countries and are still much lower than those in children. Healthcare stakeholders have to act on at least four levels to counteract this low vaccine uptake: enhance immunization confidence in population, remove complacency around infectious diseases, improve convenience by ensuring vaccines are more accessible, and be mindful of cultural acceptance by better understanding and considering different public concerns ().
Behavioral, economic, and anthropological studies should be conducted to better understand the needs and expectations of the public. These studies would help develop evidence-based strategies to guide health authorities and HCPs on how best to communicate the importance of vaccination to vaccine-hesitant parents and patients, both from personal and societal viewpoints. Improved communication is especially needed in societies where complacency about vaccine-preventable diseases has been established for a long time. The medical community and policymakers should invest more in proactive strategies to communicate understandable and accessible scientific evidence and counter antivaccine activists through fact checking, debunking, or positive narratives about vaccination [Citation58]. Social media campaigns should be used to disseminate reliable information about vaccinations to a wide audience [Citation61].
In many countries, each public health sector is compartmentalized and this current ‘silo effect’ [Citation111] is a significant hurdle for implementing a global public health prevention plan. Different public health programs (e.g. tobacco control program, obesity control program, vaccination program) have to be cross-fertilized to be more efficient. In the future, a ‘stop smoking’ style campaign could be expanded to all other healthy lifestyle choices, which includes immunization. A global public health prevention plan should be collectively promoted with, at its heart, the healthy lifestyle pyramid updated to include the role of life-course immunization: ‘Don’t smoke, eat well, be physically active, and stay immunized at all stages of life’ should become the new slogan ().
The role of pediatricians, general practitioners, and public health specialists as the providers and ambassadors of vaccination culture toward other HCP categories should be emphasized. This would ensure that healthcare systems speak with one voice to the patients and families. Strong recommendations from HCPs have been critical to the success of childhood immunization programs, similar recommendations are now needed to improve adult immunization rates.
Currently, many opportunities for vaccination are being missed at scheduled medical visits and during in-patient encounters [Citation131–Citation133]. A missed vaccination opportunity is defined as a medical visit where a patient eligible for vaccination remained unvaccinated. In the United States, 90% of adults with high-risk conditions have missed at least one potential opportunity for receiving influenza vaccination [Citation131]. In many countries, there is no structured approach by which HCPs can use other medical visits (e.g. general check-up visits, occupational health checks) to check the vaccination status of individuals and offer missing vaccinations if required. To avoid missed opportunities for vaccination, HCPs should systematically assess patients’ vaccination history and recommend the necessary vaccines. Appropriate vaccination documentation (e.g. electronic vaccination certificates) is therefore crucial to reliably assess the vaccinations administered throughout life [Citation11]. The key messages and scope of our perspective is provided in .
6. Five-year view
In the next few years, data from large epidemiological surveillance platforms in many different regions will become available to help evaluate the local burden of infectious diseases in populations of all ages, notably in older adults. This will help determine areas where disease prevention efforts should be focused. In addition, electronic immunization registries will be set up to improve the quality of data used for measuring vaccine safety and effectiveness as well as the impact of vaccination programs. Such registries will also allow HCPs and patients to access information on their vaccination status through user-friendly interfaces, which will improve compliance to vaccination schedules.
Although it is still difficult to recruit special populations (i.e. pregnant women, frail individuals, and older adults) in clinical trials, it will be possible in the future if all stakeholders work together to change the current paradigm [Citation77]. This will strengthen the scientific evidence supporting adequate vaccination recommendations in these populations.
The overall burden of infectious diseases will continue to decrease as new vaccines are developed and licensed. Vaccines against remaining challenges, such as RSV and GBS, could be available for pregnant women and those with chronic conditions within the next decade. Universal influenza vaccines that protect against all type A viruses and which will bypass the need for annual revaccinations, will enter clinical development [Citation46,Citation134]. The pharmaceutical industry will also continue to work toward solutions that increase vaccine uptake, for example by developing combined vaccines, improving vaccine immunogenicity to reduce the numbers of doses required, and developing more convenient administration routes.
Further sociological and behavioral studies conducted over the next few years will help identify new, more effective approaches and educational materials that can be used to increase public awareness of the benefits of vaccination throughout life. Campaigns sponsored by health departments on social media such as Facebook, Twitter, and Instagram will help reach the public to disseminate accurate health information. To reach a real consensus between public health programs, individual vaccinators, HCPs, and the general public regarding vaccination and to help sustain or improve confidence in vaccines, future vaccine implementation programs should always consider and adapt to the needs of individuals. This will be possible only if target populations are convinced of the benefits of vaccines and are able to receive them in an easy way.
Key issues
Vaccination provides protection and health benefits at all stages of life but requires a paradigm shift because vaccination uptake beyond childhood is poor. The two main aspects to be added to the classical ‘3Cs’ model is the removal of silos between healthcare specialties involved in prevention and a 4th C for cultural acceptance, hence the new ‘4Cs’ model.
Improving the convenience, enhancing the confidence, removing the complacency, and being mindful of cultural aspects would be important to convert ‘vaccine availability’ to ‘vaccination acceptability’. The recipe for success is linked to creating digital forums for discussion where the public viewpoint is listened to, understood, and included to support life-course immunization.
It is time to add vaccination to the toolbox of healthy living: ‘Don’t smoke, eat well, be physically active, and get vaccinated’ as a whole program and to make vaccination an integral part of social norms regarding health.
Disease prevention programs among adolescents, adults, older adults, and during pregnancy must be improved and include vaccination components. Behavioral and sociological studies are as important as scientific studies to ensure the appropriate approaches and communications are used to increase public awareness and acceptance.
Progress in healthcare and health technologies has increased life expectancy. It is now time to improve health over this longer lifespan through vaccination, so that people can live healthier, longer lives.
Declaration of interest
R.K. Philip received educational grants and honoraria from Merck MSD and the GSK group of companies for activities outside the submitted work. K. Attwell received travel, accommodation, and registration support from the GSK group of companies as an invited speaker at the ESPID 2017 symposium. T. Breuer and A. Di Pasquale are employees of the GSK group of companies and hold shares in the GSK group of companies. P.L. Lopalco received educational grants from Pfizer and the GSK group of companies, and honoraria from Sanofi and Merck MSD for activities outside the submitted work. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Authors’ contributions
All authors provided substantial scientific input, reviewed the literature, contributed to the writing, and reviewed the manuscript. All authors gave their final approval and are accountable for all aspects of the work.
Acknowledgments
Authors would like to thank T. Mark Doherty (GSK, Belgium) for the critical review of the manuscript. They also thank Business & Decision Life Sciences platform for editorial assistance and manuscript coordination, on behalf of GSK. Vincent Laporte coordinated manuscript development and editorial support. Writing assistance was provided by Dr. Julie Harriague (4Clinics, France), on behalf of GSK.
Additional information
Funding
References
- He W, Goodkind D, Kowal P. An Aging World: 2015 - International Population Reports [Internet]. Washington (DC): U.S. Census Bureau. [cited 21 Sep 2017]. Available from: https://www.census.gov/content/dam/Census/library/publications/2016/demo/p95-16-1.pdf.
- Centers for Disease Control and Prevention (CDC). Ten great public health achievements–United States, 1900-1999. MMWR Morb Mortal Wkly Rep. 1999;48(12):241–243.
- Delany I, Rappuoli R, De Gregorio E. Vaccines for the 21st century. EMBO Mol Med. 2014;6(6):708–720.
- Thomas-Crusells J, McElhaney JE, Aguado MT. Report of the ad-hoc consultation on aging and immunization for a future WHO research agenda on life-course immunization. Vaccine. 2012;30(42):6007–6012.
- Doherty M, Schmidt-Ott R, Santos JI, et al. Vaccination of special populations: protecting the vulnerable. Vaccine. 2016;34(52):6681–6690.
- World Health Organization. Active Ageing: A Policy Framework [Internet]. Geneva (Switzerland): World Health Organization. [cited 14 Feb 2018]. Available from: http://apps.who.int/iris/bitstream/10665/67215/1/WHO_NMH_NPH_02.8.pdf.
- Gavazzi G, Krause KH. Ageing and infection. Lancet Infec Dis. 2002;2(11):659–666.
- Goronzy JJ, Weyand CM. Understanding immunosenescence to improve responses to vaccines. Nat Immunol. 2013;14(5):428–436.
- Garau J, Hodin MW, Kalache A. Life-course immunization: a driver of healthy aging [Internet]. The Global Coalition on Aging. [cited 15 Sep 2017]. Available from: https://globalcoalitiononaging.com/wp-content/uploads/2018/07/life-course-immunization_gcoa-for-web-1.pdf
- World Health Organization. Global vaccine action plan 2011-2020 [Internet]. Geneva (Switzerland): World Health Organization. [cited 10 Mar 2017]. Available from: http://www.who.int/immunization/global_vaccine_action_plan/GVAP_doc_2011_2020/en/
- Weinberger B. Adult vaccination against tetanus and diphtheria: the European perspective. Clin Exp Immunol. 2017;187(1):93–99.
- Steeper M, Plebanski M, Flanagan KL. The global challenge and future strategies for keeping the world’s aging population healthy by vaccination. Trans R Soc Trop Med Hyg. 2016;110(8):427–431.
- National Vaccine Advisory Committee. A pathway to leadership for adult immunization: recommendations of the National Vaccine Advisory Committee: approved by the National Vaccine Advisory Committee on June. 14, 2011. Public Health Rep. 2012;127(Suppl 1):1–42.
- National Prevention Council. Healthy Aging in Action [Internet]. Washington (DC): U.S. Department of Health and Human Services, Office of the Surgeon General. [cited 4 Dec 2017]. Available from: https://www.cdc.gov/aging/pdf/healthy-aging-in-action508.pdf
- Ali KA, Celentano LP. Finding the balance in life-course immunization. Eurohealth. 2016;22(3):22–32.
- World Health Organization. European Immunization Week 2017 [Internet]. Geneva (Switzerland): World Health Organization. [cited 15 Sep 2017]. Available from: http://www.euro.who.int/en/media-centre/events/events/2017/04/european-immunization-week-2017
- Bonanni P, Chiamenti G, Conforti G, et al. The 2016 lifetime immunization schedule approved by the Italian scientific societies: a new paradigm to promote vaccination at all ages. Hum Vaccin Immunother. 2017;13(11): 2531–2537.
- Signorelli C, Iannazzo S, Odone A. The imperative of vaccination put into practice. Lancet Infec Dis. 2018;18(1):26–27.
- Burioni R, Odone A, Signorelli C. Lessons from Italy’s policy shift on immunization. Nature. 2018;555(7694):30.
- Signorelli C, Guerra R, Siliquini R, et al. Italy’s response to vaccine hesitancy: an innovative and cost effective national immunization plan based on scientific evidence. Vaccine. 2017;35(33):4057–4059.
- Lévy-Bruhl D, Desenclos J-C, Quelet S, et al. Extension of French vaccination mandates: from the recommendation of the steering committee of the citizen consultation on vaccination to the law. Euro Surveill. 2018;23(17):pii=18-00048. Available from: https://doi.org/10.2807/1560-7917.ES.2018.23.17.18-00048
- Yang YT, Studdert DM. Linking Immunization Status and. Eligibility for welfare and benefits payments: the Australian “No Jab, No Pay” legislation. JAMA. 2017;317(8):803–804.
- Kanitz EE, Wu LA, Giambi C, et al. Variation in adult vaccination policies across Europe: an overview from VENICE network on vaccine recommendations, funding and coverage. Vaccine. 2012;30(35):5222–5228.
- Sanderson W, Scherbov S. Rethinking age and aging. Popul Bull. 2008;63(4):3–16.
- Crews DE, Zavotka S. Aging, disability, and frailty: implications for universal design. J Physiol Anthropol. 2006;25(1):113–118.
- World Health Organization. Vaccines against influenza WHO position paper - November 2012. Releve Epidemiologique hebdomadaire/Section D’hygiene Du Secretariat De La Societe Des Nations = Weekly Epidemiological record/Health Section of the Secretariat of the League of Nations. 2012;87(47):461–476.
- ACIP Adult Immunization Work Group, Bridges CB, Woods L, Coyne-Beasley T. Centers for disease control and prevention. Advisory Committee on Immunization Practices (ACIP) recommended immunization schedule for adults aged 19 years and older–United States, 2013. MMWR Supplements. 2013;62(1):9–19.
- Kim DK, Riley LE, Harriman KH, et al. Advisory committee on immunization practices recommended immunization schedule for adults aged 19 years or older - United States, 2017. MMWR Morb Mortal Wkly Rep. 2017;66(5):136–138.
- Department of Health. Immunise Australia Program - Older Australians [Internet]. Canberra (ACT): Australian Government. [cited 15 Nov 2017]. Available from: http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/older-australians
- National Health Service. NHS vaccination schedule [Internet]. London (UK): National Health Service. [cited 13 Nov 2017]. Available from: https://www.nhs.uk/Conditions/vaccinations/Pages/vaccination-schedule-age-checklist.aspx
- European Centre for Disease Prevention and Control. Seasonal influenza vaccination in Europe vaccination recommendations and coverage rates in the EU member states for eight influenza seasons: 2007–2008 to 2014–2015 [Internet]. Stockholm: ECDC. [cited 13 Nov 2017]. Available from: https://ecdc.europa.eu/sites/portal/files/documents/influenza-vaccination-2007%E2%80%932008-to-2014%E2%80%932015.pdf
- Chlibek R, Smetana J, Pauksens K, et al. Safety and immunogenicity of three different formulations of an adjuvanted varicella-zoster virus subunit candidate vaccine in older adults: a phase II, randomized, controlled study. Vaccine. 2014;32(15):1745–1753.
- Leroux-Roels I, Leroux-Roels G, Clement F et al. A phase 1/2 clinical trial evaluating safety and immunogenicity of a varicella zoster glycoprotein E subunit vaccine candidate in young and older adults. J Infect Dis. 2012;206(8):1280–1290.
- Lal H, Cunningham AL, Godeaux O, et al. Efficacy of an adjuvanted herpes zoster subunit vaccine in older adults. N Engl J Med. 2015;372(22):2087–2096.
- Cunningham AL, Lal H, Kovac M, et al. Efficacy of the herpes zoster subunit vaccine in adults 70 years of age or older. N Engl J Med. 2016;375(11):1019–1032.
- Chu HY, Englund JA. Maternal immunization. Clin Infect Dis. 2014;59(4):560–568.
- Bethancourt CN, Wang TL, Bocchini JA Jr. Vaccination during pregnancy: first line of defense for expecting mothers and vulnerable young infants. Curr Opin Pediatr. 2017;29(6):737–743.
- Swamy GK, Heine RP. Vaccinations for pregnant women. Obstet Gynecol. 2015;125(1):212–226.
- Regan AK. The safety of maternal immunization. Hum Vaccin Immunother. 2016;12(12):3132–3136.
- Lahra MM, Enriquez RP. Australian Meningococcal Surveillance Programme annual report, 2015. Commun Dis Intell Q Rep. 2016;40(4):E503–E511.
- Vyse A, Ellsbury G, Madhava H. Protecting UK adolescents and adults against meningococcal serogroup B disease. Expert Rev Vaccines. 2018;17(3):229–237.
- Rose KC. Adolescent vaccines: latest recommendations, addressing barriers, and improving vaccine rates. NASN Sch Nurse. 2017;32(4):217–222.
- World Health Organization. Tetanus vaccine. WHO position paper. Releve Epidemiologique hebdomadaire/Section D’hygiene Du Secretariat De La Societe Des Nations = Weekly Epidemiological record/Health Section of the Secretariat of the League of Nations. 2006;81(20):198–208.
- World Health Organization. Pertussis vaccines: WHO position paper - September 2015. Releve Epidemiologique hebdomadaire/Section D’hygiene Du Secretariat De La Societe Des Nations = Weekly Epidemiological record/Health Section of the Secretariat of the League of Nations. 2015;90(35):433–458.
- World Health Organization. Diphtheria vaccines: WHO position paper. Releve Epidemiologique hebdomadaire/Section D’hygiene Du Secretariat De La Societe Des Nations = Weekly Epidemiological record/Health Section of the Secretariat of the League of Nations. 2006;81(3):21–32.
- Houser K, Subbarao K. Influenza vaccines: challenges and solutions. Cell Host Microbe. 2015;17(3):295–300.
- World Health Organization. Measles vaccines: WHO position paper - April 2017. Releve Epidemiologique hebdomadaire/Section D’hygiene Du Secretariat De La Societe Des Nations = Weekly Epidemiological record/Health Section of the Secretariat of the League of Nations. 2017;92(17):205–227.
- Patel MK, Gacic-Dobo M, Strebel PM, et al. Progress toward regional measles elimination - worldwide, 2000-2015. MMWR Morb Mortal Wkly Rep. 2016;65(44):1228–1233.
- Fine PEM, Mulholland K. Community immunity. In: Plotkin SA, Orenstein WA, Offit PA, editors. Vaccines. 6th Edition ed. Philadelphia, United States: Elsevier/Saunders; 2013. p. 1395–1412.
- Centers for Disease Control and Prevention. CDC glossary [Internet]. Atlanta (GA): CDC. [cited 11 Sep 2017]. Available from: https://www.cdc.gov/vaccines/terms/glossary.html
- Kim TH, Johnstone J, Loeb M. Vaccine herd effect. Scand J Infect Dis. 2011;43(9):683–689.
- Centers for Disease Control and Prevention. Direct and indirect effects of routine vaccination of children with. 7-valent pneumococcal conjugate vaccine on incidence of invasive pneumococcal disease–United States, 1998-2003. MMWR Morb Mortal Wkly Rep. 2005;54(36):893–897.
- Fitzwater SP, Chandran A, Santosham M, et al. The worldwide impact of the seven-valent pneumococcal conjugate vaccine. Pediatr Infect Dis J. 2012;31(5):501–508.
- Attwell K, Smith DT, Ward PR. ‘The Unhealthy Other’: how vaccine rejecting parents construct the vaccinating mainstream. Vaccine. 2018;36(12):1621–1626.
- Attwell K, Smith DT. Parenting as politics: social identity theory and vaccine hesitant communities. Int J Health Governance. 2017;22(3):183–198.
- Teresa Aguado M, Barratt J, Beard JR, et al. Report on WHO meeting on immunization in older adults: Geneva, Switzerland, 22-23 March 2017. Vaccine. 2018;36(7):921–931.
- MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164.
- Philip RK, Shapiro M, Paterson P, et al. Is it time for vaccination to “Go Viral”? Pediatr Infect Dis J. 2016;35(12):1343–1349.
- Milkman KL, Beshears J, Choi JJ, et al. Using implementation intentions prompts to enhance influenza vaccination rates. Proc Natl Acad Sci U S A. 2011;108(26):10415–10420.
- Bedford H, Attwell K, Danchin M, et al. Vaccine hesitancy, refusal and access barriers: the need for clarity in terminology. Vaccine. 2017;pii: S0264-410X(17)31070-8. doi: 10.1016/j.vaccine.2017.08.004.
- Betsch C, Brewer NT, Brocard P, et al. Opportunities and challenges of web 2.0 for vaccination decisions. Vaccine. 2012;30(25):3727–3733.
- Forkner-Dunn J. Internet-based patient self-care: the next generation of health care delivery. J Med Internet Res. 2003;5(2):e8.
- Pias-Peleteiro L, Cortes-Bordoy J, Martinon-Torres F. Google: what about the human papillomavirus vaccine? Hum Vaccin Immunother. 1712-1719;9(8):2013.
- Kata A. Anti-vaccine activists, web 2.0, and the postmodern paradigm–an overview of tactics and tropes used online by the anti-vaccination movement. Vaccine. 2012;30(25):3778–3789.
- Aquino F, Donzelli G, De Franco E, et al. The web and public confidence in MMR vaccination in Italy. Vaccine. 2017;35(35): 4494–4498.
- Betsch C, Renkewitz F, Betsch T, et al. The influence of vaccine-critical websites on perceiving vaccination risks. J Health Psychol. 2010;15(3):446–455.
- Kata A. A postmodern Pandora’s box: anti-vaccination misinformation on the Internet. Vaccine. 2010;28(7):1709–1716.
- McCartney M. Margaret McCartney: evidence in a post-truth world. BMJ. 2016;355:i6363.
- Fine P, Eames K, Dl H. “Herd immunity”: a rough guide. Clin Infect Dis. 2011;52(7):911–916.
- Buttenheim AM, Asch DA. Making vaccine refusal less of a free ride. Hum Vaccin Immunother. 2013;9(12):2674–2675.
- Benin AL, Wisler-Scher DJ, Colson E, et al. Qualitative analysis of mothers’ decision-making about vaccines for infants: the importance of trust. Pediatrics. 2006;117(5):1532–1541.
- Reich J. Neoliberal mothering and vaccine refusal: imagined gated communities and the privilege of choice. Gend Soc. 2014;28(5):679–704.
- Sobo EJ. What is herd immunity. How Does It Relate to Pediatric Vaccination Uptake? US Parent Perspectives. Soc Sci Med. 2016;165:187–195.
- Hershley JC, Asch DA, Thumasathit T, et al. The roles of altruism, free riding, and bandwagoning in vaccination decisions. Organ Behav Hum Decis Process. 1994;59(2):177–187.
- Ndeffo Mbah ML, Liu J, Bauch CT, et al. The impact of imitation on vaccination behavior in social contact networks. PLoS Comput Biol. 2012;8(4):e1002469.
- Williams WW, Lu PJ, O’Halloran A, et al. Surveillance of vaccination coverage among adult populations - United States, 2015. MMWR Surveill Summ. 2017;66(11):1–28.
- Tan L. Adult vaccination: now is the time to realize an unfulfilled potential. Hum Vaccin Immunother. 2015;11(9):2158–2166.
- Tin Tin Htar M, Stuurman AL, Ferreira G, et al. Effectiveness of pneumococcal vaccines in preventing pneumonia in adults, a systematic review and meta-analyses of observational studies. PLoS One. 2017;12(5):e0177985.
- Norris T, Vahratian A, Cohen RA. Vaccination coverage among adults aged 65 and over: United States, 2015. NCHS Data Brief. 2017;281:1–8.
- Bonanni P, Ferro A, Guerra R, et al. Vaccine coverage in Italy and assessment of the 2012-2014 National Immunization Prevention Plan. Epidemiol Prev. 2015;39(4 Suppl 1):146–158.
- Jorgensen P, Mereckiene J, Cotter S, et al. How close are countries of the WHO European region to achieving the goal of vaccinating 75% of key risk groups against influenza? Results from national surveys on seasonal influenza vaccination programmes, 2008/2009 to 2014/2015. Vaccine. 2018;36(4):442–452.
- Ding H, Black CL, Ball S et al. Influenza vaccination coverage among pregnant women - United States, 2016-17 Influenza season. MMWR Morb Mortal Wkly Rep. 2017;66(38):1016–1022.
- Kerr S, Van Bennekom CM, Liang JL, et al. Tdap vaccination coverage during pregnancy - selected sites, United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66(41):1105–1108.
- Walker TY, Elam-Evans LD, Singleton JA, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years - United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66(33):874–882.
- Gahr P, DeVries AS, Wallace G, et al. An outbreak of measles in an undervaccinated community. Pediatrics. 2014;134(1):e220–228.
- Carrillo-Santisteve P, Lopalco PL. Measles still spreads in Europe: who is responsible for the failure to vaccinate? Clin Microbiol Infect. 2012;18(Suppl 5):50–56.
- Dabbagh A, Patel MK, Dumolard L, et al. Progress toward regional measles elimination - worldwide, 2000-2016. MMWR Morb Mortal Wkly Rep. 2017;66(42):1148–1153.
- Dube E, Gagnon D, Nickels E, et al. Mapping vaccine hesitancy–country-specific characteristics of a global phenomenon. Vaccine. 2014;32(49):6649–6654.
- de Gomensoro E, Del Giudice G, Doherty TM. Challenges in adult vaccination. Ann Med. 2018;50(3):181–192.
- Yaqub O, Castle-Clarke S, Sevdalis N, et al. Attitudes to vaccination: a critical review. Soc Sci Med. 2014;112:1–11.
- Opel DJ, Heritage J, Taylor JA, et al. The architecture of provider-parent vaccine discussions at health supervision visits. Pediatrics. 2013;132(6):1037–1046.
- Smith PJ, Kennedy AM, Wooten K, et al. Association between health care providers’ influence on parents who have concerns about vaccine safety and vaccination coverage. Pediatrics. 2006;118(5):e1287–1292.
- Holm MV, Blank PR, Szucs TD. Developments in influenza vaccination coverage in England, Scotland and wales covering five consecutive seasons from 2001 to 2006. Vaccine. 2007;25(46):7931–7938.
- Collins J, Alona I, Tooher R, et al. Increased awareness and health care provider endorsement is required to encourage pregnant women to be vaccinated. Hum Vaccin Immunother. 2014;10(10):2922–2929.
- Maher L, Hope K, Torvaldsen S, et al. Influenza vaccination during pregnancy: coverage rates and influencing factors in two urban districts in Sydney. Vaccine. 2013;31(47):5557–5564.
- Arden NH. Control of influenza in the long-term-care facility: a review of established approaches and newer options. Infect Control Hosp Epidemiol. 2000;21(1):59–64.
- Kroger AT, Atkinson WL, Marcuse EK, et al. General recommendations on immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2006;55(RR–15):1–48.
- Maltezou HC, Poland GA. Immunization of health-care providers: necessity and public health policies. Healthcare (Basel). 2016;4:3.
- Black CL, Yue X, Ball SW, et al. Influenza vaccination coverage among health care personnel - United States, 2016-17 Influenza Season. MMWR Morb Mortal Wkly Rep. 2017;66(38):1009–1015.
- Srivastav A, Black CL, Lu PJ, et al. Tdap vaccination among healthcare personnel, internet panel survey, 2012-2014. Am J Prev Med. 2017;53(4):537–546.
- Hofmann F, Ferracin C, Marsh G, et al. Influenza vaccination of healthcare workers: a literature review of attitudes and beliefs. Infection. 2006;34(3):142–147.
- Jiang C, Whitmore-Sisco L, Gaur AH, et al. A quality improvement initiative to increase Tdap (tetanus, diphtheria, acellular pertussis) vaccination coverage among direct health care providers at a children’s hospital. Vaccine. 2018;36(2):214–219.
- Ridda I, Lindley R, MacIntyre RC. The challenges of clinical trials in the exclusion zone: the case of the frail elderly. Australas J Ageing. 2008;27(2):61–66.
- Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. Sci World J. 2001;1:323–336.
- Roberts JN, Gruber MF. Regulatory considerations in the clinical development of vaccines indicated for use during pregnancy. Vaccine. 2015;33(8):966–972.
- de Martino M. Dismantling the taboo against vaccines in pregnancy. Int J Mol Sci. 2016;17:6.
- Streefland P, Chowdhury AM, Ramos-Jimenez P. Patterns of vaccination acceptance. Soc Sci Med. 1999;49(12):1705–1716.
- Seeber L, Michl B, Rundblad G, et al. A design thinking approach to effective vaccine safety communication. Curr Drug Saf. 2015;10(1):31–40.
- Herath C, Zhou Y, Gan Y, et al. A comparative study of interprofessional education in global health care: a systematic review. Medicine. 2017;96(38):e7336.
- Drozd EM, Miller L, Johnsrud M. Impact of pharmacist immunization authority on seasonal influenza immunization rates across states. Clin Ther. 2017;39(8):1563–1580 e1517.
- Harris K, Maurer J, Black C, et al. Workplace efforts to promote influenza vaccination among healthcare personnel and their association with uptake during the 2009 pandemic influenza A (H1N1). Vaccine. 2011;29(16):2978–2985.
- Jacobson Vann JC, Szilagyi P. Patient reminder and patient recall systems to improve immunization rates. Cochrane Database Syst Rev. 2005;3:CD003941.
- Larson HJ, Cooper LZ, Eskola J, et al. Addressing the vaccine confidence gap. Lancet. 2011;378(9790):526–535.
- Ozawa S, Stack ML. Public trust and vaccine acceptance–international perspectives. Hum Vaccin Immunother. 2013;9(8):1774–1778.
- Murakami H, Kobayashi M, Hachiya M, et al. Refusal of oral polio vaccine in northwestern Pakistan: a qualitative and quantitative study. Vaccine. 2014;32(12):1382–1387.
- Jegede AS. What led to the Nigerian boycott of the polio vaccination campaign? PLoS Med. 2007;4(3):e73.
- Oubari H, Tuttle R, Rath B, et al. Communicating vaccine safety to the media and general public. Curr Drug Saf. 2015;10(1):80–86.
- Hardt K, Schmidt-Ott R, Glismann S, et al. Sustaining vaccine confidence in the 21st century. Vaccines. 2013;1(3):204–224.
- World Health Organization. Vaccination and trust library [Internet]. Geneva (Switzerland): World Health Organization. [cited 21 Sep 2017]. Available from: http://www.euro.who.int/en/health-topics/disease-prevention/vaccines-and-immunization/publications/vaccination-and-trust
- Muzumdar JM, Pantaleo NL. Comics as a medium for providing information on adult immunizations. J Health Commun. 2017;22(10):783–791.
- Diamond J, McQuillan J, Spiegel AN, et al. Viruses, vaccines and the public. Mus Soc Issues. 2016;11(1):9–16.
- Brewer NT, Chapman GB, Gibbons FX, et al. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol. 2007;26(2):136–145.
- Ropeik D. How society should respond to the risk of vaccine rejection. Hum Vaccin Immunother. 2013;9(8):1815–1818.
- Signorelli C, Iannazzo S, Odone A. The imperative of vaccination put into practice. Lancet Infect Dis. 2018;18(1):26–27.
- Pianigiani G. Proof of children’s vaccinations? Italy will now take parents’ word for it [Internet]. New York City (NY): The New York Times. [cited 05 Aug 2018]. Available from: https://www.nytimes.com/2018/07/05/world/europe/italy-vaccines.html
- Laws are not the only way to boost immunization. Nature. 2018;553(7688):249–250.
- Rodriguez-Fernandez R, Martinez-Lopez AB, Perez-Moreno J, et al. Impact of an influenza vaccine educational programme on healthcare personnel. Epidemiol Infect. 2016;144(11):2290–2294.
- Danchin MH, Costa-Pinto J, Attwell K, et al. Vaccine decision-making begins in pregnancy: correlation between vaccine concerns, intentions and maternal vaccination with subsequent childhood vaccine uptake. Vaccine. 2017;pii: S0264-410X(17)31069-1. doi: 10.1016/j.vaccine.2017.08.003.
- Quadri-Sheriff M, Hendrix KS, Downs SM, et al. The role of herd immunity in parents’ decision to vaccinate children: a systematic review. Pediatrics. 2012;130(3):522–530.
- Standaert BA, Rappuoli R. How is the economic assessment of vaccines performed today? J Mark Access Health Policy. 2017;5(1):1335163.
- Lu PJ, O’Halloran A, Ding H, et al. Uptake of influenza vaccination and missed opportunities among adults with high-risk conditions, United States, 2013. Am J Med. 2016;129(6):636e1–636e11.
- Hyle EP, Rao SR, Jentes ES, et al. Missed opportunities for measles, mumps, rubella vaccination among departing U.S. adult travelers receiving pretravel health consultations. Ann Intern Med. 2017;167(2):77–84.
- Link-Gelles R, Chamberlain AT, Schulkin J, et al. Missed opportunities: a national survey of obstetricians about attitudes on maternal and infant immunization. Matern Child Health J. 2012;16(9):1743–1747.
- Subbarao K, Matsuoka Y. The prospects and challenges of universal vaccines for influenza. Trends Microbiol. 2013;21(7):350–358.